Published online Oct 19, 2022. doi: 10.5498/wjp.v12.i10.1298
Peer-review started: March 19, 2022
First decision: May 30, 2022
Revised: June 15, 2022
Accepted: September 2, 2022
Article in press: September 2, 2022
Published online: October 19, 2022
Processing time: 212 Days and 4.4 Hours
Orthorexia nervosa (ON) is the persistent concern of maintaining the self-imposed diet to improve one's health. Many factors have been associated to ON in univ-ersity students.
To assess the prevalence of ON in Italian and Spanish university students in relation to eating attitude and psychological distress, and the possible overlaps between ON (evaluated with different scored questionnaires from the originally proposed ORTO-15), distress and risk of eating disorders.
This study was carried out on 160 students recruited at La Sapienza University of Rome and at the Catholic University of Murcia. Questionnaires were administered to evaluate ON (ORTO-15 and sub-scores), body concerns (Multidimensional Body-Self Relations Questionnaire, MBSRQ, and Body Uneasiness test, BUT), psychological distress (Kessler Psychological Distress Scale, K10), physical activity (International Physical Activity Questionnaire, IPAQ), eating attitude (Eating Attitudes Test, EAT-26) and malnutrition (Starvation Symptom Inventory, SSI). Sex differences, within the same country, and differences between Italian and Spanish students, within the same sex, were evaluated.
The ORTO-15 positive subjects, assessed with the originally proposed cut-off, were above 70% in both Italian and Spanish students, with a higher prevalence in the Spanish sample (Italian females 76.3%, Italian males 70.7%; Spanish females 97.0%, Spanish males 96.3%). According to ORTO-7, about 30% of Italian and 48% of Spanish students were positive to ON with no significant sex differences. When excluding students underweight (UW), overweight (OW) or obese (OB), as well as those potentially at risk of eating disorders or presenting mild, moderate and severe distress, in the resultant normal weight (NW)-K10neg-EAT-26neg subgroup, we did not find many correlations observed in the whole sample, including those between ORTO scores and BUT, SSI, Total MBSRQ and some of its components. Moreover, ORTO-7 resulted in the only ON score unrelated with Body Mass Index, MBSRQ components and IPAQ-assessed intense activity, in the NW-K10neg-EAT-26neg subgroup. After this sort of “exclusion diagnosis”, the prevalence of ON of these students on the overall sample resulted in 16.9%, 12.2%, 15.2% and 25.9% for Italian females, Italian males, Spanish females and Spanish males, respectively.
In some university students ON could be a symptom of other conditions related to body image concerns and distress, as well as to high physical activity and appearance, fitness, health or illness orientation (from MBSRQ). However, ORTO-7 became independent from these confounding variables, after the exclusion of UW, OW, OB and students positive to EAT-26 and K10, suggesting the possibility of identifying orthorexic subjects with this specific questionnaire.
Core Tip: This study explores the overlap of orthorexia nervosa with eating attitude and psychological distress in Italian and Spanish university students. After excluding, among normal weight students, those with high score on the Kessler Distress Scale and Eating Attitudes Test, we did not find correlations among orthorexia and Starvation Symptoms Inventory, Body Uneasiness Test, and Multidimensional Body Self-Relations Questionnaire (MBSRQ), observed in the whole sample. After this kind of “exclusion diagnosis”, sub-scores of MBSRQ indicating body concerns correlated with ORTO-12 and ORTO-9, whereas ORTO-7 resulted the only score unrelated with all outcomes, including fitness and health orientations (MBSRQ), and intense physical activity.
- Citation: Aiello P, Toti E, Villaño D, Raguzzini A, Peluso I. Overlap of orthorexia, eating attitude and psychological distress in some Italian and Spanish university students. World J Psychiatry 2022; 12(10): 1298-1312
- URL: https://www.wjgnet.com/2220-3206/full/v12/i10/1298.htm
- DOI: https://dx.doi.org/10.5498/wjp.v12.i10.1298
The term orthorexia nervosa (ON) is referred to the psychological obsession with a healthy, organic and pure diet, and it is often based on stereotyped or erroneous nutritional beliefs, which can lead to dietary restrictions with resulting nutritional deficiencies[1-4]. Although ON shares several aspects in common with Anorexia Nervosa (AN)[5] and other eating disorders (EDs)[6], and around 70% of health professionals[7,8] believe that ON should be a distinct, clinically recognized ED, it is not included in the ICD-11 (International Statistical Classification of Diseases and Related Health Problems)[9,10]. In the Diagnostic and Statistical Manual of Mental Disorders, the terminology “eating disorders” has been changed to “Feeding and Eating Disorders”, including eight categories: AN, bulimia nervosa, binge ED, pica, rumination, Avoidant or Restrictive Food Intake Disorder (ARFID), Other Specified Feeding and Eating Disorder (OSFED), and unspecified feeding and EDs[11]. Among these, ON has yet to be recognized as a separate ED, but has been included in OSFED, whereas ARFID refers to a persistent avoidance of food for various reasons (depressed temperament, phobias, sensory repulsion of the appearance, smell, texture of food), not necessarily associated with the search for a healthy diet that characterizes the subject with ON.
Although individuals with ON have an obsessive focus on healthy eating and may eliminate entire food groups, fearing they are unhealthy, they can later develop a typical ED[7,11]. Despite the awareness of clinicians on this condition[7,8,12], it is assumed that the estimate of subjects affected by ON is very complex, given the lack of explicit diagnostic criteria[13-16]. In particular, it has been recently pointed out that the conflicting data on the prevalence of ON depend on differences in the tools used and in the cut-off points[17]. Moreover, authors concluded that the use of the ORTO-15 questionnaire to diagnose ON is questionable due to a high percentage of false-positive results[17], and different cut-offs or sub-scores have been proposed[18-24]. Abdullah et al[18] have suggested that a cut-off point of 35 is preferable than a cut-off at 40, and have reported that ON tendency is affected by sex and body mass index (BMI), and not affected by educational level. No differences were found in the prevalence of ON among students attending health-scientific, economic-humanistic, sport sciences and dietetics and nutrition university courses[25,26]. However, the reported prevalence of ON in university students was variable and affected by EDs, dieting and a high level of physical activity (PA)[25-30].
Among the criticisms relative to ORTO-15, Roncero et al[31] highlighted the risk of including those who are on-diet among the individuals with ON, and the redundancy between the ORTO-15 and the Eating Attitudes Test (EAT-26). Accordingly, an overlap between ORTO-15 and EAT-26 has been reported in university students[32,33], but individuals with ON had lower psychological distress than those with ED risk[33]. Furthermore, it has been reported that overweight (OW) preoccupation and appearance orientation (AO), assessed with the Multidimensional Body-Self Relations Questionnaire-Appearance Scale (MBSRQ-AS), were significant predictors of ON[34].
The aim of this observational study was to evaluate the prevalence of ON in Italian and Spanish university students in relation to eating attitude and psychological distress, and the possible overlaps between ON (evaluated with different scored questionnaires), distress and risk of EDs. Moreover, a decision tree for the exclusion diagnosis of ON in healthy university students has been proposed.
This study was carried out on a sub-group of participants from a previous study[35]. Undergraduate and doctoral students aged between 18 years and 35 years were recruited at La Sapienza University of Rome and at the Catholic University of Murcia. All the volunteers included in the study signed the informed consent, accompanied by an informative note, and the recruiter assigned them an alphanumeric code to guarantee privacy during the data management (all details about recruitment and protocol are available online at https://www.clinicaltrials.gov/ct2/show/NCT04099420). Body mass and stature were measured with the OMRON BF511 electronic scale and the SECA 217 portable stadiometer, respectively. BMI was calculated with the following formula: BMI = weight (kg)/height squared (m2). Moreover, several standardized questionnaires were administered.
The ORTO-15 test is a questionnaire made up of 15 multiple-choice items based on a Likert scale (always, often, sometimes, never)[36]. The items concern three areas: the cognitive-rational area (items 1, 5, 6, 11, 12, 14), the clinical area (items 3, 7-9, 15), mainly related to anxiety-inducing and obsessive psychiatric disorders, and the emotional area (items 2, 4, 10, 13)[36]. A score of 1 was given to responses that were more indicative of ON, whereas a score of 4 was attributed to those that indicated a normal eating behavior. Therefore, lower scores correspond to a more pathological behavior, and total score ranges from 15 to 60, with the cut-off point equal to 40[36]. This value has been questioned as it was considered too high; consequently, a lower cut-off (35) was also chosen[18,19].
Additional versions of the ORTO test have been developed based on the selection of ORTO-15 items that more specifically could be indicative of the presence of symptoms of ON. ORTO-12 is a shorter version of 12 items, obtained by excluding items 5, 6 and 8 from the original ORTO-15, since they contribute less to the definition of ON, but a specific cut-off point was not determined[20]. ORTO-11 excludes items 5, 8, 14 and 15 of the ORTO-15. Final score ranges from 11 to 44, and a cut-off point < 25 has been considered the most appropriate to suggest a tendency to ON[21]. The ORTO-9 is a version of ORTO test which excludes items 1, 2 and 8, with a cut-off < 26.7. This test was found to be ineffective in predicting ON[22]. The ORTO-7 is based on items (1, 3, 4, 7, 9, 11 and 13) that mostly highlight the presence of ON with a cut-off ≤ 19[23,24].
Two questionnaires were used to evaluate body image concerns, the MBSRQ[37,38] and the Body Uneasiness Test (BUT).
We evaluated the total MBSRQ and the MBSRQ Factor Subscales (FSs): AO, fitness orientation (FO), health orientation (HOr) and illness orientation (IO). In addition to these FSs, we evaluated the MBSRQ subscales: body areas satisfaction scale (BASS) and OW preoccupation (OP). Each of the MBSRQ scales has its corresponding items that can be answered by a primary number from 1 (strongly disagree) to 5 (strongly agree). The score of contraindicative items (6, 15-17, 23, 25, 28, 32-34, 36-38, 40, 42, 43, 45, 47-49) is reversed (i.e., 1 = 5, 2 = 4, 4 = 2, 5 = 1). MBSRQ subscale scores are the means of the constituent items. The MBSRQ-AS is the shorter (34-item version) form of MBSRQ that assesses only the appearance-related components of the body image construct[37].
On the other hand, BUT includes two parts, BUT A (34 statements) and BUT B (37 body parts). Items are rated on a 6 points Likert-type scale (range 0-5, from “never” to “always”) and high rates indicate greater body uneasiness[39]. In addition to the total score, we evaluated BUT A weight phobia (WP, fear of being or becoming fat) and body image concerns (BIC, worries related to physical appearance) components.
Eating Attitudes Test (EAT-26) and Starvation Symptom Inventory (SSI) were administered to participants. The former is a standardized measure of symptoms and concerns characteristic of EDs, whereas the latter can reveal the presence of malnutrition.
EAT-26 is made up of 26 items and represent a screening tool to assess “ED risk”[40]. Although it does not provide a diagnosis of ED, the EAT-26 items include the subscales: “dieting” scale (items 1, 6, 7, 10, 11, 12, 14, 16, 17, 22, 23, 24, 26) and “bulimia and food preoccupation” scale (items 3, 4, 9, 18, 21, 25). Four behavioral questions are included to determine the presence of extreme weight-control behaviors. These items assess self-reported binge eating, self-induced vomiting, use of laxatives and treatment for ED over the preceding 6 mo. Participants were required to judge whether the item applied “always”, “very often”, “often”, “sometimes”, “rarely” or “never”. Each extreme response in the “anorexic” direction is scored as a worth of 3 points, while the adjacent alternatives are weighted as 2 points and 1 point, respectively. A score ≥ 20 on the EAT-26 does not necessarily mean that respondent has an ED. However, it indicates a high level of concern about dieting, body weight or problematic eating behaviors.
SSI is a 16-item questionnaire and participants were asked to estimate the number of days out of the preceding 28, in which they had experienced symptoms of starvation (hunger, poor concentration, heightened satiety, dizziness, reduction in rate of weight loss) on a 7-point Likert scale: never (0), 1-5 d (1), 6-12 d (2), 13-15 (3), 16-22 (4), 23-27 (5), and always (6)[41]. The highest score indicates increased frequency of starvation symptoms over the last 28 d.
The Kessler Psychological Distress Scale (K10)[42] and the International Physical Activity Questionnaire (IPAQ)[43] were used to evaluate distress and PA level, respectively.
K10 is a 10-item questionnaire about emotional states, each with a five-level response scale. The measure can be used as a brief screen to identify levels of distress[42]. Each item is scored from 1 (none of the time) to 5 (all of the time). Scores from the 10 items were then summed, yielding a minimum score of 10 and a maximum score of 50. According to the total score, the likelihood of having a mental disorder (psychological distress) is established[42]; in particular, 10-19 likely to be well, 20-24 likely to have a mild disorder, 25-29 likely to have a moderate disorder, and 30-50 likely to have a severe disorder.
The IPAQ (short form)[43] includes items assessing the frequency and duration of PA in three ranges of intensity: intense PA (8.0 metabolic equivalent of tasks: METs), moderate PA (4.0 METs), and walking fast (3.3 METs), moderate (3.0 METs) and slow (2.5 METs) pace[43]. Based on collected data about the frequency and duration of PA, energy expenditure (expressed as MET-min/wk) has been estimated. One MET is the rate of energy expenditure at rest, and it is approximately equal to 3.5 mL O2 kg-1 min-1 in adults. According to the Italian Society of Endocrinology, IPAQ allows to classify population in three PA levels: Low (the lowest level of PA, less than 700 METs-min/wk), Moderate (Total PA between 700 and 2519 METs-min/wk) and High (Total PA of at least 2520 METs- min/wk).
Categorical variables were expressed as percentages and significance assessed by the χ2 test. Continuous variables showing a normal pattern (normality test Shapiro-Wilk passed) were expressed as means with SD, otherwise data were expressed as median (25%-75% range). Results were analyzed by analysis of variance (ANOVA, Shapiro-Wilk test passed), or by Kruskal-Wallis one-way analysis of variance on ranks (Shapiro-Wilk test failed). The significance of the differences between females and males within the same country, and those between the different countries within the same sex, were evaluated using the Student-Newman-Keuls method (Shapiro-Wilk test passed) or the Dunn’s method (Shapiro-Wilk Test failed). Spearman correlation was performed between variables. The level of significance was set below 5% (P < 0.05).
Characteristics of students and differences between Italy and Spain (evaluated within the same sex), and sex differences (evaluated within the same country) are reported in Table 1. Only in Italy, females (IT-F) had a significant lower BMI than males (IT-M), whereas the different prevalence of underweight (UW), OW and obese (OB) students, as well as of volunteers who practice Low, Moderate or High PA, did not reach significance in both countries (Table 1). However, Spanish males (SP-M) on average practiced more PA than females (SP-F), and sex differences were found in IPAQ intense (MET-min/wk from intense activities) in both countries (Table 1). No differences were found in smoking habits, whereas a high percentage of SP-M reported mild psychological distress (assessed by K10) than IT-M (Table 1). SP-M were also those with higher total MBSRQ, MBSRQ-AO, -FO, -HOr, -AS and -BASS, whereas no differences were found in MBSRQ-IO and -OP (Table 2). On the contrary, IT-F had higher BUT-A - BIC and - WP than IT-M, but lower compared to SP-F (Table 2). Differences in total BUT and in its components (BUT-A and BUT-B) did not reach statistical significance (Table 2).
| IT-F, n = 59 | IT-M, n = 41 | SP-F, n = 33 | SP-M, n = 27 | |
| Age (yr) | 24 (23-28) | 25 (23-28) | 23 (21-28) | 24 (24-26) |
| Height (m) | 1.64 ± 0.06a | 1.78 ± 0.08a | 1.63 ± 0.06a | 1.78 ± 0.07a |
| Weight (kg) | 55.9 (53.0-61.0)a | 77.0 (70.9-87.5)a | 58.7 (52.4-66.5)a | 76.3 (67.1-82.0)a |
| BMI (kg/m2) | 20.7 (19.4-22.4)a | 24.5 (22.1-27.1)a | 23.3 (20.2-24.5) | 24.1 (21.8-25.5) |
| Underweight (%) | 11.9 | 0.0 | 9.1 | 3.7 |
| Overweight (%) | 6.8 | 31.7 | 15.1 | 25.9 |
| Obese (%) | 5.1 | 9.7 | 3.0 | 3.7 |
| IPAQ (MET-min/wk) | 2232 (1080-4986) | 4380 (2305-6277) | 2100 (1202-4395)a | 4970 (2575-6780)a |
| IPAQ walking | 630 (315-1260) | 700 (488-1323) | 525 (244-1230) | 600 (240-1470) |
| IPAQ moderate | 720 (160-1680) | 600 (240-1440) | 600 (240-1440) | 720 (120-1440) |
| IPAQ intense | 480 (0-1920)a | 2160 (400-3840)a | 800 (0-1680)a | 2400 (960-4320)a |
| PA low (%) | 16.9 | 7.3 | 18.2 | 7.4 |
| PA moderate (%) | 40.7 | 19.5 | 36.4 | 14.8 |
| PA high (%) | 42.4 | 73.2 | 45.5 | 77.8 |
| Smokers (%) | ||||
| Habitual | 15.3 | 19.5 | 9.1 | 7.7 |
| Occasional | 16.9 | 19.5 | 15.2 | 15.4 |
| Ex-smokers | 8.5 | 9.8 | 9.1 | 3.8 |
| K10 | 15.0 (13.0-19.0) | 14.0 (12.0-17.0) | 19.0 (15.0-27.5) | 17.0 (14.0-20.0) |
| Mild (%) | 11.9 | 0.0b | 15.2 | 25.9b |
| Moderate (%) | 6.9 | 9.8 | 18.2 | 3.7 |
| Severe (%) | 5.1 | 4.9 | 15.2 | 3.7 |
| IT-F, n = 59 | IT-M, n = 41 | SP-F, n = 33 | SP-M, n = 27 | |
| MBSRQ | 227.0 ± 21.7 | 231.6 ± 27.6b | 227.9 ± 24.3a | 249.3 ± 27.5a,b |
| MBSRQ-AO | 3.3 ± 0.9 | 3.2 ± 0.5b | 3.5 ± 0.5 | 3.5 ± 0.5b |
| MBSRQ-FO | 3.4 (3.0-3.9) | 3.5 (3.2-4.2) | 3.5 (3.0-4.0)a | 4.2 (3.6-4.4)a |
| MBSRQ-HOr | 3.4 ± 0.5 | 3.4 ± 0.6 | 3.2 ± 0.6a | 3.6 ± 0.6a |
| MBSRQ-IO | 3.3 ± 0.6 | 3.3 ± 0.5 | 3.4 ± 0.5 | 3.6 ± 0.6 |
| MBSRQ-AS | 3.1 ± 0.3 | 3.1 ± 0.4b | 3.1 ± 0.4a | 3.4 ± 0.4a,b |
| MBSRQ-BASS | 3.2 ± 0.7 | 3.4 ± 0.6 | 3.1 ± 0.8a | 3.5 ± 0.7a |
| MBSRQ-OP | 2.0 (1.8-2.8) | 2.5 (1.8-3.0) | 2.5 (2.1-3.0) | 2.5 (2.0-3.3) |
| BUT | 33.0 (19.0-61.0) | 16.0 (6.0-39.0) | 60.0 (30.5-82.0) | 35.0 (21.0-74.0) |
| BUT-A | 16.0 (9.0-36.0) | 10.0 (2.0-20.0) | 33.0 (12.5-51.0) | 18.0 (13.0-42.0) |
| BUT-A - WP | 0.9 (0.4-1.6)b | 0.5 (0.1-1.0) | 1.8 (0.8-2.6)b | 1.1 (0.6-1.8) |
| BUT-A - BIC | 0.7 (0.2-1.3)a | 0.2 (0.0-0.9)a | 0.9 (0.5-1.6) | 0.6 (0.2-1.6) |
| BUT-B | 15.0 (7.0-31.0) | 11.0 (3.5-21.0) | 25.5 (14.0-42.5) | 21.0 (8.0-36.0) |
Concerning ORTO-15, lower values (indicating high ON) were observed in Spanish students compared to Italians, when using the first proposed cut-off point of 40[36], and with ORTO-12, -11 and -9 (Table 3). By using the lower cut-off point of 35 for ORTO-15 or the ORTO-11, -9, and -7, IT-F resulted with less tracts of ON than SP-F (Table 3). Both SP-F and SP-M had higher EAT-26 total score than Italian counterparts, despite dieting and bulimia components did not reach statistical significance (Table 3). Similar results came from SSI, suggesting more starvation symptoms in Spaniards compared to Italians (Table 3).
| IT-F, n = 59 | IT-M, n = 41 | SP-F, n = 33 | SP-M, n = 27 | |
| ORTO-15 | 36.8 ± 3.4a | 36.4 ± 34.2a | 34.2 ± 3.6a | 33.8 ± 3.4a |
| Cut-off 40 (%) | 76.3a | 70.7a | 97.0a | 96.3a |
| Cut-off 35 (%) | 23.7a | 36.5 | 48.5a | 55.5 |
| ORTO-12 | 30.7 ± 3.0a | 30.4 ± 3.4a | 27.5 ± 2.9a | 27.2 ± 2.7a |
| ORTO-11 | 27.8 ± 2.8a | 27.6 ± 3.4a | 25.2 ± 2.9a | 25.4 ± 3.0a |
| Cut-off 25 (%) | 11.9a | 19.5a | 36.4a | 25.9a |
| ORTO-9 | 30.4 ± 3.4a | 30.0 ± 3.7a | 27.8 ± 3.2a | 27.1 ± 3.2a |
| Cut-off 26.7 (%) | 13.6a | 19.5a | 30.3a | 40.7a |
| ORTO-7 | 20.0 (18.0-22.0)a | 19.0 (18.0-21.0) | 19.0 (15.5-19.5)a | 19.0 (16.0-19.0) |
| Cut-off 19 (%) | 32.2 | 29.3 | 48.5 | 48.1 |
| EAT-26 | 6.0 (3.0-10.0)a | 5.0 (3.0-8.5)a | 11.0 (5.0-17.5)a | 13.0 (7.0-17.0)a |
| Cut-off 20 (%) | 8.5 | 4.9 | 21.2 | 11.1 |
| Dieting | 2.0 (0.0-5.0) | 2.0 (0.04.5) | 4.0 (0.5-9.5) | 6.0 (3.0-9.0) |
| Bulimia | 3.0 (3.0-3.0) | 3.0 (3.0-3.0) | 3.0 (3.0-5.5) | 3.0 (3.0-5.0) |
| SSI | 14.0 (8.0-22.0)a | 10.0 (4.5-16.0)a | 24.0 (20.0-43.0)a | 18.0 (12.0-30.0)a |
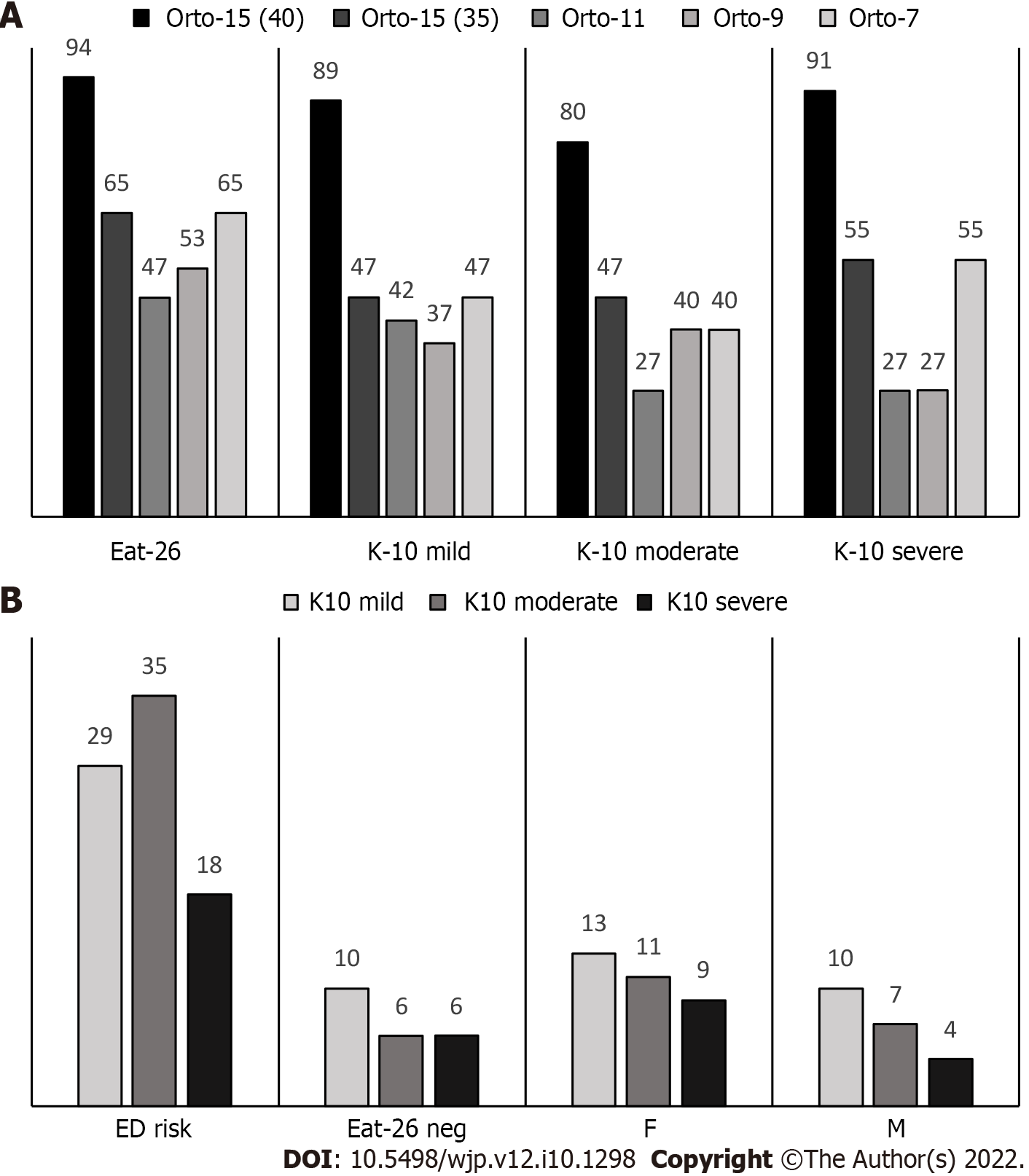
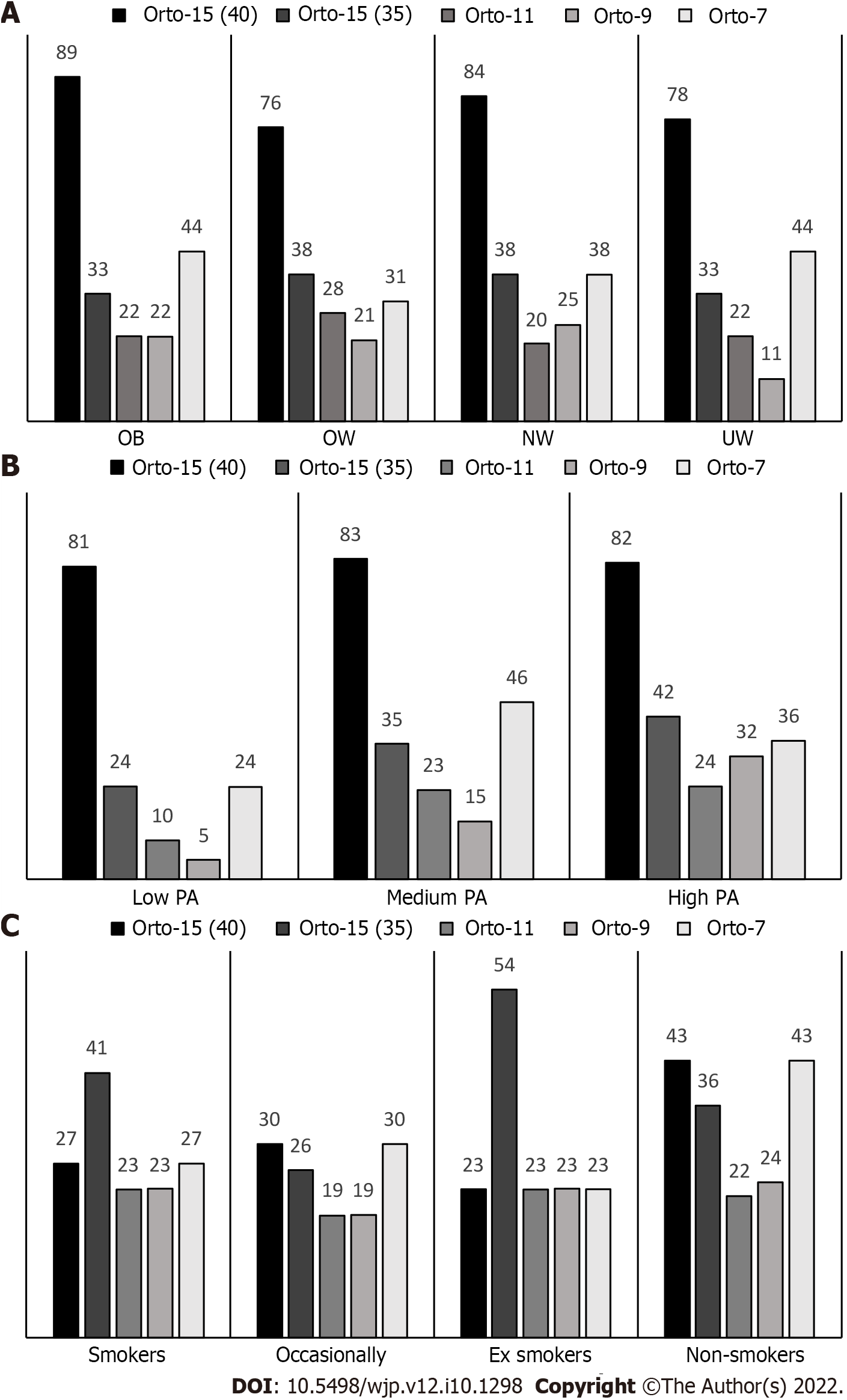
Figure 1A illustrates the prevalence of ON in the whole sample (n = 160), by using different cut-off points and scores for ORTO questionnaire, among students who presented ED risk (EAT-26) or mild, moderate, and severe psychological distress (K10). In addition to the overlaps among these conditions and ON, psychological distress was observed both in students presenting ED risk or in those resulting negative to the EAT-26 test, without sex differences (Figure 1B). On the other hand, in Figure 2 is presented the prevalence of ON among different BMI classes and lifestyle factors, such as PA level and smoking habits.
From the aforementioned results, and in order to reduce the potential confounder as being on caloric restriction[31], Spearman correlations were evaluated in both the total sample (n = 160, 92 F and 68 M) and a subgroup of students (n = 66, 38 F and 28 M) with normal weight (NW), excluding those who suffered from mild, moderate and severe distress, or potentially at ED risk (NW-K10neg-EAT-26neg).
As regards the NW-K10neg-EAT-26neg group, all subjects resulted with ON when ORTO-15 (40 cut-off point) was applied, whereas a prevalence of 37.9% was observed applying ORTO-15 (35 cut-off point), 18.2% considering ORTO-11, 22.7% with ORTO-9, and 40.0% with ORTO-7. Concerning lifestyle, the percentage of non-smokers (60.6%) was higher (P < 0.05) compared to those of ex-smokers (7.6%) and smokers (13.6%) among students with ON, assessed with ORTO-15 (40 cut-off). Similar results were reported when ORTO-15 (35 cut-off point) was used, with a prevalence of ON in non-smokers and smokers corresponding to 60.0% and 16.0%, respectively, as well as for results of ORTO-11 (prevalence of ON: non-smokers 66.7% and smokers 16.7%), ORTO-9 (prevalence of ON: non-smokers 66.7% and smokers 13.3%) and ORTO-7 (prevalence of ON: non-smokers 74.1% and smokers 7.4%). Among the students with ON, the percentage of those practicing high PA was higher (P < 0.05) compared to low PA for ORTO-15 (cut-off 40: high PA 54.4% and low PA 15.2%; cut-off 35: high PA 68.0% and low PA 8.0%), ORTO-11 (high PA 75.0% and low PA 0%), ORTO-9 (high PA 80.0% and low PA 0.0%) and ORTO-7 (high PA 59.3% and low PA 11.1%).
Considering the whole sample, among the different ORTO scores a relationship between ORTO-9 and BMI was found, and Table 4 depicts the Spearman correlations between ORTO scores and those from the other questionnaires. All ORTO scores were inversely correlated to SSI (Table 4), which indicates that high ON corresponds to more starvation symptoms since ORTO has reverse scores. Similarly, all ORTO scores were correlated to EAT-26 and its components (Table 4). On the contrary, the relationships between each ORTO score and BUT components were different (Table 4). Weight phobia (BUT A-WP) was correlated with ORTO-12, ORTO-9 and ORTO-7. The latter resulted the only one not related to MBRSQ-AS, MBSRQ and its health component (MBSRQ-HOr), as well as to the MBSRQ-OP (Table 4). Moreover, the correlation coefficients between ORTO scores and MBSRQ-AO and -FO were lower for ORTO-7 compared to the other scores (Table 4). On the other hand, ORTO-7 resulted in the only one that was related to the MBSRQ-BASS, and ORTO-9 was the only score related to IPAQ and to its intense activities and walking components (Table 4).
| ORTO-15 | ORTO-12 | ORTO-11 | ORTO-9 | ORTO-7 | |
| BMI (n = 160) | NS | NS | NS | -0.184a | NS |
| BMI NW-K10neg-EAT-26neg | -0.315a | -0.304a | -0.284a | -0.432c | NS |
| SSI (n = 160) | -0.169a | -0.264c | -0.223b | -0.244b | -0.228b |
| EAT-26 (n = 160) | -0.363c | -0.414c | -0.349c | -0.432c | -0.357c |
| Dieting (n = 160) | -0.429c | -0.444c | -0.387c | -0.516c | -0.307c |
| Bulimia (n = 160) | -0.188a | -0.263c | -0.180a | -0.304c | -0.223b |
| BUT (n = 160) | NS | NS | NS | NS | -0.160a |
| BUT A — WP (n = 160) | NS | -0.187a | NS | -0.181a | -0.166a |
| BUT B (n = 160) | NS | NS | NS | NS | -0.165a |
| MBSRQ (n = 160) | -0.354c | -0.279c | -0.341c | -0.414c | NS |
| MBSRQ-AO (n = 160) | -0.333c | -0.296c | -0.326c | -0.359c | -0.177a |
| MBSRQ-AO NW-K10neg-EAT-26neg (n = 66) | NS | -0.285a | NS | -0.289a | NS |
| MBSRQ-FO (n = 160) | -0.361c | -0.310c | -0.358c | -0.414c | -0.180a |
| MBSRQ-FO NW-K10neg-EAT-26neg (n = 66) | -0.304a | -0.371a | -0.373a | -0.450c | NS |
| MBSRQ-HOr (n = 160) | -0.341c | -0.248b | -0.333c | -0.402c | NS |
| MBSRQ-HOr NW-K10neg-EAT-26 neg (n = 66) | -0.358b | -0.408c | -0.433c | -0.491c | NS |
| MBSRQ-IO (n = 160) | -0.162a | NS | -0.181a | NS | NS |
| MBSRQ-BASS (n = 160) | NS | NS | NS | NS | -0.169a |
| MBSRQ-OP (n = 160) | -0.177a | -0.216b | -0.165a | -0.302c | NS |
| MBSRQ-OP NW-K10neg-EAT-26neg (n = 66) | NS | -0.366b | NS | -0.357b | NS |
| MBRSQ-AS (n = 160) | -0.195a | -0.155a | -0.161a | -0.265c | NS |
| MBSRQ-AS NW-K10neg-EAT-26neg (n = 66) | NS | -0.244a | NS | -0.306a | NS |
| IPAQ (n = 160) | NS | NS | NS | -0.183a | NS |
| Walking (n = 160) | NS | NS | NS | -0.162a | NS |
| Intense activity (n = 160) | NS | NS | NS | -0.178a | NS |
| Intense activity NW-K10neg-EAT-26neg (n = 66) | -0.404c | -0.330b | -0.273a | -0.461c | NS |
In the NW-K10neg-EAT-26neg subgroup, we did not find many correlations as observed in the whole sample, including those between ORTO scores and BUT, SSI, total MBSRQ and some of its components (Table 4). Although no relationship was found among ORTO score and SSI in the NW-K10neg-EAT-26neg subgroup, SSI was correlated with MBSRQ-OP (0.291, P < 0.05). The latter, as well as MBSRQ-AO and -AS, was correlated with ORTO-12 and ORTO-9 (Table 4), but also with BMI (0.260, P < 0.05).
On the other hand, in the NW-K10neg-EAT-26neg subgroup, MET-min/wk from intense activities correlated with ORTO-15, -12, -11 and -9 (Table 4), as well as with BMI (0.442, P < 0.001), MBSRQ-FO (0.629, P < 0.001), -HOr (0.387, P < 0.01), that were highly related (coefficient of correlation MBSRQ-FO vs MBSRQ-HOr: 0.629, P < 0.001) and, to a lesser extent, IPAQ-intense activity was related to MBSRQ-OP (0.253, P < 0.05). MBSRQ-IO correlated with both MBSRQ-HOr (0.447, P < 0.001) and -AO (0.256, P < 0.05), that was related to MBSRQ-FO (0.329, P < 0.01). Interestingly, ORTO-7 resulted in the only score unrelated neither with BMI nor with the other evaluated outcomes in the NW-K10neg-EAT-26neg subgroup (Table 4). The prevalence of ON from ORTO-7 in students included in the NW-K10neg-EAT-26neg subgroup on the overall sample resulted to be 16.9%, 12.2%, 15.2% and 25.9% for IT-F, IT-M, SP-F and SP-M, respectively.
In light of the reported overlaps of ON with other conditions and of the criticism highlighted from literature about ORTO-15[17-34], we have evaluated the prevalence of ON among 160 Italian and Spanish university students, from the 194 recruited in a previous study[35], who agreed to fill the standardized questionnaires: EAT-26, K10, BUT, MBSRQ, and IPAQ. The sample had, on average, a medium adherence to the Mediterranean diet and a low risk of excessive alcohol consumption[35]. Concerning country differences, the prevalence of mild distress was higher in SP-M compared to IT-M (Table 1), whereas IT-F had lower BUT-A -WP than SP-F (Table 2). SP-M had higher total MBSRQ, MBSRQ-AO, -FO, -HOr, -BASS and -AS, whereas no differences were found in MBSRQ-IO and -OP (Table 2).
Higher SSI, EAT-26 and ON, by using ORTO-15 (40 cut-off), -12, -11 and -9, were observed in Spanish students compared to Italians, regardless of sex (Table 3). Accordingly, no significant difference between female and male students in ORTO-15 has been reported in university students[25,44,45].
Among NW Polish university students, ORTO-15 correlated with MBSRQ-OP, -AO, -FO, -HOr and -BASS in females, whereas in male students, body image concerns were not associated with ON[38]. The Spearman correlations (Table 4) confirmed the previously reported relationship between ON, depending on ORTO score applied to the whole sample, and MBSRQ-OP, -AO[34], and EAT-26[32,33], and we have observed overlaps between ORTO scores, EAT-26 and K10 (Figure 1). Although the prevalence of UW, OW and OB students did not reach significance in the whole sample, IT-F had a lower BMI (Table 1) and higher BUT-A – BIC (Table 2) than IT-M.
In order to reduce the potential confounder as being on a diet[31], we have evaluated a subgroup of NW students, excluding volunteers who presented distress or ED risk (NW-K10neg-EAT-26neg). All students in the NW-K10neg-EAT-26neg group had ON, when ORTO-15 with the 40 cut-off was applied, whereas the percentage of ON varied with ORTO-15 (35 cut-off), -11, -9 and -7. Concerning lifestyle, the percentage of non-smokers was higher compared to those of smokers among students with ON in the NW-K10neg-EAT-26neg group. In this context, it has been proposed to distinguish between ON and healthy orthorexia (HO), a non-pathological tendency to follow a healthy diet[46]. HO can be the successful result of dissemination campaigns aimed to increase nutrition knowledge from WHO and National recommendations, but the proposed etiology of ON includes high level of education, pseudoscientific nutritional news on social media and psychological factors[12]. From a study carried out in nutrition and dietetics, university students emerged that Instagram use might be considered as an ON-risk factor[47]. Besides, K10 median of the scores of students enrolled in health-related study courses was higher than those of non-health-related degree courses[48]. Furthermore, it has been suggested that obsessive healthy eating fixations may increase the risk for ED in athletes and that more education and awareness are warranted to minimize the risk for ON and ED in student-athletes[30]. High level of PA in association with ON, assessed with ORTO-15 using cut-off scores of 35, was more often seen in men from sports science and less often in women from business course[27]. With a cut-off of 40, ORTO-15 resulted lower among students who performed more than ten h/wk of exercise, regardless of the engagement in university sport teams, including athletes competing in aesthetic and weight dependent sports[28]. In our sample, sex differences were found in MET-min/wk from intense activities in both countries (Table 1). In the NW-K10neg-EAT-26neg group, among the students with ON, the percentage of those practicing high PA was higher compared to those having low PA, whereas we did not find correlations observed in the whole sample, including those between ORTO scores and BUT, SSI, and total MBSRQ.
The present study has both strengths and limitations, taking into account the suggestion of a pilot study[49] that reported high levels of disparity among psychometric scores, including ORTO-15, EAT-26 and MBSRQ, recommending the use of multiple psychometric instruments for ON diagnosis. Furthermore, the evaluation of dietary intakes of 10 individuals (assessed using 24-h recall) failed to meet the guidelines for several nutrients[49]. As a point of strength, we have used different stan-dardized questionnaires in order to exclude students presenting overlaps. As a limitation, we did not evaluate the nutritional status. However, the relationships between SSI and all ORTO scores observed in the whole sample, but not in the NW-K10neg-EAT-26neg subgroup, suggest that students with more starvation symptoms were excluded from the applied exclusion criteria. In fact, the greatest strength is that ORTO-7 resulted in the only score unrelated neither with BMI nor with the other evaluated outcomes in the NW-K10neg-EAT-26neg subgroup (Table 4). The prevalence of ON from ORTO-7 after the “exclusion diagnosis” in the NW-K10neg-EAT-26neg subgroup on the overall sample ranged between 12.2% and 25.9%, values lower than those reported in the whole sample. However, it was higher than some observed with other sub-scores of ORTO test (Table 4). This finding suggests that, among the limitations, we did not include the OCD in the “exclusion diagnosis”[50]. However, Łucka et al[29] using ORTO-15 (score of 35 was considered as cut-off point), EAT-26 and Maudsley Obsessive Compulsive Inventory (MOCI), found that individuals with suspected ON (ORTO-15, score of 35) had higher BMI and EAT-26 score, whereas MOCI did not differ from ORTO-15 negative group. From that, authors suggested that ON meets the criteria of ED and not of OCD[29]. On the other hand, considering the relationship among other ORTO scores and body concerns, and high PA component of IPAQ, also questionnaires evaluating exercise addiction[51,52] and muscle dysmorphia[26] should be included in the “exclusion diagnosis”.
Among exclusion diagnosis (gastrointestinal disorders) there are functional dyspepsia[53], non-celiac gluten sensitivity (NCGS)[54,55] and irritable bowel syndrome (IBS)[55]. Both NCGS and IBS are more prevalent in young women compared to men[55], and up to 90% of patients with IBS exclude certain foods to improve their gastrointestinal symptoms[56]. Besides, negative effects of prescribing restrictive diets can be observed due to the association between ED and gastrointestinal symptoms[56]. In this context, the differential diagnosis and assessment of AN already began with the exclusion of diseases, including inflammatory bowel disease (Crohn’s disease or ulcerative colitis), malignancies, thyrotoxicosis, diabetes, cerebral tumor, major depressive or schizophrenic illnesses[10].
Although the scientific community is divided into those who consider ON as a separate ED and those who do not[7], agreement exists on the needs of prevention (primary and secondary) and some diagnostic criteria, as reviewed by Atzeni et al[16], including: obsessive concern for healthy eating, fear anxiety and avoidance of certain foods components (additives, preservatives, fats or other elements considered unhealthy). Furthermore, there is broad consensus on the induction of malnutrition by ON and impacts on social and professional functioning. Other suggested criteria (not endorsed by all experts) included differences between ON and OCD or from schizophrenia, excessive time spent or rituals in preparing meals, excessive spending money for buying healthy foods; anxieties and fears concerning transgressions, and the exclusion of individuals who observe a religious practice or have medical problems[16]. Our work suggests including EDs and psychological distress among the medical problems for the exclusion diagnosis of ON in healthy NW individuals. Otherwise, we suggest considering ON as a symptom of other diseases or a disease-induced comorbidity.
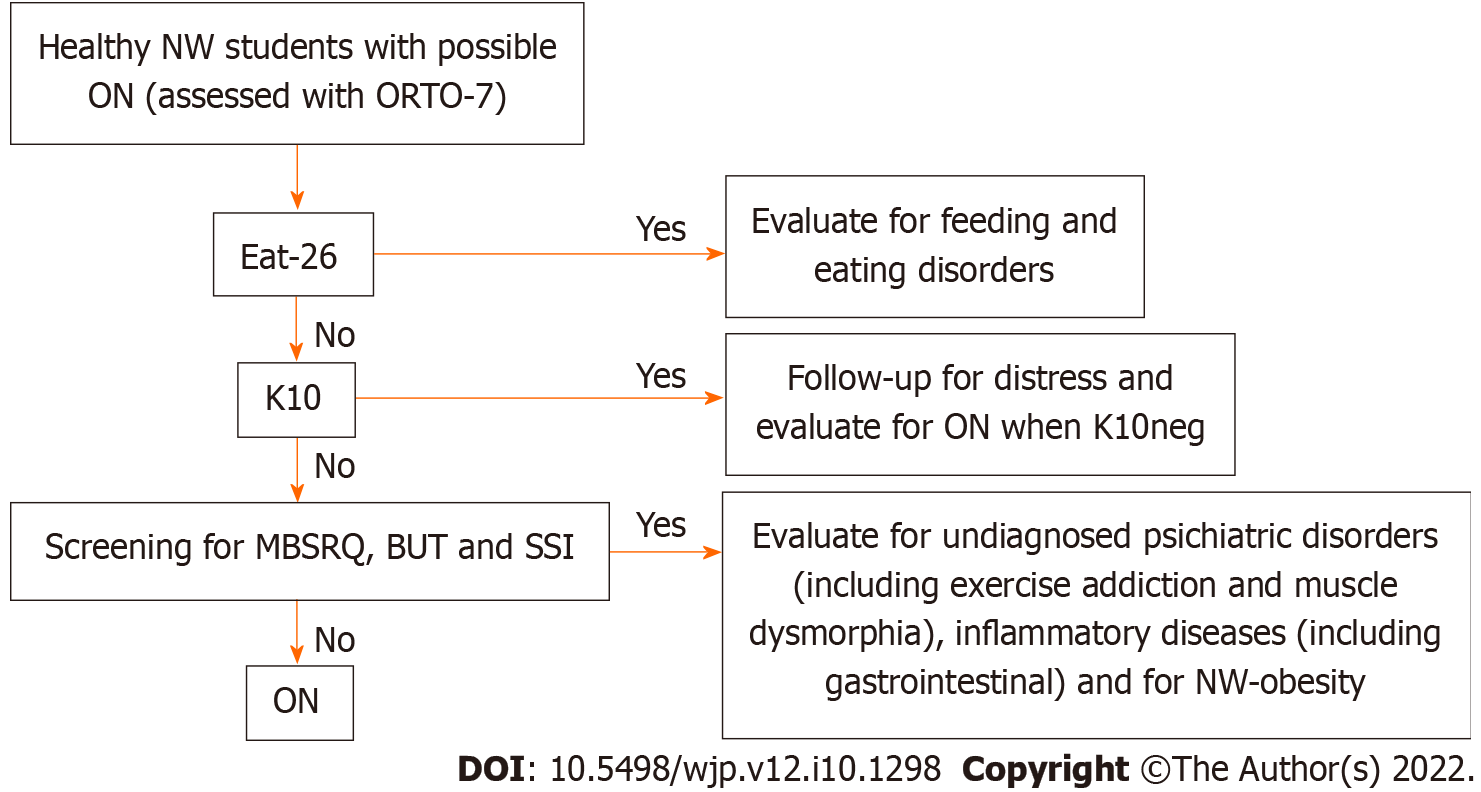
Although a generalization to the whole population should not be made, considering the recent suggestions on the need for further investigation of the comorbidity between ON and OCD across different cultural groups[50], it emerged that ON could be an indicator/symptom of other problems related to body image perception, as well as high PA, psychological distress, appearance, fitness, health, or IO, in some university students. Accordingly, recent studies have found relationships between ON, vigorous-intensity PA and dieting[47,57]. In our study, the ORTO-7 was found to be independent from these confounders, after the exclusion of UW, OW, OB, and EAT-26 and K10 positive students, suggesting the possibility of defining subjects with ON. Therefore, considering the overlap conditions, we suggest a decision tree for differential/exclusion diagnosis of ON (Figure 3). In order to identify the real orthorexic subjects among healthy students with NW, firstly the presence of EDs should be assessed, followed by the evaluation of the distress level, and lastly the presence of body image concerns and malnutrition (Figure 3). Moreover, a high percentage of students (25.5% males and 40.1% females) with NW obesity (NWO) have been reported, and stress management behavior decreased the risk of NWO in females[58]. In this context, Villa et al[47] observed that ON was associated not only with heavy exercise but also with sedentary behavior. In students with NWO, low PA could be associated with dieting, inducing ON. In conclusion, due to the several confounders and overlap conditions, flowcharts, diagnostic algorithms and a decision tree for differential diagnosis and management of ON should be included, as well as guidelines and consensus statements of experts in the future.
Many factors have been associated to orthorexia nervosa in university students.
To assess the prevalence of orthorexia nervosa in Italian and Spanish university students.
To assess the prevalence of orthorexia nervosa in relation to eating attitude and psychological distress.
Questionnaires were administered to evaluate orthorexia nervosa, body concerns, psychological distress, physical activity, eating attitude and starvation symptoms.
When excluding students underweight (UW), overweight (OW) or obese (OB), as well as those potentially at risk of eating disorders or presenting distress, in the resultant normal weight (NW)-K10neg-EAT-26neg subgroup, we did not find many correlations observed in the whole sample, including those between ORTO scores and Body Uneasiness Test, Starvation Symptom Inventory, Total Multidimensional Body-Self Relations Questionnaire (MBSRQ) and some of its components. Moreover, ORTO-7 resulted the only ON score unrelated with Body Mass Index, MBSRQ components and IPAQ-assessed intense activity, in the NW-K10neg-EAT-26neg subgroup. After this sort of “exclusion diagnosis”, ORTO-7 became independent from these confounding, after the exclusion of UW, OW, OB and students positive to EAT-26 and K10, suggesting the possibility of identifying orthorexic subjects with this specific questionnaire.
In some university students ON could be a symptom of other conditions related to body image concerns and distress, as well as to high physical activity and appearance, fitness, health or illness orientation. ORTO-7 became independent from these confounding factors, after the exclusion of UW, OW, OB and students positive to EAT-26 and K10, suggesting the possibility of identifying orthorexic subjects with this specific questionnaire.
Considering the overlap conditions, we suggest a decision tree for differential/exclusion diagnosis of ON.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Psychiatry
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Ekine-Afolabi B, United Kingdom; Wierzbicka A, Poland S-Editor: Gao CC L-Editor: Filipodia P-Editor: Zhang XD
| 1. | Parra-Fernández ML, Manzaneque-Cañadillas M, Onieva-Zafra MD, Fernández-Martínez E, Fernández-Muñoz JJ, Prado-Laguna MDC, Brytek-Matera A. Pathological Preoccupation with Healthy Eating (Orthorexia Nervosa) in a Spanish Sample with Vegetarian, Vegan, and Non-Vegetarian Dietary Patterns. Nutrients. 2020;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 2. | Voglino G, Parente E, Bert F, Lo Moro G, Corradi A, Lapiccirella M, Gualano MR, Siliquini R. Orthorexia Nervosa, a challenging evaluation: analysis of a sample of customers from organic food stores. Psychol Health Med. 2021;26:478-486. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 3. | Moroze RM, Dunn TM, Craig Holland J, Yager J, Weintraub P. Microthinking about micronutrients: a case of transition from obsessions about healthy eating to near-fatal "orthorexia nervosa" and proposed diagnostic criteria. Psychosomatics. 2015;56:397-403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 188] [Article Influence: 17.1] [Reference Citation Analysis (0)] |
| 4. | Dunn TM, Bratman S. On orthorexia nervosa: A review of the literature and proposed diagnostic criteria. Eat Behav. 2016;21:11-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 327] [Cited by in RCA: 356] [Article Influence: 39.6] [Reference Citation Analysis (0)] |
| 5. | Dell'Osso L, Carpita B, Muti D, Cremone IM, Massimetti G, Diadema E, Gesi C, Carmassi C. Prevalence and characteristics of orthorexia nervosa in a sample of university students in Italy. Eat Weight Disord. 2018;23:55-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 68] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 6. | Busatta D, Cassioli E, Rossi E, Campanino C, Ricca V, Rotella F. Orthorexia among patients with eating disorders, student dietitians and general population: a pilot study. Eat Weight Disord. 2022;27:847-851. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 7. | Gramaglia C, Gattoni E, Ferrante D, Abbate-Daga G, Baldissera E, Calugi S, Cascino G, Castellini G, Collantoni E, Favaro A, Marzola E, Monteleone AM, Monteleone P, Oriani MG, Renna C, Ricca V, Salvo P, Santonastaso P, Segura-Garcia C, Volpe U, Zeppegno P. What do Italian healthcare professionals think about orthorexia nervosa? Eat Weight Disord. 2022;27:2037-2049. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Reynolds R, McMahon S. Views of health professionals on the clinical recognition of orthorexia nervosa: a pilot study. Eat Weight Disord. 2020;25:1117-1124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 9. | Claudino AM, Pike KM, Hay P, Keeley JW, Evans SC, Rebello TJ, Bryant-Waugh R, Dai Y, Zhao M, Matsumoto C, Herscovici CR, Mellor-Marsá B, Stona AC, Kogan CS, Andrews HF, Monteleone P, Pilon DJ, Thiels C, Sharan P, Al-Adawi S, Reed GM. The classification of feeding and eating disorders in the ICD-11: results of a field study comparing proposed ICD-11 guidelines with existing ICD-10 guidelines. BMC Med. 2019;17:93. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 65] [Cited by in RCA: 73] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 10. | Treasure J, Duarte TA, Schmidt U. Eating disorders. Lancet. 2020;395:899-911. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 266] [Cited by in RCA: 502] [Article Influence: 100.4] [Reference Citation Analysis (0)] |
| 11. | Balasundaram P, Santhanam P. Eating Disorders. 2022 Jun 27. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. [PubMed] |
| 12. | Douma ER, Valente M, Syurina EV. Developmental pathway of orthorexia nervosa: Factors contributing to progression from healthy eating to excessive preoccupation with healthy eating. Experiences of Dutch health professionals. Appetite. 2021;158:105008. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 13. | Opitz MC, Newman E, Alvarado Vázquez Mellado AS, Robertson MDA, Sharpe H. The psychometric properties of Orthorexia Nervosa assessment scales: A systematic review and reliability generalization. Appetite. 2020;155:104797. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 43] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 14. | Valente M, Syurina EV, Donini LM. Shedding light upon various tools to assess orthorexia nervosa: a critical literature review with a systematic search. Eat Weight Disord. 2019;24:671-682. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 60] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 15. | Cena H, Barthels F, Cuzzolaro M, Bratman S, Brytek-Matera A, Dunn T, Varga M, Missbach B, Donini LM. Definition and diagnostic criteria for orthorexia nervosa: a narrative review of the literature. Eat Weight Disord. 2019;24:209-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 218] [Article Influence: 36.3] [Reference Citation Analysis (0)] |
| 16. | Atzeni E, Converso D, Loera B. [Orthorexia Nervosa between growing attention to food quality and eating disorders: diagnostic criteria and evaluation tools]. Riv Psichiatr. 2020;55:201-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 17. | Niedzielski A, Kaźmierczak-Wojtaś N. Prevalence of Orthorexia Nervosa and Its Diagnostic Tools-A Literature Review. Int J Environ Res Public Health 2021; 18 . [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 58] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 18. | Abdullah MA, Al Hourani HM, Alkhatib B. Prevalence of orthorexia nervosa among nutrition students and nutritionists: Pilot study. Clin Nutr ESPEN. 2020;40:144-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 19. | Plichta M, Jezewska-Zychowicz M. Orthorexic Tendency and Eating Disorders Symptoms in Polish Students: Examining Differences in Eating Behaviors. Nutrients. 2020;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 20. | Babeau C, Le Chevanton T, Julien-Sweerts S, Brochenin A, Donini LM, Fouques D. Structural validation of the ORTO-12-FR questionnaire among a French sample as a first attempt to assess orthorexia nervosa in France. Eat Weight Disord. 2020;25:1771-1778. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 21. | Parra-Fernandez ML, Rodríguez-Cano T, Perez-Haro MJ, Onieva-Zafra MD, Fernandez-Martinez E, Notario-Pacheco B. Structural validation of ORTO-11-ES for the diagnosis of orthorexia nervosa, Spanish version. Eat Weight Disord. 2018;23:745-752. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 22. | Missbach B, Hinterbuchinger B, Dreiseitl V, Zellhofer S, Kurz C, König J. When Eating Right, Is Measured Wrong! PLoS One. 2015;10:e0135772. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 140] [Cited by in RCA: 141] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 23. | Moller S, Apputhurai P, Knowles SR. Confirmatory factor analyses of the ORTO 15-, 11- and 9-item scales and recommendations for suggested cut-off scores. Eat Weight Disord. 2019;24:21-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 31] [Article Influence: 5.2] [Reference Citation Analysis (1)] |
| 24. | Moller S, Apputhurai P, Knowles SR. Correction to: Confirmatory factor analyses of the ORTO 15-, 11- and 9-item scales and recommendations for suggested cut-off scores. Eat Weight Disord. 2019;24:981. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 25. | Guglielmetti M, Ferraro OE, Gorrasi ISR, Carraro E, Bo S, Abbate-Daga G, Tagliabue A, Ferraris C. Lifestyle-Related Risk Factors of Orthorexia Can Differ among the Students of Distinct University Courses. Nutrients. 2022;14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 26. | Gorrasi ISR, Bonetta S, Roppolo M, Abbate Daga G, Bo S, Tagliabue A, Ferraris C, Guglielmetti M, Arpesella M, Gaeta M, Gallé F, Di Onofrio V, Liguori F, Liguori G, Gilli G, Carraro E. Traits of orthorexia nervosa and muscle dysmorphia in Italian university students: a multicentre study. Eat Weight Disord. 2020;25:1413-1423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 27. | Malmborg J, Bremander A, Olsson MC, Bergman S. Health status, physical activity, and orthorexia nervosa: A comparison between exercise science students and business students. Appetite. 2017;109:137-143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 70] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 28. | Clifford T, Blyth C. A pilot study comparing the prevalence of orthorexia nervosa in regular students and those in University sports teams. Eat Weight Disord. 2019;24:473-480. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 35] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 29. | Łucka I, Janikowska-Hołoweńko D, Domarecki P, Plenikowska-Ślusarz T, Domarecka M. Orthorexia nervosa - a separate clinical entity, a part of eating disorder spectrum or another manifestation of obsessive-compulsive disorder? Psychiatr Pol. 2019;53:371-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 30. | Uriegas NA, Winkelmann ZK, Pritchett K, Torres-McGehee TM. Examining Eating Attitudes and Behaviors in Collegiate Athletes, the Association Between Orthorexia Nervosa and Eating Disorders. Front Nutr. 2021;8:763838. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 31. | Roncero M, Barrada JR, Perpiñá C. Measuring Orthorexia Nervosa: Psychometric Limitations of the ORTO-15. Span J Psychol. 2017;20:E41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 81] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 32. | Gramaglia C, Gambaro E, Delicato C, Marchetti M, Sarchiapone M, Ferrante D, Roncero M, Perpiñá C, Brytek-Matera A, Wojtyna E, Zeppegno P. Orthorexia nervosa, eating patterns and personality traits: a cross-cultural comparison of Italian, Polish and Spanish university students. BMC Psychiatry. 2019;19:235. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 47] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 33. | Farchakh Y, Hallit S, Soufia M. Association between orthorexia nervosa, eating attitudes and anxiety among medical students in Lebanese universities: results of a cross-sectional study. Eat Weight Disord. 2019;24:683-691. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 49] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 34. | Barnes MA, Caltabiano ML. The interrelationship between orthorexia nervosa, perfectionism, body image and attachment style. Eat Weight Disord. 2017;22:177-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 152] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 35. | Aiello P, Peluso I, Villaño Valencia D. Alcohol Consumption by Italian and Spanish University Students in Relation to Adherence to the Mediterranean Diet and to the Food Neophobia: A Pilot Study. Healthcare (Basel). 2022;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 36. | Donini LM, Marsili D, Graziani MP, Imbriale M, Cannella C. Orthorexia nervosa: validation of a diagnosis questionnaire. Eat Weight Disord. 2005;10:e28-e32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 265] [Cited by in RCA: 300] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 37. | Roncero M, Perpiñá C, Marco JH, Sánchez-Reales S. Confirmatory factor analysis and psychometric properties of the Spanish version of the Multidimensional Body-Self Relations Questionnaire-Appearance Scales. Body Image. 2015;14:47-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 31] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 38. | Brytek-Matera A, Donini LM, Krupa M, Poggiogalle E, Hay P. Orthorexia nervosa and self-attitudinal aspects of body image in female and male university students. J Eat Disord. 2015;3:2. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 89] [Cited by in RCA: 99] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 39. | Cuzzolaro M, Vetrone G, Marano G, Garfinkel PE. The Body Uneasiness Test (BUT): development and validation of a new body image assessment scale. Eat Weight Disord. 2006;11:1-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 217] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 40. | Rivas T, Bersabé R, Jiménez M, Berrocal C. The Eating Attitudes Test (EAT-26): reliability and validity in Spanish female samples. Span J Psychol. 2010;13:1044-1056. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 87] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 41. | Calugi S, Miniati M, Milanese C, Sartirana M, El Ghoch M, Dalle Grave R. The Starvation Symptom Inventory: Development and Psychometric Properties. Nutrients. 2017;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 42. | Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E, Howes MJ, Normand SL, Manderscheid RW, Walters EE, Zaslavsky AM. Screening for serious mental illness in the general population. Arch Gen Psychiatry. 2003;60:184-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3209] [Cited by in RCA: 3537] [Article Influence: 160.8] [Reference Citation Analysis (0)] |
| 43. | Società Italiana Endocrinologia. Questionario sull’attività fisica quotidiana (IPAQ). [cited 10 October 2021]. In: Società Italiana Endocrinologia [Internet]. Available from: http://www.societaitalianadiendocrinologia.it/public/pdf/questionario_ipaq.pdf. |
| 44. | Brytek-Matera A, Fonte ML, Poggiogalle E, Donini LM, Cena H. Orthorexia nervosa: relationship with obsessive-compulsive symptoms, disordered eating patterns and body uneasiness among Italian university students. Eat Weight Disord. 2017;22:609-617. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 55] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 45. | Oberle CD, Samaghabadi RO, Hughes EM. Orthorexia nervosa: Assessment and correlates with gender, BMI, and personality. Appetite. 2017;108:303-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 131] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 46. | Depa J, Barrada JR, Roncero M. Are the Motives for Food Choices Different in Orthorexia Nervosa and Healthy Orthorexia? Nutrients. 2019;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 72] [Cited by in RCA: 87] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 47. | Villa M, Opawsky N, Manriquez S, Ananías N, Vergara-Barra P, Leonario-Rodriguez M. Orthorexia nervosa risk and associated factors among Chilean nutrition students: a pilot study. J Eat Disord. 2022;10:6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 11] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 48. | Pehlivan Ş, Tokur Kesgi N M, Uymaz P. Psychological distress and mental health literacy in university students. Perspect Psychiatr Care. 2021;57:1433-1441. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 49. | Mitrofanova E, Mulrooney H, Petróczi A. Assessing psychological and nutritional impact of suspected orthorexia nervosa: a cross-sectional pilot study. J Hum Nutr Diet. 2021;34:42-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 50. | Brytek-Matera A, Pardini S, Modrzejewska J, Modrzejewska A, Szymańska P, Czepczor-Bernat K, Novara C. Orthorexia Nervosa and its association with obsessive-compulsive disorder symptoms: initial cross-cultural comparison between Polish and Italian university students. Eat Weight Disord. 2022;27:913-927. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 51. | Trott M, Jackson SE, Firth J, Fisher A, Johnstone J, Mistry A, Stubbs B, Smith L. Exercise Addiction Prevalence and Correlates in the Absence of Eating Disorder Symptomology: A Systematic Review and Meta-analysis. J Addict Med. 2020;14:e321-e329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 20] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 52. | Oberle CD, Watkins RS, Burkot AJ. Orthorexic eating behaviors related to exercise addiction and internal motivations in a sample of university students. Eat Weight Disord. 2018;23:67-74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 61] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 53. | Mounsey A, Barzin A, Rietz A. Functional Dyspepsia: Evaluation and Management. Am Fam Physician. 2020;101:84-88. [PubMed] |
| 54. | Tanveer M, Ahmed A. Non-Celiac Gluten Sensitivity: A Systematic Review. J Coll Physicians Surg Pak. 2019;29:51-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 55. | Ahmed H, Hallam R, Webster G, Rej A, Croall ID, Coleman SH, Key T, Buckle R, Shaw CC, Goodwin J, Aziz I, Sanders DS. NCGS like IBS 'type' symptoms is a diagnosis of exclusion. Nutr J. 2021;20:79. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 56. | McGowan A, Harer KN. Irritable Bowel Syndrome and Eating Disorders: A Burgeoning Concern in Gastrointestinal Clinics. Gastroenterol Clin North Am. 2021;50:595-610. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 57. | Brytek-Matera A, Pardini S, Szubert J, Novara C. Orthorexia Nervosa and Disordered Eating Attitudes, Self-Esteem and Physical Activity among Young Adults. Nutrients. 2022;14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 17] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 58. | Maitiniyazi G, Chen Y, Qiu YY, Xie ZX, He JY, Xia SF. Characteristics of Body Composition and Lifestyle in Chinese University Students with Normal-Weight Obesity: A Cross-Sectional Study. Diabetes Metab Syndr Obes. 2021;14:3427-3436. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |