Published online Aug 19, 2025. doi: 10.5498/wjp.v15.i8.106092
Revised: April 12, 2025
Accepted: June 17, 2025
Published online: August 19, 2025
Processing time: 174 Days and 4.3 Hours
Sleep deprivation is a common problem in society, and bedtime procrastination (BtP) has become a significant cause of poor sleep among healthy individuals across various countries.
To study BtP, sleep behavior, and subjective well-being in the Indian population.
This was a cross-sectional study. The recruited participants were evaluated using the BtP Scale, World Health Organzation-5 Well-Being index, Patient Health Ques
A total of 401 participants were recruited for the study. Symptoms of anxiety were higher in the female participants compared to males. Among females, there was a significant positive correlation between BtP score with symptoms of anxiety (r = 0.23) and depression (r = 0.15) and a negative correlation with subjective well
BtP worsens anxiety, depression, sleep quality, and subjective well-being. It needs to be targeted for the promotion and prevention of mental health.
Core Tip: Bedtime procrastination (BtP) has a significant positive correlation with anxiety and depression, irrespective of sex. About 40% of people use electronic gadgets excessively (more than 6 hours daily). Females using electronic gadgets have significantly higher levels of anxiety than males. BtP negatively affects well-being and sleep quality in males.
- Citation: Parasher G, Gupta S, Kar SK. Interplay among bedtime procrastination, sleep patterns, and subjective wellbeing in the Indian population: An observational study. World J Psychiatry 2025; 15(8): 106092
- URL: https://www.wjgnet.com/2220-3206/full/v15/i8/106092.htm
- DOI: https://dx.doi.org/10.5498/wjp.v15.i8.106092
The Centre for Disease Control classifies sleep deprivation as a public health epidemic associated with the development of a variety of diseases[1]. The American Academy of Sleep Medicine and Sleep Research Society developed a consensus recommending a minimum of 7 hours of sleep per night for adults, otherwise associated with adverse health outcomes like metabolic disturbances, mental health disorders, and increased risk of death[2].
While the effects of good sleep are well known, incidences of poor sleep have increased in a post-pandemic era, with significant effects on the functionality of a person. An online survey reported that 61% of the 41000 respondents from India slept for less than 6 hours of uninterrupted sleep in the past year[3]. A survey done by Gupta et al[4]. after the coronavirus disease 2019 Lockdown in the Indian population, on a sample size of 958, observed a significant change in sleep habits compared to the pre-lockdown, regarding later bedtime, delayed sleep, and increased daytime napping. Reduced sleep and an increased incidence of depressive symptoms were observed across different occupational groups[4]. Dunn et al[5] reported poor sleep quality, prolonged latency, and excessive daytime sleepiness in the later years of college due to academic requirements among university students in India. Chronic sleep deprivation significantly affects memory span, decision-making, executive function, planning, social cognition, and verbal learning[6].
The term “Revenge Bedtime Procrastination” has gained fame post-pandemic on various social media platforms, glorifying it as a cause of sleep deprivation in healthy individuals. Zhang et al[7], in a study in 2020, evaluated the effects of smartphone addiction and BtP on the sleep quality of university students. They found a positive relationship between BtP and poor sleep quality. Similar studies have been conducted on the Indian population to show the detrimental effects of smartphone dependency on general health profile[8], sleep quality[9,10], cyberchondriac behavior, health anxiety and subjective well-being[11].
Kroese et al[12] first introduced this phenomenon called Bedtime Procrastination (BtP), defining it as “failing to go to bed at the intended time, while no external circumstances prevent a person from doing so”. BtP is widespread among young people[12,13]. Furthermore, studies were conducted to understand its prevalence and association with sleep quality, depression, and anxiety[10,14-17]. A meta-analysis by Hill et al[18] on BtP reported that BtP was moderately negatively associated with sleep duration [z = -0.31; 95% confidence interval (CI): -0.37 to -0.24] and sleep quality (z = -0.35; 95%CI: -0.42 to -0.27), and moderately positively associated with daytime fatigue (z = 0.32; 95%CI: 0.25 to 0.38)[18]. A study on students reported that higher general procrastination and higher BtP among students is associated with higher sleep insufficiency and daytime fatigue[19], which seems to impair the general well-being of the individuals. A study from Pakistan reported that BtP significantly worsens sleep disturbance and produces fatigue and mental health problems in students[20]. Similarly, another study on students reported that studyholics experience higher insomnia and BtP[21]. An Indian study reported that smartphone addiction and BtP often lead to dissatisfaction in life, significantly affecting overall well-being[22].
To the best of our knowledge, only one study has been conducted in India by Shukla et al[23] to determine the prevalence of BtP among Indian university students. Despite the absence of published research exploring the causes and impacts of BtP, we hypothesize that this phenomenon is widespread within the general Indian population. It contributes to diminished subjective sleep quality, adversely affects mental health, and compromises subjective well-being. Our study assessed the prevalence of BtP among individuals in India. Additionally, we examined the association of BtP with sleep quality, psychological health, and overall well-being.
The study was a web-based cross-sectional study conducted under the Department of Psychiatry of a tertiary centre in Lucknow. A self-reporting questionnaire was created using Google Forms. Convenience sampling was used to collect data. To reach a broader audience, unrestricted by location and occupation, we conducted an online survey and made it accessible on various social media platforms. The questionnaire was circulated to all the contacts in the university, including students, professors, and workers, using the email ID database available on the university portal. Further, the questionnaire was made available to a larger population by circulating the questionnaire link on social media networking sites like WhatsApp, Twitter, Facebook, Instagram, and Telegram. Duplication of respondents was eliminated as only a single response was admissible for one email ID.
Participants residing in India and between 18 and 60 years of age were included in the study. The exclusion criteria included patients reporting diagnosed psychiatric disorders (except personality disorders), sleeping disorders, or respiratory illnesses like asthma, chronic obstructive pulmonary disease. The sample size for this study was found to be 385, considering the expected prevalence of 50% and a 95%CI with a 5% margin of error in an infinite population using the iface sample size estimation software (https://sampsize.sourceforge.net/iface/). The study was conducted following the Declaration of Helsinki and approved by the Institutional Ethics Committee of King George's Medical University, Lucknow, Uttar Pradesh, India, with Ethical approval reference code: 128th ECM IIA/P3 with Letter No. 26/Ethics/2024 dated 02-04-2024.
We created a Google Form with multiple parts. The first part included personal details like email ID, age, sex, residence, highest completed level of education, comorbidities, and recreational drug use practices. The tools used in the study were validated in the Indian population and were used in previous studies.
BtP scale: A nine-item questionnaire developed by Kroese et al[24], with a five-point Likert scale. It consists of five negative and four positive statements. Each item can score from 1 (almost never) to 5 (almost always), while items 2, 3, 7, and 9 are reverse-coded. Hence, the range of total scores is 9-45, with more significant scores indicating a higher frequency of engaging in BtP.
World Health Organization-5 Wellbeing Index: This is a simple tool for screening general well-being. It consists of a five-item questionnaire with five statements answered on a Likert scale[25].
Patient Health Questionnaire-2: This is a two-item scale used to inquire about the frequency of depressed mood and anhedonia. Its score ranges from 0 to 6. A score of 3 or more is indicative of likely depression[26].
Generalized Anxiety Disorder 2-item: This consists of two questions the subject must answer for the initial screening of generalized anxiety disorder. The score ranges from 0 to 6, and 3 is the preferred cut-off[27].
Munich Chronotype Questionnaire: This self-reporting questionnaire tests typical sleep behavior over the past four weeks for work and work-free days separately[28].
Single-item Sleep Quality Scale: It is a self-rated, global sleep quality assessment tool. The questionnaire requires the respondent to rate the overall quality of sleep over a 7-day recall period on a discretizing visual analogue scale, whereby the respondent marks an integer score from 0 to 10, according to the following five categories: 0 = terrible, 1-3 = poor, 4-6 = fair, 7-9 = good, and 10 = excellent[29].
The data obtained from Google Forms were tabulated in Excel sheets, and the prevalence of BtP was determined and compared for different subgroups. The data were checked for their distribution patterns. As the data were normally distributed, we applied a parametric test to analyze the data.
The sociodemographic and clinical characteristics are presented in percentages and proportions. Our study analyzed categorical variables using Pearson's χ2 test and continuous variables using the t-test. Pearson's correlational analysis evaluated the association of BtP with other outcome variables. P < 0.05 was considered statistically significant. We performed Statistical analysis using the Statistical Package for Social Sciences (version 24.0; IBM Corp., Armonk, NY, United States).
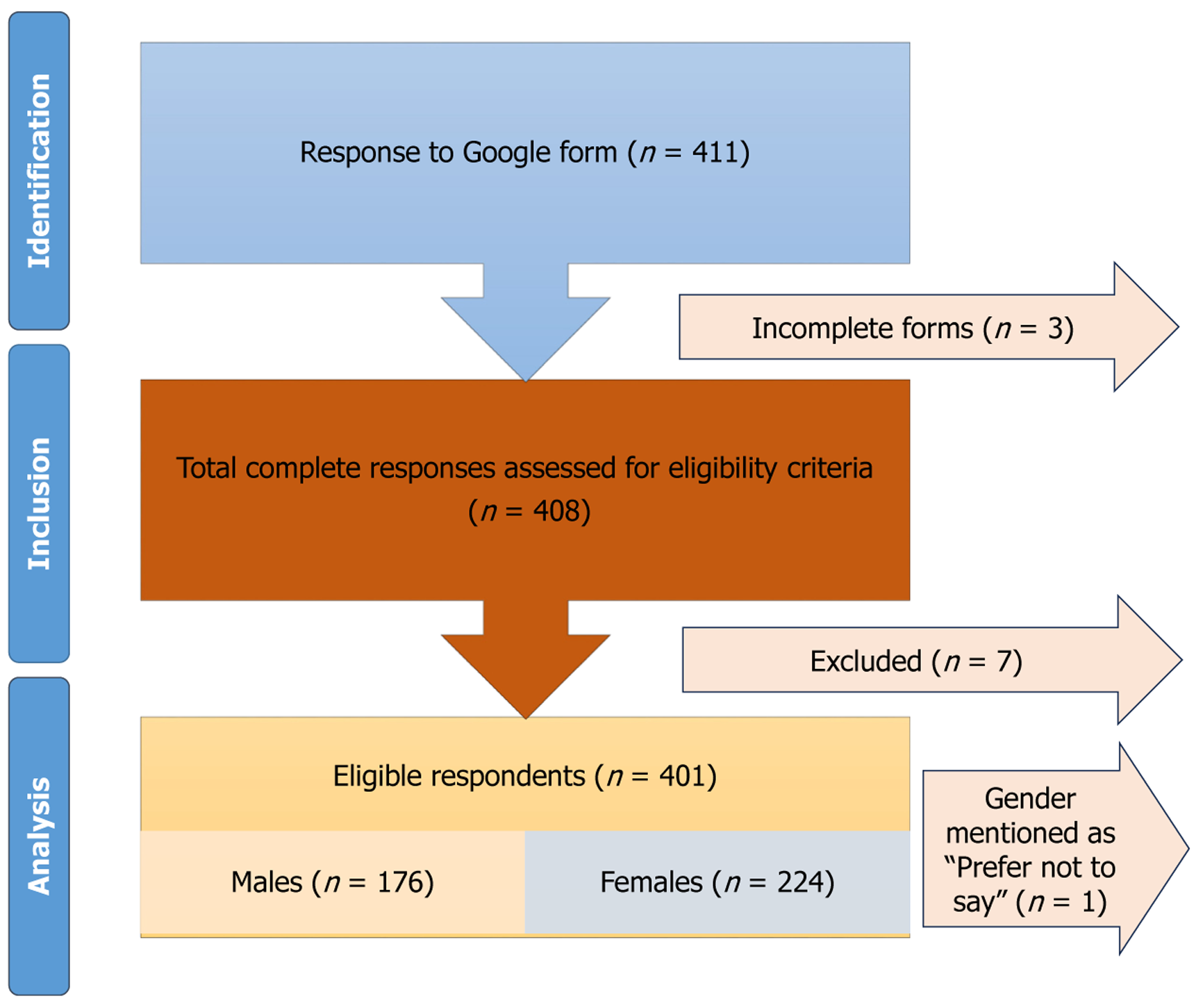
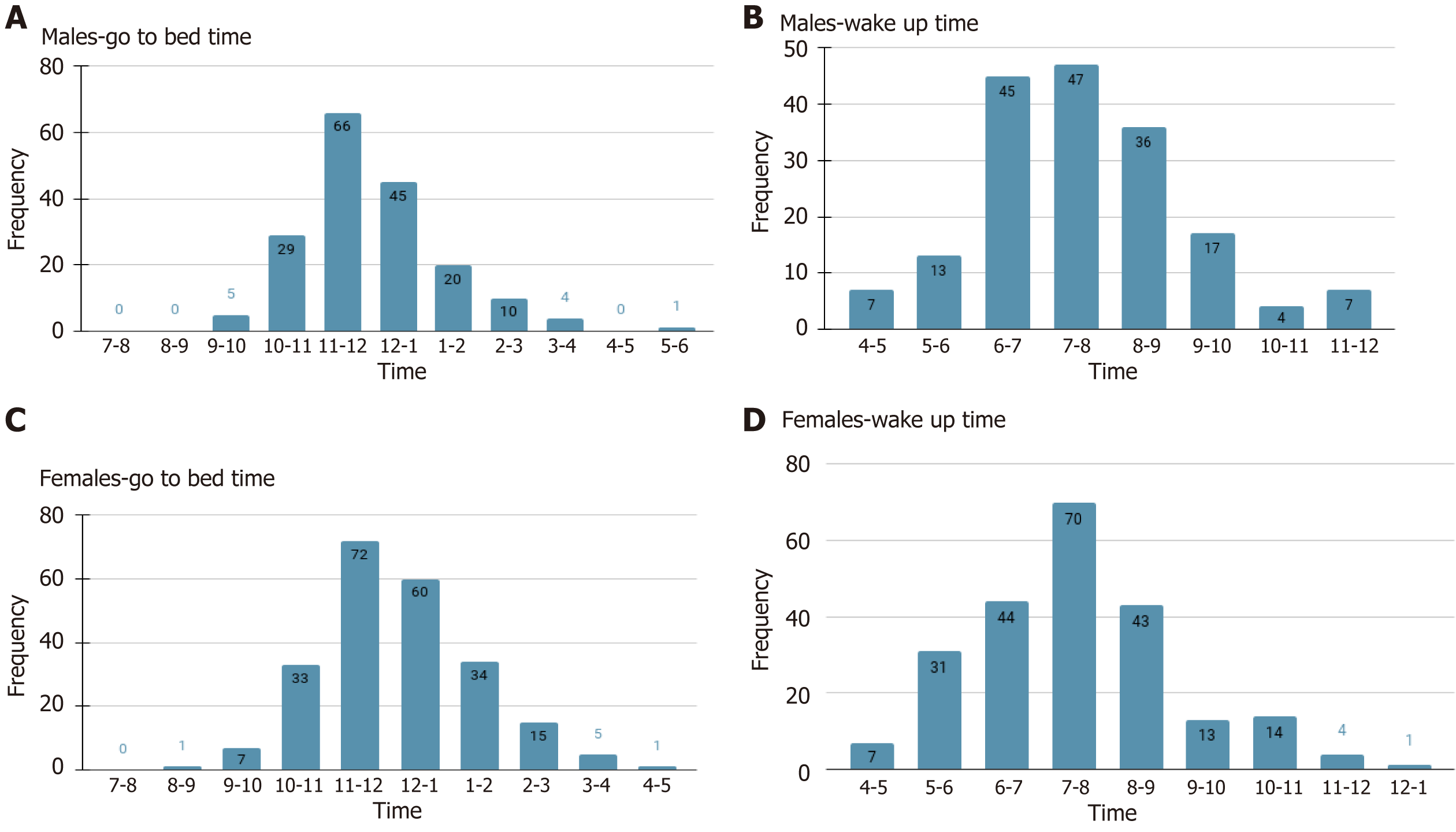
The total number of participants in the study was 401, of whom 176 were males and 224 were females (Figure 1). The general characteristics of the dataset are given in Table 1. The result shows that 2.8% of men went to sleep between 9 PM and 10 PM, 52% between 10 PM and 12 PM, 25% between 12 AM and 1 AM, and a few after 1 AM (18%). Among women, 3% sleep before 10 PM, 45% between 10 PM and 12 PM, 26% between 12 AM and 1 AM, and about 23% go to sleep after 1 AM. About 51% of males woke up between 6 AM and 8 AM, 20% between 8 AM and 9 AM, and about 30% woke up after 9 AM. Among women, 50% woke up between 6 AM and 8 AM, 19% between 8 AM and 9 AM, and only 12% woke up after 9 AM (Figure 2). More than 40% of the participants use their electronic gadgets for more than 6 hours per day on average, and professional work is the single most common reason for using them (Table 2).
| Domain | n (%) |
| Age group, years | |
| < 25 | 191 (47.63) |
| 25-50 | 196 (48.87) |
| > 50 | 14 (3.49) |
| Sex | |
| Male | 176 (43.89) |
| Female | 224 (55.86) |
| Prefer not to say | 1 (0.25) |
| Occupation | |
| Students pursuing a professional course | 150 (37.4) |
| Salaried jobs | 143 (35.6) |
| Students of the general stream | 40 (9.9) |
| Self-employed | 30 (7.48) |
| Unemployed | 15 (3.74) |
| Housewife | 8 (1.99) |
| Others | 15 (3.74) |
| Religion | |
| Hindu | 361 (90) |
| Muslim | 20 (4.98) |
| Sikh | 4 (0.99) |
| Others | 16 (3.99) |
| Domicile | |
| Urban | 322 (80.29) |
| Semi-urban | 51 (12.71) |
| Rural | 28 (6.98) |
| Question asked | Total responses | Male | Female |
| Do you have a personal electronic gadget? | 401 | 176 | 224 |
| How many hours in a day do you spend on electronic gadgets? | |||
| Less than 2 hours | 21 (5.2) | 9 | 12 |
| 2-4 hours | 85 (21.2) | 39 | 46 |
| 4-6 hours | 134 (33.4) | 55 | 79 |
| 6-8 hours | 96 (23.9) | 46 | 50 |
| More than 8 hours | 65 (16.2) | 27 | 37 |
| The single major reason for using an electronic gadget | |||
| Official/professional work | 123 (30.6) | 71 | 52 |
| Study | 114 (28.4) | 39 | 75 |
| Social media | 82 (20.4) | 32 | 50 |
| Entertainment | 76 (18.9) | 32 | 44 |
| Study and entertainment | 1 (0.2) | 0 | 1 |
| Both official and entertainment | 2 (0.49) | 1 | 1 |
| Finding job | 1 (0.2) | 0 | 1 |
| All of the above | 2 (0.49) | 2 | 0 |
Symptoms of anxiety were significantly higher in the female group (2.19 ± 1.5) compared to the male group (1.5 ± 1.38) (t [398] = 4.4; P < 0.05). Subjective well-being was slightly higher in males (54.7 ± 20.02) than in females (52.03 ± 20.0)
| Variables | Females (n = 224), mean ± SD | Males (n = 176), mean ± SD | Test of significance | Effect size (Cohen’s d); 95%CI |
| GAD-2 | 2.191 ± 1.545 | 1.534 ± 1.389 | t = 4.412, df = 398, P = 0.0001 | 0.444 (0.245 to 0.644) |
| PHQ-2 | 1.987 ± 1.531 | 1.721 ± 1.384 | t = 1.799, df = 398, P = 0.0728 | 0.181 (-0.017 to 0.379) |
| WHO-5 | 52.035 ± 20.003 | 54.704 ± 20.022 | t = 1.983, df = 398, P = 0.048 | -0.133 (-0.331 to 0.064) |
| GAD-2 | χ2 = 9.409 | Risk ratio = 1.71 | ||
| Screen positive1 | 74 (33.03) | 34 (19.32) | P = 0.002 | Risk difference = 0.137 |
| Screen negative | 150 (66.97) | 142 (80.68) | ||
| PHQ-2 | χ2 = 0.862 | Risk ratio = 1.162 | ||
| Screen positive1 | 68 (30.36) | 46 (26.14) | P = 0.353 | Risk difference = 0.042 |
| Screen negative | 156 (69.64) | 130 (73.86) |
Among males, there was a significant negative correlation between the age of participants with BtP score (r = -0.3) and anxiety (r = -0.19). Sleep latency had a significant negative correlation with subjective well-being (r = -0.24) and sleep quality (r = -0.24), and a positive correlation with procrastination time (r = 0.4). Sleep duration had a significant negative correlation with procrastination time (r = -0.27). A significant positive correlation was reported between procrastination time and BtP score (r = 0.2), depression (r = 0.27), and anxiety (r = 0.29), whereas a negative correlation was reported with subjective well-being (r = -0.19) and sleep quality (r = -0.3). BtP score had a significant positive correlation with depression (r = 0.18) and anxiety (r = 0.35), whereas a negative correlation was seen with sleep quality (r = -0.25; Table 4).
| Variables | Age of the participants | Sleep latency in minutes | Hours of sleep | Procrastination time (minutes) | BtP score | PHQ-2 score | GAD-2 score | WHO-5 score |
| Sleep latency in minutes | R = -0.0056 | - | - | - | - | - | - | - |
| P = 0.937 | ||||||||
| Hours of sleep | R = -0.0941 | R = -0.044 | - | - | - | - | - | - |
| P = 0.215 | P = 0.562 | |||||||
| Procrastination time (minutes) | R = -0.0822 | R = 0.4034 | R = -0.276 | - | - | - | - | - |
| P = 0.279 | P < 0.00001c | P = 0.0002c | ||||||
| BtP score | R = -0.396 | R = 0.0242 | R = -0.0614 | R = 0.2003 | - | - | - | - |
| P < 0.00001c | P = 0.750 | P = 0.421 | P = 0.0076b | |||||
| PHQ-2 score | R = -0.192 | R = 0.1203 | R = -0.0586 | R = 0.2708 | R = 0.1891 | - | - | - |
| P = 0.011a | P = 0.1117 | P = 0.444 | P = 0.0003c | P = 0.0119a | ||||
| GAD-2 score | R = -0.1098 | R = 0.1011 | R = -0.1297 | R = 0.2961 | R = 0.3561 | R = 0.5769 | - | - |
| P = 0.146 | P = 0.181 | P = 0.088 | P = 0.00007c | P < 0.00001c | P < 0.00001c | |||
| WHO-5 score | R = 0.1021 | R = - 0.246 | R = 0.0469 | R = -0.1948 | R = -0.1471 | R = -0.3933 | R = -0.2971 | - |
| P = 0.177 | P = 0.0009c | P = 0.536 | P = 0.0095b | P = 0.0515 | P < 0.00001c | P = 0.00006c | ||
| SISS (sleep quality) | R = 0.0505 | R = -0.2487 | R = 0.1403 | R = -0.3029 | R = -0.2555 | R = -0.2362 | R = -0.2811 | R = 0.418 |
| P = 0.506 | P = 0.0009c | P = 0.063 | P = 0.00004c | P = 0.0006c | P = 0.0016b | P = 0.00016c | P < 0.00001c |
A significant negative correlation was found between the ages of the female participants and BtP score (r = -0.15), depressive symptoms (r = -0.16), anxiety symptoms (r = -0.15), and sleep quality (r = -0.13). Sleep latency had a significant negative correlation with duration of sleep (r = -0.15), subjective well-being (r = -0.14), and sleep quality (r = -0.13) and a significant positive correlation with procrastination time (r = 0.17). Sleep duration had a significant negative correlation with BtP score (r = -0.18) and a significant positive correlation with sleep quality (r = 0.32). A significant positive correlation was found between procrastination time and BtP score (r = 0.15) and anxiety (r = 0.19). BtP score had a significant positive correlation with depression (r = 0.15) and anxiety (r = 0.23), whereas a negative correlation was seen with subjective wellbeing (r = -0.23) and sleep quality (r = -0.24). Anxiety and depression had a significant negative correlation with sleep quality and subjective wellbeing (Table 5).
| Variables | Age of the participants | Sleep latency in minutes | Hours of sleep | Procrastination time (minutes) | BtP score | PHQ-2 score | GAD-2 score | WHO-5 score |
| Sleep latency in minutes | R = -0.0881 | - | - | - | - | - | - | - |
| P = 0.189 | ||||||||
| Hours of sleep | R = -0.1091 | R = -0.1573 | - | - | - | - | - | - |
| P = 0.104 | P = 0.0187a | |||||||
| Procrastination time (minutes) | R = 0.0244 | R = 0.1732 | R = -0.1257 | - | - | - | - | - |
| P = 0.716 | P = 0.0094b | P = 0.0597 | ||||||
| BtP score | R = -0.1518 | R = 0.1042 | R = -0.1812 | R = 0.1541 | - | - | - | - |
| P = 0.0229a | P = 0.1199 | P = 0.0066b | P = 0.0210a | |||||
| PHQ-2 score | R = -0.1671 | R = 0.0839 | R = 0.016 | R = 0.1128 | R = 0.1578 | - | - | - |
| P = 0.0123a | P = 0.211 | P = 0.8117 | P = 0.0921 | P = 0.0181a | ||||
| GAD-2 score | R = -0.1593 | R = 0.054 | R = -0.0522 | R = 0.1904 | R = 0.2303 | R = 0.6355 | - | - |
| P = 0.0172a | P = 0.4212 | P = 0.4387 | P = 0.0042 | P = 0.0005c | P < 0.00001c | |||
| WHO-5 score | R = 0.038 | R = -0.1486 | R = 0.0581 | R = -0.0769 | R = -0.2326 | R = -0.6183 | R = -0.4855 | - |
| P = 0.572 | P = 0.0257a | P = 0.3868 | P = 0.2511 | P = 0.0004c | P < 0.00001c | P < 0.00001c | ||
| SISS | R = -0.1335 | R = -0.1347 | R = 0.3271 | R = -0.1253 | R = -0.2419 | R = -0.2163 | R = -0.3065 | R = 0.3785 |
| P = 0.045a | P = 0.0435a | P < 0.00001c | P = 0.0618 | P = 0.0003c | P = 0.0011b | P < 0.00001c | P < 0.00001c |
This demographic analysis revealed a predominance of participants aged 18 to 50, primarily from urban areas, and a slight female majority. In males, there was a decrease in BtP scores and depressive symptoms with increasing age. A similar trend was noted in the female group, in addition to a decrease in GAD-2 score and an overall improvement in perceived sleep quality with age.
BtP is widespread among young people[12,13]. The age-related trends observed in our male and female cohorts suggest that older adults may adopt healthier sleep practices, possibly due to increased awareness of the consequences of poor sleep or shifts in lifestyle priorities. This might also be because young adults, mostly university students or in their early careers, have compromised sleep due to academic burdens or career progression. A cross-sectional study intending to detect excessive daytime sleepiness among college students found that students taking professional courses and science streams seem more at risk[30].
In our study, there was no significant difference between the sexes in reporting perceived poor sleep quality using the single-item Sleep Quality Scale. However, females had fewer hours of sleep. A study conducted by Shad et al[31] in college students of medical and non-medical backgrounds found that sleep quality did not significantly differ by sex.
Various studies have had different findings in this arena. Two studies reported that females had significantly better sleep times and quality than males[32,33]. A study by Kaur[34] found that sleep quality was worse among female undergraduate non-medical students.
Our analysis revealed increased screening rates for anxiety and depression and decreased perceived sleep quality and overall well-being score with increasing BtP score. Two studies found an independent association between depression and BtP, where the severity of depression increased with increasing BtP, eventually contributing to depression[15,16].
Furthermore, studies have shown that anxiety has a positive effect on BtP[14], which is expected since people with high anxiety levels also have high avoidance behavior and may regulate negative emotions through BtP[35]. A study done by Li et al[36] reported that higher procrastination scores were associated with higher risks of insomnia symptoms.
While for students, the leading cause of procrastination was studying, professionals procrastinated mainly for leisure or work completion. Other responses included stress, surrounding atmosphere, irregular schedule, and children. In a qualitative study by Nauts et al[37], individuals with BtP reported that when they were tired and stressed at the end of the day, they opted to delay their bedtime and engage in different activities despite knowing its negative impact on their sleep. They distinguished between deliberate procrastination, mindless procrastination, and strategic delay.
Magalhães et al[38] further distinguished between BtP and while-in-bed procrastination. Their study reported that 59.5% of participants engaged in while-in-bed procrastination, while the rest procrastinated before bed. From the data collected by the short Munich Chronotype Questionnaire tool, we calculated BtP and while-in-bed procrastination among the participants. BtP could only be calculated among participants with different workdays and weekends. While in-bed procrastination seems highly prevalent among the participants, with 117 males and females reporting more than 15 minutes of procrastination while in bed. The individuals with more procrastination time had higher BtP scores and fewer hours of sleep and perceived sleep quality as poor. They also had higher scores for anxiety and depression and low scores for perceived general well-being. More procrastination time was related to increased sleep latency.
Alarm dependency was seen in 71.75% (287) of participants. 50% of participants took over 5 minutes to get out of bed after waking up. 32% of participants had a delayed sleep schedule on weekends only.
Our data mainly comprised students pursuing professional courses (37.4%) and salaried persons (35.6%). A longitudinal study done to find a correlation between work settings and sleep revealed that persons without children had longer and better sleep when doing work from home (WFH) than those in work from office (WFO)[39]. Also, WFH persons had higher well-being compared to WFO. Although in our study, participants with WFH mentioned children as a cause of delay in going to bed, but had equal risk of high BtP scores, poor sleep, and low well-being scores.
All participants had personal electronic gadgets; 40% spent more than 6 hours on gadgets; 30.6% used electronic devices mainly for professional work, 28.4% for studies, 20.4% for social media usage, and 18.9% mainly for enter
Sleep latency had a significant negative correlation with sleep duration, subjective well-being, sleep quality and a significant positive correlation with procrastination time. The time taken to fall asleep is an important indicator of distress. The longer time takes to fall asleep, more is the distress and the poorer the quality of sleep. These distressing sleep latency prolongation and BtP are expected to adversely affect the subjective well-being.
The prevalence of BtP was evident in the respondents, although fewer participants preferred leisure to make up for work or studies. More procrastination time leads to altered sleep quality by affecting sleep latency, which affects individuals' mental and overall well-being. No other risk factor was identified in the study that predisposed the individuals to BtP or poor sleep quality.
Our study included an array of healthy individuals belonging to different sectors of the profession and of different ages. As the existing studies are limited to specific groups of populations (students, professionals, females, adolescents) of different backgrounds, and BtP is studied with reference to different variables (sleep quality, quality of life, subjective well-being, smartphone use, subjective satisfaction), the findings are grossly heterogeneous.
We tried to address problems related to BtP, as there is a lack of such data from the Indian population. Since most of our sample came from a professional background, we cannot generalize our findings to a larger population subset. Also, we worked with a limited sample size. Since it was a cross-sectional study, we cannot conclude our study regarding an individual's BtP and cognitive dysfunction.
This study had several limitations. One major limitation was the small sample size. The study design was cross-sectional in nature, which fails to establish causality. The participants were mostly between 18 and 50 years old, and the inclusion criteria were up to the age of 60; hence, the findings cannot be generalized to older adults. Due to the limitations of the sampling technique (convenient sampling and web-based survey), there is unequal representation of all socio
Our study covered multiple aspects of sleep, including perceived quantity, quality, and latency, its associated effect on mental and physical well-being, and the reason behind its insufficiency. Revenge BtP can be identified as one cause. People's awareness of its detrimental effects might affect their nighttime habits and help them in self-management.
We conclude that there is a positive correlation between increased BtP score and depression and anxiety, and a negative correlation with the feeling of subjective well-being. BtP score was associated with poor sleep quality and higher sleep latency. Previous literature suggests similar detrimental effects of electronic gadgets and work pressure affecting sleep quality, but only a handful come from the Indian subcontinent. We also noted that BtP and poor sleep quality were higher in the younger age group than in older people. Moreover, we found that many people attributed their BtP to professional rather than leisure activities. BtP has become a rising problem in our society, and more work is required to address it and spread awareness among society.
| 1. | Ramos AR, Wheaton AG, Johnson DA. Sleep Deprivation, Sleep Disorders, and Chronic Disease. Prev Chronic Dis. 2023;20:E77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 26] [Reference Citation Analysis (0)] |
| 2. | Watson NF, Badr MS, Belenky G, Bliwise DL, Buxton OM, Buysse D, Dinges DF, Gangwisch J, Grandner MA, Kushida C, Malhotra RK, Martin JL, Patel SR, Quan SF, Tasali E. Recommended Amount of Sleep for a Healthy Adult: A Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep. 2015;38:843-844. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 221] [Cited by in RCA: 632] [Article Influence: 63.2] [Reference Citation Analysis (0)] |
| 3. | LocalCircles. 61% Indians are getting less than 6 hours of uninterrupted sleep. 2025. [cited 12 January 2025]. Available from: https://www.localcircles.com/a//press/page/world-sleep-day-survey. |
| 4. | Gupta R, Grover S, Basu A, Krishnan V, Tripathi A, Subramanyam A, Nischal A, Hussain A, Mehra A, Ambekar A, Saha G, Mishra KK, Bathla M, Jagiwala M, Manjunatha N, Nebhinani N, Gaur N, Kumar N, Dalal PK, Kumar P, Midha PK, Daga R, Tikka SK, Praharaj SK, Goyal SK, Kanchan S, Sarkar S, Das S, Sarkhel S, Padhy SK, Sahoo S, Satyanarayana Rao TS, Dubey V, Menon V, Chhabra V, Lahan V, Avasthi A. Changes in sleep pattern and sleep quality during COVID-19 lockdown. Indian J Psychiatry. 2020;62:370-378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 201] [Article Influence: 40.2] [Reference Citation Analysis (0)] |
| 5. | Dunn C, Goodman O, Szklo-Coxe M. Sleep duration, sleep quality, excessive daytime sleepiness, and chronotype in university students in India: A systematic review. J Health Soc Sci. 2022;7:36-52. [DOI] [Full Text] |
| 6. | Ramrakhiyani VC, Deshmukh SV. Study of the Incidence and Impact of Chronic Sleep Deprivation in Indian Population with Special Emphasis on Neuropsychology Testing. Indian J Sleep Med. 2019;14:23-28. [DOI] [Full Text] |
| 7. | Zhang MX, Wu AMS. Effects of smartphone addiction on sleep quality among Chinese university students: The mediating role of self-regulation and bedtime procrastination. Addict Behav. 2020;111:106552. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 121] [Article Influence: 24.2] [Reference Citation Analysis (0)] |
| 8. | Mishra S, Kar SK, Shankar A. Internet addiction and health profile among medical, dental and nursing graduates of India. Minerva Psychiatry. 2023;64:290-295. [RCA] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 9. | Chatterjee S, Kar SK. Smartphone Addiction and Quality of Sleep among Indian Medical Students. Psychiatry. 2021;84:182-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 28] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 10. | Haque S, Singh S, Narayan J, Tripathi A, Ahmad M, Kumar T, Verma S. Effect of smartphone use on sleep and mental health status of Indian medical students: a cross-sectional study. Int J Res Med Sci. 2024;12:3737-3746. [DOI] [Full Text] |
| 11. | Agrawal V, Khulbe Y, Singh A, Kar SK. The digital health dilemma: Exploring cyberchondria, well-being, and smartphone addiction in medical and non-medical undergraduates. Indian J Psychiatry. 2024;66:256-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 12. | Kroese FM, Evers C, Adriaanse MA, de Ridder DTD. Bedtime procrastination: A self-regulation perspective on sleep insufficiency in the general population. J Health Psychol. 2016;21:853-862. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 139] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 13. | Kadzikowska-Wrzosek R. Insufficient Sleep among Adolescents: The Role of Bedtime Procrastination, Chronotype and Autonomous vs. Controlled Motivational Regulations. Curr Psychol. 2020;39:1031-1040. [RCA] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 38] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 14. | Campbell RL, Bridges AJ. Bedtime procrastination mediates the relation between anxiety and sleep problems. J Clin Psychol. 2023;79:803-817. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 15. | Guo J, Meng D, Ma X, Zhu L, Yang L, Mu L. The impact of bedtime procrastination on depression symptoms in Chinese medical students. Sleep Breath. 2020;24:1247-1255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 32] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 16. | Hou X, Hu J. Depression and bedtime procrastination: Chain mediation of brooding and perceived stress. Heliyon. 2023;9:e22672. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 17. | Ma X, Meng D, Zhu L, Xu H, Guo J, Yang L, Yu L, Fu Y, Mu L. Bedtime procrastination predicts the prevalence and severity of poor sleep quality of Chinese undergraduate students. J Am Coll Health. 2022;70:1104-1111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 36] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 18. | Hill VM, Rebar AL, Ferguson SA, Shriane AE, Vincent GE. Go to bed! A systematic review and meta-analysis of bedtime procrastination correlates and sleep outcomes. Sleep Med Rev. 2022;66:101697. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 36] [Reference Citation Analysis (0)] |
| 19. | Herzog-Krzywoszanska R, Krzywoszanski L, Kargul B. General procrastination and bedtime procrastination as serial mediators of the relationship between temporal perspective and sleep outcomes. Sci Rep. 2024;14:31175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 20. | Yasin N, Mushtaq R, Karamat A. Bedtime Procrastination, Sleep Disturbance, Fatigue and Mental Health in Female University Students: Mediation Analysis. J Prof Appl Psychol. 2024;5:215-223. [DOI] [Full Text] |
| 21. | Alshammari TK, Rogowska AM, Basharahil RF, Alomar SF, Alseraye SS, Al Juffali LA, Alrasheed NM, Alshammari MA. Examining bedtime procrastination, study engagement, and studyholism in undergraduate students, and their association with insomnia. Front Psychol. 2022;13:1111038. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 22. | Aiya S, Bhansali N. The Relationship between Mindfulness, Bedtime Procrastination, Smartphone Addiction and General Well Being in Emerging Adults. Int J Indian Psychol. 2023;11:2944-2955. |
| 23. | Shukla A, Andrade C. Prevalence of Bedtime Procrastination in University Students and Reexamination of the Bedtime Procrastination Scale. Prim Care Companion CNS Disord. 2023;25:22m03334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 24. | Kroese FM, De Ridder DT, Evers C, Adriaanse MA. Bedtime procrastination: introducing a new area of procrastination. Front Psychol. 2014;5:611. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 103] [Cited by in RCA: 166] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 25. | Topp CW, Østergaard SD, Søndergaard S, Bech P. The WHO-5 Well-Being Index: a systematic review of the literature. Psychother Psychosom. 2015;84:167-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1669] [Cited by in RCA: 2422] [Article Influence: 242.2] [Reference Citation Analysis (0)] |
| 26. | Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41:1284-1292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3238] [Cited by in RCA: 4302] [Article Influence: 195.5] [Reference Citation Analysis (0)] |
| 27. | Plummer F, Manea L, Trepel D, McMillan D. Screening for anxiety disorders with the GAD-7 and GAD-2: a systematic review and diagnostic metaanalysis. Gen Hosp Psychiatry. 2016;39:24-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1320] [Cited by in RCA: 1110] [Article Influence: 123.3] [Reference Citation Analysis (0)] |
| 28. | Jankowski KS. Composite Scale of Morningness: psychometric properties, validity with Munich ChronoType Questionnaire and age/sex differences in Poland. Eur Psychiatry. 2015;30:166-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 95] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 29. | Snyder E, Cai B, DeMuro C, Morrison MF, Ball W. A New Single-Item Sleep Quality Scale: Results of Psychometric Evaluation in Patients With Chronic Primary Insomnia and Depression. J Clin Sleep Med. 2018;14:1849-1857. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 231] [Article Influence: 33.0] [Reference Citation Analysis (0)] |
| 30. | Kaur G, Singh A. Excessive daytime sleepiness and its pattern among Indian college students. Sleep Med. 2017;29:23-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 32] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 31. | Shad R, Thawani R, Goel A. Burnout and Sleep Quality: A Cross-Sectional Questionnaire-Based Study of Medical and Non-Medical Students in India. Cureus. 2015;7:e361. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 32. | Giri P, Baviskar M, Phalke D. Study of sleep habits and sleep problems among medical students of pravara institute of medical sciences loni, Western maharashtra, India. Ann Med Health Sci Res. 2013;3:51-54. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 61] [Cited by in RCA: 80] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 33. | Manzar MD, Zannat W, Kaur M, Hussain ME. Sleep in university students across years of university education and gender influences. Int J Adolesc Med Health. 2015;27:341-348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 34. | Kaur G. A study on the sleep quality of Indian college students. JSM Brain Sci. 2018;3:1018. |
| 35. | Ball TM, Gunaydin LA. Measuring maladaptive avoidance: from animal models to clinical anxiety. Neuropsychopharmacology. 2022;47:978-986. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 35] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 36. | Li X, Buxton OM, Kim Y, Haneuse S, Kawachi I. Do procrastinators get worse sleep? Cross-sectional study of US adolescents and young adults. SSM Popul Health. 2020;10:100518. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 37. | Nauts S, Kamphorst BA, Stut W, De Ridder DTD, Anderson JH. The Explanations People Give for Going to Bed Late: A Qualitative Study of the Varieties of Bedtime Procrastination. Behav Sleep Med. 2019;17:753-762. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 56] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 38. | Magalhães P, Cruz V, Teixeira S, Fuentes S, Rosário P. An Exploratory Study on Sleep Procrastination: Bedtime vs. While-in-Bed Procrastination. Int J Environ Res Public Health. 2020;17:5892. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 39. | Massar SAA, Ong JL, Lau T, Ng BKL, Chan LF, Koek D, Cheong K, Chee MWL. Working-from-home persistently influences sleep and physical activity 2 years after the Covid-19 pandemic onset: a longitudinal sleep tracker and electronic diary-based study. Front Psychol. 2023;14:1145893. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |