Published online Apr 26, 2022. doi: 10.12998/wjcc.v10.i12.3764
Peer-review started: June 26, 2021
First decision: September 1, 2021
Revised: October 14, 2021
Accepted: March 4, 2022
Article in press: March 4, 2022
Published online: April 26, 2022
Processing time: 298 Days and 22 Hours
The clinical advantages of painless colonoscopy can reduce the fear and discomfort of patients and increase the detection rate of diseases. Propofol has the characteristics of fast effect and short action time. It is a common choice for painless endoscopic sedation and anesthetics. However, propofol can cause severe respiratory and circulatory depression. Therefore, it is important to find a way to reduce the dose of propofol.
To explore the effect of wrist-ankle acupuncture on propofol dose during colonoscopy.
Two hundred patients who were going to receive selective painless colonoscopy in Hebei Hospital of Traditional Chinese Medicine were selected and divided into wrist-ankle acupuncture group (WAA group, n = 100) and control group (CON group, n = 100). After entering the operation room, patients were given 0.025 mg/kg nabufine intravenously and propofol at the initial dose of 0.5 mg/kg. In patients who did not fall asleep, propofol (10 mg/time) was given until loss of consciousness. Prior to anesthesia, patients in WAA group were punctured by specialist in the inferior 1, 2 and 3 regions according to the zoning principle of wrist-ankle acupuncture. The primary endpoint was required dose of propofol, and the secondary endpoints were the incidence of hypoxemia and hypotension. Furthermore, the following data were recorded: The operation time, wake-up time, incidence of nausea and vomiting, incidence of abdominal distention, post-colonoscopy pain, examiners' satisfaction, patients' satisfaction and Borg fatigue index. This study has been registered in the Chinese Clinical Trial Registry (Registration Code: ChiCTR1900022177).
The induced dose of propofol and the total dose of propofol in WAA group were 80 mg and 110 mg, respectively, which were significantly lower than those in CON group (P < 0.05). The incidences of hypoxemia and hypotension in the WAA group were 2.2% and 3.3%, respectively, significantly lower than those in the CON group (P < 0.05). The incidence of abdominal distension in the WAA group was 8.8%, which was significantly lower than that in the CON group (P < 0.05, 28.9%). The waking time of WAA group was 3.26 ± 0.87 min, which was significantly lower than that of CON group (6.06 ± 0.88 min, P < 0.05).
Wrist-ankle acupuncture can reduce the induction dose and total dose of propofol as well as the incidence of adverse reactions in painless colonoscopy without affecting the satisfaction of examiners and patients. This procedure is simple in operation and easy to promote in clinical practice.
Core Tip: Two hundred patients scheduled for painless colonoscopy were selected and divided into wrist-ankle acupuncture group (n = 100) and control group ( n = 100). The operation time, recovery time, incidence of nausea and vomiting, incidence of abdominal distension, pain after colonoscopy, satisfaction of examiners, satisfaction of patients and Borg fatigue index were recorded. The results showed that ankle acupuncture can reduce the induction dose and total dose of propofol, reduce the occurrence of adverse reactions of painless colonoscopy and does not affect the satisfaction of examiners and patients.
- Citation: He T, Liu C, Lu ZX, Kong LL, Li Y, Xu Z, Dong YJ, Hao W. Effect of wrist-ankle acupuncture on propofol dosage during painless colonoscopy: A randomized controlled prospective study. World J Clin Cases 2022; 10(12): 3764-3772
- URL: https://www.wjgnet.com/2307-8960/full/v10/i12/3764.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i12.3764
Wrist-ankle acupuncture was developed by Professor Zhang Xinshu from the Department of Psychiatry and Neurology, the First Affiliated Hospital of the Second Military Medical University of the Chinese People’s Liberation Army. Inspired by acupuncture, acupuncture points and acupuncture method, a therapy gradually developed from practice. Wrist-ankle acupuncture is the abbreviation of wrist-ankle acupuncture therapy. It refers to the method of selecting a specific needle entry point at the wrist and ankle and piercing a certain length along the longitudinal axis of the limb along the subdermis to treat diseases. Compared with other acupuncture therapies, it has the characteristics of simple acupoint selection, long needle retention time, safety and reliability and no side effects. Therefore, the operation of wrist-ankle acupuncture is simpler and does not require electric acupuncture and other equipment, so it is easier to apply in anesthesia[1-2].
Colonoscopy is the gold standard for diagnosing lower gastrointestinal diseases. However, it is an invasive examination that inevitably brings pain to the examinee. To deal with that, painless colonoscopy is commonly applied clinically for examination. The most adopted anesthetics for painless colonoscopy at the moment primarily consist of intravenous anesthetics and anesthetic sedatives, among which propofol and etomidate are the most common ones[3-4]. In terms of its clinical superiority, painless colonoscopy can reduce patients' fear and discomfort and improve the detection rate of disease. Propofol is characterized by quick effect and short action time, which is a common choice of sedative and anesthetics in painless endoscopy. However, propofol can cause severe respiratory and circulatory inhibition. Therefore, it is of great clinical significance to find an approach to reduce the dose of propofol. Recent application of acupuncture anesthesia has gradually achieved good results in the field of digestive endoscopy[5]. Accordingly, this study was carried out to analyze whether wrist-ankle acupuncture during painless colonoscopy can reduce the induction dose and total dose of propofol, so as to reduce the occurrence of related complications.
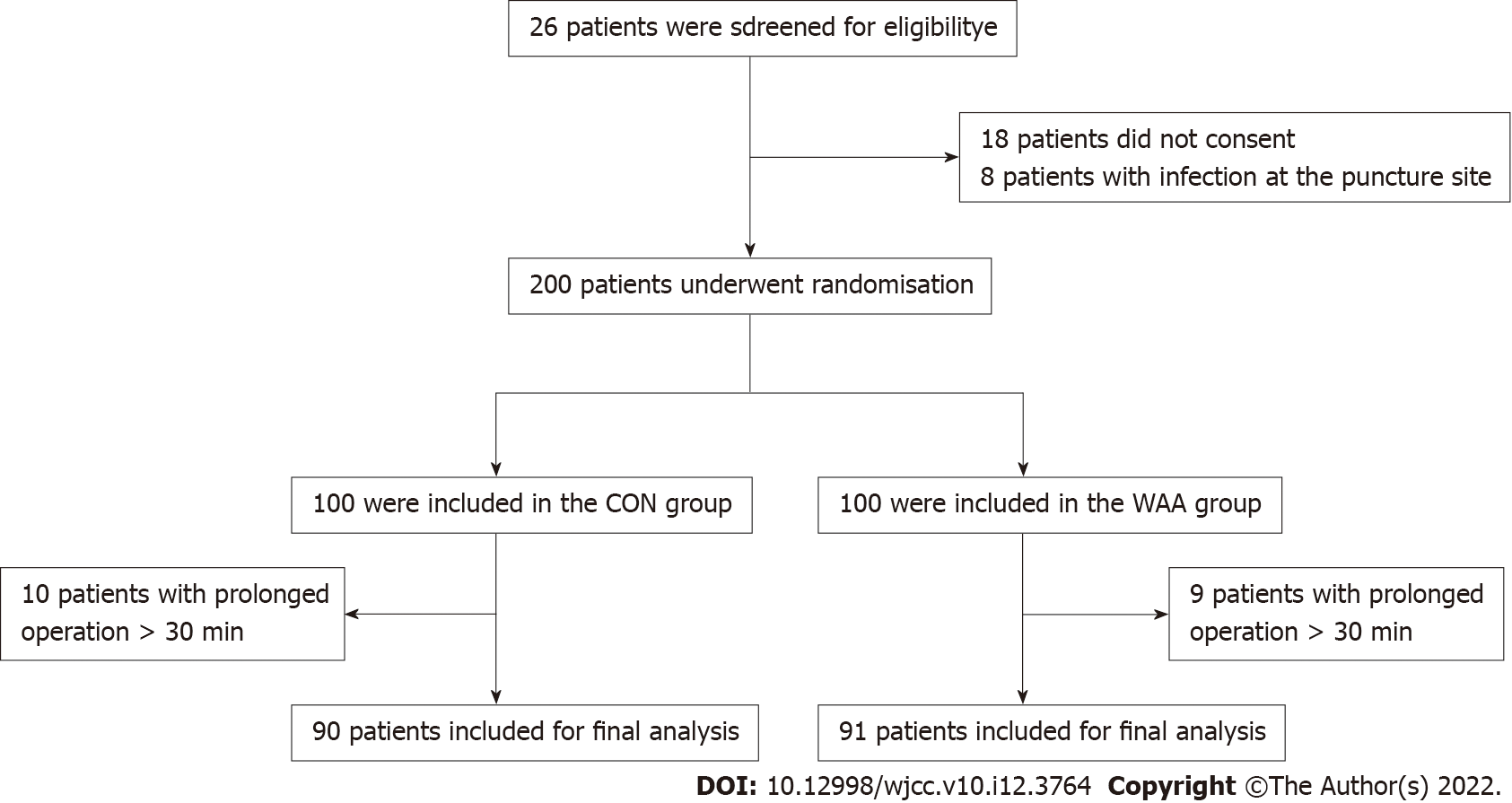
The subjects of this study were 200 patients who were going to receive selective painless colonoscopy in Hebei Hospital of Traditional Chinese Medicine from August 2019 to November 2019. Enrolled patients were divided into wrist-ankle acupuncture group (WAA group, n=100) and control group (CON group, n = 100) based on the random number table method. Finally, 91 cases were included in WAA group and 90 cases in CON group after the exclusion of 19 cases from the study due to prolonged operation time (> 30 min) (Figure 1).
Inclusion criteria: (1) Patients 18-79 years old; (2) American Society of Anesthesiologists classification of grade I-II; and (3) No contraindications for colonoscopy.
Exclusion criteria: (1) Patients who refused painless colonoscopy; (2) Pregnant woman; (3) Patients with allergic history of propofol injection; (4) Patients who were intolerant to opioids; (5) Patients who took potential neuromodulatory drugs (e.g., diazepam, etc) before operation; (6) Patients with cerebrovascular accident; (7) Patients with a history of craniocerebral injury or neurosurgery; (8) Patients with impaired verbal communication; (9) Patients with mental disorder; and (10) Patients with infection at the puncture site.
Rejection criteria: (1) Patients with prolonged operation time > 30 min; (2) Patients who voluntarily withdrew from the operation; and (3) Patients who were not anesthetized or operated as required after inclusion. Nineteen cases were rejected for prolonged operation time. The purpose of these criteria was to unify the control standards and to count the rejected cases as attrition. These patients were recorded in the same way as the other patients, but the early data of the cases are not included because these cases are not unified control standards.
This study has been registered in China Clinical Trial Registration Center (registration code: ChiCTR1900022177,http://www.chictr.org.cn/). This study has been approved by the Medical Ethics Committee of Hebei Hospital of Traditional Chinese Medicine, with informed consent signed by all patients.
Enrolled patients were divided into WAA group and CON group based on the random number table method. The allocation was concealed in an opaque envelope. An anesthesiologist trained in wrist-ankle acupuncture was responsible for unsealing the envelope prior to wrist-ankle acupuncture and then performed accordingly but was not responsible for patient care or collection of variable data related to the research. Another anesthesiologist was only in charge of intraoperative management of all patients and was blinded to patient grouping. Meanwhile, the endoscopist (the same physician for colonoscopy) and the nurse (the same trained nurse) were both blinded to the grouping of patients.
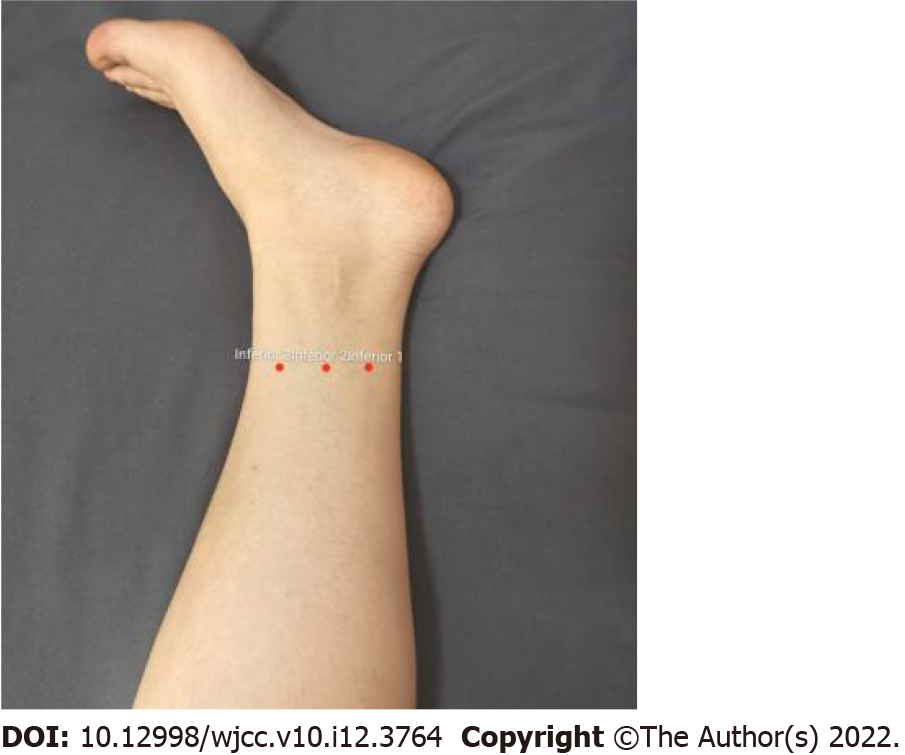
Patients were informed to keep fasting status for 12 h and receive catharsis prior to the examination with the confirmation that no medication was taken before anesthesia. Prior to anesthesia, patients in WAA group were punctured by skilled personnel in the inferior 1, 2 and 3 regions using the needling instrument of filiform needle (No. 32, 1 inch, 0.25 mm × 25 mm in diameter; Hwato, Suzhou, China) according to the zoning principle of wrist-ankle acupuncture (Figure 2). During the operation, patients in both groups were lying on their left side and were given oxygen by nasal catheter (6 L/min), associated with the monitoring of blood pressure, heart rate and pulse oxygen saturation (SpO2). Before the injection, the patients were asked to take several deep breaths, followed by intravenous injection of nabufine (0.025 mg/kg) and infusion of propofol (0.5 mg/kg). After waiting for 5 s, patients who did not fall asleep were given another 10 mg of propofol per time as appropriate. Colonoscopy was not performed until the disappearance of eyelash reflex and no response after calling. When there was movement, frowning and hemodynamic changes (heart rate > 20 times/min, systolic blood pressure > 20% of the basic value) in the patients during operation, additional propofol (10 mg/time) was provided until the patients were unconscious again. During colonoscopy, there was no need for adding propofol when patients opened their eyes without painful expression or movement.
The primary endpoint was the required dose of propofol, while the secondary endpoints were the incidence of hypoxemia (oxygen saturation < 95%) and hypotension (systolic blood pressure < 20%). Furthermore, the following data were recorded: The operation time (from the beginning to the end of the examination), wake-up time (from the end of the examination to the time when patients could correctly answer his/her name and birthday), incidence of nausea and vomiting, incidence of abdominal distention, visual analog scale (VAS) score of pain 15 min and 30 min after entering the recovery room, examiners' satisfaction (VAS score, 0-10 points), patients' satisfaction (VAS score, 0-10 points) and Borg fatigue index.
The examiners' satisfaction and patients' satisfaction: After the examination, the endoscopist and patients used the VAS scale of 0-10 points to evaluate satisfaction with the examination.
Borg fatigue index: 0 point, no fatigue; 0.5 point, extremely slight fatigue, almost imperceptible; 1 point, quite slight fatigue; 2 points, slight fatigue; 3 points, moderate fatigue; 4 points, slightly serious fatigue; 5 points, serious fatigue; 6-8 points, quite serious fatigue; 9 points, extremely serious fatigue; and 10 points, extreme fatigue, reaching the limit.
With α = 0.05 and power = 0.95 as the inspection levels, the mean and the standard deviation of CON group was 145 mg and 72.0, and the mean and the standard deviation of propofol dose was 115 mg and 45 in WAA group, according to the pre-test results. By using a two-tailed test, the sample size of each group was 88 cases by using PASS11.0 statistical software. Considering an escaping rate of 10%, 200 patients were included and randomly divided, with 100 cases in each group.
SPSS 23.0 (Armonk, NY, United States) and GraphPad Prism 7.0 (San Diego, CA, United States) were used for data processing and plotting. Measurement data of normal distribution is expressed as mean ± standard deviation (`x ± s), and the measurement data of non-normal distribution is represented by median (interquartile spacing). χ2 test was used to compare the counting data. Rank-sum test was used for non-normal distribution measurement data in both groups. The measurement data of normal distribution between the two groups were tested by two independent sample t test. Besides, the fatigue index was measured by repeated measurement design analysis of variance. P < 0.05 indicates the difference was statistically significant.
As shown in Table 1, there was no significant difference in sex, age, body mass index and operation time of examination between the two groups (P > 0.05).
| WAA group (n = 91) | CON group (n = 90) | t value/χ2 value | P value | |
| Sex (male/female) | 40/51 | 46/44 | 0.93 | 0.33 |
| Age (years-old) | 49.34 ± 1.11 | 49.73 ± 1.12 | 0.25 | 0.80 |
| Body mass index (kg) | 67.75 ± 13.58 | 65.54 ± 11.50 | 1.18 | 0.24 |
| Operation time of examination (min) | 15.98 ± 0.66 | 16.08 ± 0.63 | 0.11 | 0.91 |
As shown in Table 2, the propofol induction dose and total propofol dose of WAA group was 80 mg and 110 mg, respectively, which were significantly lower than those of CON group (P < 0.05).
| Groups | WAA group (n = 91) | CON group (n = 90) | t value/χ2 value | P value |
| Propofol induction dose (mg) | 80.0 (20) | 115.0 (20) | -9.35 | < 0.0001 |
| Total propofol dose (mg) | 110.0 (40) | 157.5 (70) | -7.15 | < 0.0001 |
| Incidence of hypoxemia, n (%) | 2 (2.2) | 10 (11.1) | 4.46 | 0.035 |
| Incidence of hypotension, n (%) | 3 (3.3) | 14 (15.6) | 7.99 | 0.005 |
| Abdominal distention, n (%) | 8 (8.8) | 26 (28.9) | 11.98 | 0.001 |
| Nausea and vomiting, n (%) | 3 (3.3) | 5 (5.6) | 0.14 | 0.46 |
The incidence of hypoxemia and hypotension in WAA group was 2.2% and 3.3%, respectively, which were significantly lower than those in CON group (P < 0.05).
The incidence of abdominal distention in WAA group was 8.8% (8 cases), which was significantly lower than that in CON group (P < 0.05). There was no significant difference in the incidence of nausea and vomiting between the two groups (P > 0.05), as listed in Table 2.
The wake-up time in WAA group was 3.26 ± 0.87 min, which was significantly lower than that in CON group (6.06 ± 0.88 min, P < 0.05). The VAS score of pain between 15 min and 30 min in WAA group after entering the recovery room was 1.38 ± 0.49 and 0.65 ± 0.48, respectively, which were significantly lower than those in CON group (2.31 ± 0.47 and 1.89 ± 0.32, P < 0.05). Although the VAS scores of pain between 30 min in both groups were lower than their counterparts between 15 min, the downswing of VAS score in WAA group was even more remarkable than in CON group. Meanwhile, the Borg fatigue index 5 min after entering the recovery room in WAA group was 1.74 ± 0.697, which was significantly lower than that in CON group (P < 0.05). No statistically significant difference was observed between the two groups in Borg fatigue index 30 min after entering the recovery room (P > 0.05).
As to patients' satisfaction and examiners' satisfaction about the whole examination, there was no significant difference in the VAS score of patients' satisfaction between the two groups (P > 0.05), but the VAS score of examiners' satisfaction in WAA group (9.89 ± 0.31) was higher than that in CON group (P < 0.05) (Table 3).
| Groups | WAA group | CON group | t value/χ2 value | P value |
| Wake-up time (min) | 3.26 ± 0.87 | 6.06 ± 0.88 | 21.5 | < 0.0001 |
| VAS score of pain between 15 min | 1.38 ± 0.49 | 2.31 ± 0.47 | 13.05 | < 0.05 |
| VAS score of pain between 30 min | 0.65 ± 0.48 | 1.89 ± 0.32 | 20.56 | < 0.05 |
| Borg fatigue index (5 min) | 1.74 ± 0.697 | 2.57 ± 0.498 | 84.92 | < 0.001 |
| Borg fatigue index (30 min) | 0.396 ± 0.492 | 0.278 ± 0.450 | 2.82 | 0.095 |
| Patients' satisfaction (VAS) | 9.57 ± 0.50 | 9.44 ± 0.50 | 1.71 | 0.88 |
| Examiners' satisfaction (VAS) | 9.89 ± 0.31 | 9.28 ± 0.45 | 158.97 | < 0.001 |
Propofol and opioids are the most commonly used painless drugs clinically. However, each of these drugs causes respiratory depression[6], and the combined use of midazolam or propofol with opioids may further increase the risk of hypoxemia and apnea[7-8]. According to the statistics of reviews related to claims in medical accidents, respiratory depression caused by excessive sedation plays a key role in painless treatment of patients' injuries[9]. The rate of respiratory and hemodynamic complications reached 10.?%-14.5% when using propofol for painless treatment[10-11]. Nowadays, attempts have been made to introduce other methods to reduce the dose of propofol, so as to reduce the side effects of propofol. It has been studied that a combined use of naborphine and propofol can provide safer anesthesia effect[12]. Besides, non-pharmaceutical methods, such as acupuncture combined with anesthesia, can also reduce the dose of narcotic drugs. Wrist-ankle acupuncture, among those, is a significantly simple, safe and reliable acupuncture therapy[13]. Wrist-ankle acupuncture can take 5 min to realize the effect of increasing pain threshold[15]. Different from traditional acupuncture, it adopts shallow subcutaneous acupuncture without soreness and pain, which improves patient’s acceptance and achieves easy intraoperative retaining. At present, wrist-ankle acupuncture has a good effect on dysmenorrhea. It is widely accepted that the discomfort related to colonoscopy mainly comes from visceral pain secondary to colon expansion and traction[17]. The authors support the theory that it is similar to visceral pain such as dysmenorrhea. Therefore, wrist-ankle acupuncture was applied to observe its effect on propofol dose during painless colonoscopy.
Reducing the induction dose and total dose of propofol can greatly decrease the complication related to anesthesia during painless colonoscopy. In this study, the mechanism of wrist-ankle acupuncture to reduce the anesthetic dose may be that acupuncture increases cerebral blood flow[18] and changes the permeability of blood-brain barrier[19], resulting in the enhanced permeability of blood-brain barrier to propofol and accelerated onset time of propofol, thus reducing the induction dose of propofol. In practice, our data indicated that many patients had opened their eyes at the end of examination. However, patients in WAA group had less complaints, movements or painful expressions, and there was no impact on the examination of the patients, leading to a reduced propofol dose in this group. The decreased demand for propofol in the process is speculated to be related to the good analgesic effect of wrist-ankle acupuncture[20-22].
Hypoxia and apnea caused by respiratory depression and airway obstruction are the most common cardiopulmonary complications of painless colonoscopy[23]. In our study, the incidence of hypoxemia and hypotension in WAA group was less than that in CON group, because wrist-ankle acupuncture can reduce the dose of propofol, especially during induction when there was a concentrated application of propofol, which might induce a higher risk of respiratory inhibition and circulatory fluctuation. In this regard, respiratory depression and hypotension were relieved in patients consequently owing to the reduced propofol dose during induction by using wrist-ankle acupuncture.
Generally, there is a need to pump air into the intestine to expand the field of vision during colonoscopy, which may produce pressure on the intestinal wall. Patients may feel abdominal pain and distention within hours or even days after the examination[24]. The movement of intestine is manifested as circular muscle contraction in fasting state after colonoscopy, which restricts the movement of colonic contents to the distal colon[25]. Abdominal distention after colonoscopy can cause anxiety and discomfort, which greatly reduce the comfort experience of patients. In this study, the incidence of abdominal distention was significantly reduced in WAA group than that in CON group (P < 0.05). It is believed that wrist-ankle acupuncture can reduce the activity of sympathetic nerve and improve the tension of the vagus nerve to realize their balance[26]. It can thus promote intestinal peristalsis to expel expanding gases rapidly, reduce the incidence of abdominal distention and relieve the anxiety of patients. It is suggested that patients in the WAA group can wake up quickly after anesthesia. This may be related to the decrease in the dose of propofol or the increase in β-endorphin secretion caused by wrist-ankle acupuncture to regulate body fatigue. Inter-group comparison indicated that the wake-up time of WAA group was superior to that of CON group, which may be caused by the decrease of total propofol dose during the whole operation, so that the patients could wake up more rapidly from anesthesia.
Furthermore, the detection result of the Borg fatigue index was better in WAA group than that in CON group 5 min after entering the recovery room. However, no obvious statistical difference was found between the two groups 30 min after entering the recovery room.
It suggests that patients in WAA group have a rapid wake-up from anesthesia. It may be related to the reduced propofol dose, or increased β-endorphin secretion resulted from wrist-ankle acupuncture to regulate human fatigue[27-29].
After the examination of patients in the two groups, the examiners' satisfaction was improved compared with in the CON group. It can be explained that the examination turnover time was shorter in WAA group since patients in this group woke up faster, and thus it was more popular with doctors. Besides, the patients' satisfaction was similar in the two groups although the incidence of abdominal distention after examination was higher in CON group. We believe that it is related to the sufficient communication with patients before examination. Patients have sufficient understanding and expectation of the occurrence of postoperative abdominal distention and thus better postoperative acceptance. Therefore, it has no significant influence on the satisfaction of patients.
There was statistically significant difference of VAS scores between the two groups at 5 min and 15 min after entering the recovery room. However, the estimated scores were all < 3 points, and the result has no significant clinical significance in our opinion. The authors consider that it may be attributed to the fact that the pain is generally mild after colonoscopy, and both groups of patients used naborphine, which may cover the symptoms of patients in CON group. There may be differences between the two groups in the case when naborphine is not used.
Meanwhile, naborphine was administrated to patients according to body weight, and thus there was no difference in the dose between the two groups.
Our study was designed as a randomized controlled study with certain limitations. It is necessary to conduct in-depth research and discussion on the related mechanism with respect to the phenomena observed in the study.
In summary, wrist-ankle acupuncture combined with propofol can significantly reduce propofol dose during painless colonoscopy, decrease the incidence of adverse drug reactions, reduce the incidence of abdominal distention after examination, improve examiners' satisfaction and safety of colonoscopy and reduce the wake-up time of patients. Thus, drug anesthesia combined with wrist-ankle acupuncture is a feasible treatment method worthy of clinical application and promotion.
Propofol is a common choice for painless endoscopic sedation and anesthetics, but it can cause severe respiratory and circulatory depression. Therefore, it is important to find a way to reduce the dose of propofol.
Wrist-ankle acupuncture may reduce propofol dose during colonoscopy.
To determine if control group patients were different from the wrist-ankle acupuncture group regarding advantages in operation time, waking time, incidence of nausea and vomiting, incidence of abdominal distension, pain after colonoscopy, examiner satisfaction, patient satisfaction and Borg fatigue index.
During colonoscopy, the wrist-ankle needle was inserted to explore whether the dose of propofol could be reduced. Patient's operation time, waking time, incidence of nausea and vomiting, incidence of abdominal distension, pain after colonoscopy, examiner satisfaction, patient satisfaction and Borg fatigue index during painless colonoscopy were compared between wrist-ankle acupuncture group and the control group.
Wrist-ankle acupuncture can reduce the induced dose and total dose of propofol, reduce the incidence of adverse reactions of painless colonoscopy and does not affect the satisfaction of the examiner and the patient.
Wrist-ankle acupuncture combined with propofol can significantly reduce propofol dose during painless colonoscopy, decrease the incidence of adverse drug reactions, reduce the incidence of abdominal distention after examination, improve examiners' satisfaction and safety of colonoscopy and reduce the wake-up time of patients.
The wrist-ankle needle is simple to operate and can reduce the dosage of propofol, and it is easy to promote in clinical practice.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: El-Nakeep S, Egypt; Patro BP, India S-Editor: Wu YXJ L-Editor: Filipodia P-Editor: Wu YXJ
| 1. | Zhang XS, Ling CQ, Zhou QH. Practical wrist and ankle needle therapy. Beijing: People's Medical Publishing House, 2002.23-28Dong Ying (reviewer), Yang Wenjun (reviser). Analysis of the epidemiological characteristics and morbidity of gastrointestinal cancer [J]. Yixue Pinglun. 2014;20:429-431. |
| 2. | Zeng K, Zhou QH. Clinical application and research progress of wrist and ankle acupuncture in the treatment of pain [J]. Zhenjiu Linchuang Zazhi. 2012;9:69-72. |
| 3. | Song YR. Anesthesia of painless colonoscopy [J]. Yixue Qianyan. 2015;13:342-343. [DOI] [Full Text] |
| 4. | Zhang XM, Han SS, Hai JY. Anesthesia effect of painless enteroscope [J]. Beifang Yaoxue Zazhi. 2017;3:188. |
| 5. | Wang RQ, Cai HL, Zheng W. Application of acupuncture anesthesia in diagnosis and treatment of digestive endoscopy [J]. Anmo Kangfu Yixue. 2015;6:32-33. |
| 6. | American Society of Anesthesiologists Task Force on Sedation and Analgesia by Non-Anesthesiologists. Practice guidelines for sedation and analgesia by non-anesthesiologists. Anesthesiology. 2002;96:1004-1017. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1504] [Cited by in RCA: 1313] [Article Influence: 57.1] [Reference Citation Analysis (0)] |
| 7. | Bailey PL, Pace NL, Ashburn MA, Moll JW, East KA, Stanley TH. Frequent hypoxemia and apnea after sedation with midazolam and fentanyl. Anesthesiology. 1990;73:826-830. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 442] [Cited by in RCA: 362] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 8. | Nieuwenhuijs DJ, Olofsen E, Romberg RR, Sarton E, Ward D, Engbers F, Vuyk J, Mooren R, Teppema LJ, Dahan A. Response surface modeling of remifentanil-propofol interaction on cardiorespiratory control and bispectral index. Anesthesiology. 2003;98:312-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 96] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 9. | Bhananker SM, Posner KL, Cheney FW, Caplan RA, Lee LA, Domino KB. Injury and liability associated with monitored anesthesia care: a closed claims analysis. Anesthesiology. 2006;104:228-234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 291] [Cited by in RCA: 225] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 10. | McQuaid KR, Laine L. A systematic review and meta-analysis of randomized, controlled trials of moderate sedation for routine endoscopic procedures. Gastrointest Endosc. 2008;67:910-923. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 332] [Cited by in RCA: 368] [Article Influence: 21.6] [Reference Citation Analysis (1)] |
| 11. | Qadeer MA, Vargo JJ, Khandwala F, Lopez R, Zuccaro G. Propofol vs traditional sedative agents for gastrointestinal endoscopy: a meta-analysis. Clin Gastroenterol Hepatol. 2005;3:1049-1056. [RCA] [DOI] [Full Text] [Cited by in Crossref: 165] [Cited by in RCA: 169] [Article Influence: 8.5] [Reference Citation Analysis (1)] |
| 12. | Pang XJ, Tang FX, Shi XQ. Clinical study on the painless colonoscopy with nabufine and propofol [J]. Zhongguo Yiyao Kexue. 2019;9:131-133. |
| 13. | Wang Q, Zhou QH. Theoretical origin and clinical application of wrist-ankle acupuncture [J]. Zhongguo Zhenjiu. 2017;37:509-512. [RCA] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 14. | Wu GC. Study on the clinical application and mechanism of acupuncture analgesia by combination of acupuncture and medicine [J]. Yixue Yanjiu. 2001;30:22-23. |
| 15. | Wang HB, Zhao S, Sun N, Li XQ, Ma SX, Li Q, Cui JM. Observation on therapeutic effect of wrist-ankle acupuncture on primary dysmenorrhea of college students [J]. Zhongguo Zhenjiu. 2013;33:996-999. [DOI] [Full Text] |
| 16. | Forster C, Vanhaudenhuyse A, Gast P, Louis E, Hick G, Brichant JF, Joris J. Intravenous infusion of lidocaine significantly reduces propofol dose for colonoscopy: a randomised placebo-controlled study. Br J Anaesth. 2018;121:1059-1064. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 52] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 17. | Zhang HX, Zhou L, Zhang TF. Effect of scalp acupuncture on acute focal cerebral ischemia-reperfusion injury in rats[J]. Zhejiang Zhongxiyi Jiehe Zazhi. 2006;16:268-269. |
| 18. | Zhang M, Zhang JY, Zhong W. Research progress of blood brain barrier opening method [J]. Guoji Yaoxue Yanjiu Zazhi. 2016;43:126-133. |
| 19. | Lin XM, Tan KP, Zhang AJ. The effect of electroacupuncture on the permeability of nerve growth factor to the blood-brain barrier and its mechanism [J]. Zhenjiu Yanjiu. 2009;34:110-113. |
| 20. | Chen L, Wang J. Research progress on humoral regulation mechanism of acupuncture analgesia [J]. Shanghai Zhongyiyao Zazhi. 2015;49:91-93. |
| 21. | Zhou QH, Hu X, Gu W. Observation on the analgesic effect of wrist-ankle acupuncture on moderate and severe liver cancer pain [J]. Zhejiang Zhongyixueyuan Xuebao. 2005;1:53-55. [DOI] [Full Text] |
| 22. | Zhao S, Zheng H, Zhan L, Zhu M. [Clinical observation of wrist-ankle needle therapy combined with patient controlled intravenous analgesia for pain after laparoscopic surgery for eccyesis]. Zhongguo ZhenJiu. 2017;37: 1173-1175. [RCA] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 23. | Qadeer MA, Lopez AR, Dumot JA, Vargo JJ. Hypoxemia during moderate sedation for gastrointestinal endoscopy: causes and associations. Digestion. 2011;84:37-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 88] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 24. | Fan HZ, Sheng JW, Yao LQ, Lou XY. The clinical study of reducing abdominal pain after colonoscopy with carbon dioxide [J]. Zhongguo Linchuang Yixue. 2010;1:42-44. |
| 25. | Yao T, Zeng JM, Fan XL. Physiology [M]. Beijing: People's Medical Publishing House, 2005; 303.. |
| 26. | Li T, Chen JQ, Xiao HL. Research progress of acupuncture on heart rate variability [J]. Zhenjiu Linchuang Zazhi. 2010;26:66-68. |
| 27. | Meng H, Wang JJ, Jiang HG, Lin L, Shi YJ, Tu Y. Effect of electroacupuncture on β-endorphin in hypothalamus of chronic stress-induced fatigue model rats [J]. Zhenjiu Linchuang Zazhi. 2003;19:59-60. |
| 28. | Hu X, Gu W, Zhou QH, Ling CQ. Analgesic effect of wrist-ankle acupuncture on pain of liver cancer and its effect on neuropeptides [J]. Zhongxiyi Jiehe Ganbing Zazhi. 2005;15:131-133. |
| 29. | Chen PB, Wang T, Yang XF, Cui J, Xia ZH. Analgesic effect of wrist and ankle on patients with cervical spondylosis and plasma? Shanghai Zazhi. 2018;37:1419-1423. [DOI] [Full Text] |