Published online Apr 26, 2022. doi: 10.12998/wjcc.v10.i12.3677
Peer-review started: August 10, 2021
First decision: October 20, 2021
Revised: November 1, 2021
Accepted: March 14, 2022
Article in press: March 14, 2022
Published online: April 26, 2022
Processing time: 254 Days and 10.2 Hours
In a previous study, basilar artery occlusion (BAO) was shown to lead to death or disability in 80% of the patients. The treatment for BAO patients in the acute stage includes thrombolysis and intra-arterial thrombectomy, but not all patients benefit from these treatments. Thus, understanding the predictors of outcome before initiating these treatments is of special interest.
To determine the predictors related to the 90-d clinical outcome in patients with BAO in an Asian population.
We performed a retrospective case review of patients admitted to a tertiary stroke center between 2015 and 2019. We used the international classification of diseases-10 criteria to identify cases of posterior circulation stroke. A neurologist reviewed every case, and patients fulfilling the criteria defined in the Basilar Artery International Cooperation Study were included. We then analyzed the patients’ characteristics and factors related to the 90-d outcome.
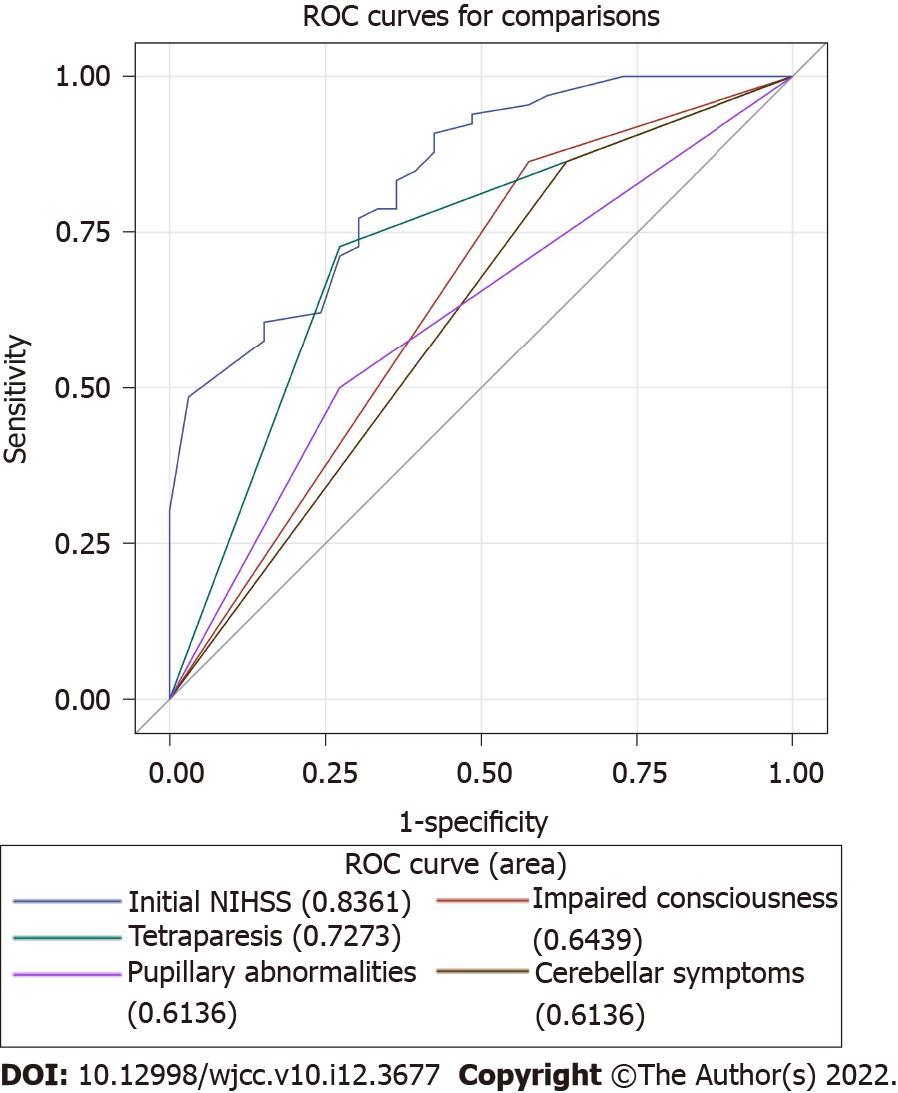
We identified a total of 99 patients as real BAO cases. Of these patients, 33 (33.3%) had a favorable outcome at 90 d (modified Rankin Scale: 0–3). Moreover, 72 patients received intra-arterial thrombectomy, while 13 patients received intravenous tissue-type plasminogen activator treatment. We observed a favorable outcome in 33.3% of the cases and an unfavorable outcome in 66.7% of the cases. We found that the initial National Institutes of Health Stroke Scale (NIHSS) score and several BAO symptoms, including impaired consciousness, tetraparesis, and pupillary abnormalities, were significantly associated with an unfavorable outcome (P < 0.05), while cerebellar symptoms were associated with a favorable outcome (P < 0.05). In the receiver operating characteristic (ROC) analysis, the areas under the ROC curve of initial NIHSS score, impaired consciousness, tetraparesis, cerebellar symptoms, and pupillary abnormalities were 0.836, 0.644, 0.727, 0.614, and 0.614, respectively. Initial NIHSS score showed a higher AUROC (0.836) compared to BAO symptoms.
The most important predictor of an unfavorable outcome was the initial NIHSS score. BAO symptoms, including tetraparesis, impaired consciousness, and pupillary abnormality were also related to an unfavorable outcome.
Core Tip: In the emergency department, basilar artery occlusion (BAO) stroke is always severe, devastating, and difficult to diagnose. And it is more difficult to determine the further treatment, thrombectomy or not? We perform a retrospective study to investigate the outcome predictors of BAO. Our study showed that initial National Institutes of Health Stroke Scale (NIHSS) was the strongest predictor to the 90 d functional outcome. And we found a best cut-off value of NIHSS 30. That is, the score higher than 30 always relate to poor outcome, even received thrombectomy. We suggest that BAO patients with NIHSS higher than 30 may not benefit from thrombectomy treatment.
- Citation: Chiu YC, Yang JL, Wang WC, Huang HY, Chen WL, Yen PS, Tseng YL, Chen HH, Tsai ST. Predictors of unfavorable outcome at 90 days in basilar artery occlusion patients. World J Clin Cases 2022; 10(12): 3677-3685
- URL: https://www.wjgnet.com/2307-8960/full/v10/i12/3677.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i12.3677
Basilar artery occlusion (BAO) is a type of acute ischemic stroke that accounts for 1% of all ischemic strokes and 8% of all symptomatic vertebrobasilar territory ischemia cases[1]. Compared with patients with anterior circulation stroke, those suffering from BAO have a high risk of morbidity and death despite the acute treatment of intravenous thrombolysis (IVT) or intra-arterial thrombectomy (IAT)[2]. Mechanical thrombectomy is beneficial for patients suffering from stroke caused by the occlusion of the proximal anterior circulation[3]. However, evidence supporting the use of IAT for BAO is still lacking, particularly in Asian populations[4]. Although some studies have shown that this intervention in patients with BAO may be effective and safe[5], large prospective observational studies have suggested that not all patients with BAO benefit from IAT or IVT[4].
Acute treatment for BAO is determined individually by the first-line stroke neurologist; thus, a comprehensive knowledge of the predictors of favorable outcome can facilitate the decision-making process and establish appropriate expectations for patients and their families[6].
A myriad of evidence shows that the initial National Institutes of Health Stroke Scale (NIHSS) score predicts clinical outcome in BAO patients[1,2,6-8]. Current meta-analyses[9] and systemic reviews[10] have confirmed that lower initial NIHSS scores independently and significantly predict favorable 90-d functional outcomes. In the multicenter, prospective Basilar Artery International Cooperation Study (BASICS) of 619 patients, there was a difference in the efficacy of treatment strategies among patients depending on the severity of the stroke. However, only few studies investigated the NIHSS[9,11] in detail. In our study, we analyzed 99 BAO patients and focused on the initial NIHSS score and other factors related to the 90-d functional outcome.
We aimed to assess the correlation between clinical outcome and possible prognostic factors, including initial NIHSS, age, sex, comorbidities, stroke type, BAO symptoms, and different treatments for BAO to promote personalized treatments for BAO that can enhance the probability of a favorable outcome.
The China Medical University Hospital (CMUH) is located in central Taiwan and has a 2054-bed capacity. The stroke center treats approximately 1300 acute ischemic stroke patients and performs 90 tissue plasminogen activator (tPA) thrombolysis procedures and 120 intra-arterial thrombectomies annually[12].
We retrospectively reviewed patient medical record data acquired between January 1, 2015 and December 31, 2019. We used the international classification of diseases-10 (ICD-10) criteria to select the admission cases of acute ischemic stroke at posterior circulation (I63.02, I63.12, I63.22, I65.1)[13]. Using the above criteria, we identified 339 cases of suspected vertebral or BAO. BAO status was confirmed by a stroke neurologist (STT) using brain scans as well as the criteria defined in the BASICS study[4]. BAO was defined as a complete obstruction of flow in the proximal, middle, or distal portion of the basilar artery by computed tomography angiography, magnetic resonance angiography, or conventional contrast angiography. Patients with bilateral vertebral artery occlusions with retrograde filling of the basilar artery were excluded. Based on these criteria, 99 cases were confirmed as BAO and were included in subsequent analyses. Among these, 72 cases received IAT, while 13 cases received IVT.
A duty neurologist routinely recorded critical variables including age, sex, NIHSS score, Glasgow Coma scale score, stroke symptoms, and cardiovascular risk factors. The time of symptom onset was also recorded; if unknown, it was considered as the last time the patient was seen well. We also defined stroke subtypes according to the TOAST classification[14]. A stroke case manager reviewed the aforementioned data of every stroke patient on the following workday.
The CMUH comprehensive stroke center follows the treatment guidelines of the Taiwan Stroke Society[15,16]. All the thrombectomies were performed by the same neuro-intervention team in the same room equipped with a biplane cerebral angiography. We used modern devices such as a stent retriever (e.g., Solitaire) and the ADAPT method by the Penumbra system[10].
This study received ethical approval from the China Medical University Hospital, CMUH109-REC2-003.
The covariates evaluated in this study included age, sex, initial NIHSS, prodromal symptoms, BAO symptoms and its duration, comorbidities prior to the admission date, acute treatment (IVT or IAT), IAT parameters (thrombolysis in cerebral infarction scale, total passage time, sent insertion, and tirofiban use), and stroke classification. The primary outcome of interest was the 90-d modified Rankin Scale (mRS) score[17]. We chose mRS to evaluate the primary outcome because of its global use and proven validity and reliability[18]. The mRS has a score range of 0–6. Based on previous study findings, we defined an mRS score of 0–3 as a favorable outcome of BAO and an mRS score of 4–6 as an unfavorable outcome[19]. For this study, we determined which covariate factors influenced the 90-d outcomes of patients suffering from BAO.
The major adverse event related to IAT and IV tPA was symptomatic intracranial hemorrhage. It was defined as a computed tomography-documented hemorrhage in combination with a more than 4-point change of the NIHSS score[20].
We used the Mann–Whitney U test and χ2 tests to calculate P values for continuous and categorical variables, respectively. We then used the receiver operating characteristic (ROC) curve analysis based on the logistic regression model to analyze the accuracy of discriminating the patients with unfavorable outcomes. All statistical analyses were performed using SAS (SAS Institute, Cary, NC, United States) version 9.4. All data were reported as mean ± SD for continuous variables and frequency (percentage) for categorical variables. The threshold for statistical significance was set at P = 0.05 based on a two-tailed test.
We identified a total of 99 patients with BAO between January 1, 2015 and December 31, 2019. Our study population consisted of 32 women and 67 men, with a mean age of 67 years. We observed favorable outcomes (mRS: 0–3) in 33.3% of the cases and unfavorable outcomes (mRS: 4–6) in 66.7% of the cases. The median NIHSS score at admission was 25 (IQR: 14–30). Among the study population, 72 patients received IAT alone or combined with IVT (IAT group), while 13 patients received IVT (Table 1).
| n | Overall | mRS 0–3 (n = 33) | mRS 4–6 (n = 66) | P value | |
| Age (yr) | 99 | 67 (60.2, 76) | 65.8 (60.4, 74) | 67.9 (59.5, 76.3) | 0.689 |
| Women, n (%) | 99 | 32 (32.3) | 9 (27.3) | 23 (34.6) | 0.447 |
| Initial NIHSS (IQR) | 99 | 25 (14, 30) | 11 (7, 25) | 29 (23, 33) | < 0.001 |
| Risk factors, n (%) | |||||
| Hypertension | 99 | 81 (81.8) | 28 (84.9) | 53 (80.3) | 0.580 |
| Diabetes mellitus | 99 | 43 (43.4) | 15 (45.5) | 28 (42.4) | 0.774 |
| Atrial fibrillation | 99 | 35 (35.3) | 10 (30.3) | 25 (37.9) | 0.457 |
| Hyperlipidemia | 99 | 37 (37.4) | 16 (48.5) | 21 (31.8) | 0.106 |
| CAD | 99 | 15 (15.1) | 8 (24.2) | 7 (10.6) | 0.074 |
| Previous stroke | 99 | 23 (23.2) | 6 (18.2) | 17 (25.8) | 0.400 |
| Smoking | 99 | 46 (46.5) | 17 (51.5) | 29 (43.9) | 0.476 |
| Etiology, n (%) | 98 | 1 | |||
| Large-artery artherosclerosis | 66 (67.3) | 22 (66.7) | 44 (67.7) | ||
| Cardioembolism | 5 (5.1) | 2 (6.1) | 3 (4.6) | ||
| Stroke of undetermined etiology | 27 (27.6) | 9 (27.3) | 18 (27.7) | ||
| Prodromal symptoms, n (%) | |||||
| Vertigo or dizziness | 99 | 27 (27.3) | 12 (36.4) | 15 (22.7) | 0.151 |
| Confusion | 99 | 10 (10.1) | 3 (9.1) | 7 (10.6) | 1 |
| Unsteady gait | 99 | 14 (14.1) | 6 (18.2) | 8 (12.1) | 0.542 |
| BAO symptoms, n (%) | |||||
| Duration hours, median (IQR) | 98 | 4 (2, 10) | 3.5 (2, 10) | 4 (3, 10) | 0.552 |
| Impaired consciousness, n (%) | 99 | 76 (76.8) | 19 (57.6) | 57 (86.4) | 0.001 |
| Tetraparesis, n (%) | 99 | 57 (57.6) | 9 (27.3) | 48 (72.7) | < 0.001 |
| Bulbar symptoms | 99 | 75 (75.6) | 26 (78.8) | 49 (74.2) | 0.619 |
| Cerebellar symptoms, n (%) | 99 | 21 (21.2) | 12 (36.4) | 9 (13.6) | 0.009 |
| Vertigo or dizziness | 99 | 32 (32.3) | 13 (39.4) | 19 (28.8) | 0.288 |
| Nausea | 99 | 17 (17.2) | 8 (24.2) | 9 (13.6) | 0.187 |
| Oculomotor abnormalities | 99 | 68 (68.7) | 19 (57.6) | 49 (74.2) | 0.092 |
| Pupillary abnormalities, n (%) | 99 | 42 (42.4) | 9 (27.3) | 33 (50) | 0.031 |
| IAT | 99 | 72 (72.7) | 21 (63.6) | 51 (77.3) | 0.151 |
| IV tPA | 99 | 13 (13.1) | 4 (12.1) | 9 (13.6) | 1 |
| SICH | 99 | 5 (5) | 1 (3) | 4 (6) |
The two patients who received IAT and three patients who received medical treatment alone developed symptomatic intracranial hemorrhage. Among these five patients, one had a favorable outcome, while four had an unfavorable outcome. The overall in-hospital mortality rate was 17.2% (17 out of 99 cases).
We found that the initial NIHSS, impaired consciousness, tetraparesis, and pupillary abnormalities were significantly associated with an unfavorable outcome, while cerebellar symptoms were associated with a favorable outcome (Table 1).
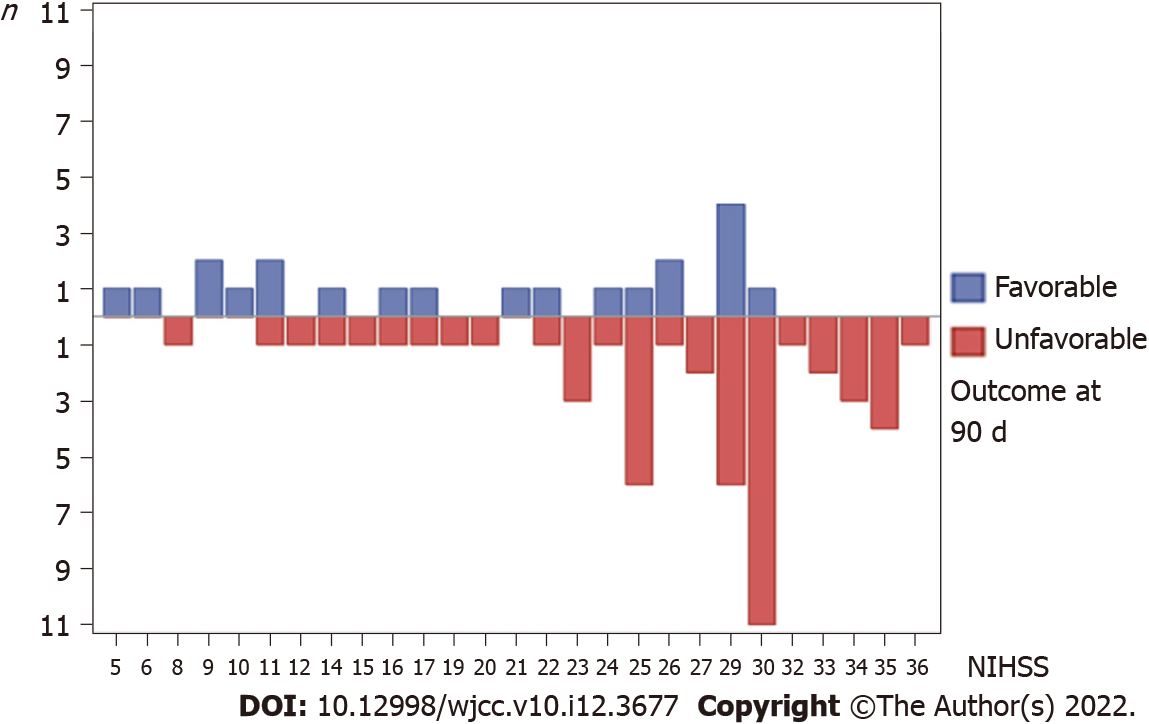
In the ROC analysis, the areas under the ROC curve of initial NIHSS, impaired consciousness, tetraparesis, cerebellar symptoms, and pupillary abnormalities were 0.836, 0.644, 0.727, 0.614, and 0.614, respectively (Figure 1). The NIHSS score was a strong predictor of the 90-d functional outcome. Moreover, we found that an NIHSS score higher than 30 was significantly associated with poor outcome in our population (Figure 2).
In our cohort, sex, gender, underline comorbidities, duration hours, and receiving IVT or IAT did not influence the outcome of BAO.
Our study represented an Asian population from a single center with a BAO diagnosis treated with IAT treatment or medical treatment alone within 24 h of symptom onset. We found that in patients who received IAT, the initial NIHSS score and BAO symptoms with tetraparesis, impaired consciousness, and pupillary abnormalities were significantly related to an unfavorable outcome at 90 d.
The initial NIHSS was a strong predictor of the 90-d functional outcome in our study. We found that patients with an initial NIHSS score higher than 30 faced difficulties reaching a functional, independent status 90 d after stroke. In our cohort, none of the 20 patients who with an initial NIHSS score higher than 30 achieved a favorable outcome at the 90-d mark.
We found two previous studies discussing the cutoff value of NIHSS in patients with BAO. In France, Fahed et al[9] found that an NIHSS score of 30 or higher was associated with mortality at 90 d, with an odds ratio of 5.569[9]. The patients’ characteristics in their study were similar to those of our cohort. Luo et al[11] found that an NIHSS score of 22 or higher significantly lowered the chance of obtaining a good clinical outcome at 90 d (mRS: 0–2), with an odds ratio of 0.157[11].
To understand how the symptoms of BAO can predict outcomes, we analyzed the recorded symptoms of BAO and found that only tetraparesis, impaired consciousness, and pupillary abnormalities indicated an unfavorable outcome in our cohort. These deficits are mostly due to occlusion of the distal basilar artery that results in infarctions in mesencephalon and thalamus[1]. It is also known that the severity of clinical symptoms is related to collaterals[1]. In a case series, BA embolism stroke most often affected the distal third[21]; therefore, sudden embolic stroke could lead to more initial severe deficits and thus result in an unfavorable outcome.
In the BASICS study, patients with a mild-to-moderate deficits had the worst outcome with IAT if the latency to treatment was longer than 9 h[4]. In our study, we applied IAT to patients with BAO up to 24 h after symptoms onset due to the poor natural course of BAO and found that the chance of improvement was significant. Contrary to the BASICS study[4], the time of presentation was not associated with outcomes in our cohort. It is possible that a highly developed and persistent collateral arterial network, and delicate plasma flow siding the clot might sustain the patency of brainstem perforators, thus rendering the time window for recanalization therapy in BAO a less important factor[22].
Our study has several limitations, including the retrospective, non-controlled study design; thus, a selection bias could not be excluded. We also had a small number of patients in the non-IAT group, which limited the multivariate analysis. In addition, we used the ICD-10 to select the patients, but some patients could have been missed if they were not coded correctly[23]. Finally, IV tPA was used in some eligible patients in both IAT and non-IAT group, and the use of tPA may have affected the clinical outcomes. Therefore, a large, randomized controlled trial will be essential to elucidate the clinical course of BAO and to better predict who will benefit from IAT, especially in an Asian population.
In our single center case series of BAO, 17.2% of the patients died in the hospital and only 33% reached a favorable outcome at 90 d. High initial NIHSS score and the BAO symptoms of tetraparesis, consciousness change, and pupillary abnormalities also indicated an unfavorable outcome at 90 d. We also found that patients with an initial NIHSS score higher than 30 did not easily reach a favorable outcome and did not benefit from IAT. A large, prospective clinical study will be important to further aid our understanding of this devastating disease.
Basilar artery occlusion (BAO) led to death or disability in 80% of the patients in a previous study. The acute treatment for BAO patients includes intravenous thrombolysis and intra-arterial thrombectomy (IAT), but not all patients benefit from these treatments.
To date, large-scale studies on the clinical characteristic and predictors of BAO patients are still lacking.
To determine the predictors related to the 90-d clinical outcome in patients with BAO in an Asian population.
We performed a retrospective case review of patients admitted to a tertiary stroke center between 2015 and 2019. We used the international classification of diseases-10 criteria to identify cases of posterior circulation stroke. A neurologist reviewed every case, and those that fulfilled the criteria defined in the Basilar Artery International Cooperation Study were included. The patients’ characteristics and factors related to outcome at 90 d were analyzed.
We identified 99 patients as real BAO cases. Among these patients, 33 (33.3%) had a favorable outcome at 90 d (modified Rankin Scale: 0–3). Moreover, 72 patients received IAT, while 13 patients received intravenous tissue-type plasminogen activator treatment. We found that initial National Institutes of Health Stroke Scale (NIHSS) and several BAO symptoms including impaired consciousness, tetraparesis, and pupillary abnormalities were significantly associated with an unfavorable outcome (P < 0.05). In the receiver operating characteristic (ROC) analysis, initial NIHSS score showed a higher AUROC (0.836) compared to BAO symptoms.
Initial NIHSS score is the most important predictor of an unfavorable outcome in patients with BAO.
Further large, prospective clinical studies of the outcome predictors of BAO are needed.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: Taiwan Neurological Society, No. 1232.
Specialty type: Medicine, research and experimental
Country/Territory of origin: Taiwan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ghannam WM, Egypt; Lal A, United States S-Editor: Fan JR L-Editor: A P-Editor: Fan JR
| 1. | Mattle HP, Arnold M, Lindsberg PJ, Schonewille WJ, Schroth G. Basilar artery occlusion. Lancet Neurol. 2011;10:1002-1014. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 306] [Cited by in RCA: 405] [Article Influence: 28.9] [Reference Citation Analysis (0)] |
| 2. | Singer OC, Berkefeld J, Nolte CH, Bohner G, Haring HP, Trenkler J, Gröschel K, Müller-Forell W, Niederkorn K, Deutschmann H, Neumann-Haefelin T, Hohmann C, Bussmeyer M, Mpotsaris A, Stoll A, Bormann A, Brenck J, Schlamann MU, Jander S, Turowski B, Petzold GC, Urbach H, Liebeskind DS; ENDOSTROKE Study Group. Mechanical recanalization in basilar artery occlusion: the ENDOSTROKE study. Ann Neurol. 2015;77:415-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 216] [Cited by in RCA: 258] [Article Influence: 25.8] [Reference Citation Analysis (0)] |
| 3. | Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, Dávalos A, Majoie CB, van der Lugt A, de Miquel MA, Donnan GA, Roos YB, Bonafe A, Jahan R, Diener HC, van den Berg LA, Levy EI, Berkhemer OA, Pereira VM, Rempel J, Millán M, Davis SM, Roy D, Thornton J, Román LS, Ribó M, Beumer D, Stouch B, Brown S, Campbell BC, van Oostenbrugge RJ, Saver JL, Hill MD, Jovin TG; HERMES collaborators. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016;387:1723-1731. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4230] [Cited by in RCA: 5414] [Article Influence: 601.6] [Reference Citation Analysis (0)] |
| 4. | Schonewille WJ, Wijman CA, Michel P, Rueckert CM, Weimar C, Mattle HP, Engelter ST, Tanne D, Muir KW, Molina CA, Thijs V, Audebert H, Pfefferkorn T, Szabo K, Lindsberg PJ, de Freitas G, Kappelle LJ, Algra A; BASICS study group. Treatment and outcomes of acute basilar artery occlusion in the Basilar Artery International Cooperation Study (BASICS): a prospective registry study. Lancet Neurol. 2009;8:724-730. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 477] [Cited by in RCA: 563] [Article Influence: 35.2] [Reference Citation Analysis (0)] |
| 5. | van Houwelingen RC, Luijckx GJ, Mazuri A, Bokkers RP, Eshghi OS, Uyttenboogaart M. Safety and Outcome of Intra-Arterial Treatment for Basilar Artery Occlusion. JAMA Neurol. 2016;73:1225-1230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 59] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 6. | Jung S, Mono ML, Fischer U, Galimanis A, Findling O, De Marchis GM, Weck A, Nedeltchev K, Colucci G, Mordasini P, Brekenfeld C, El-Koussy M, Gralla J, Schroth G, Mattle HP, Arnold M. Three-month and long-term outcomes and their predictors in acute basilar artery occlusion treated with intra-arterial thrombolysis. Stroke. 2011;42:1946-1951. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 93] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 7. | Antunes Dias F, Castro-Afonso LH, Zanon Zotin MC, Alessio-Alves FF, Martins Filho RKDV, Camilo MR, Nakiri GS, Abud DG, Pontes-Neto OM. Collateral Scores and Outcomes after Endovascular Treatment for Basilar Artery Occlusion. Cerebrovasc Dis. 2019;47:285-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 8. | Dias FA, Alessio-Alves FF, Castro-Afonso LH, Cougo PT, Barreira CMA, Camilo MR, Nakiri GS, Abud DG, Pontes-Neto OM. Clinical Outcomes of Patients with Acute Basilar Artery Occlusion in Brazil: An Observational Study. J Stroke Cerebrovasc Dis. 2017;26:2191-2198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 9. | Fahed R, Di Maria F, Rosso C, Sourour N, Degos V, Deltour S, Baronnet-Chauvet F, Léger A, Crozier S, Gabrieli J, Samson Y, Chiras J, Clarençon F. A leap forward in the endovascular management of acute basilar artery occlusion since the appearance of stent retrievers: a single-center comparative study. J Neurosurg. 2017;126:1578-1584. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 24] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 10. | Watson CCL, Feria A, Chen CJ, Camacho A. Outcomes and Complications of Endovascular Mechanical Thrombectomy in the Treatment of Acute Posterior Circulation Occlusions: A Systematic Review. World Neurosurg. 2021;145:35-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 11. | Luo G, Mo D, Tong X, Liebeskind DS, Song L, Ma N, Gao F, Sun X, Zhang X, Wang B, Jia B, Fernandez-Escobar A, Miao Z. Factors Associated with 90-Day Outcomes of Patients with Acute Posterior Circulation Stroke Treated By Mechanical Thrombectomy. World Neurosurg. 2018;109:e318-e328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 58] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 12. | Tsai ST, Wang WC, Lin YT, Huang WS, Huang HY, Wang CJ, Lin EZ, Kung WL, Guo YC, Lin KH, Lu MK, Yen PS, Chen WL, Tseng YL, Kuo CC, Cho DY, Chen CC, Tsai CH. Use of a Smartphone Application to Speed Up Interhospital Transfer of Acute Ischemic Stroke Patients for Thrombectomy. Front Neurol. 2021;12:606673. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Hsieh MT, Hsieh CY, Tsai TT, Wang YC, Sung SF. Performance of ICD-10-CM Diagnosis Codes for Identifying Acute Ischemic Stroke in a National Health Insurance Claims Database. Clin Epidemiol. 2020;12:1007-1013. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 73] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 14. | Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, Marsh EE 3rd. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993;24:35-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7474] [Cited by in RCA: 8872] [Article Influence: 277.3] [Reference Citation Analysis (0)] |
| 15. | Chen CH, Sung SF, Hsieh CY, Chen PL, Tsai LK, Huang HY, Jeng JS. 2019 Taiwan Stroke Society Guideline for Intravenous Thrombolysis in Acute Ischemic Stroke Patients. Formos J Stroke. 2019;. [DOI] [Full Text] |
| 16. | Tang SC, Chen CJ, Lee CW, Wang KC, Lai YJ, Chi NF, Yeh SJ, Chan L, Jeng JS, Liu HM. 2019 Taiwan Stroke Society Guideline for Endovascular Thrombectomy in Acute Ischemic Stroke Patients. Formos J Stroke. 2019;. [DOI] [Full Text] |
| 17. | Fuentes B, Alonso de Leciñana M, Ximénez-Carrillo A, Martínez-Sánchez P, Cruz-Culebras A, Zapata-Wainberg G, Ruiz-Ares G, Frutos R, Fandiño E, Caniego JL, Fernández-Prieto A, Méndez JC, Bárcena E, Marín B, García-Pastor A, Díaz-Otero F, Gil-Núñez A, Masjuán J, Vivancos J, Díez-Tejedor E; Madrid Stroke Network. Futile Interhospital Transfer for Endovascular Treatment in Acute Ischemic Stroke: The Madrid Stroke Network Experience. Stroke. 2015;46:2156-2161. [RCA] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 65] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 18. | Banks JL, Marotta CA. Outcomes validity and reliability of the modified Rankin scale: implications for stroke clinical trials: a literature review and synthesis. Stroke. 2007;38:1091-1096. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 994] [Cited by in RCA: 1553] [Article Influence: 86.3] [Reference Citation Analysis (0)] |
| 19. | Rangaraju S, Haussen D, Nogueira RG, Nahab F, Frankel M. Comparison of 3-Month Stroke Disability and Quality of Life across Modified Rankin Scale Categories. Interv Neurol. 2017;6:36-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 87] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 20. | Wahlgren N, Ahmed N, Dávalos A, Ford GA, Grond M, Hacke W, Hennerici MG, Kaste M, Kuelkens S, Larrue V, Lees KR, Roine RO, Soinne L, Toni D, Vanhooren G; SITS-MOST investigators. Thrombolysis with alteplase for acute ischaemic stroke in the Safe Implementation of Thrombolysis in Stroke-Monitoring Study (SITS-MOST): an observational study. Lancet. 2007;369:275-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1562] [Cited by in RCA: 1666] [Article Influence: 92.6] [Reference Citation Analysis (0)] |
| 21. | Voetsch B, DeWitt LD, Pessin MS, Caplan LR. Basilar artery occlusive disease in the New England Medical Center Posterior Circulation Registry. Arch Neurol. 2004;61:496-504. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 147] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 22. | Lindsberg PJ, Pekkola J, Strbian D, Sairanen T, Mattle HP, Schroth G. Time window for recanalization in basilar artery occlusion: Speculative synthesis. Neurology. 2015;85:1806-1815. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 84] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 23. | McCormick N, Bhole V, Lacaille D, Avina-Zubieta JA. Validity of Diagnostic Codes for Acute Stroke in Administrative Databases: A Systematic Review. PLoS One. 2015;10:e0135834. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 277] [Cited by in RCA: 330] [Article Influence: 33.0] [Reference Citation Analysis (0)] |