Copyright
©2010 Baishideng Publishing Group Co.
World J Radiol. Nov 28, 2010; 2(11): 440-448
Published online Nov 28, 2010. doi: 10.4329/wjr.v2.i11.440
Published online Nov 28, 2010. doi: 10.4329/wjr.v2.i11.440
Figure 1 Virtual intravascular endoscopy visualization of the true lumen, false lumen and intimal flap (arrow) in a Stanford type B aortic dissection.
Corresponding orthogonal views (axial, coronal and sagittal) confirm the location of virtual intravascular endoscopy position inside the false lumen (F) looking toward the true lumen (T) and intimal flap.
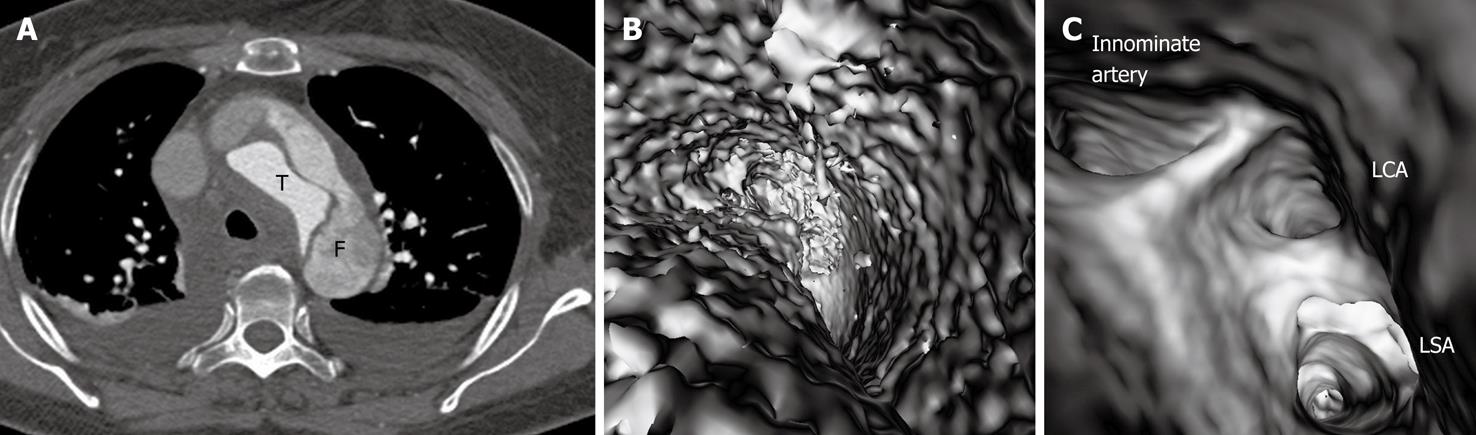
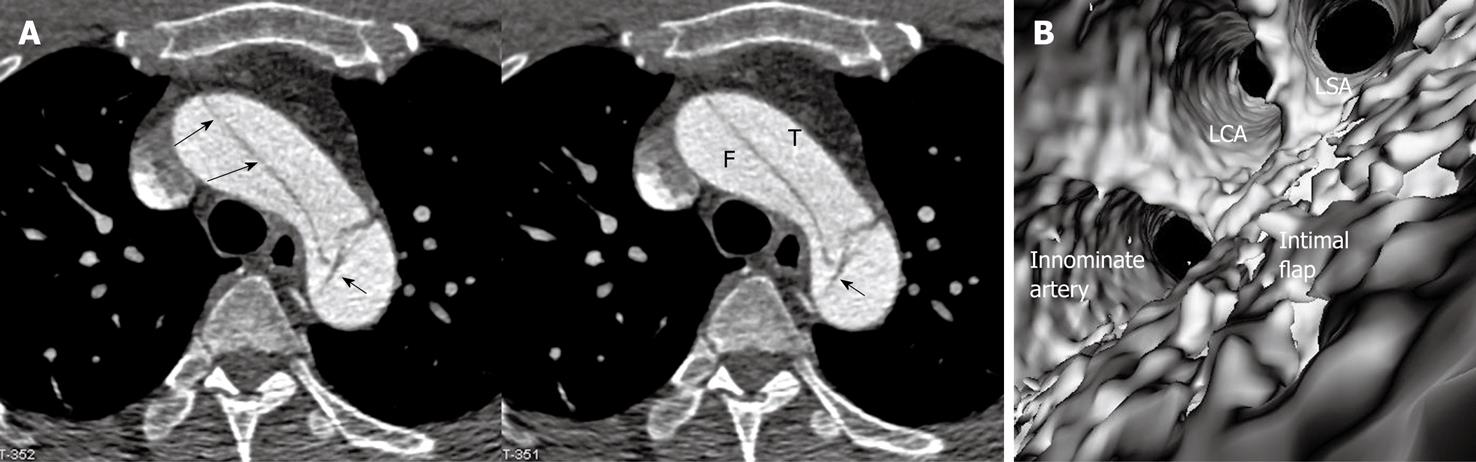
Figure 2 Stanford type A dissection with the true lumen smaller than the false lumen.
The false lumen (F) has lower computed tomography (CT) attenuation than that in the true lumen (T) due to thrombus formation (A), thus a lower CT threshold (90 HU) was applied to view the false lumen intraluminally (B), while a higher CT attenuation (300 HU) was applied to demonstrate the true lumen. Corresponding virtual intravascular endoscopy (C) shows the involvement of three aortic branches by the dissection, namely left subclavian artery (LSA), left common carotid artery (LCA) and innominate artery when the view is positioned inside the false lumen. Bilateral pleural effusion is present on the 2D axial image.
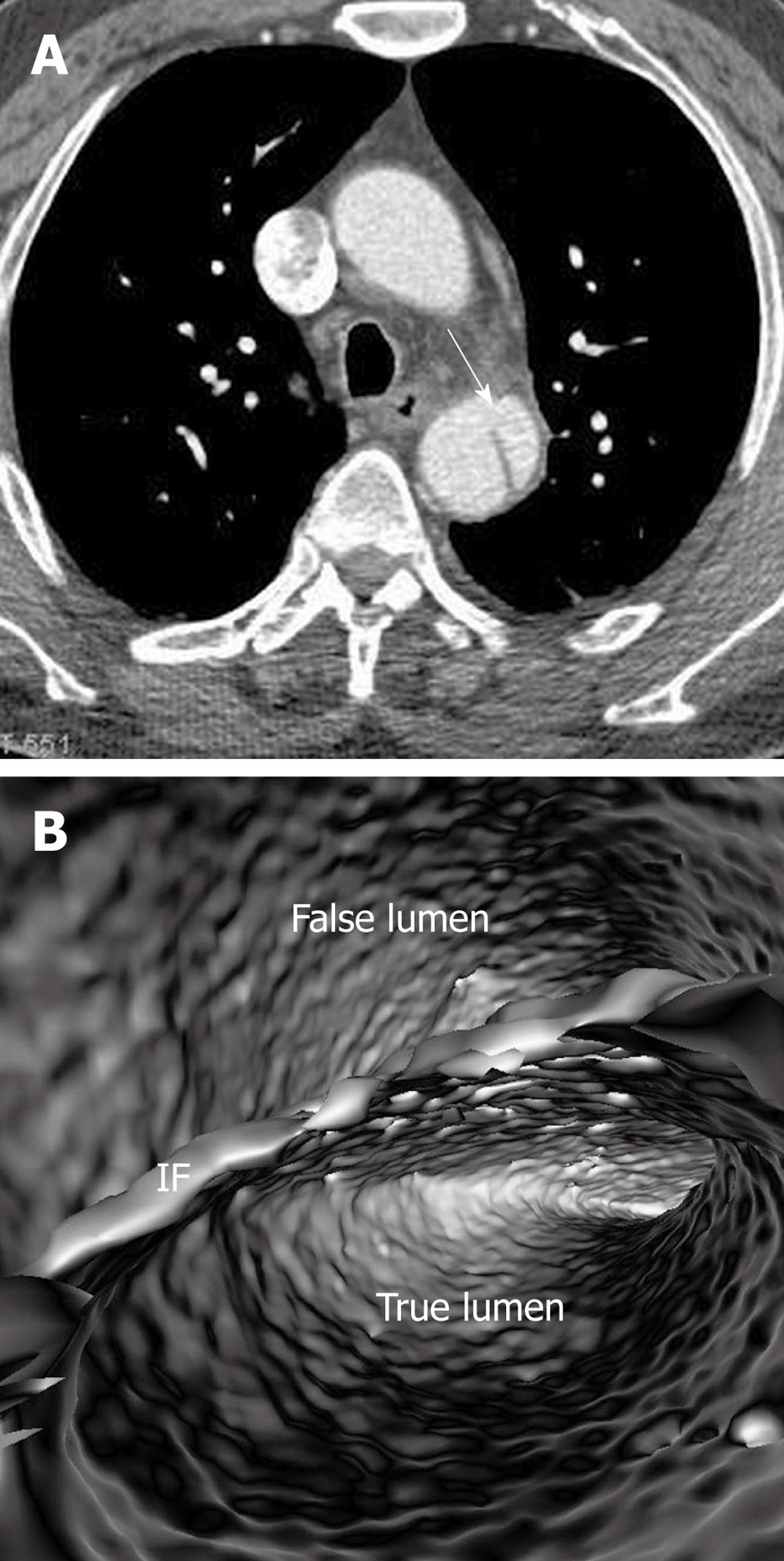
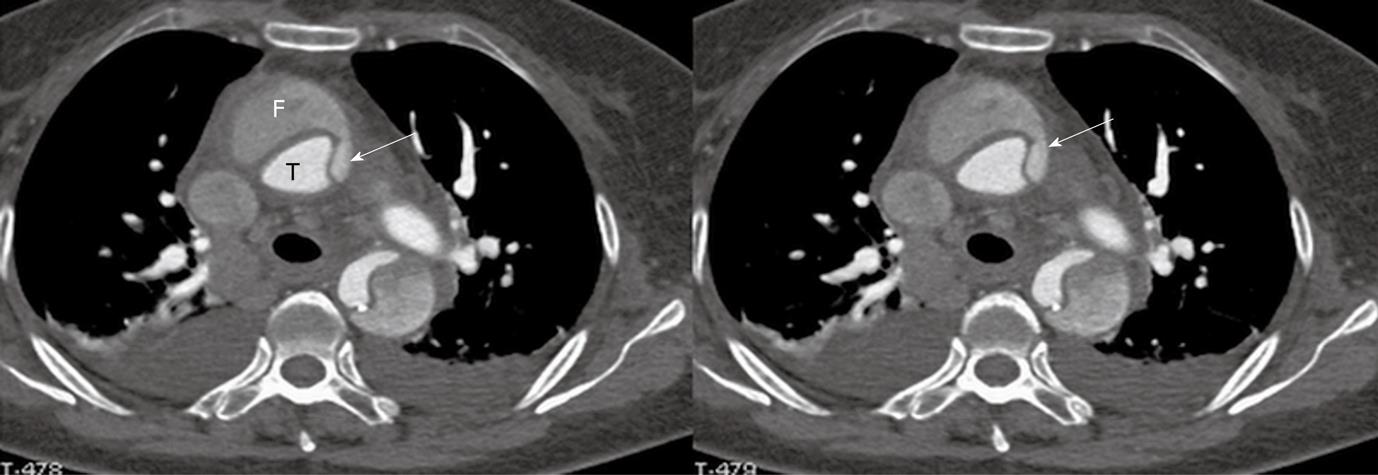
Figure 3 Stanford type B dissection with similar computed tomography attenuation in both true and false lumens (A).
Virtual intravascular endoscopy clearly demonstrates the true and false lumens separated by the intimal flap (IF) in a single image (B). Arrow in A indicates the intimal flap.
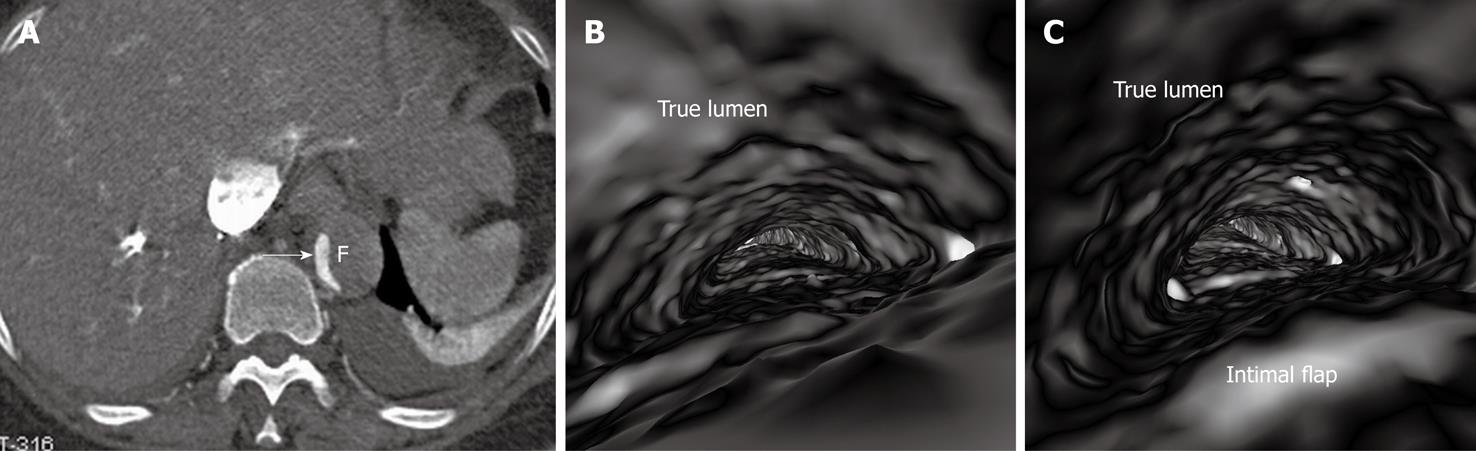
Figure 4 Stanford A dissection with abdominal artery branches involved.
The false lumen (F) is thrombosed (A) with the true lumen being compressed to a much narrowed space. Virtual endoscopy views inside the true lumen clearly demonstrate the narrowed true lumen (B) and the intimal flap (C). Arrow in A indicates the true lumen.
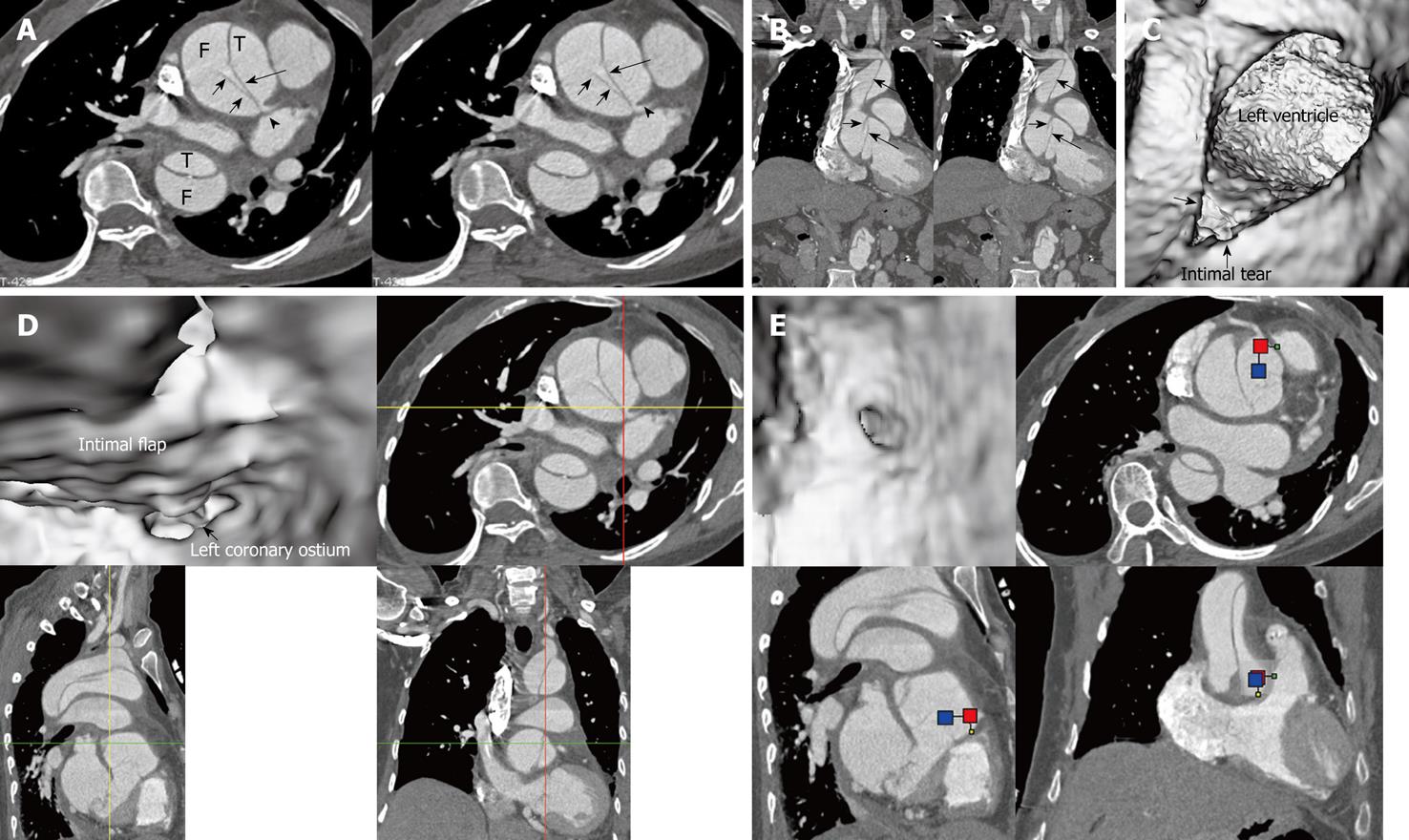
Figure 5 Stanford type A dissection with the dissection originating at the aortic root.
The intimal flap is clearly displayed on 2D axial and coronal reformatted images (long arrows in A and B) with the left coronary artery arising from the true lumen (T) (arrowhead). Virtual intravascular endoscopy shows the intimal tear which is located at the aortic root (arrow in C) proximal to the left ventricle. Both of the coronary ostia arise from the true lumen with the intimal flap extending to the left coronary ostium (D, E). Short arrows in A and B indicate the cobweb sign in the false lumen (F).
Figure 6 Stanford type A dissection with direct communication between the true lumen and false lumens (arrows in A).
The true lumen (T) was obviously narrowed due to compression by the false lumen (F) with thrombus formed in the false lumen as shown on the sagittal reformatted image (B). The intimal flap (short arrows in B) arises from the level of the left ventricle (long arrows in B); C: A protrusion sign was observed on virtual intravascular endoscopy (VIE) images; D, E: The long intimal tear was identified at the ascending aorta posterior to the protrusion from the false lumen on different VIE visualizations. Pleural effusion is present at both sides on 2D axial images.
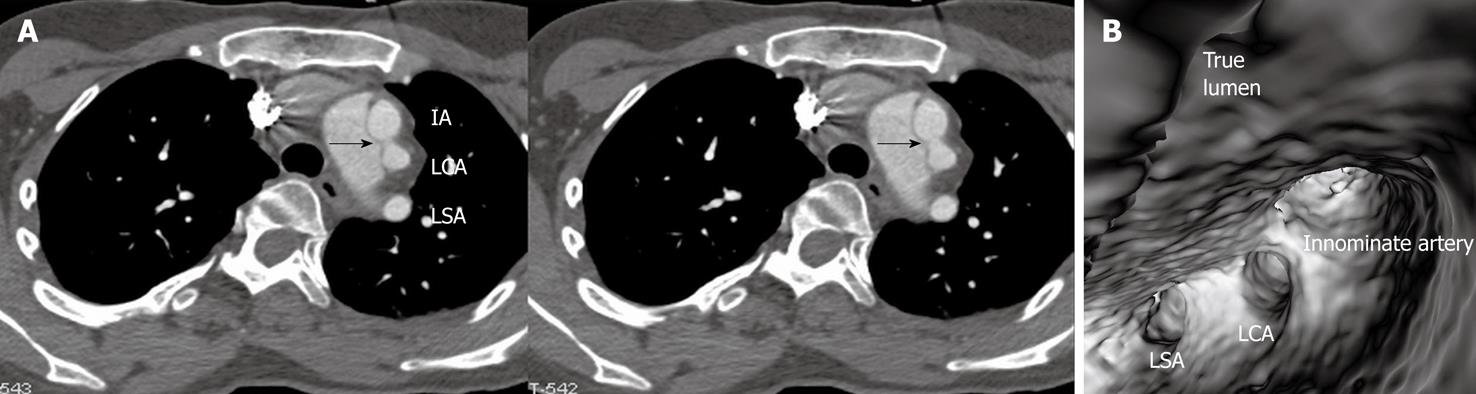
Figure 7 Stanford type A dissection with involvement of the three main artery branches on 2D axial image (A).
Virtual intravascular endoscopy confirms that these three branches arise from the narrowed true lumen (B). Arrows in A indicate the intimal flap. LSA: Left subclavian artery; LCA: Left common carotid artery; IA: Innominate artery.
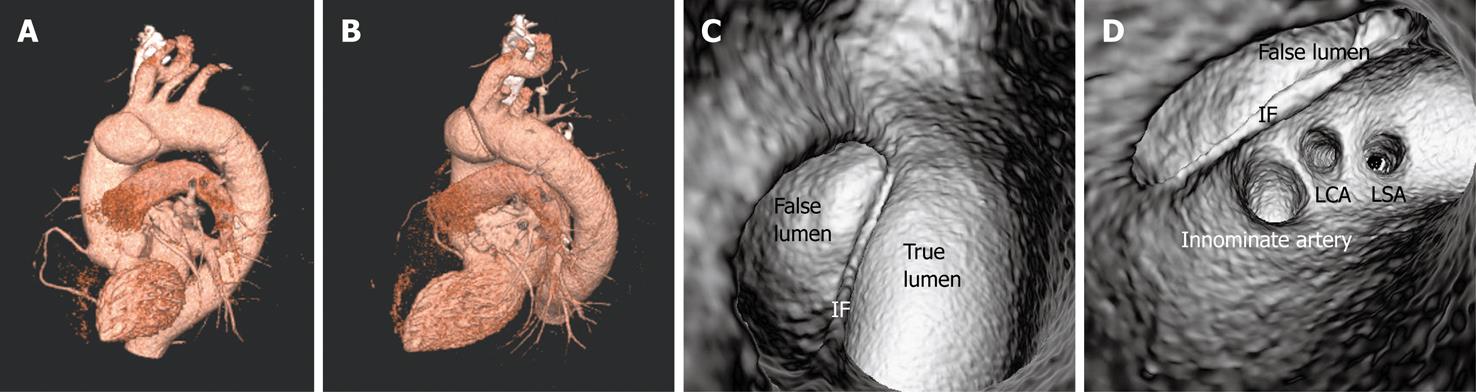
Figure 8 Figure 8 Stanford type A dissection is restricted to the ascending aorta on 3D volume rendering images (A, B).
Both true and false lumens are clearly demonstrated on virtual intravascular endoscopy (VIE) visualization and these two lumens are separated by an intimal flap (IF) (C). The three main artery branches are perfused by the true lumen as shown on VIE view (D). LSA: Left subclavian artery; LCA: Left common carotid artery.
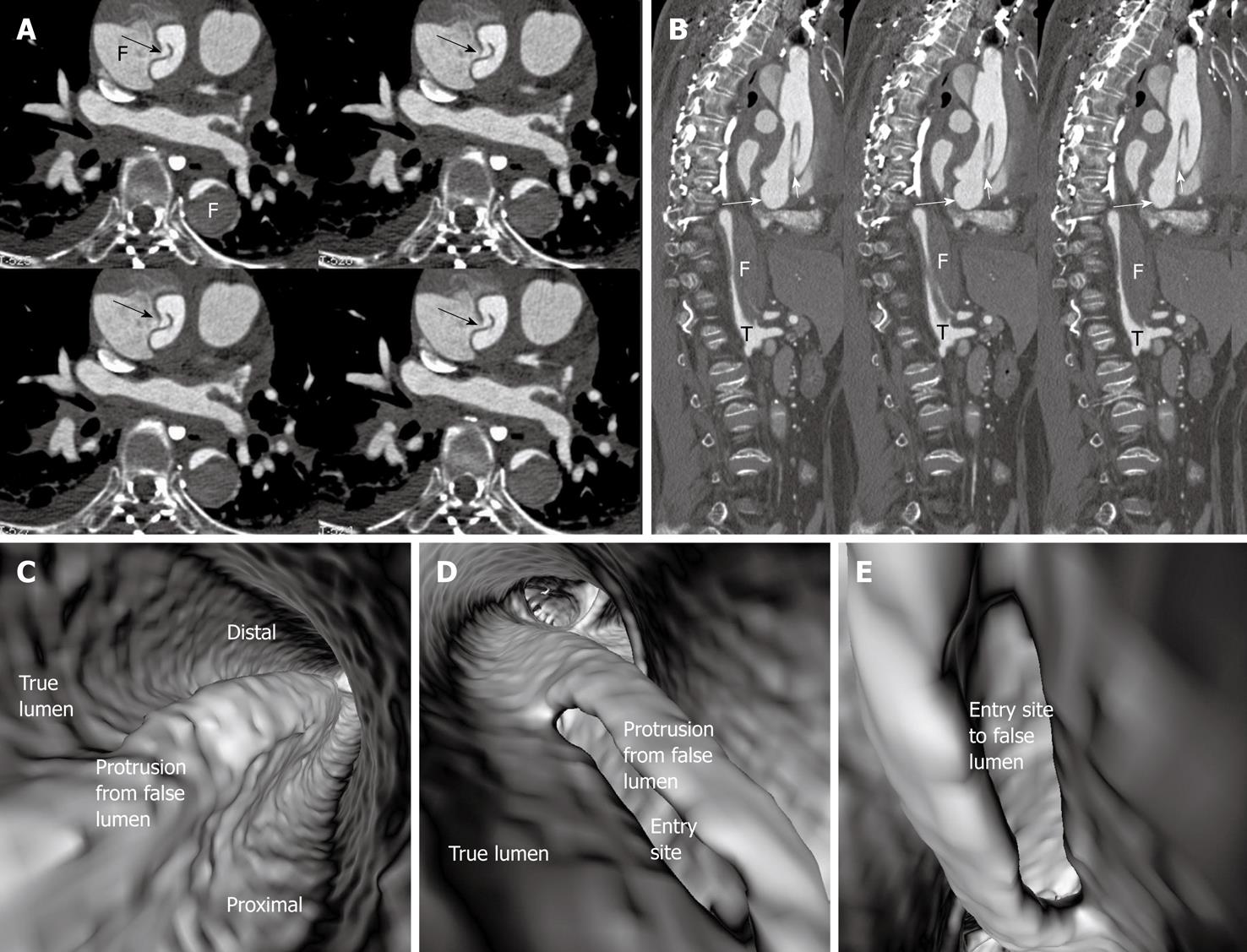
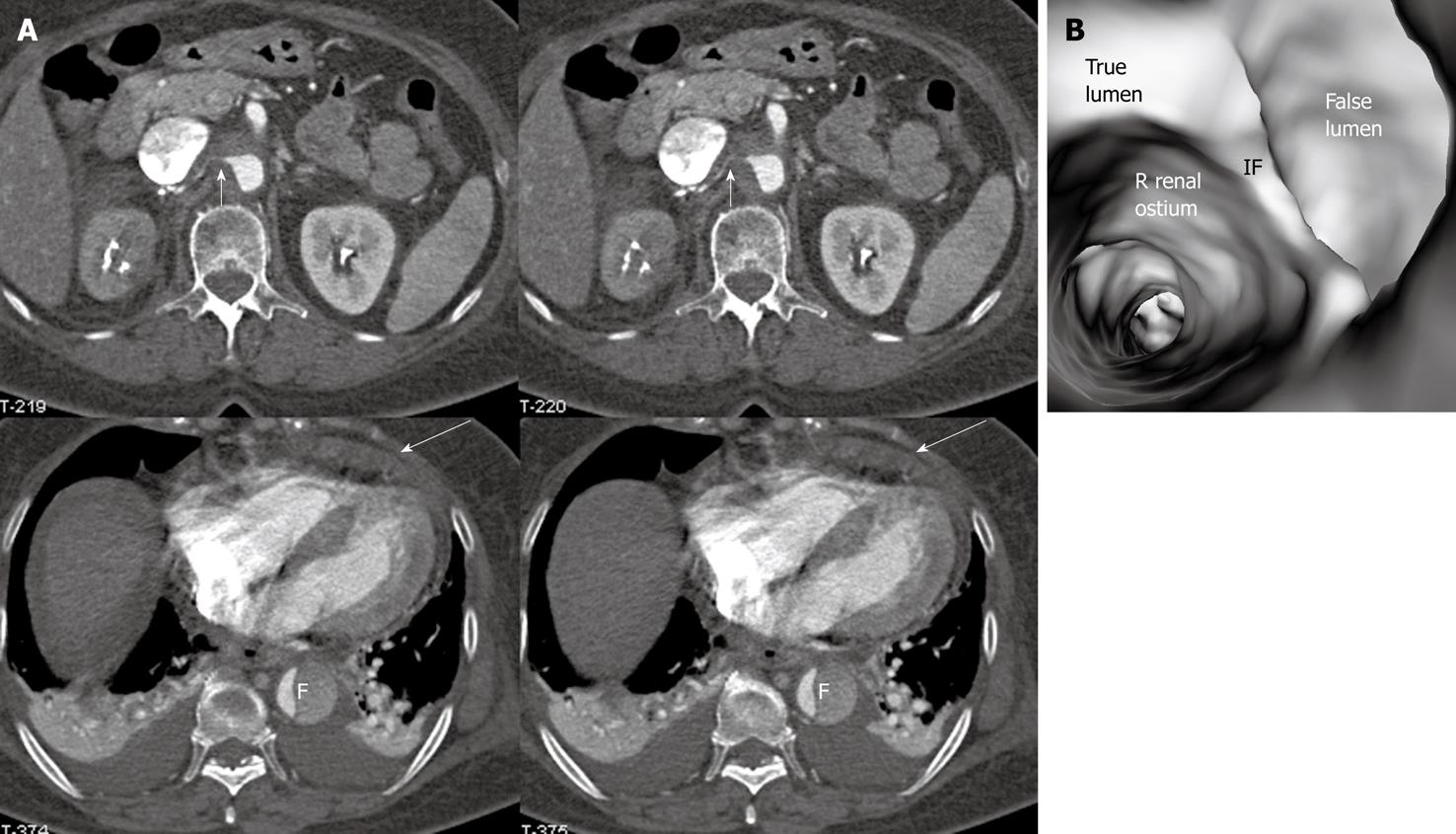
Figure 9 Stanford type B dissection with the true lumen much smaller than the false lumen.
The right renal artery arises from the compressed true lumen resulting in right renal infarction (A). Virtual intravascular endoscopy confirms the origin of the right renal ostium coming from the true lumen which is separated from the false lumen (F) by an intimal flap (IF) (B). Short arrows in A indicate the right renal artery, while long arrows in A refer to pericardial effusion. Pleural effusion is also present at both sides.
Figure 10 Stanford type A dissection with three aortic branches arising from the true lumen.
An irregular intimal flap is displayed on virtual intravascular endoscopy visualization (B). A cob-web sign (short arrows) is noticed in the false lumen (F) on 2D axial image (A). Long arrows indicate the intimal flap. T: True lumen; LSA: Left subclavian artery; LCA: Left common carotid artery.
Figure 11 Stanford type A dissection with appearance of a beak sign (arrows) extending from the false lumen to surround the true lumen.
The true lumen (T) is smaller than the false lumen (F). Bilateral pleural effusion is also noticed on 2D images.
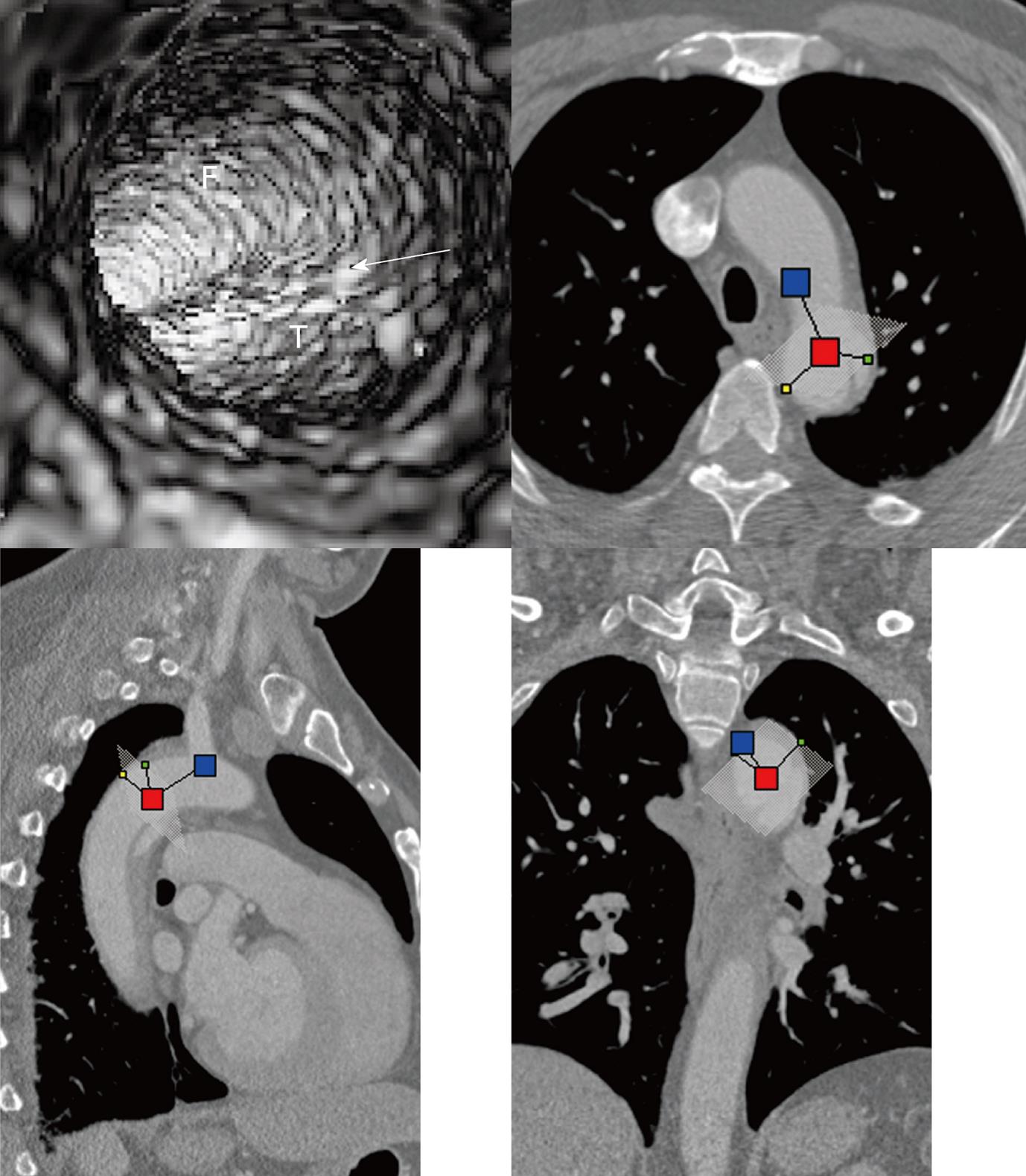
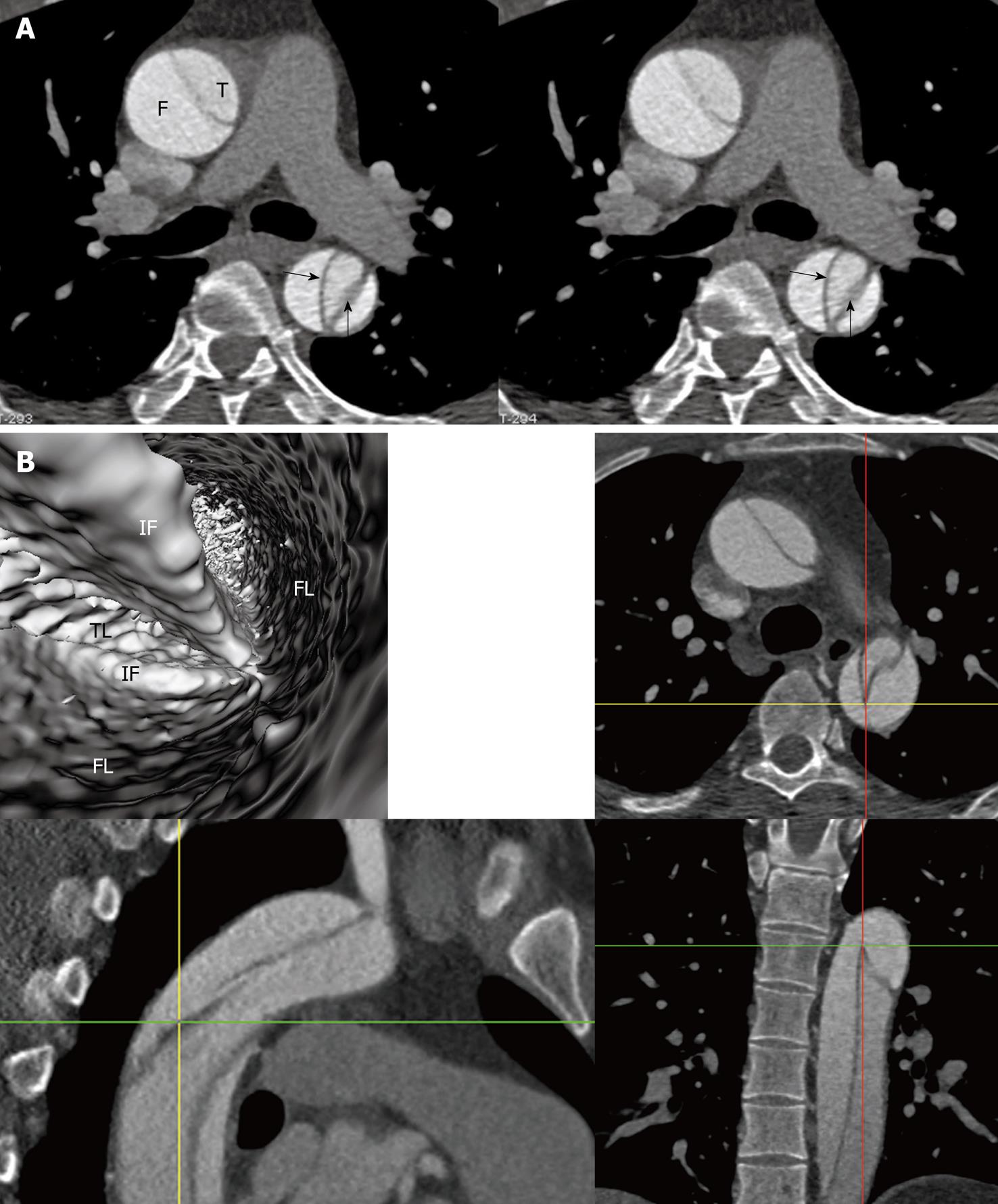
Figure 12 Stanford type A dissection with appearance of intimointimal intussusception (arrows in A).
Corresponding virtual intravascular endoscopy shows the centrally narrowed true lumen (TL) was surrounded by the false lumen (FL) and separated by two intimal flaps (IF). The exact position of the VIE view is confirmed by the orthogonal views which are shown in B.
- Citation: Sun Z, Cao Y. Multislice CT virtual intravascular endoscopy of aortic dissection: A pictorial essay. World J Radiol 2010; 2(11): 440-448
- URL: https://www.wjgnet.com/1949-8470/full/v2/i11/440.htm
- DOI: https://dx.doi.org/10.4329/wjr.v2.i11.440