Published online Dec 18, 2016. doi: 10.5312/wjo.v7.i12.808
Peer-review started: June 17, 2016
First decision: July 29, 2016
Revised: August 9, 2016
Accepted: October 1, 2016
Article in press: October 3, 2016
Published online: December 18, 2016
Processing time: 179 Days and 14.6 Hours
To investigate whether autologous blood transfusion (ABT) drains and intra-operative cell salvage reduced donor blood transfusion requirements during scoliosis surgery.
Retrospective data collection on transfusion requirements of patients undergoing scoliosis surgery is between January 2006 and March 2010. There were three distinct phases of transfusion practice over this time: Group A received “traditional treatment” with allogeneic red cell transfusion (ARCT) in response to an intra- or post-operative anaemia (Hb < 8 g/dL or a symptomatic anaemia); Group B received intra-operative cell salvage in addition to “traditional treatment”. In group C, ABT wound drains were used together with both intra-operative cell salvage and “traditional treatment”.
Data from 97 procedures on 77 patients, there was no difference in mean preoperative haemoglobin levels between the groups (A: 13.1 g/dL; B: 13.49 g/dL; C: 13.66 g/dL). Allogeneic red cell transfusion was required for 22 of the 37 procedures (59%) in group A, 17 of 30 (57%) in group B and 16 of 30 (53%) in group C. There was an overall 6% reduction in the proportion of patients requiring an ARCT between groups A and C but this was not statistically significant (χ2 = 0.398). Patients in group C received fewer units (mean 2.19) than group B (mean 2.94) (P = 0.984) and significantly fewer than those in group A (mean 3.82) (P = 0.0322). Mean length of inpatient stay was lower in group C (8.65 d) than in groups B (12.83) or A (12.62).
When used alongside measures to minimise blood loss during surgery, ABT drains and intra-operative cell salvage leads to a reduced need for donor blood transfusion in patients undergoing scoliosis surgery.
Core tip: To our knowledge this is the first report of autologous blood transfusion (ABT) drain use in scoliosis surgery and suggests that its use is both safe and cost effective. When used as part of a systematic programme to minimise blood loss during surgery, the use of ABT drains and intra-operative cell salvage leads to a reduced need for donor blood transfusion in patients undergoing scoliosis surgery.
- Citation: Loughenbury PR, Berry L, Brooke BT, Rao AS, Dunsmuir RA, Millner PA. Benefits of the use of blood conservation in scoliosis surgery. World J Orthop 2016; 7(12): 808-813
- URL: https://www.wjgnet.com/2218-5836/full/v7/i12/808.htm
- DOI: https://dx.doi.org/10.5312/wjo.v7.i12.808
Autologous blood reinfusion techniques have become commonplace in many fields of orthopaedic surgery, especially in hip and knee arthroplasty[1,2]. These techniques can reduce the need for donor blood and the risks that accompany its use, such as incorrect blood component transfused, transfusion reactions, viral/prion disease transmission, and the metabolic and immunological consequences of tranfusing allogeneic blood[3].
The use of autologous blood reinfusion in spinal surgery is less commonly reported. Intra-operative cell salvage has been associated with reduced transfusion requirements in scoliosis surgery[4,5], but the use of post-operative reinfusion devices is not well documented. Reports are limited to short segment spinal fusion and have not included corrective surgery to treat scoliosis[6]. This study was designed to determine the effect of sequentially introducing intra-operative cell salvage and post-operative autologous blood transfusion (ABT) drains in scoliosis surgery. These were used alongside a number of efforts to reduce the need for allogeneic red cell transfusion (ARCT) during scoliosis surgery including a move from two-stage (anterior and posterior) surgery to a single stage (posterior) technique, and measures such as optimisation of pre-surgical haemoglobin levels, oral iron supplements and the antifibrinolytic drug tranexamic acid.
This study aimed: To examine the impact of using ABT drains and intra-operative cell salvage on the allogeneic transfusion requirements for scoliosis surgery in our unit; to evaluate the volume of blood drained and re-transfused using ABT drains.
This is a retrospective analysis of all patients undergoing surgery for scoliosis in a single centre between January 2006 and March 2010. All patients undergoing corrective scoliosis surgery were included, including revision procedures. Patients under the age of six were excluded, as autologous re-transfusion systems are not recommended for use below this age.
Data was collected from the patient case notes, the transfusion laboratory database and the hospital results server. A data collection form was developed and completed by either the Transfusion Practitioner or Specialist Registrar working in the unit. Patient demographics, details of any preoperative optimisation required, pre- and post-operative haemoglobin levels, donor and autologous transfusion requirements, length of hospital stay and post-operative complications were documented.
The transfusion trigger remained constant across the series. An intra- or post-operative anaemia (Hb < 8 g/dL) or symptomatic anaemia initiated treatment with ARCT. The volume and timing of these transfusions was recorded.
Over this time period there were three distinct phases of transfusion practice: (1) Group A: January to December 2006: “Traditional treatment”: These patients received ARCT in response to the transfusion trigger. No autologous blood was transfused (n = 37); (2) Group B: January to December 2007. Intra-operative cell salvage was implemented using the Sorin Dideco (Sorin Group, Mirandola, Italy) system (n = 30); (3) Group C: January 2008 to March 2010. In addition to intra-operative cell salvage a Bellovac™ (Astra Tech, AB) autologous blood transfusion wound drain was used. Blood collected in the Bellovac™ (Astra Tech) drain was reinfused in accordance with manufacturers guidelines within 6 h of the procedure. The volume of blood collected and reinfused was recorded using the Bellovac™ ABT Management chart provided with the drain (n = 30).
Administration of pharmacological agents, such as tranexamic acid, was led by the Consultant Anaesthetist for the case, with no standard guidelines. The doses of any preoperative antifibrinolytics were therefore variable, but were recorded for all patients.
Statistical analysis was carried out using Microsoft Excel. χ2 tests were used to determine the significance of changes in the proportion of patients requiring an ARCT and produce a two-tailed P value of significance. Where means are compared a paired t-test was used.
Data was collected for 97 procedures on 77 patients between January 2006 and March 2010. Median age of patients was 15 (range 8-74). Group A (January 2006 to December 2006) contained 37 procedures with a median patient age of 15 (range 8-33); group B (January 2007 to December 2007) contained 30 procedures with a median patient age of 16 (range 9-57) and group C (January 2008 to March 2010) contained 30 procedures with a median patient age of 15 (range 11-74). The case mix in each group is detailed in Table 1.
| Group | n | Median age (range) | Case mix |
| A | 37 | 15 (8-33) | 8 posterior |
| 3 anterior | |||
| 12 anterior/posterior staged | |||
| 2 anterior/posterior combined | |||
| B | 30 | 16 (9-57) | 8 posterior |
| 3 anterior | |||
| 6 anterior/posterior staged | |||
| 7 anterior/posterior combined | |||
| C | 30 | 15 (11-74) | 22 posterior |
| 1 anterior | |||
| 2 anterior/posterior | |||
| 3 anterior/posterior combined |
There was no difference in the mean preoperative haemoglobin level. The mean preoperative haemoglobin was 13.09 g/dL (95%CI: 12.60-13.58) in group A, 13.49 g/dL (95%CI: 12.89-14.08) in group B and 13.66 g/dL (95%CI: 13.19-14.13) in group C.
In group A one patient received a 50 mg dose of tranexamic acid before surgery but no other patients received antifibrinolytic therapy. No patients in group B received antifibrinolytic therapy. In group C, 9 out of 30 patients (30%) were given tranexamic acid before surgery with the dose varying from 350 mg to 1 g. There were no patients in any group taking antiplatelet medication or other agents that would increase bleeding risk.
Patients in group A did not receive any autologous blood. Those in group B received intra-operative transfusion of blood collected through the cell saver. The mean volume of blood reinfused was 413.4 mL (SD 287.34 mL). There were technical problems that interrupted reinfusion in 4 out of 30 cases.
Patients in group C received autologous blood from both the cell saver and ABT drains. Intraoperative cell-salvage was used successfully during 26 out of 30 procedures (87%). Technical problems or insufficient volume collected prevented reinfusion in the remaining four cases. The mean volume of cell saver blood reinfused was 525.4 mL (SD 302.96 mL). ABT drains were used successfully in 28 out of 30 cases. Technical problems and unavailability of equipment prevented reinfusion in the other two cases. The mean volume of blood received through the ABT drain was 442 mL (SD 169.38 mL).
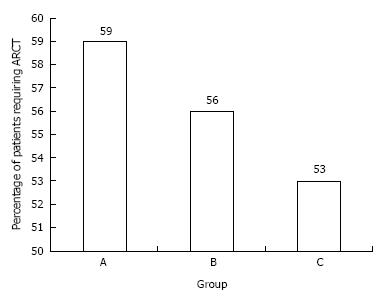
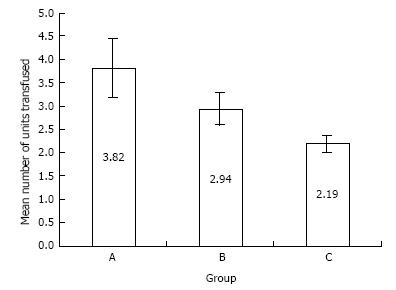
A comparison of the ARCT requirements in groups A, B and C is shown in Table 2 and Figures 1 and 2.
| Group | Proportion requiring ARCT | Total number of units received | Mean ARCT (standard deviation) |
| A | 22/37 (59%) | 84 (73 units packed red cells, 8 units fresh frozen plasma, 2 units of cryoprecipitate and one unit of platelets | 3.82 units (3.79) |
| B | 17/30 (57%) | 50 units packed red cells | 2.94 units (1.82) |
| C | 16/30 (53%) | 37 units packed red cells | 2.19 units (0.91) |
There was an overall 6% reduction in the proportion of patients requiring an ARCT between groups A and C (Figure 1) but this was not statistically significant (χ2 = 0.398). The percentage of patients receiving an ARCT fell from 59% in group A to 56% in group B (not significant; χ2 = 0.068) and 53% in group C (not significant; χ2 = 0.134).
In patients requiring allogeneic transfusion, the mean number of units transfused fell from 3.82 units (SD 3.79) in group A to 2.94 (SD 1.82) in group B (not significant; P = 0.894) and 2.19 units (SD 0.91) in group C (not significant; P = 0.0843). However, the reduction in the mean number of allogeneic units transfused in groups A and C was statistically significant: - 3.82 units in group A to 2.19 units in group C (Figure 2; P = 0.0322). There was no difference in ARCT requirements when comparing primary and revision procedures.
A reduction in the length of hospital stay between the groups was also noted. The mean length of stay was 12.62 d (range 8-21) in group A, 12.83 d (range 6-31) in group B and 8.65 d (range 5-23) in group C.
There were no complications relating to allogeneic or autologous transfusion in groups A and B. One patient in group C developed a pyrexia of unknown origin following surgery but this settled without the need for medical intervention. This patient received reinfused blood through the ABT drain but not the cell saver and did not receive any allogeneic blood. There were no other complications in group C.
As part of an integrated blood conservation programme, autologous blood reinfusion can reduce the need for, and the potential complications of, donor blood transfusion. These include transfusion of incorrect blood components, transfusion reactions, viral/prion disease transmission, coagulopathy, and the metabolic and immunological consequences of tranfusing allogeneic blood[3].
Autologous blood reinfusion in the form of cell salvage has become commonplace in many fields of orthopaedic surgery[1,2]. Its use in other adult elective orthopaedic procedures has been shown to reduce the rate of exposure to allogeneic red cell transfusion (RR = 0.42; 95%CI: 0.32-0.54)[7]. In adult spinal surgery, transfusion requirements in both elective surgery and operative fracture fixation are significantly lower when cell salvage is used[1]. The benefits of cell salvage in scoliosis surgery are less clear, but have been reported in both posterior and anterior scoliosis surgery[4,8]. In their retrospective case-controlled study of 137 consecutive patients, Mirza et al[8] underlined the benefits of cell salvage in instrumented anterior scoliosis surgery. The need for allogeneic blood fell from 39.4% in the control group (n = 33) to 6.7% in the study group (n = 104) (P < 0.0001). Bowen et al[4] reported a retrospective case control study in which the routine use of the cell saver during posterior spinal fusion for paediatric idiopathic scoliosis, was associated with decreased allogeneic transfusion rates, particularly for procedures lasting over 6 h and where expected blood loss was over 30% of blood volume.
The use of ABT drains has also become more popular in orthopaedic procedures over the last ten years. Post-operative collection and reinfusion of red cells has been shown to reduce the need for donor blood transfusion in both knee and hip arthroplasty[9,10]. In spinal surgery, re-transfusion drains have been shown to be safe and reduce the need for donor blood during short segment fusion in adults[6]. The use of ABT drains in scoliosis surgery has not previously been reported.
In our study both cell salvage and ABT drains were sequentially introduced and lead to a modest, but not statistically significant, reduction in the percentage of patients receiving an allogeneic transfusion. However, those patients who were transfused were exposed to significantly fewer allogeneic units (donor exposures), falling from 3.82 to 2.19 units when both intraoperative cell salvage and ABT drains were used.
In common with all retrospective studies, it is impossible to adjust for all confounders, both known and unknown. The reduction in donor blood exposure we achieved occurred alongside a number of other changes to minimise blood loss during surgery during the study period. There was a trend towards less invasive surgical procedures in groups B and C, partly due to changes in the implant systems used which provided a greater ability to achieve an adequate curve correction using a single stage posterior procedure. There was also a trend towards an increased use of antifibrinolytics in group C (30% of whom received tranexamic acid), and there is good evidence that this can lead to lower transfusion rates in paediatric scoliosis surgery[11].
In the absence of randomised controlled trials, the results of retrospective series, such as this, must be interpreted with caution. However, the methods described were found to be safe and practical in routine practice and contributed to a clinically and financially worthwhile reduction in the use of donor red cells.
We also observed a fall in the length of inpatient hospital stay in patients in group C. This is probably multifactorial, including changes to surgical practice that lead to earlier postoperative mobilisation and discharge. However, changes in transfusion practice may have contributed as several previous studies have reported reduced length of hospital stay in orthopaedic patients exposed to less donor blood[12].
There is good evidence to suggest that cell salvage is a cost effective method to reduce the need for donor blood transfusion[13]. A cost analysis of the data presented in our study is detailed in Table 3. This confirms that the use of cell salvage alone and the use of cell salvage with ABT drains was cost neutral in our study.
| Group A donor blood only | Group B cell salvage | Group C cell salvage + ABT drain | |
| Number of RBC units transfused | 84 | 50 | 37 |
| Total cost of RBC transfusion (£) | 10416 | 6200 | 4588 |
| Number of patients receiving cell salvage | 0 | 30 | 30 |
| Total cost of cell Salvage (£) | 0 | 2100 | 2100 |
| Number of patients receiving ABT drains | 0 | 0 | 30 |
| Total cost of ABT drains (£) | 0 | 0 | 1620 |
| Overall transfusion cost | 10416 | 8300 | 8308 |
| Number of patients | 37 | 30 | 30 |
| Overall cost per patient (£) | 281.51 | 276.67 | 276.93 |
In conclusion, to our knowledge this is the first report of ABT drain use in scoliosis surgery and suggests that its use is both safe and cost effective. When used as part of a systematic programme to minimise blood loss during surgery, the use of ABT drains and intra-operative cell salvage lead to a reduced need for donor blood transfusion in patients undergoing scoliosis surgery in our unit. The lowest donor blood transfusion rates were seen when both modalities were used, leading to a 6% reduction in the number of donor transfusion episodes and a significant reduction in the mean units of red cells transfused per episode (2.19 compared to 3.82). The programme proved practical and cost-effective to implement in a busy surgical unit.
Autologous blood reinfusion techniques have become commonplace in many fields of orthopaedic surgery, especially in hip and knee arthroplasty. These techniques can reduce the need for donor blood and the risks that accompany its use.
Intra-operative cell salvage has been associated with reduced transfusion requirements in scoliosis surgery, but the use of post-operative reinfusion devices is not well documented.
To the authors’ knowledge this is the first report of autologous blood transfusion (ABT) drain use in scoliosis surgery and suggests that its use is both safe and cost effective.
When used as part of a systematic programme to minimise blood loss during surgery, the use of ABT drains and intra-operative cell salvage can reduce the need for donor blood transfusion in patients undergoing scoliosis surgery.
ABT and allogeneic red cell transfusion.
This is a case control study reporting the use of ABT drains in scoliosis surgery and suggests that its use is both safe and cost effective. When used as part of a systematic programme to minimise blood loss during surgery, ABT drains and intra-operative cell salvage lead to a significantly reduced need for donor blood transfusion in patients undergoing scoliosis surgery.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: United Kingdom
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Erkan S, Luo XH, Jain A S- Editor: Qiu S L- Editor: A E- Editor: Lu YJ
| 1. | Goulet JA, Bray TJ, Timmerman LA, Benson DR, Bargar WL. Intraoperative autologous transfusion in orthopaedic patients. J Bone Joint Surg Am. 1989;71:3-8. [PubMed] |
| 2. | Huët C, Salmi LR, Fergusson D, Koopman-van Gemert AW, Rubens F, Laupacis A. A meta-analysis of the effectiveness of cell salvage to minimize perioperative allogeneic blood transfusion in cardiac and orthopedic surgery. International Study of Perioperative Transfusion (ISPOT) Investigators. Anesth Analg. 1999;89:861-869. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 169] [Cited by in RCA: 141] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 3. | Bolton-Maggs PH. Conference report: the 2015 SHOT symposium and report--what’s new? Transfus Med. 2015;25:295-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 4. | Bowen RE, Gardner S, Scaduto AA, Eagan M, Beckstead J. Efficacy of intraoperative cell salvage systems in pediatric idiopathic scoliosis patients undergoing posterior spinal fusion with segmental spinal instrumentation. Spine (Phila Pa 1976). 2010;35:246-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 88] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 5. | Weiss JM, Skaggs D, Tanner J, Tolo V. Cell Saver: is it beneficial in scoliosis surgery? J Child Orthop. 2007;1:221-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 33] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Sebastián C, Romero R, Olalla E, Ferrer C, García-Vallejo JJ, Muñoz M. Postoperative blood salvage and reinfusion in spinal surgery: blood quality, effectiveness and impact on patient blood parameters. Eur Spine J. 2000;9:458-465. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 42] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 7. | Carless PA, Henry DA, Moxey AJ, O’Connell DL, Fergusson DA. Cell salvage for minimising perioperative allogeneic blood transfusion. Cochrane Database Syst Rev. 2003;CD001888. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 49] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 8. | Mirza AH, Aldlyami E, Bhimarasetty C, Thompson AG, Spilsbury J, Marks DS. The role of peri-operative cell salvage in instrumented anterior correction of thoracolumbar scoliosis: a case-controlled study. Acta Orthop Belg. 2009;75:87-93. [PubMed] |
| 9. | Peter VK, Radford M, Matthews MG. Re-transfusion of autologous blood from wound drains: the means for reducing transfusion requirements in total knee arthroplasty. Knee. 2001;8:321-323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Smith LK, Williams DH, Langkamer VG. Post-operative blood salvage with autologous retransfusion in primary total hip replacement. J Bone Joint Surg Br. 2007;89:1092-1097. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 31] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 11. | Grant JA, Howard J, Luntley J, Harder J, Aleissa S, Parsons D. Perioperative blood transfusion requirements in pediatric scoliosis surgery: the efficacy of tranexamic acid. J Pediatr Orthop. 2009;29:300-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 78] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 12. | Jans Ø, Kehlet H, Hussain Z, Johansson PI. Transfusion practice in hip arthroplasty--a nationwide study. Vox Sang. 2011;100:374-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 13. | Haynes S, Payne K, Elliott RA, McCollum C. Cost-effectiveness of cell salvage and alternative methods of minimising perioperative allogeneic blood transfusion: a systematic review and economic model. Davies L, Brown TJ, editors. Winchester, England: Health Technology Assessment 2006; iii-iv, ix-x, 1-210. |