Published online Sep 9, 2025. doi: 10.5409/wjcp.v14.i3.102309
Revised: March 7, 2025
Accepted: March 27, 2025
Published online: September 9, 2025
Processing time: 244 Days and 23.4 Hours
Gastroesophageal reflux disease (GERD) is common among neonates, particularly those requiring mechanical ventilation. Pepsin, a reliable marker of gastric aspi
To determine the incidence of GERD, associated risk factors, and morbidities among full-term mechanically ventilated neonates by detecting pepsin in endo
This study included 97 full-term neonates admitted to the neonatal intensive care unit at Cairo University Hospitals from April 2023 to March 2024. ETA samples were collected at three intervals: Immediately post-intubation (Sample A), 48 hours after intubation (Sample B), and just before extubation (Sample C). Pepsin concentration was measured using enzyme-linked immunosorbent assay. Clinical data, including hospital stay duration and feeding parameters, were correlated with pepsin levels.
Pepsin was detected in 76 (78.4%) of Sample A, 78 (81.3%) of Sample B, and 47 (68.1%) of Sample C. A significant positive correlation was found between pepsin levels and FiO2 in Sample B (r = 0.203, P = 0.047). Prolonged hospital stay was also associated with pepsin detection in Samples B and C (P < 0.05). A negative correlation was observed between feeding amount and pepsin levels across all samples (P < 0.05).
The incidence of GERD in full-term mechanically ventilated neonates is high, correlating with pepsin levels, FiO2, feeding intolerance, and hospital stay, highlighting the importance of early detection.
Core Tip: This study evaluates the incidence of gastroesophageal reflux disease (GERD) in mechanically ventilated full-term neonates using pepsin detection in endotracheal aspirates (ETA). Conducted on 97 neonates, the study demonstrates that pepsin was detected in 76.7% of samples collected, with significant correlations between pepsin levels, FiO2, feeding amount, and hospital stay duration. The findings highlight the association of GER episodes with feeding intolerance and prolonged hospitalization, emphasizing the importance of early GER detection through ETA pepsin measurement. These insights can guide clinical interventions to mitigate complications and improve neonatal outcomes, though further studies are warranted to explore preventive strategies and optimize care in this vulnerable population.
- Citation: Elrefaee A, Abdel-Razek ARA, Abdelkhalek ZS, Samaan P, Kamal AF. Incidence of gastro-esophageal reflux disease in mechanically ventilated full-term Egyptian neonates by detection of pepsin in endotracheal aspirate. World J Clin Pediatr 2025; 14(3): 102309
- URL: https://www.wjgnet.com/2219-2808/full/v14/i3/102309.htm
- DOI: https://dx.doi.org/10.5409/wjcp.v14.i3.102309
Gastroesophageal reflux disease (GERD) is a common diagnosis among neonates, affecting approximately one in ten newborns admitted to the neonatal intensive care unit (NICU). It is associated with prolonged hospital stays and increased healthcare costs[1]. GERD in preterm infants is often misunderstood, over diagnosed, and overtreated[2]. Neonatal GERD is characterized by the backflow of stomach contents from the high-pressure stomach into the lower-pressure esophagus[3].
The lower esophageal sphincter (LES) relaxes intermittently, allowing stomach contents to move into the esophagus. Several factors can trigger LES relaxation, including swallowing, gastric distension, straining, and caffeine administration[4]. While cuffed endotracheal tubes in ventilated pediatric and adult patients help prevent aspiration, microaspiration can still occur in neonates who are intubated with uncuffed endotracheal tubes[5].
The clinical presentation of GERD is nonspecific, spanning various symptom categories. Respiratory symptoms include stridor, coughing, aspiration, and wheezing; gastrointestinal symptoms involve emesis, poor oral intake, and regurgitation. Cardiorespiratory symptoms include episodes of desaturation, apnea, and bradycardia, while neurogenic symptoms may present as irritability or back-arching[6].
Pepsin, a key digestive enzyme in the stomach, is absent in the normal esophagus and respiratory system. However, it can be detected in the lungs when gastric contents are aspirated, making it a valuable biochemical marker of silent as
GERD is more prevalent in preterm neonates than in full-term ones, but the significant complications associated with GERD highlight the need to evaluate its prevalence and risk factors in full-term neonates. Understanding these factors is essential for mitigating preventable risks and improving outcomes in neonatal care[9].
The objective of this study was to determine the incidence of GERD, as well as the risk factors and morbidities associated with GERD, in full-term mechanically ventilated neonates.
This study was conducted on 97 full-term neonates admitted to the NICU at Cairo University Hospitals between April 2023 and March 2024. This study was conducted in accordance with the principles outlined in the Declaration of Helsinki and approved by the Research Ethics Committee of the Faculty of Medicine, Cairo University (No. MD-430-2022). Written informed consent was obtained from the parents or legal guardians of all participating neonates before enrollment in the study.
The study included full-term neonates who required mechanical ventilation during their hospital stay. Neonates with certain surgical conditions, including diaphragmatic hernia, tracheoesophageal fistula, and esophageal atresia, were excluded, as were those with repaired esophageal atresia. Preterm neonates and those with associated congenital anomalies were also not eligible for inclusion.
Clinical data were gathered from patient medical records and during clinical examinations. The collected data included general clinical characteristics, such as weight, sex, mode of delivery, Appearance, Pulse, Grimace, Activity, Respiration (APGAR) score, resuscitation method, age at intubation, and medications administered during the NICU stay, including inotropes, sedatives, steroids, and anti-reflux medications such as prokinetic agents (Domperidone and Trimebutine) and proton pump inhibitors. Additionally, the neonates' final outcomes were recorded.
During the mechanical ventilation period, each neonate underwent three endotracheal aspirate (ETA) collections for pepsin measurement. The first sample (Sample A) was collected immediately after intubation, the second (Sample B) 48 hours post-intubation, and the third (Sample C) immediately before extubation. Aspirates were obtained using open suction with normal saline lavage (1–2 mL/kg) and a suction pressure of 80–120 mmHg. Catheter sizes were selected to be less than 50% of the internal diameter of the endotracheal tube, adjusted according to the neonate's weight. During suction, the neonates were positioned with the head elevated at 45 degrees, and their oxygen saturation and hemodynamic parameters were stabilized prior to the procedure. Analgesia or sedation boluses were administered as needed.
The collected aspirates were processed using the Micro enzyme-linked immunosorbent assay (ELISA) 2000–3000, pre-coated with antibodies specific to pepsin. The samples were centrifuged at 2000–3000 rpm for 20 minutes, and the supernatant was transferred into sterile tubes and stored at -20 °C for later analysis using an ELISA kit. The ELISA measured pepsin concentration using the sandwich assay technique. Standards and samples were placed in micro-ELISA strip plate wells pre-coated with anti-pepsin antibodies. After incubation and washing to remove unbound components, a horseradish peroxidase (HRP)-conjugated anti-pepsin antibody was added, followed by further incubation. A substrate solution reactive with HRP was added, leading to a color change from blue to yellow, indicating pepsin presence. Optical density (OD) was measured at 450 nm, with the pepsin concentration determined by comparing OD values to a reference curve. A pepsin level of 0.0625 ng/mL was established as the assay's sensitivity threshold.
Data analysis was performed using the SPSS version 17.0 (Chicago, IL, United States). Statistical significance was assessed using the Student’s t-test and χ2 test where appropriate. Log-transformation was applied to normalize skewed data. The Mann-Whitney U test and χ2 test were used to compare variables between groups, while comparisons across multiple groups were performed using one-way analysis of variance. A P value of < 0.05 was considered statistically significant. Continuous data are presented as mean ± SD, while categorical data are expressed as percentages.
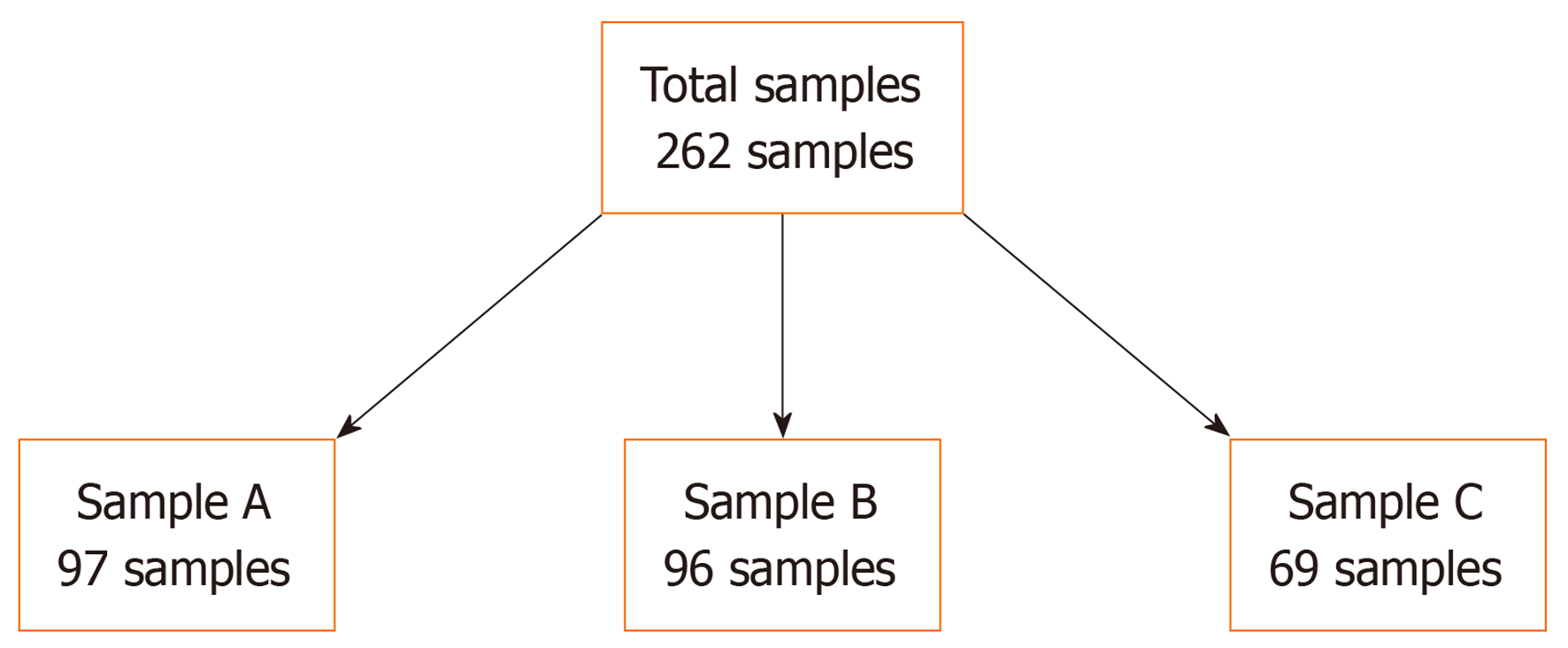
Sample A (immediately after intubation) was done to 97 of the studied cases. Sample B (after 48 hours of intubation) was done to 96 of the studied cases, and Sample C (immediately before extubation) was done to 69 of the studied cases based on the survival of the cases during the time of sample withdrawal (Figure 1). Chest imaging was done during the duration of the study.
The studied neonates had a median age at intubation of 1 day, with an interquartile range (IQR) of 1–2 days and a range from 1 to 10 days. Intubation since birth was recorded in 65 cases (67.0%), while 32 neonates (33.0%) were intubated later. Males comprised 66 (68.0%) of the cases, and females 31 (32.0%). The mean birth weight was 2.84 ± 0.45 kg, with a range of 1.89 to 4.5 kg. Most neonates (76, 78.4%) had birth weights appropriate for gestational age (≥ 2.5 kg), while 21 neonates (21.6%) were small for gestational age (< 2.5 kg). Cesarean section was the predominant mode of delivery, occurring in 83 cases (85.6%), with only 14 cases (14.4%) born via normal vaginal delivery. The median APGAR score at 1 minute was 3 (IQR: 1–3), with scores ranging from 0 to 7. At 5 minutes, the median APGAR score increased to 7 (IQR: 6–8), with a range of 2 to 10. Resuscitation methods included positive pressure ventilation in 35 cases (36.1%), tactile stimulation in 12 cases (12.4%), and intubation in 50 cases (51.5%) (Table 1).
| Characteristics | Total (n = 97) |
| Age on intubation (days) | |
| Median (IQR) | 1 (1–2) |
| Range | 1–10 |
| Intubation since birth | |
| Yes | |
| 65 (67.0) | |
| No | 32 (33.0) |
| Sex | |
| Male | 66 (68.0) |
| Female | 31 (32.0) |
| Birth weight (kg) | |
| mean ± SD | |
| 2.84 ± 0.45 | |
| Range | 1.89–4.5 |
| Weight for age | |
| Appropriate for GA (2.5 kg or more) | |
| 76 (78.4) | |
| Small for GA (less than 2.5 kg) | 21 (21.6) |
| Mode of delivery | |
| Cesarean section | 83 (85.6) |
| Normal vaginal delivery | 14 (14.4) |
| APGAR score at 1 minute | |
| Median (IQR) | 3 (1–3) |
| Range | 0-7 |
| APGAR score at 5 minutes | |
| Median (IQR) | 7 (6–8) |
| Range | 2–10 |
| Resuscitation | |
| Positive pressure ventilation | 35 (36.1) |
| Tactile stimulation | 12 (12.4) |
| Intubation | 50 (51.5) |
The indications for mechanical ventilation among the studied neonates varied. Pulmonary hypertension was the most common cause, accounting for 42 cases (43.3%), followed by respiratory distress of undefined cause in 18 cases (18.6%). Hypoxic-ischemic encephalopathy was present in 14 neonates (14.4%), while pneumonia and meconium aspiration were identified as causes in 11 (11.3%) and 10 (10.3%) cases, respectively. Additionally, 2 neonates (2.1%) required ventilation due to heart failure.
Pepsin levels were measured in three samples collected from the studied neonates. In Sample A, the median pepsin concentration was 0.87 ng/mL (IQR: 0.11–2.58), with values ranging from 0.01 to 31 ng/mL. Pepsin was detected in 76 cases (78.4%), while it was not detected in 21 cases (21.6%). For Sample B, the median pepsin concentration was 0.84 ng/mL (IQR: 0.23–2.68), with a range of 0.01 to 12.5 ng/mL. Pepsin was detected in 78 cases (81.3%) and not detected in 18 cases (18.8%). In Sample C, the median concentration was 0.43 ng/mL (IQR: 0.05–1.63), with a range from 0.01 to 8.68 ng/mL. Pepsin was detected in 47 cases (68.1%), while it was not detected in 22 cases (31.9%) (Table 2)
| Characteristics | Total (n = 97) |
| Sample A ETA pepsin (ng/mL) | |
| Median (IQR) | 0.87 (0.11–2.58) |
| Range | 0.01–31 |
| Pepsin detection in sample A | |
| Not detected | 21 (21.6) |
| Detected | 76 (78.4) |
| Sample B ETA pepsin (ng/mL) | |
| Median (IQR) | 0.84 (0.23–2.68) |
| Range | 0.01–12.5 |
| Pepsin detection in sample B | |
| Not detected | 18 (18.8) |
| Detected | 78 (81.3) |
| Sample C ETA pepsin (ng/mL) | |
| Median (IQR) | 0.43 (0.05–1.63) |
| Range | 0.01–8.68 |
| Pepsin detection in sample C | |
| Not detected | 22 (31.9) |
| Detected | 47 (68.1) |
No significant differences were observed between pepsin detection in Sample A and ETA culture results (P = 0.129), in Sample B and ETA culture results (P = 0.595), or in Sample C and ETA culture results (P = 0.776) (Table 3).
| Pepsin detection in sample A | Test value | P value | |||
| No detection (n = 21) | Detected (n = 76) | ||||
| ETA culture | Not done | 5 (23.8) | 8 (10.5) | 4.0961 | 0.129 |
| No growth | 10 (47.6) | 30 (39.5) | |||
| Positive | 6 (28.6) | 38 (50) | |||
| Pepsin detection in sample B | |||||
| ETA culture | Not done | 2 (11.1) | 11 (14.1) | 1.0391 | 0.595 |
| No growth | 6 (33.3) | 34 (43.6) | |||
| Positive | 10 (55.6) | 33 (42.3) | |||
| Pepsin detection in sample C | |||||
| ETA culture | Not done | 3 (13.6) | 4 (8.5) | 0.506 | 0.776 |
| No growth | 9 (40.9) | 22 (46.8) | |||
| Positive | 10 (45.5) | 21 (44.7) | |||
The median duration of hospital stay for the studied cases was 15 days (IQR: 10–22), ranging from 4 to 35 days. Regarding outcomes, 38 neonates (39.2%) died, while 59 (60.8%) were discharged (Table 4).
| Characteristics | Total (n = 97) |
| Duration of hospital stay (days) | |
| Median (IQR) | 15 (10–22) |
| Range | 4–35 |
| Outcome | |
| Died | 38 (39.2) |
| Discharged | 59 (60.8) |
A significant association was found between pepsin detection in Sample B and pepsin detection in Sample C (P = 0.034). However, no significant differences were observed between pepsin detection in Sample B and pepsin levels in Sample A (P = 0.189) or Sample C (P = 0.073). Additionally, the detection of pepsin in Sample B was not significantly associated with pepsin detection in Sample A (P = 0.053) (Table 5).
| Pepsin detection in sample B | Test value | P value | ||
| No detection (n = 18) | Detected (n = 78) | |||
| Sample A ETA pepsin (ng/mL) | -1.314 | 0.189 | ||
| Median (IQR) | ||||
| 0.48 (0.02–1.9) | 0.94 (0.28–2.67) | |||
| Range | 0.01–7.27 | 0.01–31 | ||
| Pepsin detection in sample A | 3.752 | 0.053 | ||
| No detection | ||||
| 7 (38.9) | 14 (17.9) | |||
| Detected | 11 (61.1) | 64 (82.1) | ||
| Sample C ETA pepsin (ng/mL) | -1.794 | 0.073 | ||
| Median (IQR) | ||||
| 0.03 (0.01–1.43) | 0.51 (0.06–1.73) | |||
| Range | 0.01–4.02 | 0.01–8.68 | ||
| Pepsin detection in sample C | 4.494 | 0.034a | ||
| No detection | ||||
| 7 (58.3) | 15 (26.8) | |||
| Detected | 5 (41.7) | 41 (73.2) | ||
Pepsin levels in Sample B showed significant positive correlations with FiO2 (r = 0.203, P = 0.047) and the duration of hospital stay (r = 0.288, P = 0.004). Pepsin levels in Sample C were also positively correlated with the duration of hospital stay (r = 0.559, P = 0.000). In contrast, pepsin levels in all three samples (A, B, and C) showed significant negative correlations with the amount of feeding: Sample A (r =
| Sample A ETA pepsin (ng/mL) | Sample B ETA pepsin (ng/mL) | Sample C ETA pepsin (ng/mL) | ||||
| r | P value | r | P value | r | P value | |
| Age on intubation (days) | -0.027 | 0.791 | 0.082 | 0.429 | -0.170 | 0.164 |
| Birth weight | 0.010 | 0.919 | 0.155 | 0.132 | -0.137 | 0.261 |
| APGAR score at 1 minute | -0.082 | 0.426 | 0.027 | 0.795 | 0.008 | 0.951 |
| APGAR score at 5 minutes | -0.020 | 0.847 | -0.062 | 0.549 | 0.087 | 0.476 |
| Proton pump inhibitor (days) | -0.004 | 0.981 | 0.054 | 0.748 | -0.049 | 0.816 |
| Prokinetic drugs (days) | 0.005 | 0.976 | -0.050 | 0.784 | -0.230 | 0.259 |
| Duration of MV (days) | 0.080 | 0.438 | 0.130 | 0.208 | -0.129 | 0.292 |
| FiO2 | 0.166 | 0.104 | 0.203 | 0.047a | 0.193 | 0.112 |
| Amount of feeding (mL/day) | -0.210 | 0.039a | -0.234 | 0.022a | -0.267 | 0.027a |
| Duration of hospital stay (days) | 0.031 | 0.766 | 0.288 | 0.004a | 0.559 | 0.000a |
No significant correlations were observed between pepsin levels and age at intubation, birth weight, APGAR scores, or the duration of mechanical ventilation across any of the samples (all P > 0.05). Additionally, no significant correlations were found between pepsin levels and the use of proton pump inhibitors or prokinetic drugs (all P > 0.05) (Table 6).
The mean birth weight of the neonates in our study was 2840 ± 450 g. Of the 97 neonates, 76 (78.4%) had birth weights appropriate for their gestational age, while 21 (21.6%) were classified as small for gestational age. All neonates underwent ETA sampling three times: The first sample (Sample A) was collected immediately after intubation, the second (Sample B) 48 hours post-intubation, and the third (Sample C) immediately before extubation.
A prospective cohort study conducted by Garland et al[10] in Wisconsin, United States, between June 2008 and August 2010, examined the prevalence of tracheal pepsin in ventilated neonates and investigated the correlation between head elevation and tracheal pepsin levels. The study included 66 neonates with a mean birth weight of 798 ± 268 g and a mean gestational age of 26.0 ± 1.7 weeks. Tracheal pepsin was detected in 35 of the 66 neonates (53%). Neonates with a head elevation in the upper quartile (≥ 14 degrees) during the first sampling (day 3) had a significantly lower incidence of tracheal pepsin (4/16 vs 9/10, P = 0.0013) compared to those with a head elevation in the lowest quartile (≤ 8 degrees). The study concluded that tracheal aspiration of gastric contents is common in ventilated neonates, and elevating the head of the bed can reduce aspiration, especially in the early days of ventilation.
In our study, pepsin levels were elevated in Sample A, particularly on days 1 and 2, with a median (IQR) of 0.87 ng/mL (0.11–2.58). Sample B, taken on day 5 of life, showed a median (IQR) pepsin level of 0.84 ng/mL (0.23–2.68). In Sample C, collected on days 7, 12, and 16, the median (IQR) pepsin level was 0.43 ng/mL (0.05–1.63). The lower sensitivity limit of our assay for pepsin detection was 0.0625 ng/mL.
Farhath et al[5] conducted a study in a 39-bed facility in New Jersey, United States, between March 2003 and October 2004, collecting 239 tracheal aspirate samples from 45 premature neonates. These samples were collected on days 1, 3, 5, 7, 14, 21, and 28 of mechanical ventilation, with additional samples obtained if ventilation continued beyond 28 days. Pepsin was detected in 222 of the 239 samples (92.8%). The study found significantly lower pepsin levels on day 1 (mean 170 ± 216 ng/mL) compared to subsequent sampling times. Pepsin levels were also higher on days 5 and 7 in neonates born at 23–25 weeks gestation compared to those born at 26–31 weeks gestation. The assay used in their study defined positive pepsin detection at a sensitivity threshold of 12.5 ng/mL.
In our cohort, 66 (68%) of the neonates were male, and 31 (32%) were female. However, no statistically significant association was found between gender and pepsin detection. In Sample A, pepsin was detected in 52 (68.4%) male neonates and 24 (31.6%) females (P = 0.879). In Sample B, pepsin was found in 53 (67.9%) males and 25 (32.1%) females (P = 0.724). In Sample C, 30 (63.8%) males and 17 (36.2%) females tested positive for pepsin (P = 0.264). A study by Czinn and Blanchard[11] suggested that GER affects 85% of infants, with an incidence 1.6 times higher in males than females.
The median age of the neonates at the time of intubation was 1 day, with an IQR of 1–2 days. Regarding ventilation modes, 63 (64.9%) neonates were ventilated using patient-triggered ventilation, 18 (18.6%) with high-frequency oscillation, and 16 (16.5%) with synchronized intermittent mandatory ventilation. Each neonate had at least one ETA sample collected during the ventilation period.
The APGAR scores at 1 and 5 minutes were not significantly associated with pepsin detection in any of the three samples. For Sample A, the P value was 0.982, for Sample B it was 0.931, and for Sample C it was 0.445. These findings align with a case-control study conducted by Dahlen et al[12], which investigated the risk factors for GERD in very low birth weight infants with bronchopulmonary dysplasia. The study included 23 patients and 23 controls, with 24-hour esophageal pH monitoring conducted between January 2001 and October 2005. It concluded that the APGAR score at 5 minutes and the duration of mechanical ventilation were not significant risk factors for GERD. Furthermore, while Dahlen et al[12] found no significant association between oxygen therapy and GERD, our study identified a positive correlation between pepsin detection in Sample B and FiO2 levels (P = 0.047).
Farhath et al[5] also reported a significant increase in pepsin levels during xanthine therapy (P = 0.036). In our study, we observed a significant relationship between pepsin detection in Sample B and Sample C, but no significant association between pepsin detection in Sample B and Sample A.
This study is limited by its single-center design, which may affect the generalizability of the findings. Additionally, the reliance on pepsin detection as a sole marker for GERD may not capture all reflux events, and the use of uncuffed endotracheal tubes could contribute to variability in microaspiration. Furthermore, the relatively small sample size and lack of long-term follow-up may limit the ability to fully assess the impact of GERD on neonatal outcomes.
The incidence of GERD in full-term mechanically ventilated neonates is high, with significant associations between pepsin levels, FiO2, feeding intolerance, and prolonged hospital stay. Early detection of GER through pepsin measurement may guide clinical interventions to improve neonatal outcomes.
The authors would like to express their gratitude to the medical and nursing staff of the NICU at Cairo University Hospitals for their valuable support in patient care and data collection. We also extend our appreciation to the Clinical and Chemical Pathology Department for their assistance in laboratory analysis. Finally, we acknowledge the parents and guardians of the neonates who participated in this study for their cooperation and trust.
| 1. | Gulati IK, Jadcherla SR. Gastroesophageal Reflux Disease in the Neonatal Intensive Care Unit Infant: Who Needs to Be Treated and What Approach Is Beneficial? Pediatr Clin North Am. 2019;66:461-473. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 2. | Ho T, Dukhovny D, Zupancic JA, Goldmann DA, Horbar JD, Pursley DM. Choosing Wisely in Newborn Medicine: Five Opportunities to Increase Value. Pediatrics. 2015;136:e482-e489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 120] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 3. | Sawyer C, Sanghavi R, Ortigoza EB. Neonatal gastroesophageal reflux. Early Hum Dev. 2022;171:105600. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 4. | Welsh C, Pan J, Belik J. Caffeine impairs gastrointestinal function in newborn rats. Pediatr Res. 2015;78:24-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Farhath S, Aghai ZH, Nakhla T, Saslow J, He Z, Soundar S, Mehta DI. Pepsin, a reliable marker of gastric aspiration, is frequently detected in tracheal aspirates from premature ventilated neonates: relationship with feeding and methylxanthine therapy. J Pediatr Gastroenterol Nutr. 2006;43:336-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 46] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 6. | Sanchez JB, Jadcherla SR. Gastroesophageal Reflux Disease in Neonates: Facts and Figures. Neoreviews. 2021;22:e104-e117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Ufberg JW, Bushra JS, Patel D, Wong E, Karras DJ, Kueppers F. A new pepsin assay to detect pulmonary aspiration of gastric contents among newly intubated patients. Am J Emerg Med. 2004;22:612-614. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Metheny NA, Dahms TE, Chang YH, Stewart BJ, Frank PA, Clouse RE. Detection of pepsin in tracheal secretions after forced small-volume aspirations of gastric juice. JPEN J Parenter Enteral Nutr. 2004;28:79-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 1.5] [Reference Citation Analysis (1)] |
| 9. | Gonzalez Ayerbe JI, Hauser B, Salvatore S, Vandenplas Y. Diagnosis and Management of Gastroesophageal Reflux Disease in Infants and Children: from Guidelines to Clinical Practice. Pediatr Gastroenterol Hepatol Nutr. 2019;22:107-121. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 36] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 10. | Garland JS, Alex CP, Johnston N, Yan JC, Werlin SL. Association between tracheal pepsin, a reliable marker of gastric aspiration, and head of bed elevation among ventilated neonates. J Neonatal Perinatal Med. 2014;7:185-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 11. | Czinn SJ, Blanchard S. Gastroesophageal reflux disease in neonates and infants : when and how to treat. Paediatr Drugs. 2013;15:19-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 84] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 12. | Dahlen HG, Foster JP, Psaila K, Spence K, Badawi N, Fowler C, Schmied V, Thornton C. Gastro-oesophageal reflux: a mixed methods study of infants admitted to hospital in the first 12 months following birth in NSW (2000-2011). BMC Pediatr. 2018;18:30. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 2.7] [Reference Citation Analysis (0)] |