Published online Jul 6, 2015. doi: 10.5527/wjn.v4.i3.388
Peer-review started: June 25, 2014
First decision: September 16, 2014
Revised: October 10, 2014
Accepted: April 8, 2015
Article in press: April 9, 2015
Published online: July 6, 2015
Processing time: 377 Days and 2.5 Hours
Antiretroviral therapy has markedly reduced acquired immune deficiency syndrome-related deaths and opportunistic infectious diseases. This has resulted in prolonged survival of individuals infected with the human immunodeficiency virus (HIV). However, this improvement in survival has been accompanied by an increase in the incidence of chronic kidney disease (CKD) and end-stage renal disease. CKD is now epidemic among HIV-infected populations in both Western and Eastern countries. Risk factors associated with CKD in HIV-infected populations include aging, hypertension, diabetes mellitus, co-infection with hepatitis C virus, a low CD4 cell count, and a high HIV viral load. Clinical experience has shown that HIV-infected individuals often have one or more concurrent risk factors for CKD. The cumulative effect of multiple risk factors on the development of CKD should be noted in this population. Glomerular disease directly related to HIV infection, so-called HIV-associated nephropathy, remains an important cause of CKD among a limited HIV population of African descent, but is less likely to be common among other urban HIV populations. The impact of exposure to nephrotoxic antiretroviral agents on the development of kidney disease is both an old and a new concern. In particular, the association of tenofovir with kidney tubular injury has been an area of great interest. The findings regarding tenofovir’s adverse effect on long-term kidney function vary among studies. The early identification and treatment of CKD is recommended for reducing the burden of patients requiring dialysis in HIV-infected populations. Periodic monitoring of urinary concentrations of albumin, protein, and tubular injury markers such as low-molecular-weight proteins may be useful for the early diagnosis of patients at risk for incident CKD. This review focuses on recent epidemiology, clinical characteristics, and management of CKD in a contemporary HIV-infected population.
Core tip: Kidneys are affected by the human immunode-
ficiency virus (HIV) and its associated therapies. As HIV subjects now have longevity while they receive combination anti-retroviral therapy (cART), kidney disease has been prominent among the current HIV subjects on cART. HIV subjects often have several coexisting risk factors of kidney disease, including diabetes and hypertension. Measurements of albuminuria, proteinuria, urinary low-molecular weight proteins, and serum cystatin C are necessary for early detection of kidney disease. Collaborative discussions between HIV experts and nephrologists are warranted to achieve the good treatment of chronic kidney disease in HIV patients.
- Citation: Ando M, Yanagisawa N. Epidemiology, clinical characteristics, and management of chronic kidney disease in human immunodeficiency virus-infected patients. World J Nephrol 2015; 4(3): 388-395
- URL: https://www.wjgnet.com/2220-6124/full/v4/i3/388.htm
- DOI: https://dx.doi.org/10.5527/wjn.v4.i3.388
Although combination anti-retroviral therapy (cART) has contributed to the longevity in individuals affected by human immunodeficiency virus (HIV), the life-span extension is followed by the emergence of chronic kidney disease (CKD), leading to their high morbidity and mortality[1-9]. Now, nephrologists are faced with several problems related to CKD among HIV populations, including how to find out subclinical kidney insults, to identify incipient stage of kidney illness, and to collaborate with HIV healthcare staff to offer how to treat CKD. The frequency of CKD is increasing in HIV patients living in Asian countries[10,11] likewise in Western countries[12,13]. Generally speaking, as the early identification of kidney disease gives a chance to exert treatments that inhibit progression of kidney dysfunction[14-16], it could be most crucial to find out HIV patients at high risk of incident CKD as the first step in weakening the frequency of CKD in this population[17-19]. The 2012 KDIGO guidelines elaborated the identification and prognosis of CKD by combining albuminuria with estimated glomerular filtration rate (eGFR)[20,21]. The review attempted to summarize recent advances in the study on CKD in the current HIV individuals.
A simple and reliable biomarker of renal insult is persistent urinary excretion of protein or albumin. Whereas 7.2%-13.7% of HIV-infected subjects manifest proteinuria on a urine dipstick test[7,9,10,22-26], 8.7%-17.8% of those subjects have albuminuria, based on the urinary excretion of albumin[10,27,28]. The frequency of a persistent loss in renal function less than 60 mL/min per 1.73 m2 varies between 3.5% and 9.7% in different HIV populations[9-12,26]. When both of the existence of urinary protein and a decline in glomerular function were considered, the frequency of CKD stages 1 to 5 ranged 15% to 24%[2,9,10,12,26]. Difference of the CKD prevalence across various countries has not been studied yet. Table 1 demonstrates the frequency of kidney disease in Japan, China, Europe, and the United States, as previously reported.
| Prevalence (%) | Countries | Ref. | |
| Proteinuria | |||
| 7.20 | United States | [7] | |
| 9.50 | Japan | [11] | |
| 13.70 | China | [10] | |
| Albuminuria | |||
| 8.70 | Norway | [25] | |
| 11.00 | United States | [26] | |
| 17.80 | Japan | [11] | |
| CKD stages 1-5 | |||
| 15.40 | Japan | [11] | |
| 15.50 | United States | [23] | |
| 16.80 | China | [10] | |
| 23.70 | United States | [13] | |
| CKD stages ≥ 3 | |||
| 3.50 | EuroSIDA | [12] | |
| 5.60 | China | [10] | |
| 5.90 | United States | [23] | |
| 9.70 | Japan | [11] | |
| 9.70 | United States | [13] |
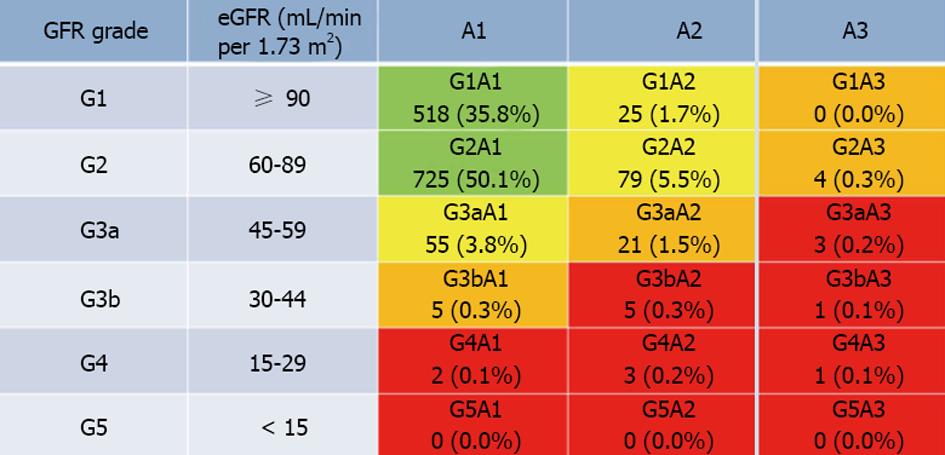
Numerous reports have shown that albuminuria seems to be one of independent risk factors of a poor prognosis among HIV-infected individuals[27,28]. A quite recent paper has shown that low-grade proteinuria is highly prevalent in a large HIV-infected white cohort on cART[29]. It is therefore reasonable to assume that the KDIGO classification would be more practical for the identification of CKD and for estimating prognosis in HIV-infected individuals than the conventional KDOQI staging. However, the measurement of albuminuria is expensive, with public health care insurance systems in most countries limiting the application to follow-up for diabetic nephropathy. Therefore, a total of 1447 HIV-infected Japanese (1351 males, 96 females; mean age, 44.4 ± 11.5 years) were classified using the 2012 KDIGO guidelines for estimating CKD risk: a combination of eGFR and dipstick proteinuria, as a convenient alternative to albuminuria[30]. Proteinuria was classified into 3 grades: [A1] ≤ +/-, [A2] 1+ to 2+, and [A3] 3+ ≤ eGFR was classified into 6 grades: [Gade 1] ≥ 90, [Grade 2] 60-89, [Grade 3a] 45-59, [Grade 3b] 30-44, [Grade 4] 15-29, and [Grade 5] < 15 mL/min per 1.73 m2, using colored heat map zones. It was shown that the prevalence rates of individuals in the green, yellow, orange, and red zones were 85.9%, 11.0%, 2.1%, and 1.0%, respectively. The prevalence of individuals at high and very high risk for a poor prognosis in the KDIGO classification was nearly halved, compared with the risk for CKD ≥ stage 3 in the KDOQI system (3.1% vs 6.6%) (Figure 1).
Glomerular and tubular diseases that are often identified in HIV-infected patients are summarized in Table 2. The traditional problems of HIV-associated nephropathy (HIVAN), HIVIC, and TMA are still crucial because of the delay in HIV diagnosis or the non-response to ART even in the contemporary cART years[31]. Patients at the earlier stage of HIVAN may manifest almost normal kidney glomerular function, albuminuria, or subclinical proteinuria. Their renal function often remains constant over some years after the start of cART[32,33]. HIV-infected individuals with African pedigree have been considered being at higher risk of HIVAN arising from podocyte proliferation and tubular dilatation with atrophy and flattening of the tubular epithelial cells[34,35].
| Diseases | Clinical characteristics |
| HIV-specific glomerular disease | |
| HIVAN | Detectable viral load, a high amount of proteinuria, albuminuria, RPGN |
| HIVIC | Proteinuria and/or hematuria, variable manifestation including AKI |
| TMA | AKI, proteinuria, hematuria with microangiopathic hemolytic anemia and thrombocytopenia |
| HIV-non-specific glomerular disease | |
| HCV-related MPGN/cryoglobulinemia | Proteinuria and/or hematuria, nephritic syndrome, a decrease in serum complements |
| Diabetec nephropathy | Proteinuria (microalbuminuria to nephrotic syndrome), a decrease in GFR |
| Glomerular sclerosis | Older patients, hypertension, no or low amount of proteinuria, coexistence of atherosclerotic diseases |
| Membranous glomerulopathy | Nephrotic syndrome; idiopathic and secondary causes associated with HBV or cancers |
| Minimal change disease | Nephrotic syndrome, use of NSAIDs |
| IgA nephropathy | Hematuria and/or proteinuria with or without renal failure |
| Post-infectious glomerulonephritis | Hematuria and/or proteinuria with or without renal failure |
| ART-associated tubular injury | |
| Acute tubular necrosis | Use of TDF |
| Cristal nephropathy | Use of IDV and ATV |
| Acute or chronic interstitial nephritis | Use of ATV |
Known risk factors of CKD in HIV patients are shown in Table 3. Epidemiologic investigations showed that variates associated with CKD in HIV-infected patients include traditional risks including elder age, hypertension, and DM[9-12,22-26]. This has been confirmed by a report from a prospective study with a 6-year median follow-up including a large white HIV cohort receiving antiretroviral treatment[36]. Lipids levels, decreased CD4 cell counts, and elevated HIV RNA load are perhaps specific risks for HIV-infected subjects[10,11,23-25]. Moreover, HCV infection contributes to renal insults in HIV people[11,25,31]. Nearly 30% of subjects with HIV are affected with HCV[37]. Liangpunsakul et al[38] performed a study to see the association between non-diabetic patients concurrently having HCV and albuminuria, based on a database from the NHANES III. Adjusted for known variates, they demonstrated that HCV co-infection was independently involved in microalbuminuria in individuals without diabetes mellitus. Furthermore, Tsui et al[39] showed a significant relationship between albuminuria and HCV seropositivity in people who were classified by age.
| Variables | Ref. |
| Black race | [34,35] |
| Older age | [9-12,22-26] |
| Low CD4 cell count | [10,11,23-25] |
| High HIV-RNA viral load | [10,11,23-25] |
| Diabetes mellitus | [9-12,22-26] |
| Hypertension | [9-12,22-26] |
| Hepatitis C virus coinfection | [11,25,31,37] |
| Proteinuria | [3,27,28,30] |
| Albuminuria | [3,29,55] |
| eGFR < 90 mL/min per 1.73 m2 | [10,12,23-25] |
| Elevation of urinary tubular markers | [56-64] |
| Use of TDF or ATV | [40-52] |
Some antiretroviral agents are related to kidney disease, hyperlipidemia, diabetes mellitus, and hypertension which may intensify the risk of incidence of CKD[40]. Whereas HIVAN was the major renal involvement before the era of ART, comorbidities and adverse renal effects of various drugs for ART now complicate the landscape of kidney disease in HIV[41]. Drug-induced decrease in kidney function was shown in some NRTIs, TDF, and protease inhibitors (PIs). In those PIs, indinavir is predisposed to generate crystalline stones and it has been changed by PIs with safer agents with integrase inhibition. In addition, atazanavir (ATV) is likely associated with acute interstitial nephritis[42,43] and sub-acute or chronic renal insufficiency due to granulomatous interstitial nephritis characterized by the coexistence of crystalline deposition[44-46]. TDF is secreted from proximal renal tubules, and may be associated with its tubular damage representing mitochondrial dysfunction[47,48]. Although studies of the Gallant et al[49] did not show that tenofovir was responsible for renal failure, HIV-infected groups on TDF at the Johns Hopkins Clinical Cohort had a significant decrease in creatinine clearance for 3 years, as compared to patients not having tenofovir[50]. Nevertheless, another study using the same cohort showed that kidney function did not significantly change between HIV-infected subjects on cART with or without the regimen including tenofovir[51]. These differences between the two studies may be derived from the difference in the cumulative time for cART. The latter included only cART-naïve subjects, while the former included both cART-naïve and -experienced subjects. These disparate results on the TDF’s nephrotoxicity remain conflicting, but a recent meta-analysis showed that the relevance of the adverse impact of TDF is mild, which may imply that restriction of “TDF use without regular monitoring of renal function” is not basically necessary[52]. Table 3 shows the known factors related to CKD in HIV-infected individuals.
The early diagnosis of renal illness in HIV patients is critical for preventing progression of prevalent renal injury and adding suitable treatment promptly. To help HIV experts with the identification of kidney disease, the IDSA guidelines suggest to conduct urinalysis and the evaluation of glomerular function at the diagnosis of HIV infection[3]. Although a dipstick test is a simple measure to use, it is unable to identify subclinical levels of urinary albumin. A comparison of a dipstick test and urinary protein concentration corrected for creatinine (PCR) in HIV-infected patients showed that the dipstick test could not detect individuals with mild or moderate proteinuria[53]. Therefore, the screening of proteinuria should be done according to PCR than dipstick test[54]. Ando et al[55] have found that a moderate to mild level of ACR (30 mg/g > ACR ≥ 10 mg/g) is an indicator of the incidence of CKD, likely emphasizing that the measurement of the ACR may be of higher relevance than that of the PCR for the detection of new CKD among HIV individuals.
The measurement of urinary biomarkers for identifying early tubular damage in HIV subjects, especially receiving cART has special importance. Some researchers measured urinary low-molecular weight proteins to examine whether patients on cART may have kidney tubular injury in the absence of renal dysfunction[56-62]. Approximately a quarter of HIV-infected patients on cART could have prevalent kidney tubular injury in the absence of renal dysfunction, probably resulting in a near future decrease in glomerular function and a higher emergence of urinary protein[63]. Also, Shlipak et al[64] indicated that novel urine biomarkers for tubular injury including KIM-1 and interleukin-18 identify risk for ensuing decrease in renal function in HIV-infected women in the Women’s Interagency HIV Study cohort. Measuring urinary low-molecular-weight proteins could be helpful to the early detection of subjects, particular those who take tenofovir, who have high risk of definite CKD. In addition, Peralta et al[65] showed that some urinary indices of tubular damage are relevant to mortality in the Women’s Interagency HIV Study.
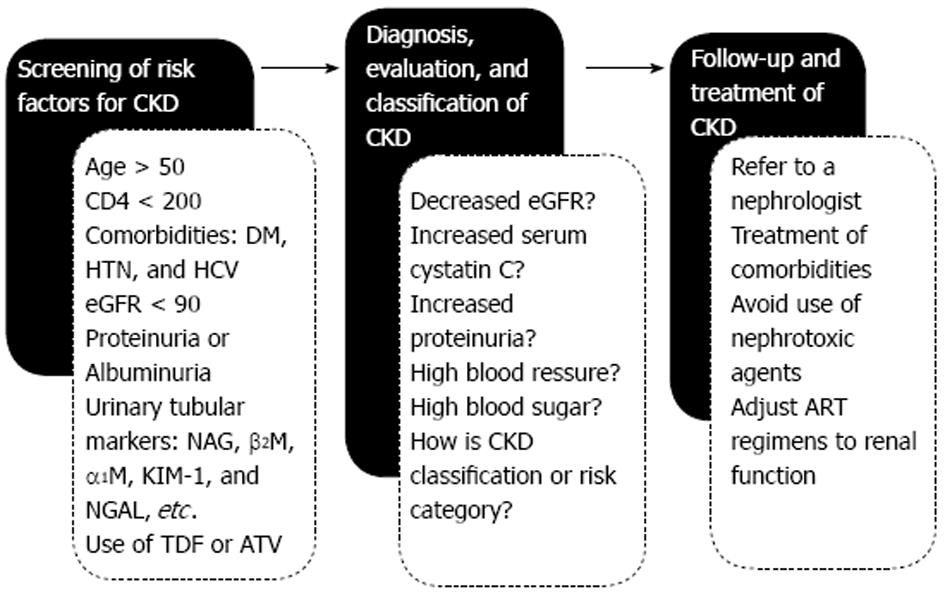
HIV-infected subjects usually possess several co-existing risks associated with renal illness, but the clinical impact of them on the emergence of chronic renal disease has remained unknown. A clinical model of predicting the incidence of CKD has been constructed. This model including age, CD4 cell count, diabetes, proteinuria, and a loss in glomerular function less than 90 mL/min per 1.73 m2 were related to the incident CKD and predicted the development of CKD[66]. In addition, Scherzer et al[67] developed a point-based score to discriminate an HIV patient’s risk of CKD over 5 years. Figure 2 shows a screening algorithm of the detection and practical management for patients infected with HIV.
Cystatin C is an index for early glomerular dysfunction and may be a potential marker of chronic inflammation. Accordingly, cystatin C is something more than a marker of renal function. In fact, its elevation portends the incidence of heart and vessel diseases and all-cause mortality in the older people[68]. Moreover, it may be associated with a high likelihood of developing cancers[69,70]. However, serum cystatin C concentration are sometimes affected by non-renal factors including age, sex, race, and others[71]. The serum cystatin C level among HIV-infected patients could be greater in those with HIV infection than those without[72], as the serum cystatin C concentration is influenced by prevalent inflammatory diseases and the HIV viral replication[73]. Validation would be needed to confirm the utility of serum cystatin C level for assessing kidney function in HIV individuals.
A careful examination of the medical history and cumulative ART exposure is important for the past and further investigation of HIV individuals with CKD. The cART has beneficial effects on HIV-related diseases, such as HIVAN and HIVIC, but has adverse effects due to the long-term cumulative exposure. In addition to the metabolic changes of glucose and lipids induced by ART, some antiretroviral drugs may directly affect kidney function. Therefore, the detection of patients at high risk of CKD by the periodic measurements of ACR, PCR, and tubular biomarkers is most crucial with special reference to renal protection.
Further examination includes the follow-up of glomerular function, the test of urinary sediments, the ultrasonography of kidneys, and the pathological assessment of biopsied kidney tissues. Renal biopsy study is required for differentiating HIVAN from other glomerular nephtitis including diabetic nephropathy and HCV-related glomerulonephropathies, however, the risk of biopsy-related complications should be fully considered.
Adverse effects of cART on kidney are likely based on the overdosing of medications[74], and thus drug dosages have to be correctly altered according to eGFR. The major treatments for CKD may involve the strict control of high blood pressure, serum sugar and lipids. ART initiation in those having HIVAN is advocated, being independent on the control of CD4+ cell count and HIV infection[75,76]. Prednisolone and ACE inhibitors could be useful for caring HIVAN[77,78].
The periodic examination of proteinuria or albuminuria combined with eGFR, serum cystatin C, and markers for renal tubular damage may enable the early detection of CKD in HIV-infected subjects.
We thank all doctors in the Department of Infectious Diseases in Komagome General Hospital for their invaluable help with writing this review.
P- Reviewer: Bellomo G, Bhimma R, Kusztal M, Tanaka H S- Editor: Tian YL L- Editor: A E- Editor: Yan JL
| 1. | Lohse N, Hansen AB, Pedersen G, Kronborg G, Gerstoft J, Sørensen HT, Vaeth M, Obel N. Survival of persons with and without HIV infection in Denmark, 1995-2005. Ann Intern Med. 2007;146:87-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 558] [Cited by in RCA: 565] [Article Influence: 31.4] [Reference Citation Analysis (0)] |
| 2. | Mocroft A, Ledergerber B, Katlama C, Kirk O, Reiss P, d’Arminio Monforte A, Knysz B, Dietrich M, Phillips AN, Lundgren JD. Decline in the AIDS and death rates in the EuroSIDA study: an observational study. Lancet. 2003;362:22-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 935] [Cited by in RCA: 920] [Article Influence: 41.8] [Reference Citation Analysis (0)] |
| 3. | Lucas GM, Ross MJ, Stock PG, Shlipak MG, Wyatt CM, Gupta SK, Atta MG, Wools-Kaloustian KK, Pham PA, Bruggeman LA. Clinical practice guideline for the management of chronic kidney disease in patients infected with HIV: 2014 update by the HIV Medicine Association of the Infectious Diseases Society of America. Clin Infect Dis. 2014;59:e96-e138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 214] [Cited by in RCA: 218] [Article Influence: 19.8] [Reference Citation Analysis (0)] |
| 4. | Eggers PW, Kimmel PL. Is there an epidemic of HIV Infection in the US ESRD program? J Am Soc Nephrol. 2004;15:2477-2485. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 5. | Schwartz EJ, Szczech LA, Ross MJ, Klotman ME, Winston JA, Klotman PE. Highly active antiretroviral therapy and the epidemic of HIV+ end-stage renal disease. J Am Soc Nephrol. 2005;16:2412-2420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 135] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 6. | Lucas GM, Mehta SH, Atta MG, Kirk GD, Galai N, Vlahov D, Moore RD. End-stage renal disease and chronic kidney disease in a cohort of African-American HIV-infected and at-risk HIV-seronegative participants followed between 1988 and 2004. AIDS. 2007;21:2435-2443. [PubMed] |
| 7. | Gardner LI, Holmberg SD, Williamson JM, Szczech LA, Carpenter CC, Rompalo AM, Schuman P, Klein RS. Development of proteinuria or elevated serum creatinine and mortality in HIV-infected women. J Acquir Immune Defic Syndr. 2003;32:203-209. [PubMed] |
| 8. | Palella FJ, Baker RK, Moorman AC, Chmiel JS, Wood KC, Brooks JT, Holmberg SD. Mortality in the highly active antiretroviral therapy era: changing causes of death and disease in the HIV outpatient study. J Acquir Immune Defic Syndr. 2006;43:27-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1002] [Cited by in RCA: 1080] [Article Influence: 56.8] [Reference Citation Analysis (0)] |
| 9. | Ryom L, Kirk O, Lundgren JD, Reiss P, Pedersen C, De Wit S, Buzunova S, Gasiorowski J, Gatell JM, Mocroft A. Advanced chronic kidney disease, end-stage renal disease and renal death among HIV-positive individuals in Europe. HIV Med. 2013;14:503-508. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 32] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 10. | Cheung CY, Wong KM, Lee MP, Liu YL, Kwok H, Chung R, Chau KF, Li CK, Li CS. Prevalence of chronic kidney disease in Chinese HIV-infected patients. Nephrol Dial Transplant. 2007;22:3186-3190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 60] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 11. | Yanagisawa N, Ando M, Ajisawa A, Imamura A, Suganuma A, Tsuchiya K, Nitta K. Clinical characteristics of kidney disease in Japanese HIV-infected patients. Nephron Clin Pract. 2011;118:c285-c291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 34] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 12. | Mocroft A, Kirk O, Gatell J, Reiss P, Gargalianos P, Zilmer K, Beniowski M, Viard JP, Staszewski S, Lundgren JD. Chronic renal failure among HIV-1-infected patients. AIDS. 2007;21:1119-1127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 162] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 13. | Fernando SK, Finkelstein FO, Moore BA, Weissman S. Prevalence of chronic kidney disease in an urban HIV infected population. Am J Med Sci. 2008;335:89-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 79] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 14. | Taal MW, Brenner BM. Predicting initiation and progression of chronic kidney disease: Developing renal risk scores. Kidney Int. 2006;70:1694-1705. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 183] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 15. | Yamagata K, Iseki K, Nitta K, Imai H, Iino Y, Matsuo S, Makino H, Hishida A. Chronic kidney disease perspectives in Japan and the importance of urinalysis screening. Clin Exp Nephrol. 2008;12:1-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 103] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 16. | Ripley E. Complementary effects of angiotensin-converting enzyme inhibitors and angiotensin receptor blockers in slowing the progression of chronic kidney disease. Am Heart J. 2009;157:S7-S16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 17. | Gansevoort RT, Bakker SJ, de Jong PE. Early detection of progressive chronic kidney disease: is it feasible? J Am Soc Nephrol. 2006;17:1218-1220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Chen N, Hsu CC, Yamagata K, Langham R. Challenging chronic kidney disease: experience from chronic kidney disease prevention programs in Shanghai, Japan, Taiwan and Australia. Nephrology (Carlton). 2010;15 Suppl 2:31-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 38] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 19. | Peralta CA, Shlipak MG, Judd S, Cushman M, McClellan W, Zakai NA, Safford MM, Zhang X, Muntner P, Warnock D. Detection of chronic kidney disease with creatinine, cystatin C, and urine albumin-to-creatinine ratio and association with progression to end-stage renal disease and mortality. JAMA. 2011;305:1545-1552. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 317] [Cited by in RCA: 340] [Article Influence: 24.3] [Reference Citation Analysis (0)] |
| 20. | Levey AS, de Jong PE, Coresh J, El Nahas M, Astor BC, Matsushita K, Gansevoort RT, Kasiske BL, Eckardt KU. The definition, classification, and prognosis of chronic kidney disease: a KDIGO Controversies Conference report. Kidney Int. 2011;80:17-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1369] [Cited by in RCA: 1612] [Article Influence: 115.1] [Reference Citation Analysis (0)] |
| 21. | Levin A, Stevens PE. Summary of KDIGO 2012 CKD Guideline: behind the scenes, need for guidance, and a framework for moving forward. Kidney Int. 2014;85:49-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 394] [Cited by in RCA: 571] [Article Influence: 47.6] [Reference Citation Analysis (0)] |
| 22. | Szczech LA, Hoover DR, Feldman JG, Cohen MH, Gange SJ, Goozé L, Rubin NR, Young MA, Cai X, Shi Q. Association between renal disease and outcomes among HIV-infected women receiving or not receiving antiretroviral therapy. Clin Infect Dis. 2004;39:1199-1206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 136] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 23. | Szczech LA, Gange SJ, van der Horst C, Bartlett JA, Young M, Cohen MH, Anastos K, Klassen PS, Svetkey LP. Predictors of proteinuria and renal failure among women with HIV infection. Kidney Int. 2002;61:195-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 158] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 24. | Gupta SK, Mamlin BW, Johnson CS, Dollins MD, Topf JM, Dubé MP. Prevalence of proteinuria and the development of chronic kidney disease in HIV-infected patients. Clin Nephrol. 2004;61:1-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 76] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 25. | Fulop T, Olivier J, Meador RS, Hall J, Islam N, Mena L, Henderson H, Schmidt DW. Screening for chronic kidney disease in the ambulatory HIV population. Clin Nephrol. 2010;73:190-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 26. | Wyatt CM, Winston JA, Malvestutto CD, Fishbein DA, Barash I, Cohen AJ, Klotman ME, Klotman PE. Chronic kidney disease in HIV infection: an urban epidemic. AIDS. 2007;21:2101-2103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 124] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 27. | Wyatt CM, Hoover DR, Shi Q, Seaberg E, Wei C, Tien PC, Karim R, Lazar J, Young MA, Cohen MH. Microalbuminuria is associated with all-cause and AIDS mortality in women with HIV infection. J Acquir Immune Defic Syndr. 2010;55:73-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 61] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 28. | Choi AI, Li Y, Deeks SG, Grunfeld C, Volberding PA, Shlipak MG. Association between kidney function and albuminuria with cardiovascular events in HIV-infected persons. Circulation. 2010;121:651-658. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 141] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 29. | Gravemann S, Brinkkoetter PT, Vehreschild JJ, Franke B, Ehren K, Bünemann E, Orbach H, Weiß V, Hellmich M, Benzing T. Low-grade proteinuria is highly prevalent in HIV-positive patients on antiretroviral treatment. AIDS. 2014;28:1783-1789. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 30. | Yanagisawa N, Muramatsu T, Yamamoto Y, Tsuchiya K, Nitta K, Ajisawa A, Fukutake K, Ando M. Classification of human immunodeficiency virus-infected patients with chronic kidney disease using a combination of proteinuria and estimated glomerular filtration rate. Clin Exp Nephrol. 2014;18:600-605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 31. | Ross MJ, Klotman PE. Recent progress in HIV-associated nephropathy. J Am Soc Nephrol. 2002;13:2997-3004. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 100] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 32. | Han TM, Naicker S, Ramdial PK, Assounga AG. A cross-sectional study of HIV-seropositive patients with varying degrees of proteinuria in South Africa. Kidney Int. 2006;69:2243-2250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 152] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 33. | Post FA, Campbell LJ, Hamzah L, Collins L, Jones R, Siwani R, Johnson L, Fisher M, Holt SG, Bhagani S. Predictors of renal outcome in HIV-associated nephropathy. Clin Infect Dis. 2008;46:1282-1289. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 59] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 34. | Freedman BI, Soucie JM, Stone SM, Pegram S. Familial clustering of end-stage renal disease in blacks with HIV-associated nephropathy. Am J Kidney Dis. 1999;34:254-258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 109] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 35. | Szczech LA, Gupta SK, Habash R, Guasch A, Kalayjian R, Appel R, Fields TA, Svetkey LP, Flanagan KH, Klotman PE. The clinical epidemiology and course of the spectrum of renal diseases associated with HIV infection. Kidney Int. 2004;66:1145-1152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 241] [Cited by in RCA: 247] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 36. | Ryom L, Mocroft A, Kirk O, Ross M, Reiss P, Fux CA, Morlat P, Moranne O, Smith C, El-Sadr W. Predictors of advanced chronic kidney disease and end-stage renal disease in HIV-positive persons. AIDS. 2014;28:187-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 56] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 37. | Vallet-Pichard A, Pol S. Natural history and predictors of severity of chronic hepatitis C virus (HCV) and human immunodeficiency virus (HIV) co-infection. J Hepatol. 2006;44:S28-S34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 57] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 38. | Liangpunsakul S, Chalasani N. Relationship between hepatitis C and microalbuminuria: results from the NHANES III. Kidney Int. 2005;67:285-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 68] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 39. | Tsui JI, Vittinghoff E, Shlipak MG, O’Hare AM. Relationship between hepatitis C and chronic kidney disease: results from the Third National Health and Nutrition Examination Survey. J Am Soc Nephrol. 2006;17:1168-1174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 84] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 40. | Daugas E, Rougier JP, Hill G. HAART-related nephropathies in HIV-infected patients. Kidney Int. 2005;67:393-403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 76] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 41. | Kumar N, Perazella MA. Differentiating HIV-associated nephropathy from antiretroviral drug-induced nephropathy: a clinical challenge. Curr HIV/AIDS Rep. 2014;11:202-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 42. | Brewster UC, Perazella MA. Acute interstitial nephritis associated with atazanavir, a new protease inhibitor. Am J Kidney Dis. 2004;44:e81-e84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 43. | Izzedine H, M’rad MB, Bardier A, Daudon M, Salmon D. Atazanavir crystal nephropathy. AIDS. 2007;21:2357-2358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 51] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 44. | Viglietti D, Verine J, De Castro N, Scemla A, Daudon M, Glotz D, Pillebout E. Chronic interstitial nephritis in an HIV type-1-infected patient receiving ritonavir-boosted atazanavir. Antivir Ther. 2011;16:119-121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 23] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 45. | Kanzaki G, Tsuboi N, Miyazaki Y, Yokoo T, Utsunomiya Y, Hosoya T. Diffuse tubulointerstitial nephritis accompanied by renal crystal formation in an HIV-infected patient undergoing highly active antiretroviral therapy. Intern Med. 2012;51:1543-1548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 46. | Schmid S, Opravil M, Moddel M, Huber M, Pfammatter R, Keusch G, Ambuhl P, Wuthrich RP, Moch H, Varga Z. Acute interstitial nephritis of HIV-positive patients under atazanavir and tenofovir therapy in a retrospective analysis of kidney biopsies. Virchows Arch. 2007;450:665-670. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 41] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 47. | Izzedine H, Harris M, Perazella MA. The nephrotoxic effects of HAART. Nat Rev Nephrol. 2009;5:563-573. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 99] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 48. | Izzedine H, Hulot JS, Vittecoq D, Gallant JE, Staszewski S, Launay-Vacher V, Cheng A, Deray G. Long-term renal safety of tenofovir disoproxil fumarate in antiretroviral-naive HIV-1-infected patients. Data from a double-blind randomized active-controlled multicentre study. Nephrol Dial Transplant. 2005;20:743-746. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 138] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 49. | Gallant JE, Parish MA, Keruly JC, Moore RD. Changes in renal function associated with tenofovir disoproxil fumarate treatment, compared with nucleoside reverse-transcriptase inhibitor treatment. Clin Infect Dis. 2005;40:1194-1198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 223] [Cited by in RCA: 217] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 50. | Gallant JE, Moore RD. Renal function with use of a tenofovir-containing initial antiretroviral regimen. AIDS. 2009;23:1971-1975. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 102] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 51. | Zimmermann AE, Pizzoferrato T, Bedford J, Morris A, Hoffman R, Braden G. Tenofovir-associated acute and chronic kidney disease: a case of multiple drug interactions. Clin Infect Dis. 2006;42:283-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 227] [Cited by in RCA: 234] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 52. | Cooper RD, Wiebe N, Smith N, Keiser P, Naicker S, Tonelli M. Systematic review and meta-analysis: renal safety of tenofovir disoproxil fumarate in HIV-infected patients. Clin Infect Dis. 2010;51:496-505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 435] [Cited by in RCA: 412] [Article Influence: 27.5] [Reference Citation Analysis (0)] |
| 53. | Siedner MJ, Atta MG, Lucas GM, Perazella MA, Fine DM. Poor validity of urine dipstick as a screening tool for proteinuria in HIV-positive patients. J Acquir Immune Defic Syndr. 2008;47:261-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 20] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 54. | Levey AS, Coresh J, Balk E, Kausz AT, Levin A, Steffes MW, Hogg RJ, Perrone RD, Lau J, Eknoyan G. National Kidney Foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Ann Intern Med. 2003;139:137-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3156] [Cited by in RCA: 3212] [Article Influence: 146.0] [Reference Citation Analysis (0)] |
| 55. | Ando M, Yanagisawa N, Ajisawa A, Tsuchiya K, Nitta K. Urinary albumin excretion within the normal range is an independent risk for near-term development of kidney disease in HIV-infected patients. Nephrol Dial Transplant. 2011;26:3923-3929. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 56. | Kabanda A, Vandercam B, Bernard A, Lauwerys R, van Ypersele de Strihou C. Low molecular weight proteinuria in human immunodeficiency virus-infected patients. Am J Kidney Dis. 1996;27:803-808. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 49] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 57. | Gatanaga H, Tachikawa N, Kikuchi Y, Teruya K, Genka I, Honda M, Tanuma J, Yazaki H, Ueda A, Kimura S. Urinary beta2-microglobulin as a possible sensitive marker for renal injury caused by tenofovir disoproxil fumarate. AIDS Res Hum Retroviruses. 2006;22:744-748. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 74] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 58. | Kinai E, Hanabusa H. Progressive renal tubular dysfunction associated with long-term use of tenofovir DF. AIDS Res Hum Retroviruses. 2009;25:387-394. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 65] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 59. | Labarga P, Barreiro P, Martin-Carbonero L, Rodriguez-Novoa S, Solera C, Medrano J, Rivas P, Albalater M, Blanco F, Moreno V. Kidney tubular abnormalities in the absence of impaired glomerular function in HIV patients treated with tenofovir. AIDS. 2009;23:689-696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 221] [Cited by in RCA: 225] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 60. | Hall AM, Edwards SG, Lapsley M, Connolly JO, Chetty K, O’Farrell S, Unwin RJ, Williams IG. Subclinical tubular injury in HIV-infected individuals on antiretroviral therapy: a cross-sectional analysis. Am J Kidney Dis. 2009;54:1034-1042. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 65] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 61. | Jaafar A, Séronie-Vivien S, Malard L, Massip P, Chatelut E, Tack I. Urinary cystatin C can improve the renal safety follow-up of tenofovir-treated patients. AIDS. 2009;23:257-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 62. | Paragas N, Nickolas TL, Wyatt C, Forster CS, Sise M, Morgello S, Jagla B, Buchen C, Stella P, Sanna-Cherchi S. Urinary NGAL marks cystic disease in HIV-associated nephropathy. J Am Soc Nephrol. 2009;20:1687-1692. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 41] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 63. | Ando M, Yanagisawa N, Ajisawa A, Tsuchiya K, Nitta K. Kidney tubular damage in the absence of glomerular defects in HIV-infected patients on highly active antiretroviral therapy. Nephrol Dial Transplant. 2011;26:3224-3229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 34] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 64. | Shlipak MG, Scherzer R, Abraham A, Tien PC, Grunfeld C, Peralta CA, Devarajan P, Bennett M, Butch AW, Anastos K. Urinary markers of kidney injury and kidney function decline in HIV-infected women. J Acquir Immune Defic Syndr. 2012;61:565-573. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 49] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 65. | Peralta C, Scherzer R, Grunfeld C, Abraham A, Tien P, Devarajan P, Bennett M, Butch A, Anastos K, Cohen M. Urinary biomarkers of kidney injury are associated with all-cause mortality in the Women’s Interagency HIV Study (WIHS). HIV Med. 2014;15:291-300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 43] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 66. | Ando M, Yanagisawa N, Ajisawa A, Tsuchiya K, Nitta K. A simple model for predicting incidence of chronic kidney disease in HIV-infected patients. Clin Exp Nephrol. 2011;15:242-247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 67. | Scherzer R, Gandhi M, Estrella MM, Tien PC, Deeks SG, Grunfeld C, Peralta CA, Shlipak MG. A chronic kidney disease risk score to determine tenofovir safety in a prospective cohort of HIV-positive male veterans. AIDS. 2014;28:1289-1295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 35] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 68. | Shlipak MG, Wassel Fyr CL, Chertow GM, Harris TB, Kritchevsky SB, Tylavsky FA, Satterfield S, Cummings SR, Newman AB, Fried LF. Cystatin C and mortality risk in the elderly: the health, aging, and body composition study. J Am Soc Nephrol. 2006;17:254-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 163] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 69. | Yanagisawa N, Ando M, Tsuchiya K, Nitta K. HIV-infected men with elevated level of serum cystatin C have a high likelihood of developing cancers. J Antivir Antiretrovir. 2012;4:38-42. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 70. | Yanagisawa N, Ando M, Tsuchiya K, Nitta K. Impact of cystatin C elevation and albuminuria on probability of adverse outcomes in HIV-infected men receiving HAART. Clin Nephrol. 2013;79:362-369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 71. | Köttgen A, Selvin E, Stevens LA, Levey AS, Van Lente F, Coresh J. Serum cystatin C in the United States: the Third National Health and Nutrition Examination Survey (NHANES III). Am J Kidney Dis. 2008;51:385-394. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 119] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 72. | Odden MC, Scherzer R, Bacchetti P, Szczech LA, Sidney S, Grunfeld C, Shlipak MG. Cystatin C level as a marker of kidney function in human immunodeficiency virus infection: the FRAM study. Arch Intern Med. 2007;167:2213-2219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 105] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 73. | Knight EL, Verhave JC, Spiegelman D, Hillege HL, de Zeeuw D, Curhan GC, de Jong PE. Factors influencing serum cystatin C levels other than renal function and the impact on renal function measurement. Kidney Int. 2004;65:1416-1421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 673] [Cited by in RCA: 707] [Article Influence: 33.7] [Reference Citation Analysis (0)] |
| 74. | Choi AI, Rodriguez RA, Bacchetti P, Volberding PA, Havlir D, Bertenthal D, Bostrom A, O’Hare AM. Low rates of antiretroviral therapy among HIV-infected patients with chronic kidney disease. Clin Infect Dis. 2007;45:1633-1639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 43] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 75. | Lucas GM, Eustace JA, Sozio S, Mentari EK, Appiah KA, Moore RD. Highly active antiretroviral therapy and the incidence of HIV-1-associated nephropathy: a 12-year cohort study. AIDS. 2004;18:541-546. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 197] [Cited by in RCA: 195] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 76. | Hammer SM, Eron JJ, Reiss P, Schooley RT, Thompson MA, Walmsley S, Cahn P, Fischl MA, Gatell JM, Hirsch MS. Antiretroviral treatment of adult HIV infection: 2008 recommendations of the International AIDS Society-USA panel. JAMA. 2008;300:555-570. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 714] [Cited by in RCA: 708] [Article Influence: 41.6] [Reference Citation Analysis (0)] |
| 77. | Hammer SM, Eron JJ, Reiss P, Schooley RT, Thompson MA, Walmsley S, Cahn P, Fischl MA, Gatell JM, Hirsch MS. Antiretroviral treatment of adult HIV infection: 2008 recommendations of the International AIDS Society-USA panel. JAMA. 2008;300:555-570. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 714] [Cited by in RCA: 708] [Article Influence: 41.6] [Reference Citation Analysis (0)] |
| 78. | Wei A, Burns GC, Williams BA, Mohammed NB, Visintainer P, Sivak SL. Long-term renal survival in HIV-associated nephropathy with angiotensin-converting enzyme inhibition. Kidney Int. 2003;64:1462-1471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 70] [Article Influence: 3.2] [Reference Citation Analysis (0)] |