Published online Jun 27, 2025. doi: 10.4240/wjgs.v17.i6.103030
Revised: March 22, 2025
Accepted: May 8, 2025
Published online: June 27, 2025
Processing time: 93 Days and 4.2 Hours
Appendicitis is an abdominal medical emergency and can be of various types. It can lead to a series of gastrointestinal symptoms and can affect health status. Therefore, attention should be paid to the diagnosis of appendicitis to improve prognosis.
To assess the value of transabdominal superficial ultrasonography (TASU) in the clinical diagnosis of various types of appendicitis.
A total of 100 patients suspected to have acute appendicitis that were admitted to our hospital between July 2022 and July 2024 were selected for this study. All of them underwent conventional abdominal ultrasonography and TASU. Taking surgical pathology as the gold standard, the diagnostic efficacy of the two ultra
Comparison with the gold standard showed that among the 100 patients su
TASU can accurately diagnose appendicitis and also be used to identify the various types of appendicitis, thereby having application value.
Core Tip: This study demonstrates the diagnostic superiority of transabdominal superficial ultrasonography (TASU) in iden
- Citation: Yue YZ, Hu Q, Lu TX. Diagnostic efficacy, imaging characteristics, and detection accuracy of transabdominal superficial ultrasonography for various types of appendicitis. World J Gastrointest Surg 2025; 17(6): 103030
- URL: https://www.wjgnet.com/1948-9366/full/v17/i6/103030.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i6.103030
Acute appendicitis is a severe and sudden onset abdominal condition that can present at any age and has a slightly higher incidence in men. The appendix is a slender blind tube harboring a large number of microorganisms, is rich in lymphatic tissue, and carries a high risk of infection. The exact cause of acute appendicitis is unknown, while lumen obstruction and bacterial invasion are major factors that are also related to congenital appendiceal dysplasia and gastrointestinal dysfunction. A contaminated diet and low immunity can also increase the risk of this disease[1,2]. Most patients have right lower quadrant pain, which can be transferred to other parts of the abdomen. Some patients may have gastrointestinal symptoms, such as anorexia, nausea and vomiting. In severe cases, patients may have a high fever and an elevated heart rate. A failure to diagnose this disease in time may delay the optimal treatment opportunity, trigger complications such as an abdominal abscess and internal or external fistula, and affect the activities of daily life[3]. Surgical pathology is the gold standard for the diagnosis of this disease, but accurately diagnosing the disease may lead to tissue trauma and makes it difficult to predict the diagnosis in advance because histopathology is carried out after the surgery. Abdominal ultrasonography is the main diagnostic method for appendicitis, having the advantages of a simple protocol, strong repeatability, and low cost. It can determine the shape, size, and location of the lesion. However, conventional abdominal ultrasonography lacks clear definitions of the scanning range and key observation areas in different scanning directions (transverse, longitudinal, and oblique views), which may affect the comprehensiveness and accuracy of diagnosis. Additionally, because conventional abdominal ultrasonography has a low probe frequency and limited resolution, it can result in a missed or misdiagnosis[4,5]. Abdominal superficial ultrasonography uses a high-frequency probe for examination and is a non-invasive imaging technique. It is suitable for evaluating superficial organs and tissue lesions, such as endometriosis. Compared with conventional ultrasonography, it significantly improves image clarity[6,7]. However, abdominal superficial ultrasonography currently lacks a standardized quantitative definition of “moderate compression”. Variations in compression applied by different clinicians may affect image quality and diagnostic outcomes. In this report, we have discussed the diagnostic value of abdominal superficial ultrasonography for diagnosing various types of appendicitis. We have also analyzed the ultrasonographic image characteristics of different types of acute appendicitis.
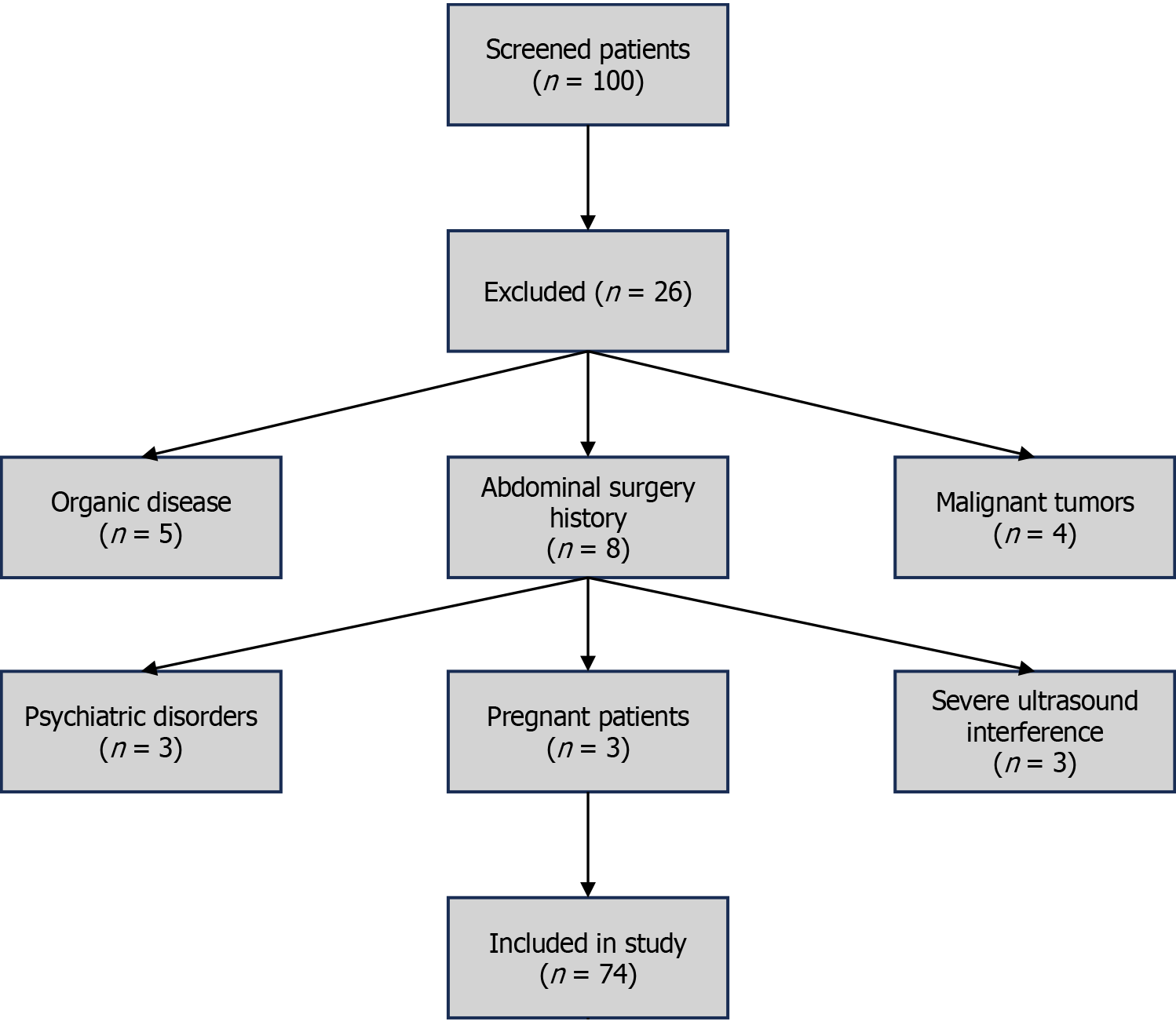
From July 2022 to July 2024, our hospital screened a total of 100 patients suspected of acute appendicitis, including 53 men and 47 women, aged between 18-70 years, with a mean age of 44.72 ± 8.16 years (see Figure 1). The body mass index ranged from 18-26 kg/m², with a mean body mass index value of 22.12 ± 1.54 kg/m2. Those patients who met the following criteria were included in the present study: (1) Age ≥ 18 years old; (2) Accompanied by upper abdominal pain, nausea and vomiting, consistent with the clinical manifestations of acute appendicitis; (3) Can tolerate abdominal ultrasonographic examination and was able to cooperate with the examination process; and (4) The clinical data of the patient were complete, including medical history, laboratory tests, imaging examination results, and surgical/pathological follow-up. A total of 26 patients did not meet the inclusion criteria, the exclusion criteria were as follows: (1) Patients with organic disease (n = 5), namely, patients with severe cardiovascular disease (such as congestive heart failure), severe liver and kidney dysfunction (such as end-stage renal disease), diabetes, and ketoacidosis which affected the reliability of disease judgment and study data; (2) A history of abdominal trauma or surgery (n = 8) including open surgery and laparoscopic surgery (due to possible formation of abdominal adhesions after surgery that affected the interpretation of ultrasonographic imaging); (3) Patients with malignant tumors (n = 4): Including previously or currently diagnosed gastrointestinal tumors and pelvic malignant tumors, in order to avoid interference with ultrasonographic examination results owing to these lesions; (4) Psychiatric patients (n = 3): Including those diagnosed with schizophrenia, bipolar disorder, and severe depression who may not have been able to accurately express symptoms or cooperate with examinations; (5) Pregnant patients (n = 3): Pregnant women who may exhibit physiological abdominal changes, such as uterine enlargement leading to changes in the position of the appendix, which would affect the accuracy of ultrasonography imaging; and (6) Serious ultrasonography interference factors (n = 3): Including severe intestinal distension, and ascites that may have led to poor ultrasonographic image quality and resulted in an inability to obtain reliable imaging data.
Routine abdominal ultrasonography examination: We employed a fully digital color Doppler ultrasonography diagnostic system (registration certificate number: Guangdong Equipment Registration 20182060115; Model specification: Remote location 8G). The frequency of the abdominal ultrasonography probe was set to 1-5 MHz. The patient was placed in a supine position, relaxing the abdominal muscles to reduce interference from intestinal gas. If necessary, patients were instructed to lie on their side or change positions to optimize imaging. After applying an appropriate amount of coupling agent to the probe, the operator scanned the blind area horizontally, vertically, and diagonally in sequence to ensure a complete coverage of the appendix. Observational content: The position, length, diameter, and course of the appendix were observed to assess echogenicity, check whether the lumen was unobstructed, and if the structure of the tube wall was intact. The presence of fluid accumulation, intestinal dilation, or free gas in the abdominal cavity around the appendix were recorded. In case of intestinal gas interference, the operator gently pressed the probe or adjusted the position of the patient to optimize imaging quality.
Abdominal superficial ultrasonography examination: The probe frequency was set to 5-12 MHz, and a high-frequency linear array probe was used for examination. As a key scanning site, the ileocecal area was used to evaluate the surrounding tissue structure, including the fat layer around the appendix and the related lymph nodes. The operator applied coupling agent on the ileocecal surface and moderately compressed the probe (pressure controlled at about 2-3 N) to reduce intestinal gas interference and improve the clarity of appendiceal imaging. The operator observed whether fluid accumulation was apparent in the appendix lumen, assessed the stratification of the appendix wall, and measured the inner diameter of the lumen (normal ≤ 6 mm, abnormal > 6 mm). Color Doppler flow imaging was employed to observe the blood flow signals around the appendix wall, record the enhancement or absence of blood flow, and to evaluate the degree of inflammation that included thickening of the appendix wall, peripheral exudation, and abnormal local echoes.
Image analysis: After the acquisition of ultrasonographic images was complete, all ultrasonographic images were analyzed independently by two ultrasonography clinicians with more than 3 years of clinical experience to ensure the reliability of image analysis. We employed blind analysis, namely, the clinicians were kept unaware of the pathological findings while they analyzed images to avoid bias. The two clinicians recorded the following information: (1) Appendix size and morphology, and inflammatory manifestations (wall thickening, luminal dilation, fluid accumulation); (2) Blood flow signal intensity and distribution characteristics; and (3) Abnormal echoes of surrounding tissues and the presence of abdominal fluid accumulation. If the conclusions drawn by the two clinicians differed from each other, these differences were resolved by mutual discussion to arrive at a final diagnostic conclusion. For image analysis, we employed the intra-group correlation coefficient to quantify the observer reliability between the two clinicians to ensure consistency and accuracy in image interpretation. Prior to undertaking this study, we conducted a statistical analysis of the diagnostic characteristics of the two clinicians, and all intra-group correlation coefficient values were found to be above 0.60, indicating that the diagnostic consistency between the two ultrasonography clinicians was statistically significant (P values were both less than 0.05).
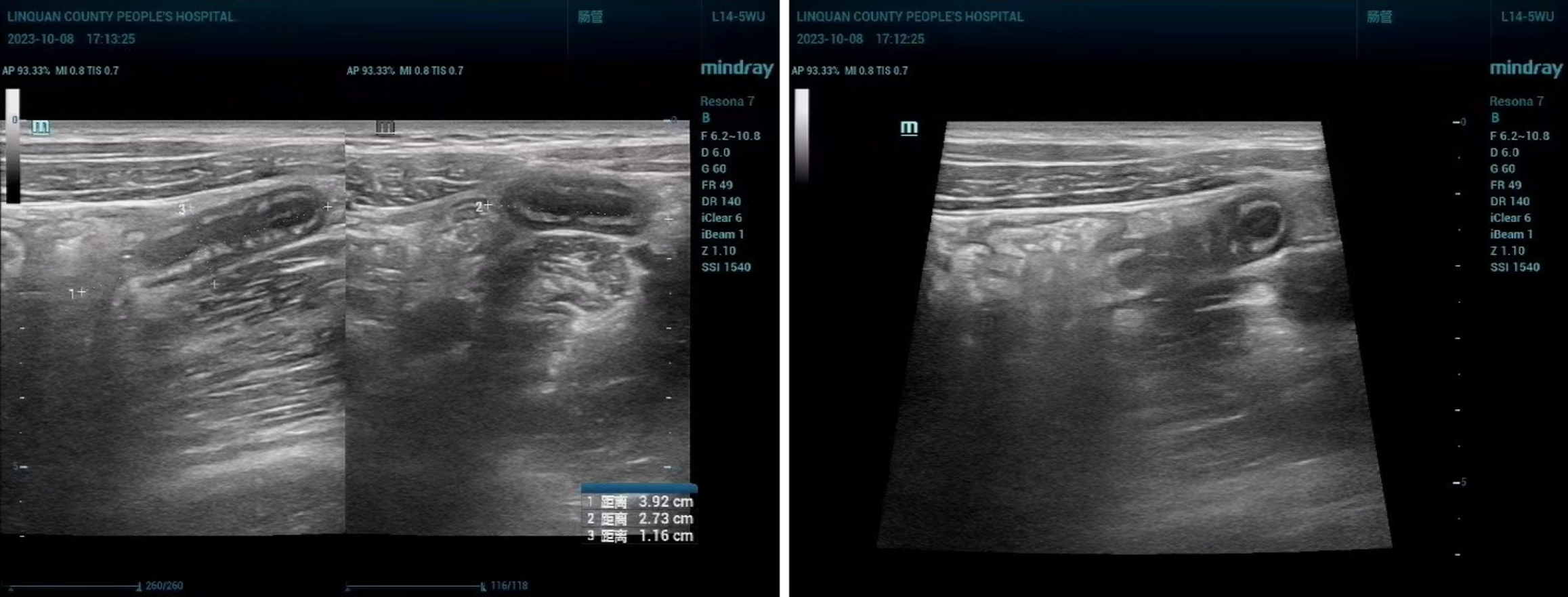
Outcome indicators: (1) Diagnostic efficiency of two ultrasonography methods: Taking surgical pathology as the diagnostic gold standard, we compared the diagnostic efficacy (sensitivity, specificity, accuracy, positive and negative predictive value) of conventional abdominal ultrasonography and transabdominal superficial ultrasonography (TASU) in the diagnosis of acute appendicitis. Judgment basis[8]: The pathological examination results showed appendiceal swelling and conjunctival congestion, accompanied by exudate and neutrophil infiltration, while an effusion could be observed in the appendiceal cavity in some patients. Abdominal ultrasonography showed the following: An enlarged appendix; the lumen had expanded and the wall thickness had increased; appendiceal cavity occlusion or a stercoral shadow was visible; the appendix had cystic mass and was accompanied by fluid collection; (2) Comparison of the diagnostic efficacy of the two ultrasonography methods (see Figure 2): The surgical and pathological results were set as the gold standard, and the diagnostic efficacy of conventional abdominal ultrasonography and TASU for acute simple appendicitis was compared. Judgment basis: Pathological examination findings showed a mild swelling of the appendix, and the lesion could be seen only in the mucosa and its underlying layers, accompanied by neutrophil infiltration. Abdominal ultrasonography showed a clear image boundary, which was difficult to distinguish from the normal tissue. The appendix was significantly thickened, with a thickened mucosa. The transverse lumen showed “concentric circles”, and the longitudinal section was “sausage-like”; (3) Comparison of the diagnostic efficacy of the two ultrasonography methods: Surgical pathology was set as the gold standard for diagnosis, and the diagnostic efficacy of conventional abdominal ultrasonography and TASU was compared for acute suppurative appendicitis. Judgment basis: Pathological examination showed an obvious swelling of the appendix, serosal congestion, pus extravasation, muscular layer and serosal layer involvement, and fluid accumulation in the appendiceal cavity. Abdominal ultrasonography showed that the appendix had become thick, and the definition of the boundary with the normal tissue was reduced. A cystic hypoecho with an irregular shape could be observed, and the echo inside the lesion was dense and distributed in dots. The transverse lumen showed a “target ring-like”, and “rat-tail-like” shape as seen through longitudinal section; (4) Comparison of the diagnostic efficacy of the two ultrasonography methods: Setting surgical pathology as the diagnostic gold standard, we compared the diagnostic efficacy of conventional abdominal ultrasonography and TASU for diagnosing acute gangrenous appendicitis. Judgment basis: Pathological examination results showed necrosis of the appendiceal wall in a black or dark purple color, with fluid collection, increased pressure, and abnormal blood supply to the surrounding tissues in the lumen. Abdominal ultrasonography showed morphological changes and obvious swelling of the appendix. The appendiceal tube wall was thickened and indistinct in level. The echoes in the cavity were dense and distributed in dots. The liquid echo was cloudy. The surrounding tissues were obviously exuded and accompanied by adhesion; and (5) Diagnostic consistency analysis: We analyzed the diagnostic consistency of TASU and pathological examination in acute appendicitis as well as various types of acute appendicitis. The consistency was found to be poor when Kappa < 0.4, medium when 0.4 ≤ Kappa ≤ 0.75 and high when Kappa > 0.75.
The data were analyzed by SPSS 22.0 statistical software, and the results were expressed as percentages (%). The enumeration data were tested by the χ2 test, and P < 0.05 indicated a statistically significant difference in comparisons.
Pathological examination post-surgery showed that among the 100 patients suspected of appendicitis, 72 cases were diagnosed as acute appendicitis (positive), and 28 cases were deemed to be normal (negative). The diagnostic efficacy of TASU for the diagnosis of acute appendicitis was higher than that of conventional abdominal ultrasonography (P < 0.05) (Table 1).
| Diagnostic method | Nature | Gold standard (units) | Sensitivity (%) | Specificity (%) | Accuracy (%) | Positive predictive value (%) | Negative predictive value (%) | |
| Positive | Negative | |||||||
| Conventional abdominal ultrasonography | Positive | 60 | 10 | 83.33 | 64.29 | 78.00 | 85.71 | 60.00 |
| Negative | 12 | 18 | ||||||
| Transabdominal superficial ultrasonography | Positive | 70 | 2 | 97.22 | 92.86 | 96.00 | 97.22 | 92.86 |
| Negative | 2 | 26 | ||||||
| χ2 | - | - | - | 7.912 | 6.778 | 14.324 | 6.076 | 8.539 |
| P value | - | - | - | 0.005 | 0.009 | < 0.001 | 0.014 | 0.003 |
Surgical pathology revealed that among the 72 patients diagnosed with appendicitis, 22 cases exhibited acute simple appendicitis (positive) and 50 cases represented other types of disease (negative). The diagnostic efficacy of TASU for the diagnosis of acute simple appendicitis was higher than that of conventional abdominal ultrasonography (P < 0.05) (Table 2).
| Diagnostic method | Nature | Gold standard (units) | Sensitivity (%) | Specificity (%) | Accuracy (%) | Positive predictive value (%) | Negative predictive value (%) | |
| Positive | Negative | |||||||
| Conventional abdominal ultrasonography | Positive | 13 | 11 | 59.09 | 78.00 | 72.22 | 54.17 | 81.25 |
| Negative | 9 | 39 | ||||||
| Transabdominal superficial ultrasonography | Positive | 20 | 3 | 90.91 | 94.00 | 93.06 | 86.96 | 95.92 |
| Negative | 2 | 47 | ||||||
| χ2 | - | - | - | 5.939 | 5.316 | 10.891 | 6.038 | 5.189 |
| P value | - | - | - | 0.015 | 0.021 | 0.001 | 0.014 | 0.023 |
Surgical pathology revealed that among the 72 patients diagnosed with appendicitis, 26 cases exhibited acute suppurative appendicitis (positive) and 46 cases represented other types of appendicitis (negative). The diagnostic efficacy of TASU for the diagnosis of acute suppurative appendicitis was higher than that of conventional abdominal ultrasonography (P < 0.05) (Table 3).
| Diagnostic method | Nature | Gold standard (units) | Sensitivity (%) | Specificity (%) | Accuracy (%) | Positive predictive value (%) | Negative predictive value (%) | |
| Positive | Negative | |||||||
| Conventional abdominal ultrasonography | Positive | 16 | 12 | 61.54 | 73.91 | 69.44 | 57.14 | 77.27 |
| Negative | 10 | 34 | ||||||
| Transabdominal superficial ultrasonography | Positive | 24 | 3 | 92.31 | 93.48 | 93.06 | 88.89 | 95.56 |
| Negative | 2 | 43 | ||||||
| χ2 | - | - | - | 6.933 | 6.452 | 13.174 | 6.984 | 6.375 |
| P value | - | - | - | 0.008 | 0.011 | < 0.001 | 0.008 | 0.012 |
Surgical pathology revealed that among the 72 patients diagnosed with appendicitis, 24 cases exhibited acute gangrenous appendicitis (positive) and 48 cases represented other types of appendicitis (negative). The diagnostic efficacy of TASU for the diagnosis of acute gangrenous appendicitis was higher than that of conventional abdominal ultrasonography (P < 0.05) (Table 4).
| Diagnostic method | Nature | Gold standard (units) | Sensitivity (%) | Specificity (%) | Accuracy (%) | Positive predictive value (%) | Negative predictive value (%) | |
| Positive | Negative | |||||||
| Conventional abdominal ultrasonography | Positive | 15 | 8 | 62.50 | 83.33 | 76.39 | 65.22 | 81.63 |
| Negative | 9 | 40 | ||||||
| Transabdominal superficial ultrasonography | Positive | 23 | 1 | 95.83 | 97.92 | 97.22 | 85.83 | 97.92 |
| Negative | 1 | 47 | ||||||
| χ2 | - | - | - | 8.084 | 6.008 | 13.642 | 7.111 | 6.954 |
| P value | - | - | - | 0.004 | 0.014 | < 0.001 | 0.008 | 0.008 |
The TASU and pathological examination findings were highly consistent for various types of acute appendicitis, namely acute appendicitis, acute simple appendicitis, acute suppurative appendicitis, and acute gangrenous appendicitis (Kappa = 0.901, P < 0.001; Kappa = 0.838, P < 0.001; Kappa = 0.851, P < 0.001; Kappa = 0.938, P < 0.001, respectively).
Acute appendicitis is a commonly occurring severe and sudden onset abdominal disease, characterized by pain in the lower right abdomen that can radiate to other areas, accompanied by symptoms such as fever and gastrointestinal discomfort. In severe cases, it can lead to complications such as perforation and peritonitis, affecting the normal life of the patient. In addition, different types of acute appendicitis have different treatment plans, so it is necessary to pay attention to preoperative classification and differential diagnosis of the disease. Although pathological examination is the gold standard for the diagnosis of acute appendicitis, it is traumatic, cannot be applied repeatedly, and can only be performed during or after surgery, with certain delays and application limitations[9,10]. Ultrasonographic examination is a widely used imaging method that observes visceral anatomical structures and pathological states through the reflection of ultrasonography waves that travel between human tissues. It has the advantages of high safety, real-time imaging, and low cost, and plays an important role in the diagnosis and efficacy evaluation of various diseases[11]. Conventional abdominal ultrasonography is one of the commonly used types of ultrasonographic examination, with strong penetrating power. It can be used to measure the length of the appendix and the extent of lesions for the diagnosis of acute appendicitis[12]. However, conventional abdominal ultrasonography has a low resolution and limited diagnostic value in near-field scanning, making it difficult to clearly display the hierarchical structure of the appendix wall, resulting in insufficient detection accuracy for small and superficial lesions.
TASU combines the characteristics of abdominal ultrasonography and superficial ultrasonography. The latter is primarily used for the examination of superficial organ lesions and has the advantages of high sensitivity, high safety, and easy operation. It is widely used for the diagnosis of diseases such as arthritis, tenosynovitis, hemangiomas, and testicular torsion. TASU uses high-frequency probes with high resolution, which can clearly display the hierarchical structure of the appendix wall and evaluate wall structure and intracavitary status. Compared with traditional abdominal ultrasonography, TASU can more accurately detect small lesions and mild inflammation, improving diagnostic accuracy[13]. The appendix is elongated and curved, with a normal length of about 7-9 cm and a lumen diameter of only 0.2 cm. When the cavity is blocked, the pressure increases, and bacteria invade: This may affect the blood supply of the appendiceal tissue, thereby inducing disease. There is no obvious swelling in the cavity in the case of acute simple appendicitis, which is characterized by thickening of the tube wall, clear boundaries, an absence of echo in the cavity, and the presence of strong echo fecal stones[14,15]. The appendix in the case of acute suppurative appendicitis is significantly swollen, with increased tension, an intracavity diameter greater than 10 mm, thickening of the wall, decreased surface smoothness, and a dense echogenicity distributed in dots, which is difficult to distinguish from surrounding tissues. The appendix wall of acute gangrenous appendicitis displays further thickening, continuous interruption, and blurred boundaries with the surrounding normal tissues. Low echo areas can be seen inside the cavity, with uneven echoes and scattered strong echoes. An echo-less mass can be seen in the lower right abdomen, accompanied by adhesions with surrounding tissues[16,17]. Compared with other imaging examinations, TASU has higher safety and real-time perfor
In summary, TASU combines the advantages of superficial ultrasonography and abdominal ultrasonography and can clearly display the anatomical structure and pathological characteristics of the appendix, making it particularly suitable for detecting mild inflammation and small lesions. Its high sensitivity performs better in the diagnosis of adult patients than conventional abdominal ultrasonography. However, further research is needed to optimize its application in pediatric patients and to complement CT/MRI in clinical practice to guide clinical decision-making more accurately. The limitation of this study is that the diagnostic efficacy of ultrasonographic examination is greatly affected by the operator experience and equipment performance, especially in identifying complex or atypical acute appendicitis, which still poses certain difficulties. In addition, the lack of a systematic evaluation of imaging characteristics in patients of different body types may affect the broad applicability of the study. Future research should further optimize the standardized process of ultrasonographic examination, improve image quality in different scanning directions, and incorporate artificial intelligence image analysis technology to enhance the accuracy and consistency of diagnosis. At the same time, the sample size can be expanded to explore the potential application of ultrasonography in the classification and prediction of appendicitis.
In summary, TASU can accurately diagnose acute appendicitis, play a role in the assessment of various types of appendicitis, and possesses promotional value.
| 1. | Dai Z, Liu J, Chen L. Clinical characteristics and application value of risk prediction models of acute appendicitis in rural Tibet: a retrospective study. Rural Remote Health. 2023;23:7709. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 2. | Castro P, Rincón J, Sánchez C, Molina I, Buitrago G. Presurgical time and associated factors as predictors of acute perforated appendicitis: a prospective cohort study in a teaching pediatric hospital in Colombia. BMC Pediatr. 2022;22:49. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 3. | Fransvea P, Fico V, Cozza V, Costa G, Lepre L, Mercantini P, La Greca A, Sganga G; ERASO study group. Clinical-pathological features and treatment of acute appendicitis in the very elderly: an interim analysis of the FRAILESEL Italian multicentre prospective study. Eur J Trauma Emerg Surg. 2022;48:1177-1188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 4. | Lv X, Zhang Y. Comparative observation on the accuracy of ultrasonography and CT in preoperative diagnosis of acute appendicitis in children. Minerva Pediatr (Torino). 2022;74:97-99. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 5. | Pedersen MRV, Østergaard ML, Nayahangan LJ, Nielsen KR, Lucius C, Dietrich CF, Nielsen MB. Simulation-based education in ultrasound - diagnostic and interventional abdominal focus. Ultraschall Med. 2024;45:348-366. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 6. | Guidry RF, McCarthy ME, Straughan DM, St Hilaire H, Schuster JD, Dancisak M, Lindsey JT. Ultrasound Imaging of the Superficial Fascial System Can Predict the Subcutaneous Strength of Abdominal Tissue Using Mean Gray Value Quantification. Plast Reconstr Surg. 2020;145:1173-1181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Avery JC, Deslandes A, Freger SM, Leonardi M, Lo G, Carneiro G, Condous G, Hull ML; Imagendo Study Group. Noninvasive diagnostic imaging for endometriosis part 1: a systematic review of recent developments in ultrasound, combination imaging, and artificial intelligence. Fertil Steril. 2024;121:164-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 16] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 8. | Hoffmann JC, Trimborn CP, Hoffmann M, Schröder R, Förster S, Dirks K, Tannapfel A, Anthuber M, Hollerweger A. Classification of acute appendicitis (CAA): treatment directed new classification based on imaging (ultrasound, computed tomography) and pathology. Int J Colorectal Dis. 2021;36:2347-2360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 9. | Morley EJ, Bracey A, Reiter M, Thode HC Jr, Singer AJ. Association of Pain Location With Computed Tomography Abnormalities in Emergeny Department Patients With Abdominal Pain. J Emerg Med. 2020;59:485-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | de Almeida Leite RM, Seo DJ, Gomez-Eslava B, Hossain S, Lesegretain A, de Souza AV, Bay CP, Zilberstein B, Marchi E, Machado RB, Barchi LC, Ricciardi R. Nonoperative vs Operative Management of Uncomplicated Acute Appendicitis: A Systematic Review and Meta-analysis. JAMA Surg. 2022;157:828-834. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 54] [Article Influence: 18.0] [Reference Citation Analysis (102)] |
| 11. | Shtina IE, Ivashova YA, Mamykina NI, Ustinova OY. [State of the hepatobiliary system on the data of ultrasonic examination in children and adolescents with overweight and obesity]. Vopr Pitan. 2023;92:60-70. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 12. | Lazow SP, Tracy SA, Staffa SJ, Estroff JA, Parad RB, Castro-Aragon IM, Fujii AM, Zurakowski D, Chen C. Abdominal ultrasound findings contribute to a multivariable predictive risk score for surgical necrotizing enterocolitis: A pilot study. Am J Surg. 2021;222:1034-1039. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 13. | Morel B, Hellec C, Fievet A, Taveau CS, Abimelech M, Dujardin PA, Brunereau L, Patat F. Reliability of 3-D Virtual Abdominal Tele-ultrasonography in Pediatric Emergency: Comparison with Standard-of-Care Ultrasound Examination. Ultrasound Med Biol. 2022;48:2310-2321. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (1)] |
| 14. | Fuhrer AE, Sukhotnik I, Ben-Shahar Y, Weinberg M, Koppelmann T. Predictive Value of Alvarado Score and Pediatric Appendicitis Score in the Success of Nonoperative Management for Simple Acute Appendicitis in Children. Eur J Pediatr Surg. 2021;31:95-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 15. | Knaapen M, Hall NJ, Moulin D, van der Lee JH, Butcher NJ, Minneci PC, Svensson JF, St Peter SD, Adams S, Nah SA, Skarsgard ED, Zani A, Emil S, Suominen JS, Aziz DA, Rai R, Offringa M, van Heurn EW, Bakx R, Gorter RR; pediatric appendicitis COS development group. International Core Outcome Set for Acute Simple Appendicitis in Children: Results of a Systematic Review, Delphi Study, and Focus Croups With Young People. Ann Surg. 2022;276:1047-1055. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 16. | Duan C, Li Y, Ma J, Song Y, Zhou L. The Impact of Laparoscopic Appendectomy and Open Appendectomy on B7-H3-Mediated Intrinsic Immune Response in Children with Acute Suppurative Appendicitis. J Inflamm Res. 2024;17:1577-1587. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 17. | Wang B, Shi L, Fu W, Liu T. Effects of Sequence of Irrigation, Suction, and Extraction in Cases of Acute Purulent Appendicitis or Gangrenous Perforated Appendicitis After Laparoscopic Appendectomy. J Laparoendosc Adv Surg Tech A. 2021;31:751-755. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |