Published online Nov 28, 2013. doi: 10.4329/wjr.v5.i11.446
Revised: October 6, 2013
Accepted: October 17, 2013
Published online: November 28, 2013
Processing time: 113 Days and 13 Hours
The authors report on a case of benign myolipoma (synonym lipoleiomyoma) which was first described in 1991. The benign soft tissue tumor is composed of smooth muscle and adipose tissue and occurs sporadically in different locations. In the available literature cases were described retroperitoneal, spinal, orbital and subcutaneous and mostly have been discovered in females. Characteristically myolipomas are very large at diagnosis and reach diameters of 7 to 30 cm particularly in peritoneal or retroperitoneal localization. The sometimes enormous size leads to a displacing growth pattern which ultimately leads to the clinical symptoms. The patients often complain of nonspecific, mostly painless abdominal or thoracic pressure. Bordered by an intact capsule the tumors show no signs of malignancy and in the available literature there is no evidence of metastatic seeding. To the best of our knowledge the presented case is the first description of a diffuse mesenteric myolipoma in a male individual. In this article, we present the multidetector computed tomographic image characteristics, macroscopic appearance and histopathological findings.
Core tip: Benign myolipoma, first described in 1991, is a benign soft tissue tumor which is composed of smooth muscle and adipose tissue and occurs sporadically in different locations. Particularly in peritoneal or retroperitoneal localization myolipomas are very large at diagnosis. The authors report for the first time of a diffuse mesenterial myolipoma in a male individual. Radiographic image characteristics based on computed tomography and macro- and histopathologic findings are presented and discussed.
- Citation: Maataoui A, Khan FM, Vogl TJ, Erler A. Mesenteric myolipoma. World J Radiol 2013; 5(11): 446-449
- URL: https://www.wjgnet.com/1949-8470/full/v5/i11/446.htm
- DOI: https://dx.doi.org/10.4329/wjr.v5.i11.446
Lipoleiomyoma usually occurs within the abdominal cavity and retroperitoneum, although it may also be found in subcutaneous location[1]. These tumors show characteristic histologic findings, being composed of mature adipose tissue and benign smooth muscle. There is no reported case of recurrence or metastasis, suggesting that complete surgical excision is curative. We report of a diffuse mesenteric myolipoma in a male individual. To the best of our knowledge the presented case is the first description of a diffuse mesenteric myolipoma in a male individual.
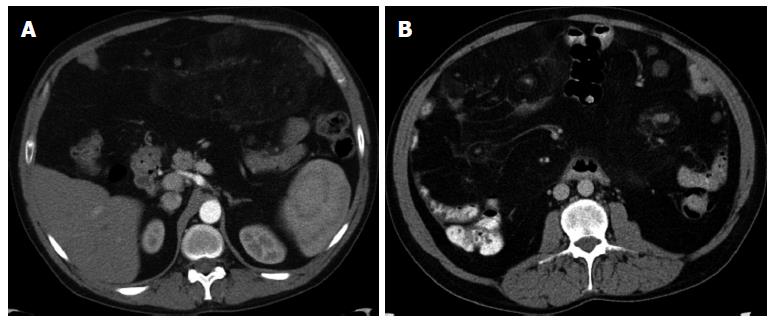
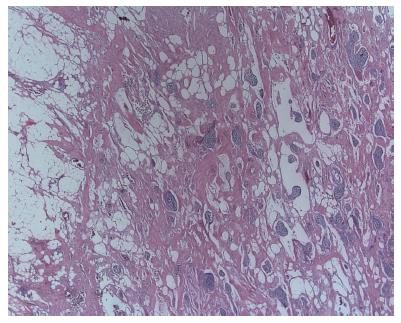
A 48-year-old patient without pre-existing condition presented with recently progressive dyspnea, chest pain and persistent abdominal bloating to the medical unit of our hospital. Multidetector computed tomography (MDCT) of the chest was performed to exclude the possibility of acute pulmonary embolism While thoracic findings were unremarkable, a mesenteric mass was detected in the upper abdominal cuts.. The mass measured 10 cm × 19 cm in its axial orientation (Figure 1A). It was mainly composed of adipose tissue with nodular lesions of soft-tissue-equivalent density. Abdominal MDCT examination was followed to further characterize the lesion. Therein, the lesion showed a diffuse pattern of spread along the entire mesentery (Figure 1B), occupying the whole abdomen down to the pelvis. In correlation with the already described findings tumor stroma showed multiple nodular lesions with soft-tissue-equivalent density, measuring up to 6 cm × 5 cm sometimes with peripheral calcifications. The mass exerted a mass effect displacing the bowel loops to the abdominal wall with separation of the mesenteric vessels. There was no infiltrative growth pattern and the solid abdominal organs were normal. Due to the morphologic findings benign and malignant tumors of adipose tissue were discussed as possible differential diagnoses. Because of the massive lesion and for further histological assessment laparotomy was performed (Figure 2). Intraoperatively the large tumor formation of the entire mesentery displaced all visceral organs to the abdominal wall. There were multiple irregular areas of necrosis within the lesion. Since the mass occupied the full width and depth of the mesentery, complete resection with consecutive loss of the entire small intestine was not possible. Three tumor bulks, each of them weighting approximately 4 kg, were removed including en-bloc resection of 1 m of small intestine in order to reduce tumor volume. The resected tumors were of elastic consistency and showed smooth margins with an intact peritoneal coverage. The cutting surface showed a dirty-yellow and grey-white color with focal areas of necrosis. The resected small bowel segment was narrowed but not obstructed (Figure 3). Hematoxylin-eosin staining revealed the presence of adipocytes without evidence of atypical cells and only little variations in size, as well as enclosed nests of spindle cells and thin walled, partly ectatic vessels (Figure 4).
Histopathologically the tumor was composed of 70% fat, 25% spindle cells and 5% vascular structures. Immunohistochemically the spindle cells were positive for actin, desmin, and vimentin, thus had characteristics of highly differentiated smooth muscle cells without evidence of mitoses or cellular atypia. The vascular structures were positive for CD34 and negative for D2-40, thus were characterized as blood vessels. In the comparative genomic hybridization (CGH-analysis) the tumor showed no gains or losses of DNA, according to a normal male karyotype. In summary, due to the three tumor components, lack of malignancy as well as the exclusion of melanocytic differentiation a benign mesenteric myolipoma was diagnosed. The diagnosis was confirmed by a histopathological reference center for soft tissue tumors.
Myolipoma is a rare benign tumor that occurs sporadically in different location. Meis and Enzinger[1] first described the tumor entity in 9 individuals. They found the majority of lesions in a retroperitoneal location. Less commonly the tumors were localized inguinal, peritoneal, subcutaneous or intramuscular. Following this first description 26 other case reports dealing with myolipoma were published until today-most of them report on female patients[2-13]. Characteristically myolipomas are very large at diagnosis and reach diameters of 7 to 30 cm[2,4-6] particularly in peritoneal or retroperitoneal localization. The sometimes enormous size leads to a displacing growth pattern which ultimately leads to the clinical symptoms. The patients often complain of nonspecific, mostly painless abdominal or thoracic pressure. On the other hand, if the lesion is located subcutaneously[7] or in other confined compartments[5] it becomes clinically symptomatic early and thus reaches significantly smaller diameters. Bordered by an intact capsule the lesions don’t show infiltrating growth characteristics into the adjacent anatomical compartments. The internal structure of the tumor is composed of highly differentiated smooth muscle and adipose tissue. Histopathologically, the tumors show no signs of malignancy. The lack of malignancy and a usually existing tumor capsule allows a curative surgical approach that provides a recurrence-free posttherapeutic course. In the available literature there is no evidence of malignant transformation or metastatic seeding of myolipomas. The radiological assessment of the lesions is mainly based on the computed tomography (CT) and magnetic resonance imaging. According to the macroscopic appearance and histopathological composition of myolipomas, the tumor shows fat or soft-tissue-attenuation or signal intensities, respectively. In the majority of cases a direct visualization of the tumor capsule is possible. There is neither significant contrast enhancement nor pathologically detectable lymph nodes. A clear differentiation between benign differential diagnoses such as spindle-cell lipoma and fatty-degenerated leiomyoma from well-differentiated liposarcoma remains difficult on the bases of imaging characteristics alone, thus histopathological assessment is necessary.
In comparison to previous reports the presented case of a myolipoma shows particular features. In the majority of cases a preferred occurrence in females is described, but retro- and intraperitoneal localizations are documented exclusively in women. In the presented case we report on a male patient in whom the tumor was localized in the mesentery and showed a diffuse expansion. Remarkably the tumor showed multiple, partially calcified tissue-islets, which were identified as focal areasis of necrosis in the macroscopic appearance and histopathological evaluation. Since the occurrence of necrosis was previously not associated with myolipoma, the differential diagnosis of a highly differentiated liposarcamo was favored initially. Despite a visible tumor capsule, the diffuse growth-pattern made a complete resection with consecutive loss of the complete small intestine, impossible. To reduce tumor volume a partial debulking of the tumor was performed resulting in marked improvement in clinical symptomatics of the patient. Because of the incomplete resection CT follow-up examinations are performed at regular intervals, which so far showed no evidence of recurrence.
P- Reviewers: Ciaccio EJ, Eghtesad B, Refaat R, Yen HH S- Editor: Gou SX L- Editor: A E- Editor: Liu XM
| 1. | Meis JM, Enzinger FM. Myolipoma of soft tissue. Am J Surg Pathol. 1991;15:121-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 61] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 2. | Ulu EM, Kirbaş I, Töre HG, Başaran C, Oztürk A, Güven G, Karadeli E, Coşkun M. Extraperitoneal pelvic myolipoma. Diagn Interv Radiol. 2010;16:227-231. [PubMed] |
| 3. | Michal M. Retroperitoneal myolipoma. A tumour mimicking retroperitoneal angiomyolipoma and liposarcoma with myosarcomatous differentiation. Histopathology. 1994;25:86-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 15] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Oh MH, Cho IC, Kang YI, Kim CY, Kim DS, Cho HD, Kim HK. A case of retroperitoneal lipoleiomyoma. J Korean Med Sci. 2001;16:250-252. [PubMed] |
| 5. | Takahashi Y, Imamura T, Irie H, Tanaka F, Fukushima J, Fukusato T, Harasawa A, Shiga J. Myolipoma of the retroperitoneum. Pathol Int. 2004;54:460-463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 17] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Behranwala KA, Chettiar K, El-Bahrawy M, Stamp G, Kakkar AK. Retroperitoneal myolipoma. World J Surg Oncol. 2005;3:72. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Lee YS, Park SE, Lee JU, Choi ES. MRI of a subcutaneous myolipoma in the ankle: a case report. Korean J Radiol. 2011;12:641-645. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Sharara N, Lee WR, Weir C. Myolipoma of the eyelid. Graefes Arch Clin Exp Ophthalmol. 1998;236:630-634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Takahashi H, Tomita Y, Yagishita A, Oda M. Sacral intradural myolipoma causing tethered cord syndrome. J Clin Neurosci. 1998;5:450-453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Brown PG, Shaver EG. Myolipoma in a tethered cord. Case report and review of the literature. J Neurosurg. 2000;92:214-216. [PubMed] |
| 11. | Fernández-Aguilar S, Saint-Aubain N, Dargent JL, Fayt I, Noel JC. Myolipoma of soft tissue: an unusual tumor with expression of estrogen and progesterone receptors. Report of two cases and review of the literature. Acta Obstet Gynecol Scand. 2002;81:1088-1090. [PubMed] |
| 12. | McGregor DK, Whitman GJ, Middleton LP. Myolipoma of the breast: mammographic, sonographic, and pathologic correlation. Breast J. 2004;10:259-260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Parratt MT, Gokaraju K, Spiegelberg BG, Miles J, Cannon SR, Briggs TW. Myolipoma affecting the erector spinae: a case report in a child. Case Rep Med. 2009;2009:520126. [PubMed] |