Copyright
©2013 Baishideng.
World J Radiol. Mar 28, 2013; 5(3): 126-142
Published online Mar 28, 2013. doi: 10.4329/wjr.v5.i3.126
Published online Mar 28, 2013. doi: 10.4329/wjr.v5.i3.126
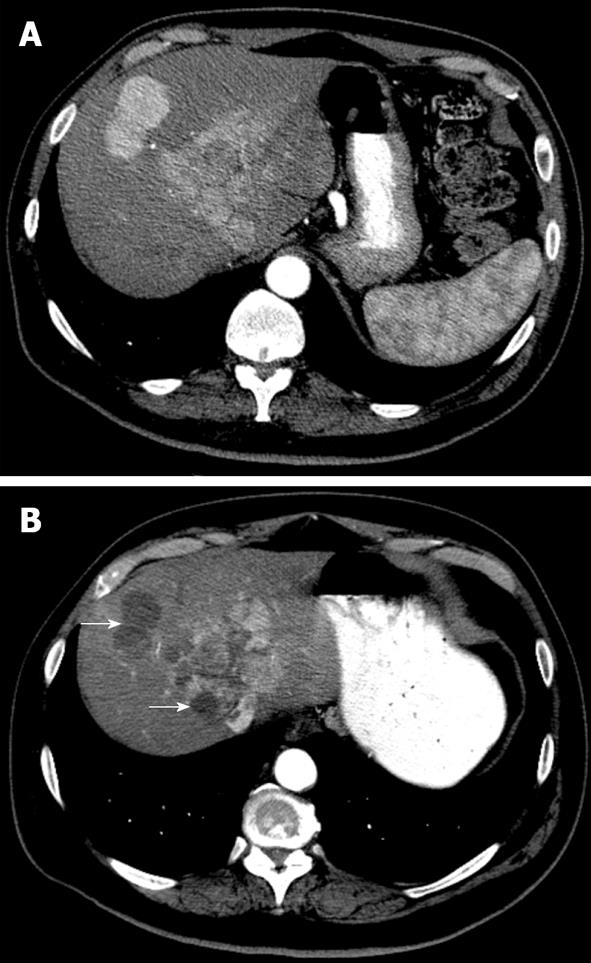
Figure 1 A 62-year-old man with multifocal hepatocellular carcinoma.
A: Baseline contrast enhanced computed tomography (CT) in the arterial phase shows enhancing nodules in segment VIII and IV; B: Contrast enhanced CT after Sorafenib shows decreased tumor enhancement with near complete disappearance of enhancement in some nodules (arrows) and only marginal decreased tumor size.
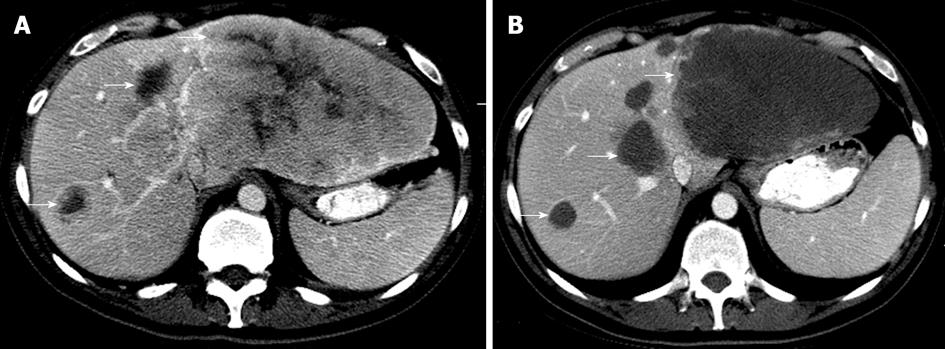
Figure 2 Axial computed tomography images in the portovenous phase of a 50-year-old female with colorectal liver metastases.
A: Pretreatment evaluation showed multiple heterogeneously enhancing hepatic masses that are compatible with known hepatic metastases. The entire left hepatic lobe was occupied by the masses. Note the thickened nodular interface between the mass and normal liver (arrow); B: Liver metastases became more homogenous and showed well-defined interfaces with the normal liver parenchyma after Folfox and Avastin, corresponding to treatment response. Note the well defined interface (arrows).
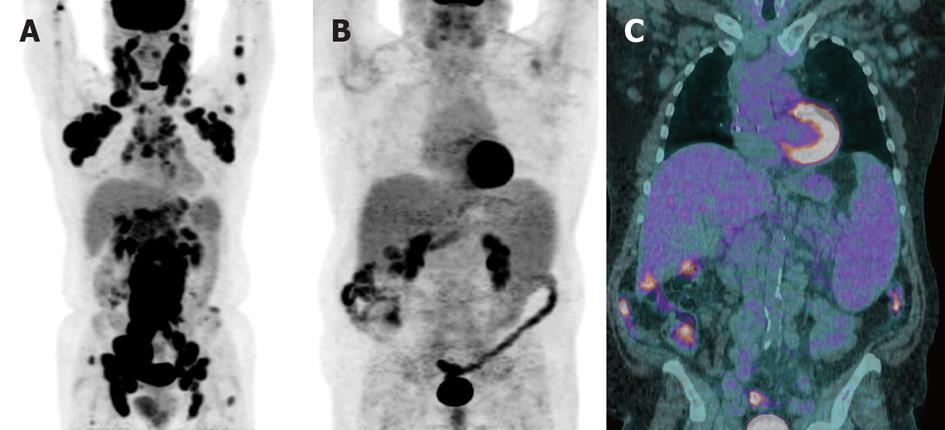
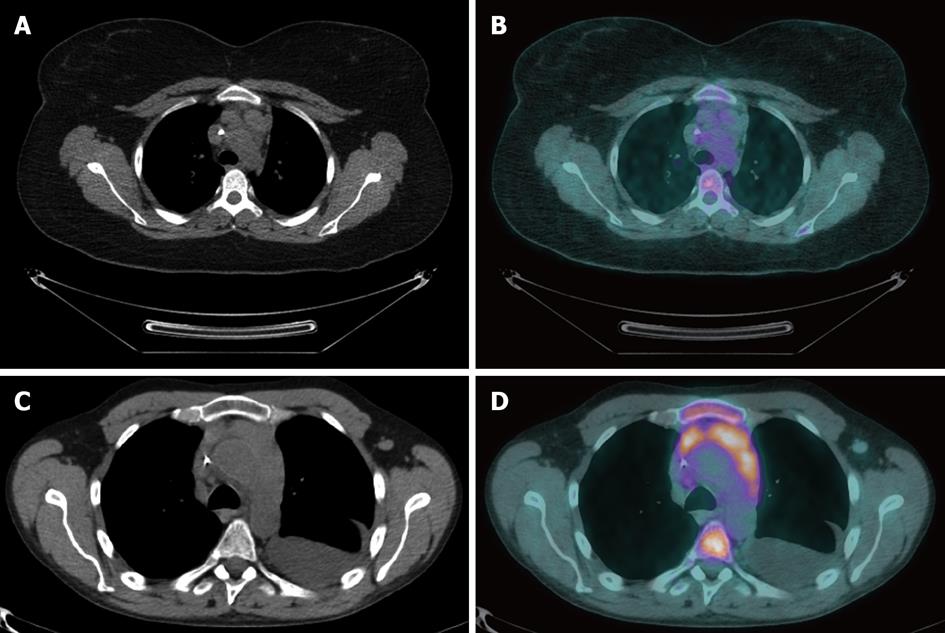
Figure 3 The fluorodeoxyglucose activity of lymphoma can be variable.
A: A positron emission tomography (PET) image of a 62-year-old male with untreated grade 2 follicular lymphoma showed strong fluorodeoxyglucose (FDG) avid lymph nodes above and below the diaphragm; B, C: A whole body PET image of a 65-year-old male with untreated chronic lymphocytic leukemia or small lymphocytic leukemia showed no FDG uptake (B) but a PET/computed tomography fusion image demonstrated retroperitoneal lymphadenopathy (C).
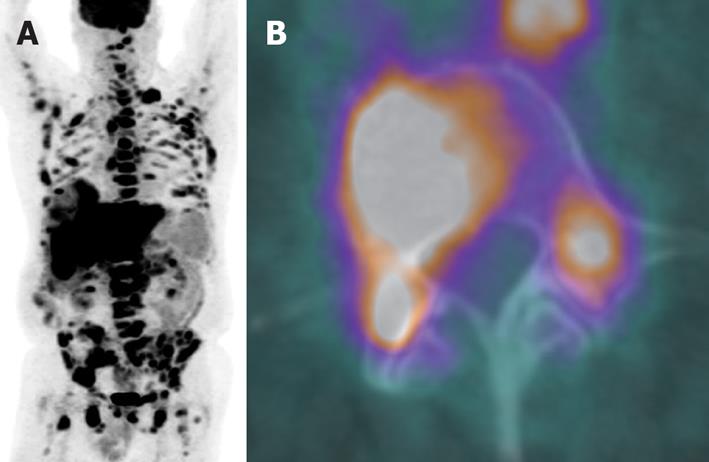
Figure 4 A whole body positron emission tomography image of a 67-year-old male with marginal zone lymphoma showed extensive disease involving lymph nodes above and below diaphragm, osseous structures and liver (A).
The bone marrow biopsy was negative but the direct biopsy from L4, which was positive on the positron emission tomography/computed tomography fusion image (B), confirmed bone marrow involvement.
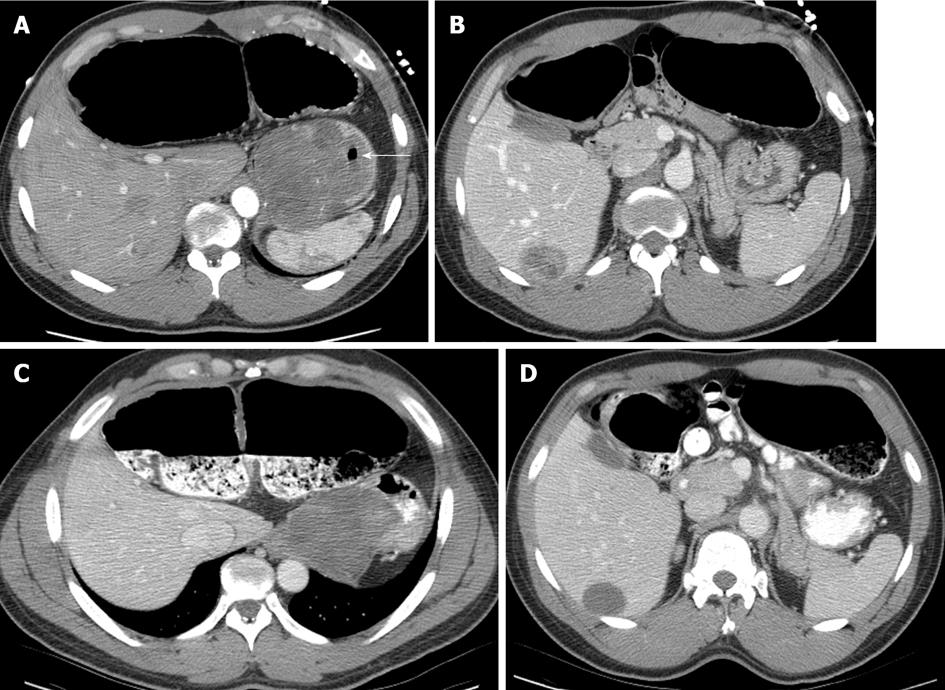
Figure 5 A computed tomography image of a 22-year-old female with Hodgkin’s lymphoma after 4 cycles of chemotherapy demonstrated residual mediastinal lymphadenopathy (A) that is not metabolically active, as seen on positron emission tomography/computed tomography fusion images, and consistent with post-therapy fibrosis (B).
A computed tomography image of a 50-year-old male with diffuse large B-cell lymphoma after 6 cycles of chemotherapy showed a residual mediastinal abnormality that represents viable tumor as shown by the abnormal actiivty on the positron emission tomography/computed tomography fusion image. Also note left pleural effusion and bone marrow activation (D).
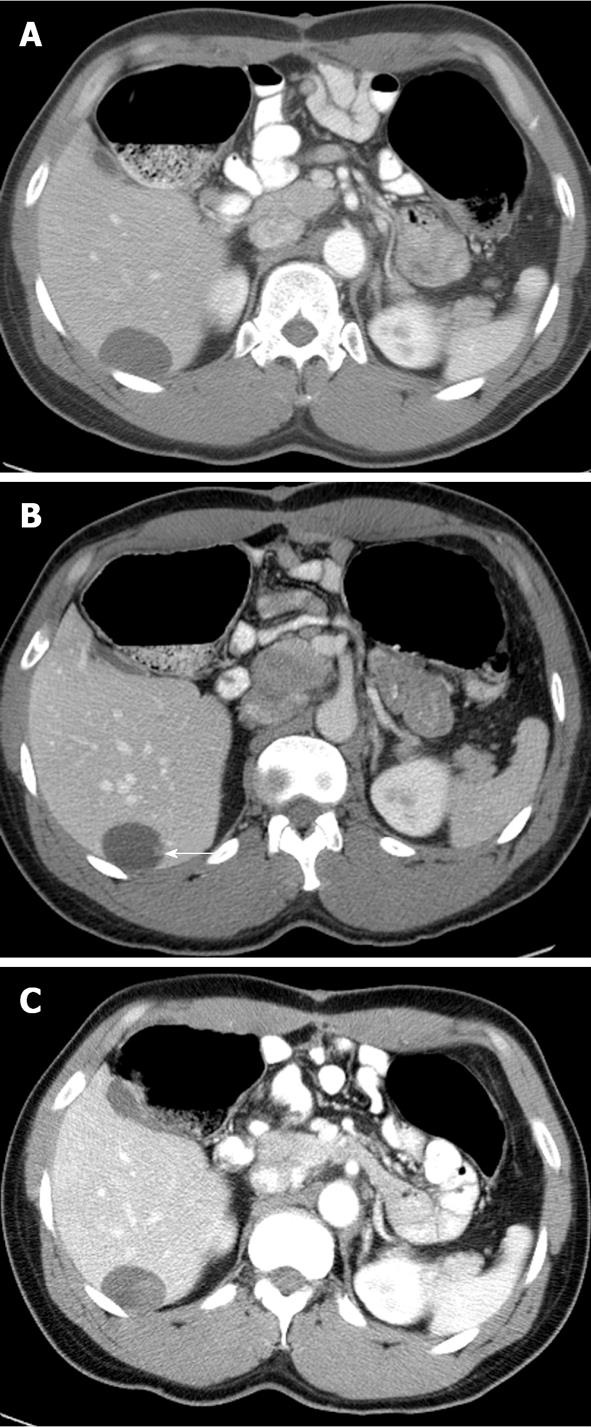
Figure 6 A computed tomography image of a 64-year-old male with metastatic gastro intestinal tumors prior to the imatinib shows a large heterogeneously enhanced gastric mass compatible with gastric gastro intestinal tumors (A) and a segment 6 hepatic metastasis (B).
The primary tumor and hepatic metastasis showed decreases in tumor size and became homogeneous in internal appearance after the targeted therapy (C, D). Note the stomach air bubble (arrow in A).
Figure 7 Axial computed tomography images of the same patient in Figure 6 at a later time showed progression of metastatic disease.
Immediately following the second course of targeted therapy, the hepatic metastasis showed homogenous hypoenhancement compatible with treatment response (A). A small nodular enhancing focus within the lesion is the radiographic finding of recurrent disease (arrow in B) which had progressed and appeared more conspicuous (C).
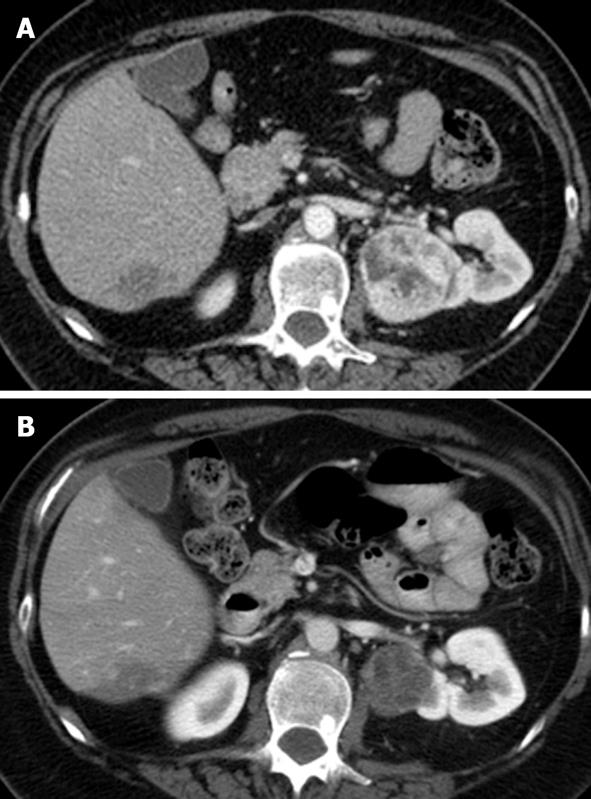
Figure 8 A computed tomography image of a 45-year-old man with clear cell type renal cell carcinoma who had received pre-operative Sorafenib.
An exophytic heterogeneously hyperenhanced right renal mass (A) demonstrated homogenous hypoenhancement after the targeted therapy (B). Note an atypical segment 6 hepatic hemangioma and a L1 bone island.
- Citation: Peungjesada S, Chuang HH, Prasad SR, Choi H, Loyer EM, Bronstein Y. Evaluation of cancer treatment in the abdomen: Trends and advances. World J Radiol 2013; 5(3): 126-142
- URL: https://www.wjgnet.com/1949-8470/full/v5/i3/126.htm
- DOI: https://dx.doi.org/10.4329/wjr.v5.i3.126