Copyright
©The Author(s) 2019.
World J Clin Cases. Mar 26, 2019; 7(6): 717-726
Published online Mar 26, 2019. doi: 10.12998/wjcc.v7.i6.717
Published online Mar 26, 2019. doi: 10.12998/wjcc.v7.i6.717
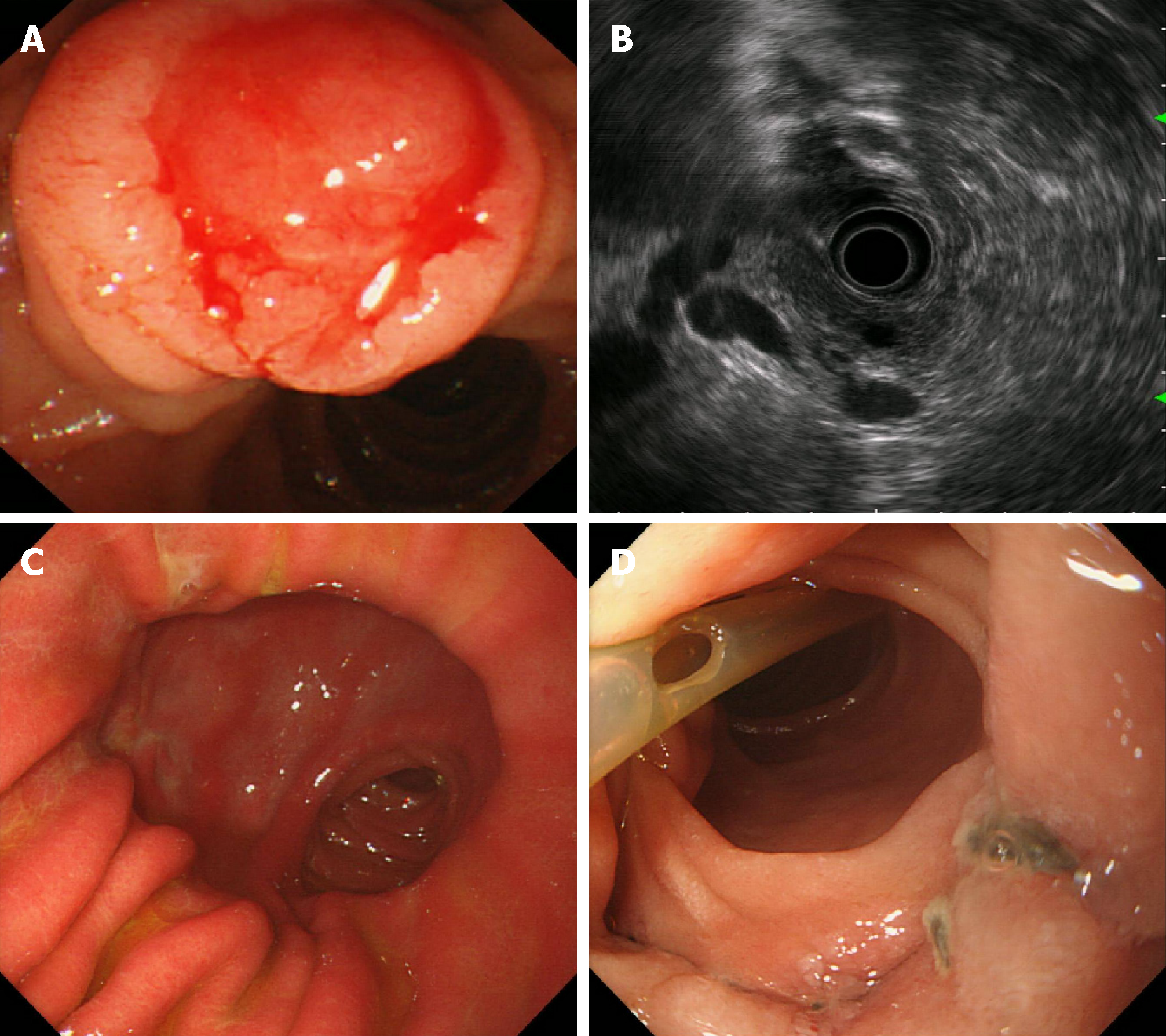
Figure 1 Gastroscopic images and endoscopic ultrasonography.
A: A swollen duodenal papilla that bled easily when touched; B: Periampullary endoscopic ultrasound showing bile duct and pancreatic duct expansion; C: Gastroscopic image 3 mo after operation; a small amount of bile refluxed to the stomach cavity, with no gastric ulcer; D: Site of bile duct, pancreatic duct, and duodenal anastomosis replantation; no anastomotic tumor relapse; visible suture knot; pancreatic duct supporting tube fell off.
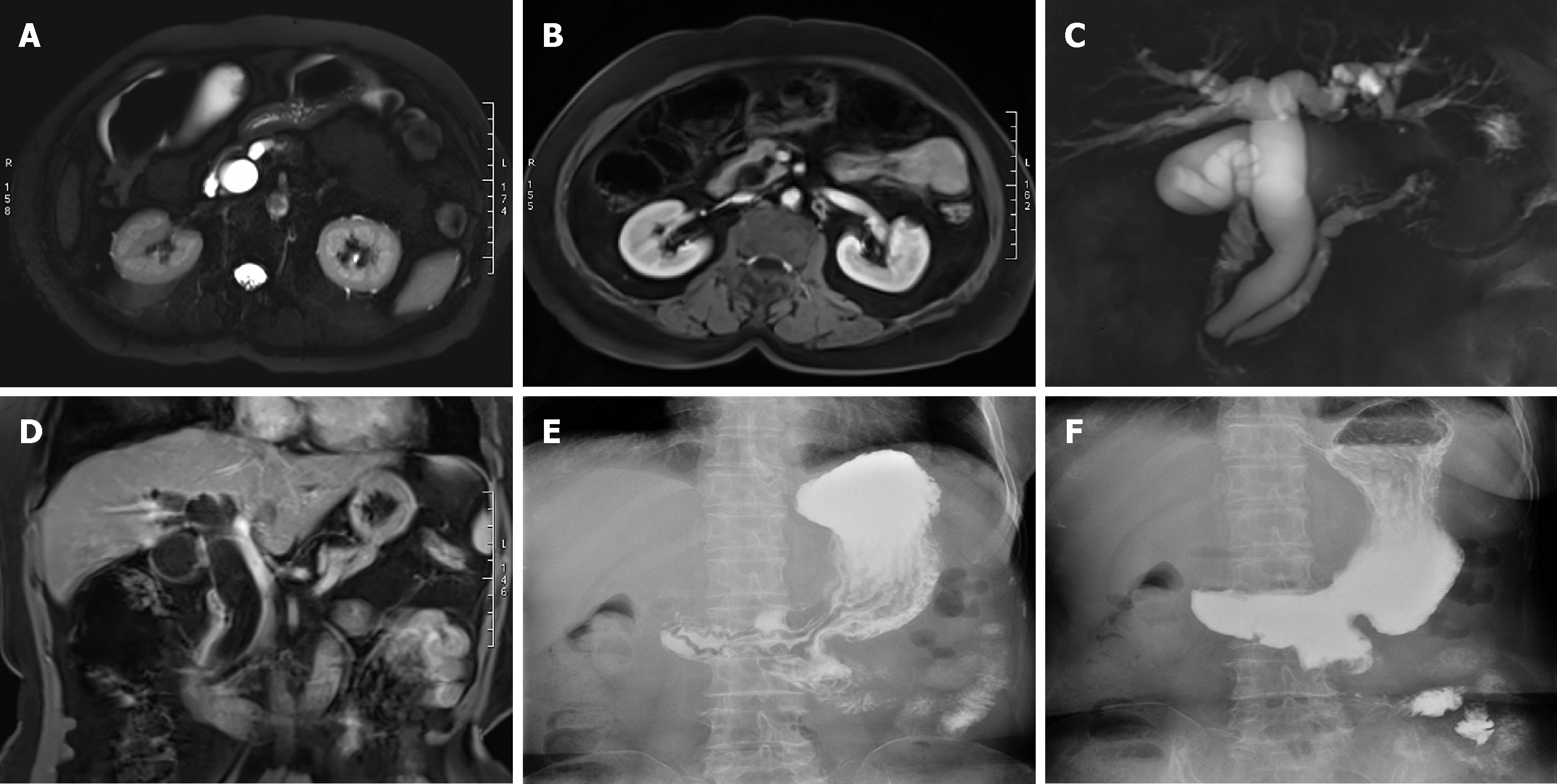
Figure 2 Magnetic resonance imaging and upper gastrointestinal iodine oil radiography.
A: Magnetic resonance imaging (MRI) T2-weighted imaging (T2WI) showing bile duct and pancreatic duct expansion; B: Enhanced MRI T1-weighted imaging (T1WI) showing bile duct and pancreatic duct expansion; C: Magnetic resonance cholangiopancreatography showing bile duct and pancreatic duct expansion and separation in the ampulla; D: Coronal MRI T1WI showing bile duct and pancreatic duct expansion; E: Upper gastrointestinal iodine oil radiography 6 mo after operation; gastric jejunum anastomosis showed stronger gastric emptying function; F: Common bile duct and pancreatic duct nonvisualization; no bile reflux in different phases.
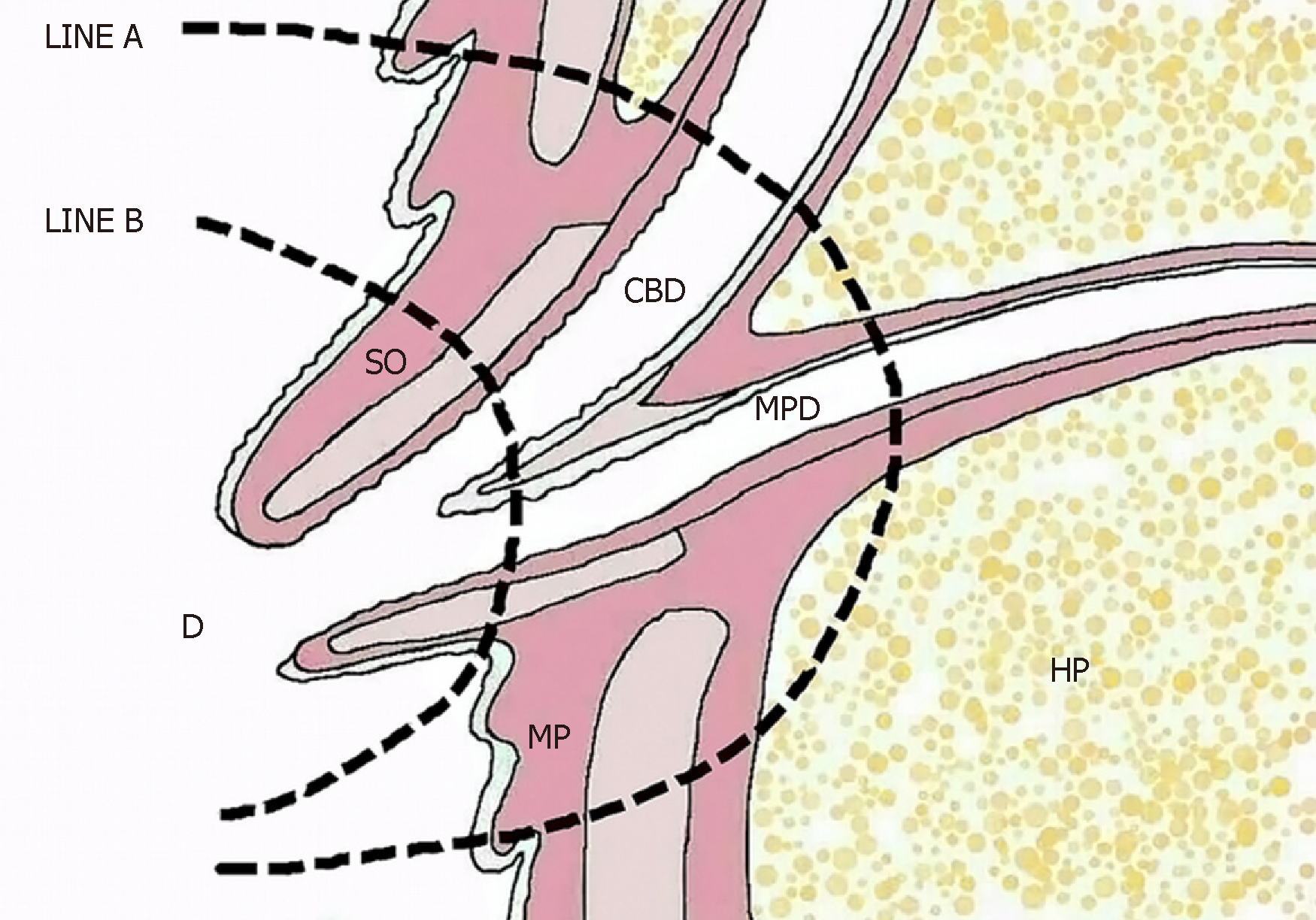
Figure 3 Diagrammatic drawing showing the ampulla of Vater.
LINE A: Local resection line; LINE B: Endoscopic papillectomy line prior to the muscularis propria. CBD: Common bile duct; MP: Muscularis propria; HP: Head of the pancreas; MPD: Main pancreatic duct; SO: Sphincter of Oddi; D: Duodenum.
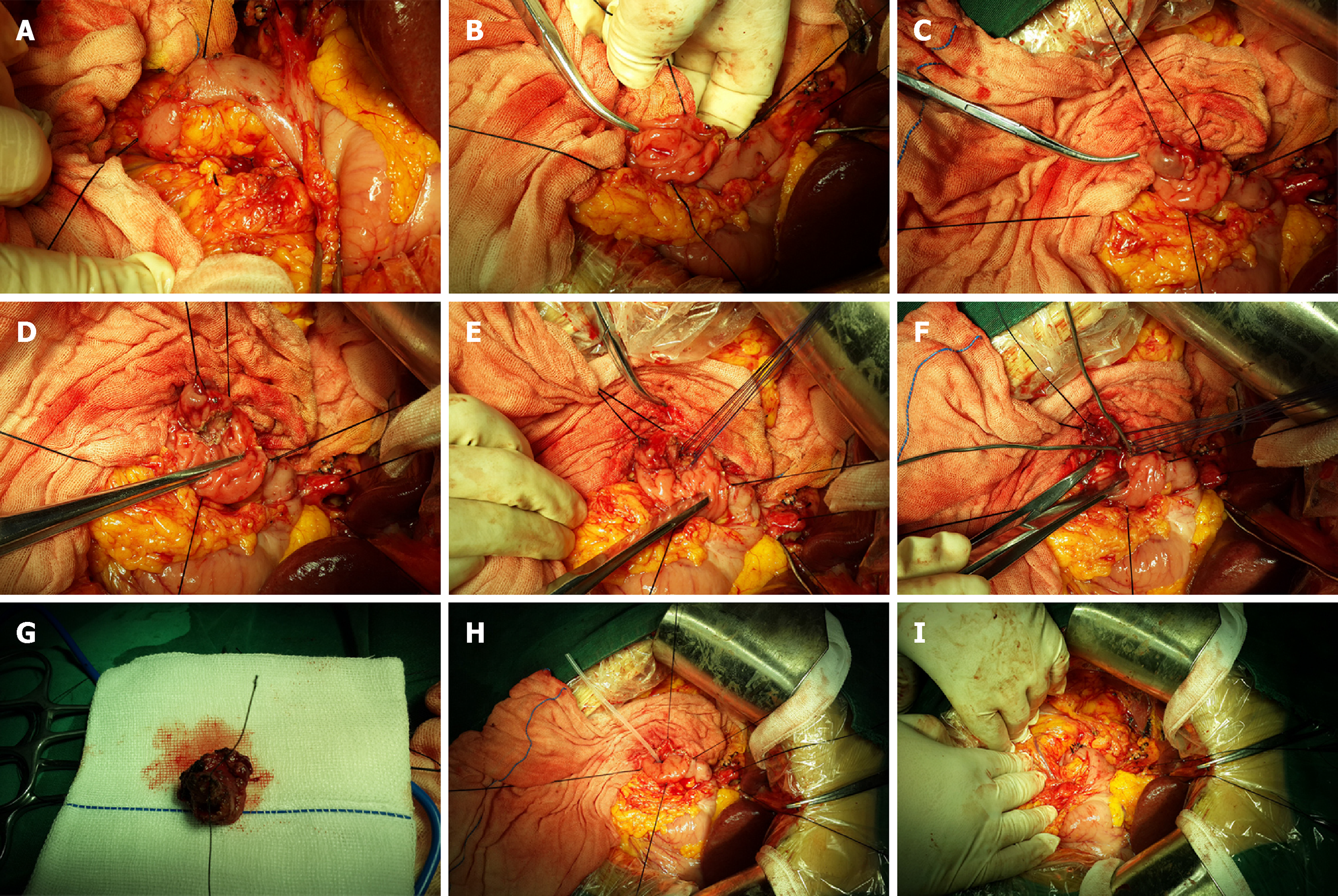
Figure 4 Surgical procedure.
A: Kocher incision, dissociation of the lateral peritoneum of the duodenal descending portion, exposure of the duodenal descending portion, and search for the position of the duodenal papilla; lesions were accurately detected; B: Anterior wall of the duodenum; lengthwise incision at the duodenal descending section showing the periampullary lesions; C: Exposure and lifting of the duodenal papilla using a transfixion suture; D: Maintaining an appropriate distance around the base of the periampullary tumor, we cut open the duodenal mucosa and the mucosal muscularis; E: The common bile duct and the main pancreatic duct end were anastomosed with the duodenal wall using interrupted sutures; F: The bile duct and the pancreatic duct passed through the biliary probes after replantation; G: Complete resection of the periampullary tumor; H: The supporting tube was inserted into the main pancreatic duct and fixed; I: The duodenal intestinal wall was closed with single-layer longitudinal suturing using absorbable sutures.
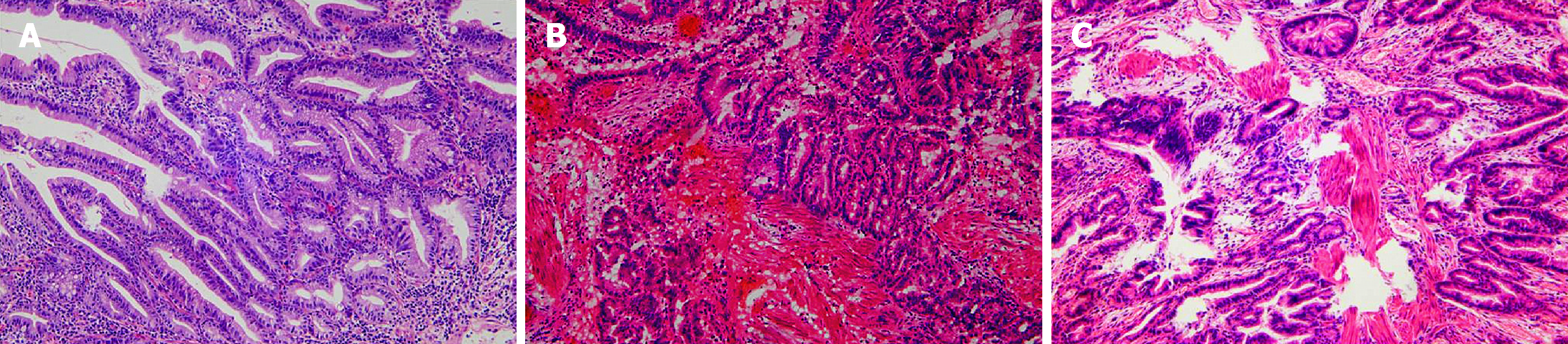
Figure 5 Pathology results (HE staining, ×100).
A: Endoscopic biopsy suggestive of tubulovillous adenoma; B: Intraoperative frozen-section pathology suggestive of adenocarcinoma (pTis); C: Postoperative pathology suggestive of adenocarcinoma (pTis). HE: Hematoxylin and eosin.
- Citation: Liu F, Cheng JL, Cui J, Xu ZZ, Fu Z, Liu J, Tian H. Surgical method choice and coincidence rate of pathological diagnoses in transduodenal ampullectomy: A retrospective case series study and review of the literature. World J Clin Cases 2019; 7(6): 717-726
- URL: https://www.wjgnet.com/2307-8960/full/v7/i6/717.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i6.717