Published online Jun 28, 2025. doi: 10.4329/wjr.v17.i6.107164
Revised: April 12, 2025
Accepted: May 21, 2025
Published online: June 28, 2025
Processing time: 101 Days and 18.9 Hours
Back pain and sciatica are common complaints that often require imaging for accurate diagnosis and management. Conventional lumbar magnetic resonance imaging (MRI) protocols typically include sagittal and axial T1 and T2 sequences; however, these may miss certain pathologies. The addition of coronal short tau inversion recovery (STIR) sequences offers the potential to enhance the detection of both spinal and extra-spinal abnormalities, thereby improving clinical decision-making and patient outcomes.
To evaluate the impact of adding coronal STIR sequences to routine lumbar MRI in diagnosing back pain and sciatica.
We prospectively analyzed data from patients aged 6 and older presenting with back pain or sciatica who underwent lumbar spine MRI at our institution. The standardized MRI protocol utilized included sagittal and axial T1 and T2 se
Our cohort comprised 274 patients (115 males, 159 females; mean age 44.91 years). Notably, 39 patients exhibited abnormalities across all sequences, while 72.63% showed normal findings on the coronal STIR sequence. Impor
Integrating coronal STIR into routine lumbar MRI enhances detection of hidden spinal and extra-spinal patho
Core Tip: Incorporating a coronal short tau inversion recovery sequence into routine lumbar magnetic resonance imaging protocols significantly enhances diagnostic accuracy for patients with back pain and sciatica. This sequence improves the detection of spinal and extra-spinal pathologies - especially sacroiliitis and pelvic abnormalities - that may be missed on standard axial and sagittal T1 and T2 sequences. Our findings support the integration of coronal short tau inversion recovery as a cost-effective, practical addition that can meaningfully influence diagnosis and clinical management.
- Citation: Al Kiswani S, Nasser M, Alzibdeh A, Lahham EE. Enhancing back pain and sciatica diagnosis: Coronal short tau inversion recovery’s role in routine lumbar magnetic resonance imaging protocols. World J Radiol 2025; 17(6): 107164
- URL: https://www.wjgnet.com/1949-8470/full/v17/i6/107164.htm
- DOI: https://dx.doi.org/10.4329/wjr.v17.i6.107164
Low back pain is linked to considerable morbidity, contributing to around 850 years lived with disability in Jordan in 2021, according to data from the Global Burden of Disease Study, 2021[1]. Back pain is one of the most common reasons for performing routine lumbar magnetic resonance imaging (MRI), which include T1-weighted, T2-weighted, and fat-suppressed fluid-sensitive sequences in both the sagittal and axial planes[2-4]. The protocol can also include transverse plane images focused on intervertebral levels with structural abnormalities identified in the sagittal view. Although sagit
This standard protocol effectively identifies common causes of back pain and sciatica, such as disc prolapse, yet may miss extra-spinal causes. Incorporating a coronal STIR sequence can enhance the detection of conditions outside the spine, such as sacroiliac, hip joint, and abdominopelvic pathologies[7]. The STIR sequence in MRI is designed to suppress fat signals, enhancing the visibility of certain pathologies like edema or inflammation[8]. Based on findings from previous studies and our experience, we began incorporating coronal STIR sequences into our lumbar spine MRI protocol for patients with back pain or sciatica, especially when standard sequences yield inconclusive results. This addition provides a broader view of the abdominal and pelvic regions, allowing assessment of sacroiliac, hip joints, and abdominopelvic organs, which may contribute to the patient’s symptoms. This study aims to evaluate the impact of adding coronal STIR imaging to routine lumbar MRI, focusing on its potential to uncover hidden causes and improve diagnostic accuracy for back pain and sciatica.
This study followed ethical standards and received approval from the institutional review board. All patient data were handled in compliance with confidentiality regulations.
This study evaluated prospectively collected data from patients presenting with back pain and sciatica who underwent lumbar spine MRI. Patient medical records and imaging data were reviewed to identify findings relevant to the study’s aim.
The study included patients aged 6 or above who reported back pain and sciatica as primary complaints and underwent a lumbar spine MRI at our hospital to identify potential underlying pathologies.
All participants underwent a standardized MRI protocol on a GE Signa HD 1.5T MRI System. The routine protocol included sagittal and axial T1- and T2-weighted sequences, with an additional coronal STIR sequence. These sequences provided a detailed evaluation of the spine and surrounding structures to detect abnormalities potentially related to back pain.
Lumbosacral MRI protocol including: (1) Sagittal T2-weighted imaging: Echo time (TE): 102 milliseconds, repetition time (TR): 2584 milliseconds, slice thickness: 4 mm, FOV: 30 cm; (2) Sagittal T1-weighted imaging: TE: Minute full, TR: 584 milliseconds, slice thickness: 4 mm, FOV: 30 cm; (3) Axial T2-weighted imaging: TE: 110 milliseconds, TR: 2600 millise
TE: 50 milliseconds, TR: 4050 milliseconds, slice thickness: 5 mm, FOV: 48 cm.
Data were prospectively gathered from observations across the T1/T2 axial and coronal STIR sequences, with a focus on structural abnormalities and variations. An experienced radiologist reviewed the images to confirm these findings.
The collected findings from the MRI scans, encompassing abnormalities and structural variations observed in the T1/T2 axial sequences and the coronal STIR sequence, were summarized as counts and percentages. A Fisher’s exact test was performed to assess the significance of differences observed between categorical variables. Statistical analysis was con
Our sample included all the patients who underwent spine MRI for evaluation of low back pain at our hospital. 115 male and 159 female patients with a mean age of 44.91 years (range 6-92 years) were included. The most common findings on T1 and T2 sequences, as well as coronal STIR sequences, are evident in Table 1. 39 patients showed abnormalities in all T1, T2, and coronal STIR sequences. Most of the cases (72.63%) had normal findings on the coronal STIR sequence. Without using coronal STIR, MRI examination was considered within normal limits in 83 subjects (30.29%). Total of 36 patients who did not show abnormalities on T1 and T2 sequences showed abnormality on coronal STIR; 26 had spinal pathologies, and 10 were non-spinal. The pathologies of these 36 cases included sacroiliitis (17 cases), fractures (4), uterine fibroids (2), ovarian abnormalities (2), scoliosis (2), Legg-Calve-Perthes disease (1), fallopian tube abnormalities (1), fibroma in the erector spinae muscle (1), hematoma (1), metabolic bone disease (1), liver and pelvic mass (1), spondylitis (1), inflammatory bone process (1), and pilonidal sinus (1). STIR sequences had added merit in detecting non-spinal pathologies in 26 patients without being found on T1 and T2 sequences. Of the 17 cases of sacroiliitis, the average age was 37.1%, and the age range was between (18-81); the median age was 36. Of them, 11 were female, and 6 were male. 5 cases were bilateral sacroiliitis. 16 patients had findings suggestive of a neoplastic process on coronal STIR sequence, with only 1 of them being shown on T1 and T2 sequences. To investigate whether the number of cases diagnosed as sacroiliitis was significantly associated with abnormalities only found with the coronal STIR sequence, a Fisher’s exact test was run. shows that most cases of sacroiliitis showed pathogenic abnormalities on the coronal STIR sequence, with a significant P-value of < 0.0001.
| Number of cases | Percentage | |
| Pathology evident on T1 and T2 sequences | ||
| Disc prolapse | 147 | 53.65% |
| Canal stenosis | 39 | 14.23% |
| Spondylolisthesis | 9 | 3.28% |
| Schmorl’s node (non-pathologic finding) | 5 | 1.82% |
| Fracture | 4 | 1.46% |
| Spinal dysraphism | 2 | 0.73% |
| Findings suggestive of a neoplastic process | 1 | 0.36% |
| Spondylodiscitis | 1 | 0.36% |
| Pathologies outside the vertebral structures | 0 | 0.00% |
| Non-pathologic findings (normal) | 83 | 30.29% |
| Pathology evident on coronal STIR sequence | ||
| Pathologies outside the vertebral structures | 26 | 9.49% |
| Sacroiliitis | 23 | 8.39% |
| Findings suggestive of a neoplastic process | 16 | 5.84% |
| Fracture | 4 | 1.46% |
| Spinal dysraphism | 1 | 0.36% |
| Legg-Calve-Perthes disease | 1 | 0.36% |
| Non-pathologic findings (normal) | 199 | 72.63% |
Our study, utilizing prospectively collected data from patients evaluated for back pain and sciatica using T1, T2, axial, and coronal STIR sequences, demonstrates that incorporating coronal STIR imaging can significantly alter expected diagnoses and impact patient management. For instance, a study by Zeitoun and Mohieddin[9] found that adding coro
Our findings align with previous research highlighting the diagnostic value of incorporating coronal STIR sequences into routine lumbar spine MRI protocols. Patriat et al[8], in a large cohort study of 600 Lumbar spine MRIs, demonstrated that the addition of a large-field coronal STIR sequence led to the detection of extra-spinal abnormalities in 11.3% of cases - many of which, including gluteal tendinobursitis, hip osteoarthritis, and sacroiliitis, were not visible on standard sagittal images. Importantly, the study also reported incidental findings with potential clinical relevance in 11.7% of patients, emphasizing the broader diagnostic reach of this sequence. Similarly, Romeo et al[5] assessed the impact of coronal STIR imaging in patients presenting with low back pain and found additional extraspinal findings in 6.4% of cases, with the majority (72%) detectable exclusively on the coronal plane. Notably, the incorporation of this sequence influenced clinical decision-making in 3.5% of cases. These findings support the growing consensus that coronal STIR imaging offers meaningful diagnostic and therapeutic benefits, particularly in detecting pathologies that may otherwise go unrecognized on conventional imaging planes[6,10].
The inclusion of coronal STIR sequences identified abnormalities in 30.29% of cases, despite normal T1 and T2 imaging. This underscores its importance in diagnosing both spinal and non-spinal pathologies, with 26 cases linked to spinal issues and 10 to non-spinal conditions. Notably, Fisher's exact test revealed a significant association between the diagnosis of sacroiliitis and abnormalities identified solely via the coronal STIR sequence (P < 0.0001).
In response to these findings, our institution has adopted coronal STIR imaging as a standard part of the lumbar MRI protocol, aiming to expedite diagnosis and improve treatment efficacy while potentially reducing unnecessary further investigations. However, this protocol change may have cost implications that necessitate additional cost-effectiveness studies.
A 2019 study in Egypt involving 50 patients corroborates our results regarding the benefits of coronal STIR sequences, identifying a 20% increase in diagnostic findings, while our study found an additional 13.14%[9]. Both studies highlight coronal STIR’s ability to unveil significant pathologies not discernible in routine MRI sequences, enhancing diagnostic accuracy. We excluded patients with a history of surgical follow-up for back imaging; however, traumatic patients were included. We found abnormalities in 85% of T1 and T2 sequences, with 14.23% of cases showing abnormalities across all sequences, and 13.14% detected exclusively on coronal STIR. Thus, the number of patients with abnormal findings increased by 13.14%.
A recent study involving 600 consecutive lumbar MRI scans, performed using the same protocol as our investigation, retrospectively reviewed cases with two musculoskeletal radiologists independently assessing coronal STIR sequences for extra-spinal abnormalities contributing to lumbar radiculopathy[9]. Extra-spinal cause on the coronal STIR sequence in 68 cases (11.3%), primarily gluteal tendon bursitis (30.9%), congestive hip osteoarthritis (25%), degenerative sacroiliac ar
Extra spinal injuries were frequently noted, with 70 cases (11.7%), of which 38% involved tumors or pseudo-tumor masses necessitating further evaluation[8]. In our study, we identified extraspinal injuries in 13.8% of the 36 patients, including fractures and hematomas. A previous study indicated higher rates of definite extra-spinal sciatica causes in patients aged 24 to 40[7]. In our study of 274 patients, the mean ages for abnormal and normal coronal STIR were 43.96 and 45.26, respectively, with no significant age difference (P = 0.5604), Table 2. Of these, 199 had normal coronal STIR findings, but 36 showed abnormalities undetected by T1 and T2 sequences, with 26 having spinal and 10 non-spinal pathologies.
Comparing our results with a study of 931 patients, which found a 6.4% rate of additional extraspinal findings, we observed a higher percentage (13.14%). Our study also revealed that around 10.9% had changes in their treatment workflow[6]. A 2015 study with a similar demographic profile highlighted degenerative disc disease as the most common finding; however, our research identified a broader range of additional pathologies, including liver and pelvic abnorma
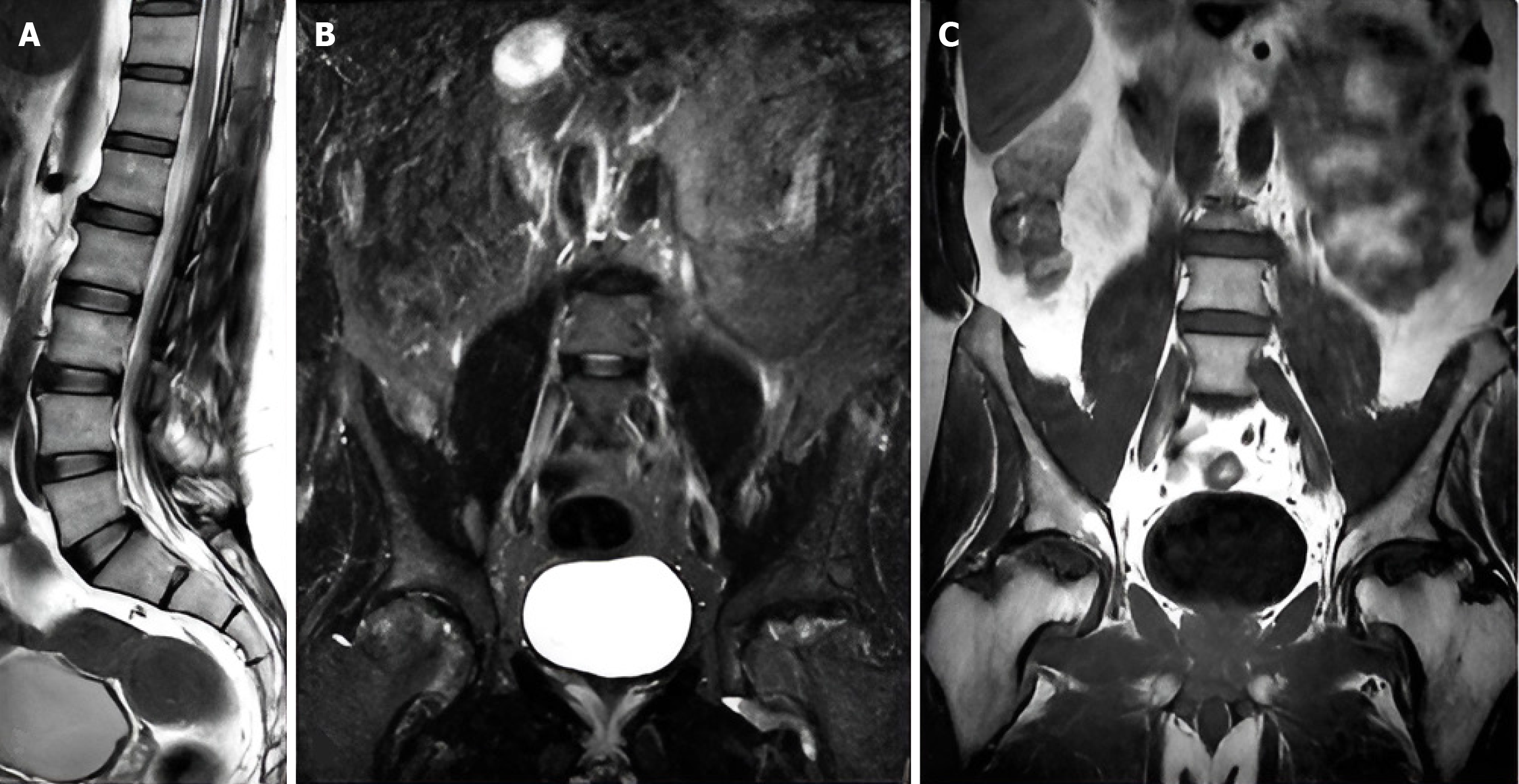
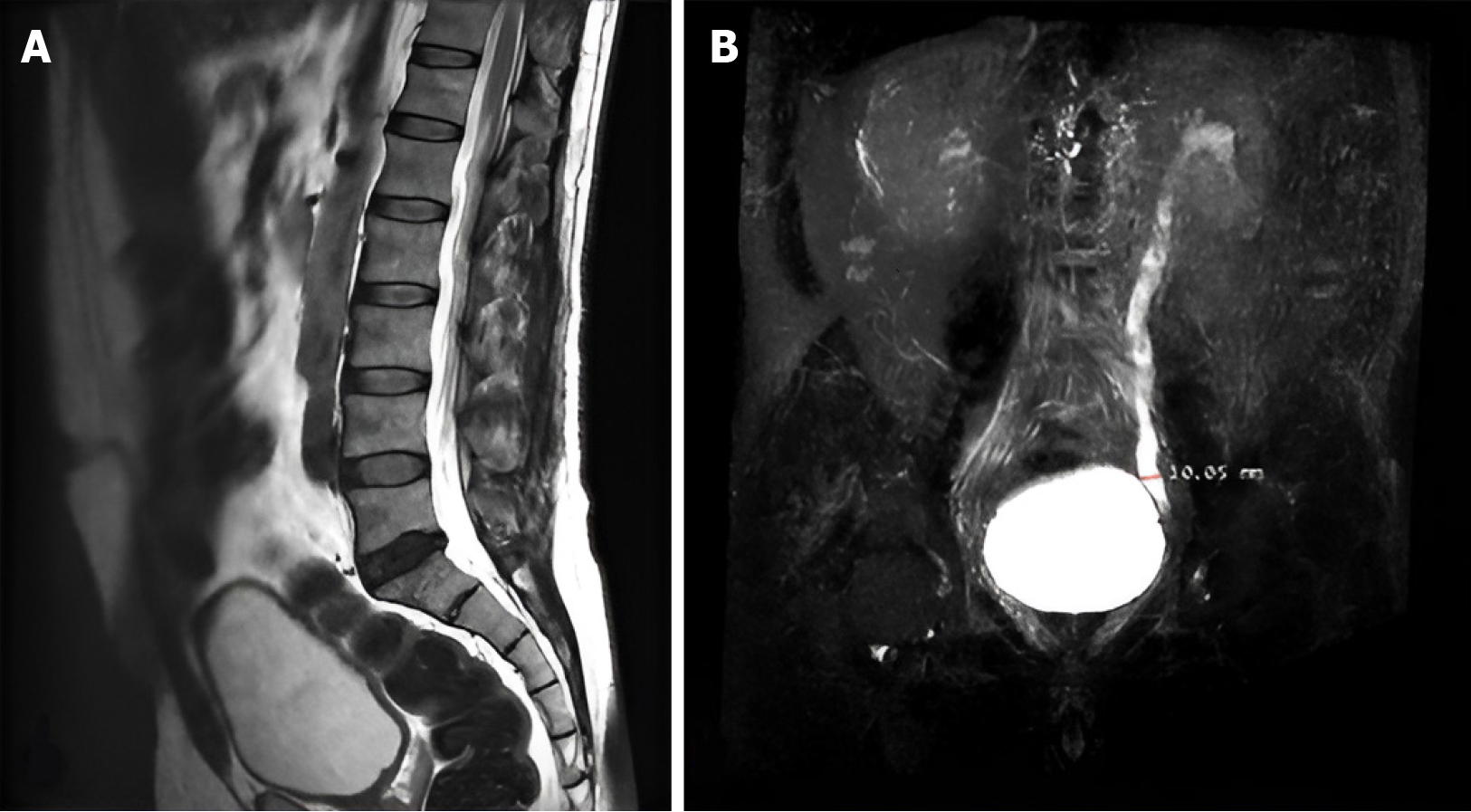
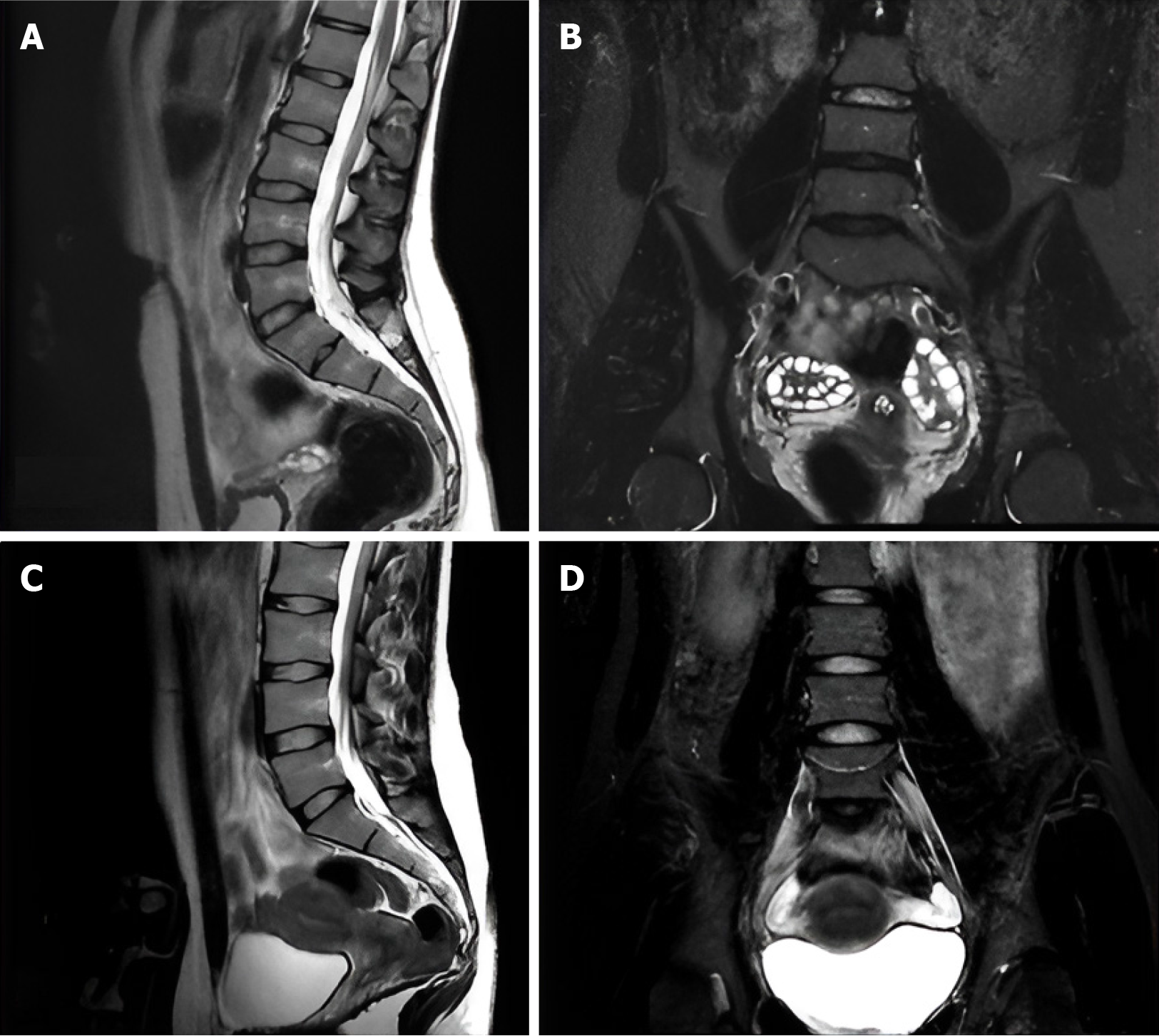
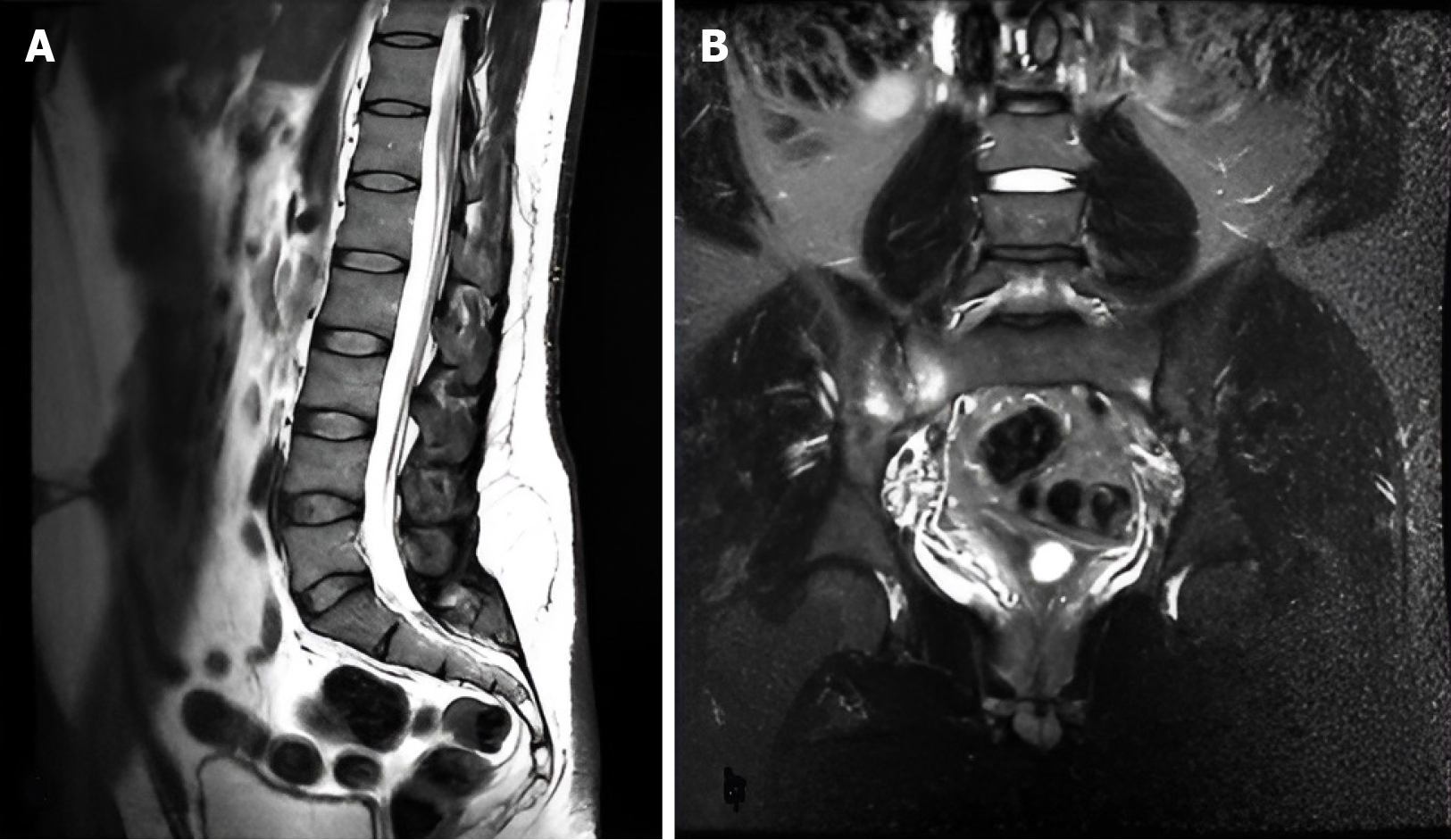
As mentioned, we have a percentage of 72% of the 36 patients with abnormal coronal STIR and normal T1 and T1, which is 9.5% of the total number of patients we included in our study, have a non-spinal pathology. The most evident were ureteric dilatation Figure 2, ovarian cysts, renal cysts, fallopian tube abnormalities, and masses, which change the treatment for the patient Figure 3. Sixteen patients had findings suggesting a neoplastic process on the coronal STIR sequence, with only one of these being detected on the T1 and T2 sequences (a bony lesion in the sacral area). The findings included seven ovarian cysts, four sacroiliac bony lesions, two uterine fibroids, one fibroma in the erector spinae muscle, one lung lesion, and one liver and pelvic mass. To determine if the number of sacroiliitis cases was significantly associated with abnormalities found solely on the coronal STIR sequence, a Fisher’s exact test was conducted, indicating that most cases of sacroiliitis exhibited pathogenic abnormalities exclusively on the coronal STIR sequence, with a significant P value of < 0.0001. This result shows that sacroiliitis is the most common finding in our study on the coronal STIR sequence Figure 4.
Our study had several limitations that should be addressed in future research. Firstly, in cases of severe pain, we opted not to proceed with the examination or add the coronal STIR sequence. When abnormalities were detected on T1 and T2 images, the examination was halted to avoid discomfort for the patient. Claustrophobia also posed a potential barrier to including this additional sequence, though it is noteworthy that very few patients reported concerns about the extended imaging time. Moreover, while the incorporation of coronal STIR can reveal diseases that are difficult to diagnose with a single sequence, it may necessitate further imaging, which could lead to additional procedural requirements.
The inclusion of coronal STIR imaging revealed additional pathologies that may be difficult to diagnose with single-sequence evaluations, emphasizing the need for comprehensive imaging protocols. To enhance future research, we re
This prospective study underscores the clinical importance and diagnostic value of incorporating coronal STIR sequences into routine lumbar MRI protocols for patients with back pain and sciatica. By significantly enhancing the detection of both spinal and extra-spinal pathologies many of which were missed on standard sequences, this approach represents a novel, cost-effective refinement to conventional imaging strategies, with direct implications for more accurate diagnosis, targeted treatment, and improved patient outcomes.
We sincerely thank the Radiology Team at KHCC for their invaluable assistance in data collection and analysis.
| 1. | GBD 2021 Diseases and Injuries Collaborators. Global incidence, prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990-2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet. 2024;403:2133-2161. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1073] [Cited by in RCA: 1439] [Article Influence: 1439.0] [Reference Citation Analysis (0)] |
| 2. | Shah LM, Hanrahan CJ. MRI of spinal bone marrow: part I, techniques and normal age-related appearances. AJR Am J Roentgenol. 2011;197:1298-1308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 105] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 3. | Vande Berg BC, Malghem J, Lecouvet FE, Maldague B. Magnetic resonance imaging of normal bone marrow. Eur Radiol. 1998;8:1327-1334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 105] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 4. | Zanchi F, Richard R, Hussami M, Monier A, Knebel JF, Omoumi P. MRI of non-specific low back pain and/or lumbar radiculopathy: do we need T1 when using a sagittal T2-weighted Dixon sequence? Eur Radiol. 2020;30:2583-2593. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 34] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 5. | Romeo V, Cavaliere C, Sorrentino C, Ponsiglione A, Ugga L, Barbuto L, Verde F, Covello M. Clinical impact of coronal-STIR sequence in a routine lumbar spine MR imaging protocol to investigate low back pain. Medicine (Baltimore). 2018;97:e10789. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Refaat M, Torky A, Reda M. Merits of Adding Coronal-STIR Sequence in a Routine Lumbo-Sacral Spine MR Imaging Protocol to Investigate Sciatica and Sciatica-Like Symptoms. Benha Med J. 2020;37:21-31. [DOI] [Full Text] |
| 7. | Tokuda O, Harada Y, Matsunaga N. MRI of soft-tissue tumors: fast STIR sequence as substitute for T1-weighted fat-suppressed contrast-enhanced spin-echo sequence. AJR Am J Roentgenol. 2009;193:1607-1614. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Patriat Q, Prigent FV, Aho S, Lenfant M, Ramon A, Loffroy R, Lambert A, Ornetti P. Diagnostic Value of an Additional Sequence (Large-Field Coronal Stir) in a Routine Lumbar Spine MR Imaging Protocol to Investigate Lumbar Radiculopathy. J Clin Med. 2023;12:6250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 9. | Zeitoun R, Mohieddin MSA. Coronal STIR sequence, a simple adjustment to routine MRI protocol for extra-spinal sciatica and sciatica-like symptoms. Egypt J Radiol Nucl Med. 2019;50:74. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Gupta R, Mittal P, Mittal A, Mittal K, Gupta S, Kaur R. Additional merit of coronal STIR imaging for MR imaging of lumbar spine. J Craniovertebr Junction Spine. 2015;6:12-15. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |