Copyright
©2010 Baishideng Publishing Group Co.
World J Radiol. Apr 28, 2010; 2(4): 122-134
Published online Apr 28, 2010. doi: 10.4329/wjr.v2.i4.122
Published online Apr 28, 2010. doi: 10.4329/wjr.v2.i4.122
Figure 1 Focal chronic pancreatitis.
Endoscopic ultrasonography (EUS) shows a mass with an irregular, inhomogeneous echo pattern, and calcification (arrow) at the head of the pancreas.
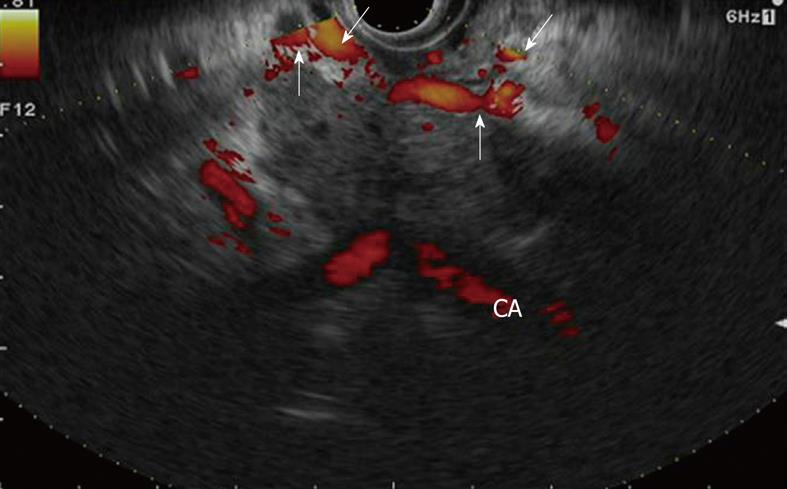
Figure 2 Pancreatic adenocarcinoma.
EUS shows a heterogeneous hypoechoic mass with irregular margins at the body of the pancreas, infiltrating the celiac artery, and development of collateral vessels around the tumor (arrows). CA: Celiac artery.
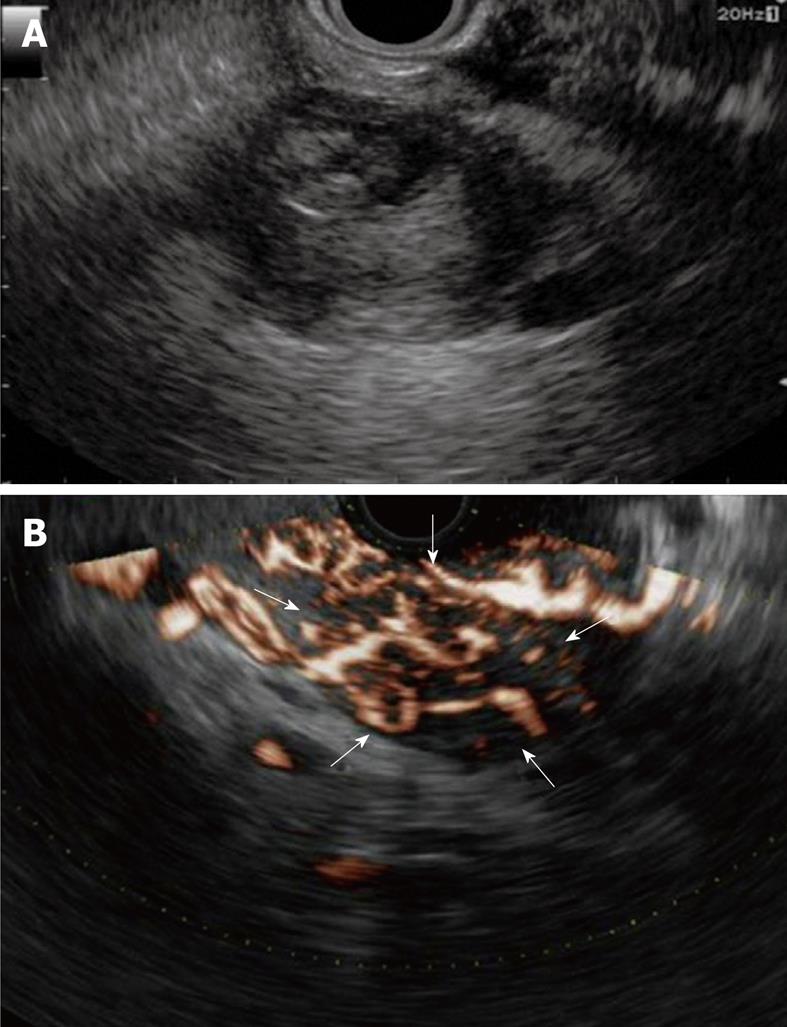
Figure 3 Neuroendocrine tumor.
A: EUS shows a heterogeneous appearance; cystic, with a solid component or pure fluid 31 mm in diameter; B: EUS using Doppler mode shows a hypervascular mass at the tail of the pancreas (arrows).
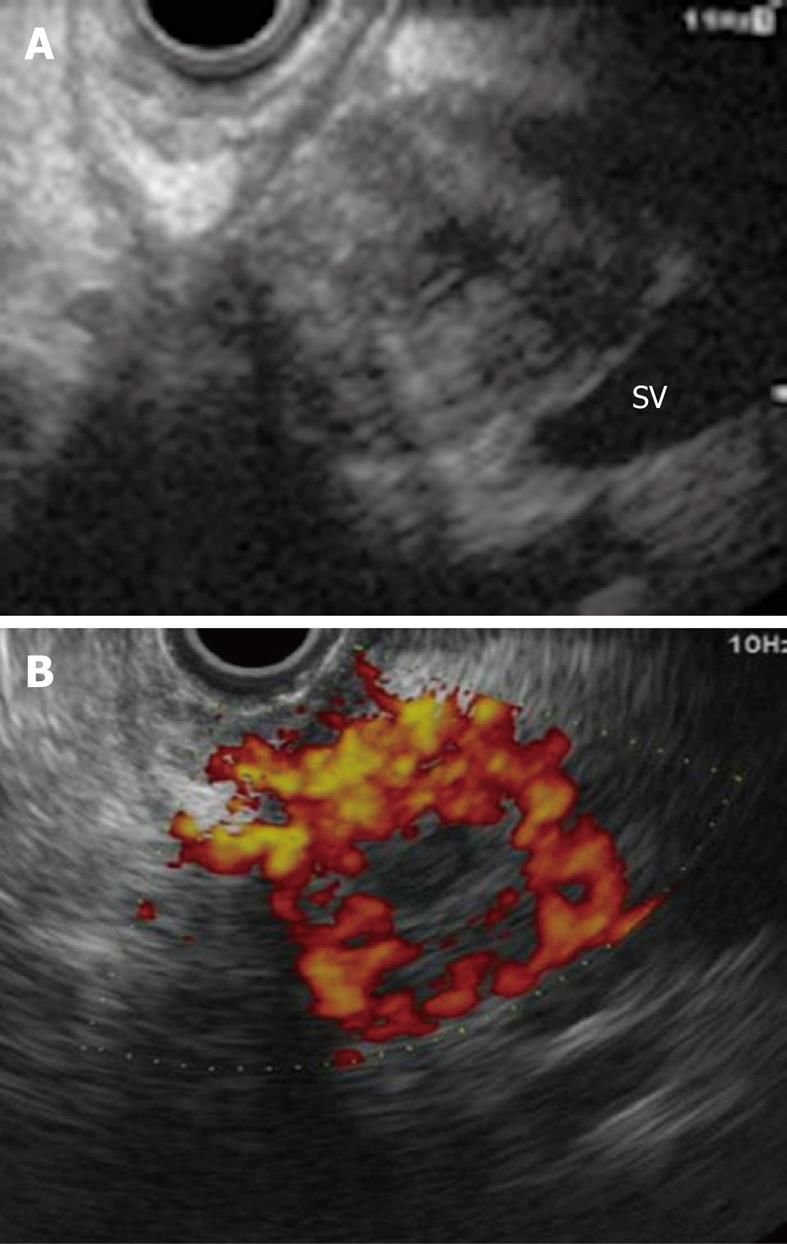
Figure 4 Metastatic pancreatic cancer from renal cell carcinoma.
A: EUS shows a heterogeneous hypoechoic mass with a central necrotic area at the head of the pancreas; B: Contrast-enhanced Doppler EUS shows a hypervascular mass. SV: Splenic vein.
Figure 5 Pseudocyst.
EUS shows a cystic lesion with a thick wall surrounding a round fluid collection at the body of the pancreas.
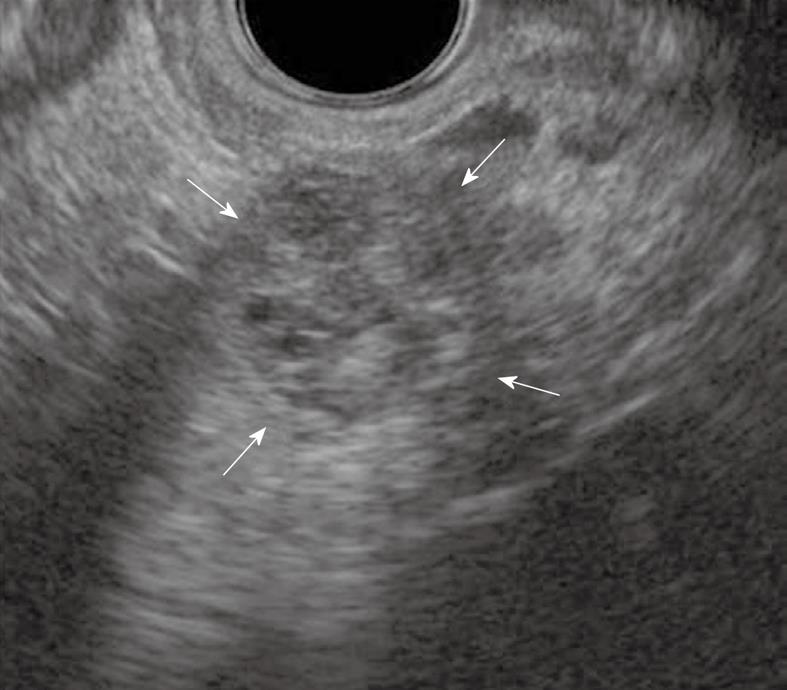
Figure 6 Serous cyst adenoma.
EUS shows a mass with a “honeycomb appearance” at the body of the pancreas 13 mm in diameter (arrows).
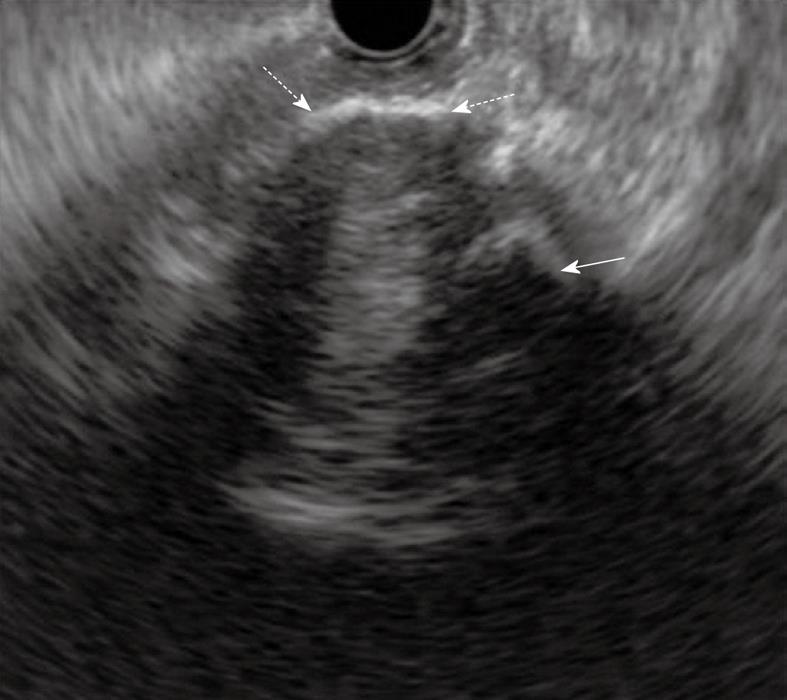
Figure 7 Solid pseudopapillary tumor.
EUS shows a tumor in part of the calcified wall (dashed arrows) with acoustic shadow and inner calcifications (arrow) at the body of the pancreas 12 mm in diameter.
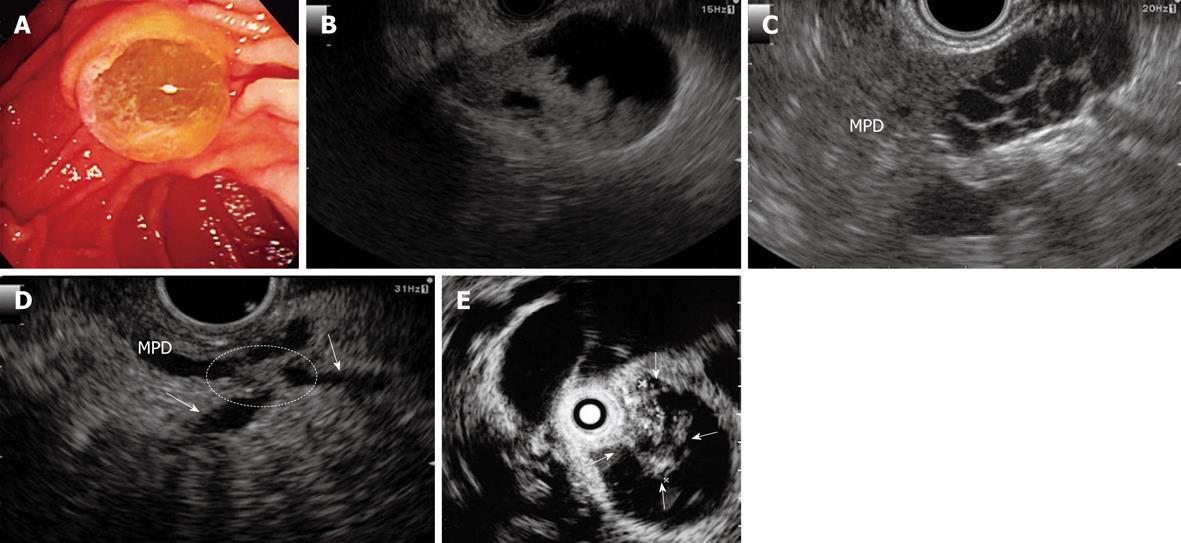
Figure 8 Intraductal papillary mucinous neoplasms (IPMN).
A: An endoscopic diagnosis of an IPMN can be established if the “fish-eye” ampulla is visualized in minority cases; B: IPMN of main duct type. EUS shows a mural nodule within by the mucinous dilatation of the pancreatic ducts, with involvement of the main duct at the tail of the pancreas; C: IPMN of side branch type. EUS shows a multiple dilatation of the side branch at the neck of the pancreas; D: IPMN of the combined type. EUS show a mural nodule stretching (circle) over the main pancreatic duct and side branches (arrows) at the body of the pancreas. E: IPMN of main duct type. Intraductal ultrasonography (IDUS) can identify tumor nodule development into the main pancreatic duct (arrows). MPD: Main pancreatic duct.
Figure 9 Mucinous cystic neoplasms (MCN).
EUS shows a separated macrocyst 40 mm in diameter.
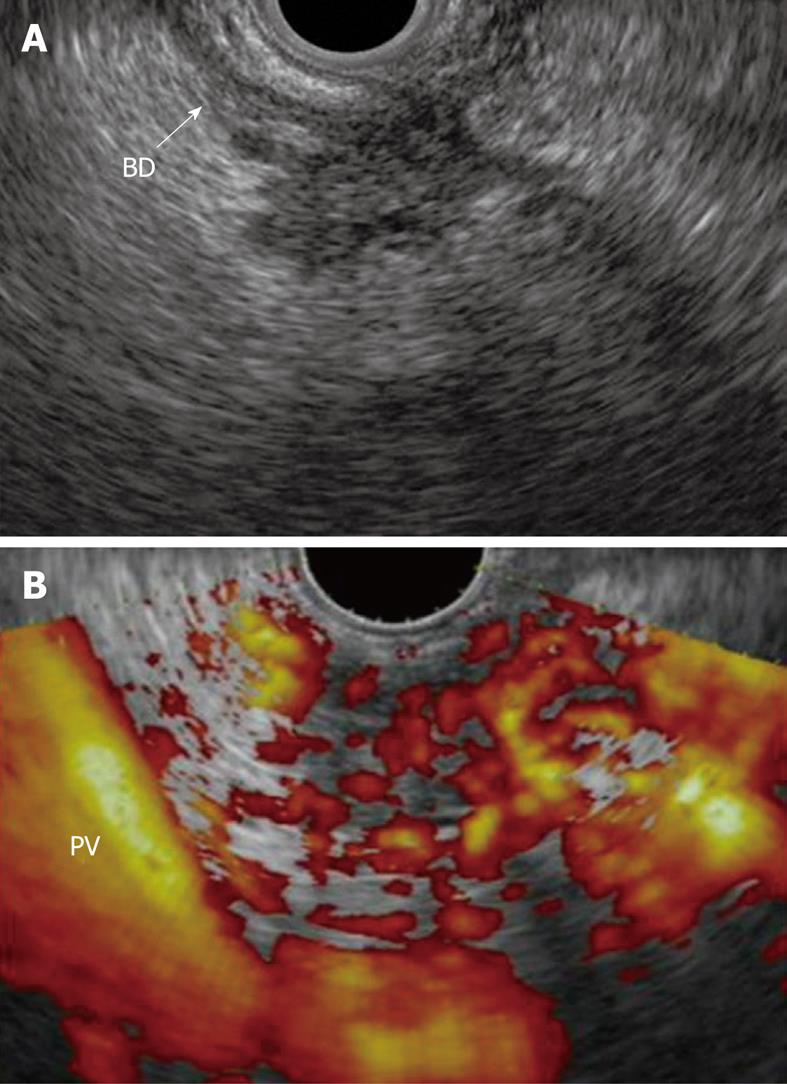
Figure 10 Focal chronic pancreatitis.
A: EUS shows a mass with an irregular and inhomogeneous echo pattern at the head of the pancreas; B: Contrast-enhanced power Doppler EUS shows an isovascular nodule compared with the surrounding pancreatic tissue. BD: Bile duct; PV: Portal vein.
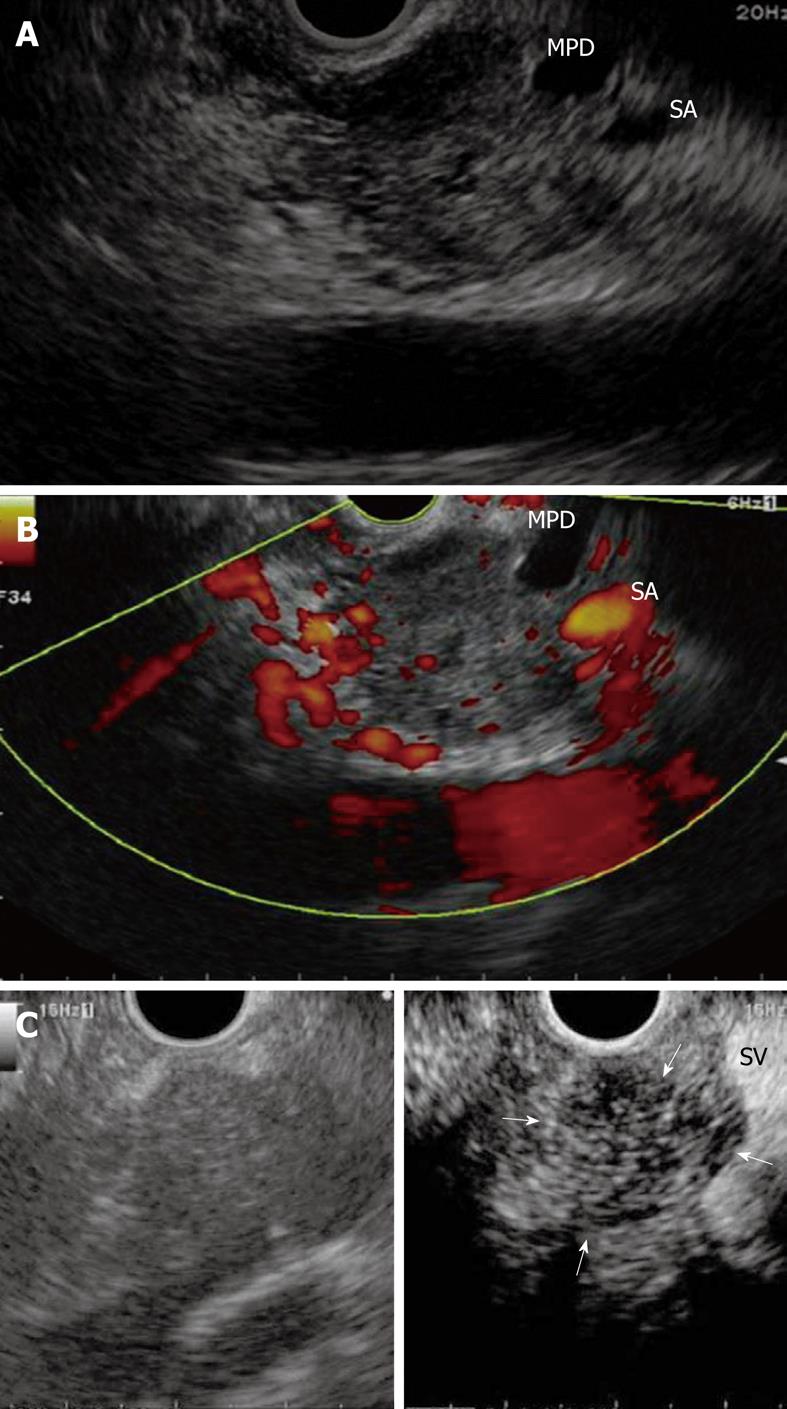
Figure 11 Pancreatic adenocarcinoma.
A: EUS shows a heterogeneous hypoechoic mass with irregular margins at the body of the pancreas and tail side main pancreatic duct enlarged due to the infiltrating mass; B: Contrast-enhanced power Doppler EUS shows a hypovascular nodule compared with the surrounding pancreatic tissue; C: Contrast-enhanced harmonic EUS showing a clear margin and hypovascular nodule compared with surrounding pancreatic tissue (arrows) without blooming artifact such as that found with Doppler imaging. Left: B-mode imaging; Right: Contrast imaging. MPD: Main pancreatic duct; SA: Splenic artery.
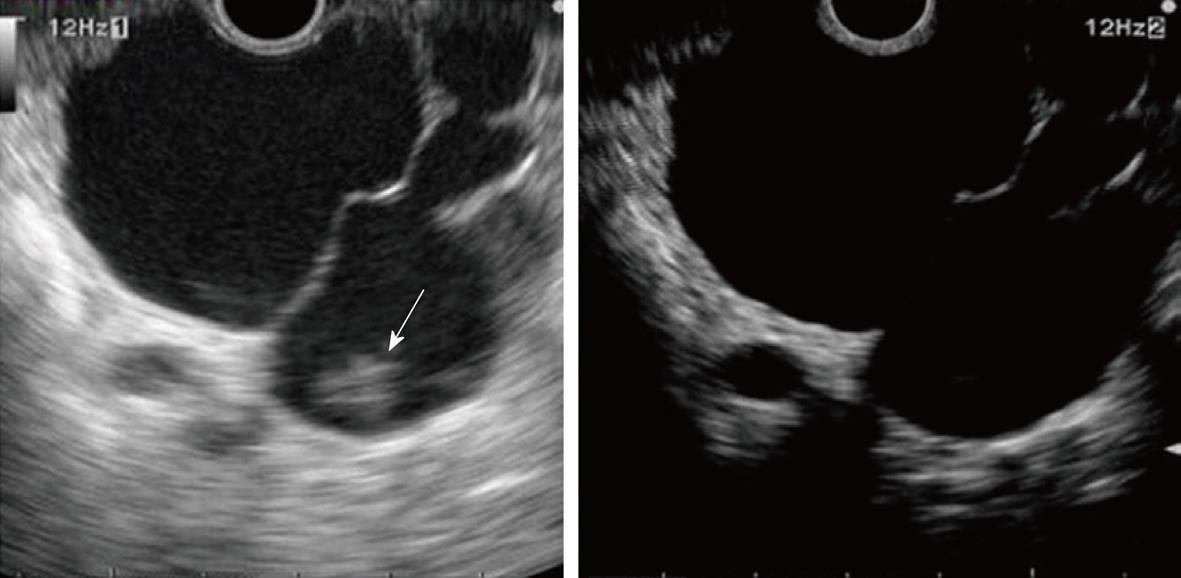
Figure 12 IPMN of side branch type.
Left (B-mode image): The nodule (arrow) in dilatation of the side branch cannot be distinguished between sediment and tumor by B-EUS; Right (contrast image): Contrast-enhanced harmonic EUS reveals that this nodule is sediment.
- Citation: Sakamoto H, Kitano M, Kamata K, El-Masry M, Kudo M. Diagnosis of pancreatic tumors by endoscopic ultrasonography. World J Radiol 2010; 2(4): 122-134
- URL: https://www.wjgnet.com/1949-8470/full/v2/i4/122.htm
- DOI: https://dx.doi.org/10.4329/wjr.v2.i4.122