Published online May 28, 2025. doi: 10.3748/wjg.v31.i20.105269
Revised: April 18, 2025
Accepted: May 12, 2025
Published online: May 28, 2025
Processing time: 131 Days and 23 Hours
Acute pancreatitis (AP), a severe pancreatic inflammatory condition, with a mor
To evaluate the efficacy of estimated plasma volume status (ePVS) in forecasting AKI in patients with AP.
In this retrospective cohort study, AP cases were recruited from the First College of Clinical Medical Science of China Three Gorges University between January 2019 and October 2023. Electronic medical records were adopted for data extrac
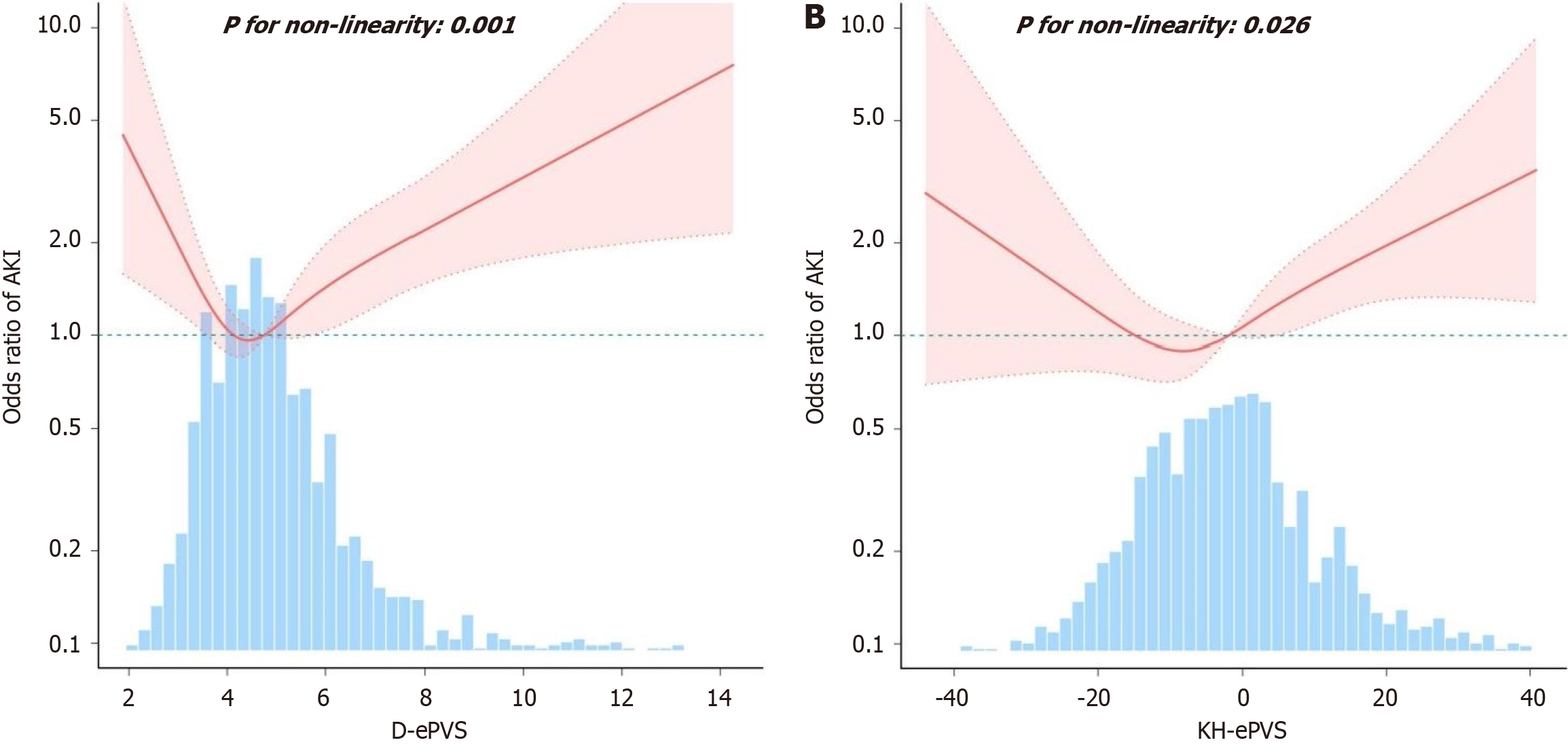
Among the 1508 AP patients, 251 (16.6%) developed AKI. ePVS was calculated using Duarte (D-ePVS) and Kaplan-Hakim (KH-ePVS) formulas. After adjusting for covariates, the AKI risk exhibited 46% [odds ratio (OR) = 1.46, 95% confidence interval (CI): 0.96-2.24] and 11% (OR = 1.11, 95%CI: 0.72-1.72) increases in the low tertile (T1) of D-ePVS and KH-ePVS, respectively, and 101% (OR = 2.01, 95%CI: 1.31-3.05) and 51% (OR = 1.51, 95%CI: 1.00-2.29) increases in the high tertile (T3) relative to the reference tertile (T2). Nonlinear curve fitting revealed a U-shaped association of D-ePVS with AKI and a J-shaped association for KH-ePVS, with inflection points at 4.3 dL/g and -2.8%, res
Our results indicated that ePVS demonstrated the nonlinear association with AKI incidence in AP patients. A U-shaped curve was observed with an inflection point at 4.3 dL/g for the Duarte formula, and a J-shaped curve at -2.8% for the Kaplan-Hakim formula.
Core Tip: This study is the largest to date examining acute kidney injury (AKI) in patients with acute pancreatitis (AP), and it is the first to explore the association between estimated plasma volume status (ePVS) and the incidence of AKI. The study utilized two formulas (Duarte and Kaplan-Hakim) to assess ePVS and its relationship with AKI risk. Through smooth curve fitting analysis, the results revealed a nonlinear relationship between ePVS and AKI risk, including U-shaped and J-shaped curves. These findings provide important reference for the prediction and management of AKI in patients with AP.
- Citation: Wu W, Zhang YP, Zhang YL, Qu XG, Zhang ZH, Zhang R, Peng ZY. Nonlinear association between estimated plasma volume status and acute kidney injury in acute pancreatitis patients. World J Gastroenterol 2025; 31(20): 105269
- URL: https://www.wjgnet.com/1007-9327/full/v31/i20/105269.htm
- DOI: https://dx.doi.org/10.3748/wjg.v31.i20.105269
Acute pancreatitis (AP), a severe pancreatic inflammatory condition, is a frequently seen gastrointestinal disease re
Directly quantifying plasma volume (PV) is challenging, which is considered the gold standard, and requires the administration of radiolabeled tracer molecules[8]. Nevertheless, the approach can be invasive, technically demanding, and impractical in continual clinical application. To address the existing limitations, estimated PV status (ePVS) has been developed as a biomarker. This metric is cost-effective, easily performed through standard blood tests, and time-efficient, demonstrating a strong correlation with radiolabeled albumin (ALB) techniques[9,10]. As it is derived from standard tests conducted at admission, ePVS is readily available, making it highly suitable for clinical application. ePVS is demonstrated as a valuable indicator of fluid status, which correlates well with cardiac filling pressures and hemodynamics[11]. It has also exhibited prognostic value in various clinical scenarios, including heart failure[12-15], dyspnea, fever[16], cardiac surgery[9,17], as well as in the general population[18]. However, based on our knowledge, the PVS prevalence and its association with volume status-related AKI within pancreatitis remains unexplored.
This study investigates the correlation of ePVS with AKI incidence among AP cases for the first time, offering insights for early risk assessment and fluid management strategies in this population.
This retrospective, observational cohort study involving human samples was approved by Hospital of Medicine Ethics Committee (ethical approval number: 2023-130-01). During data processing, patient information was anonymous. This study was performed following Declaration of Helsinki. Patient data were obtained through retrospectively reviewing electronic medical records of AP cases from Yichang Central People’s Hospital, the First College of Clinical Medical Science of China Three Gorges University between January 2019 and October 2023.
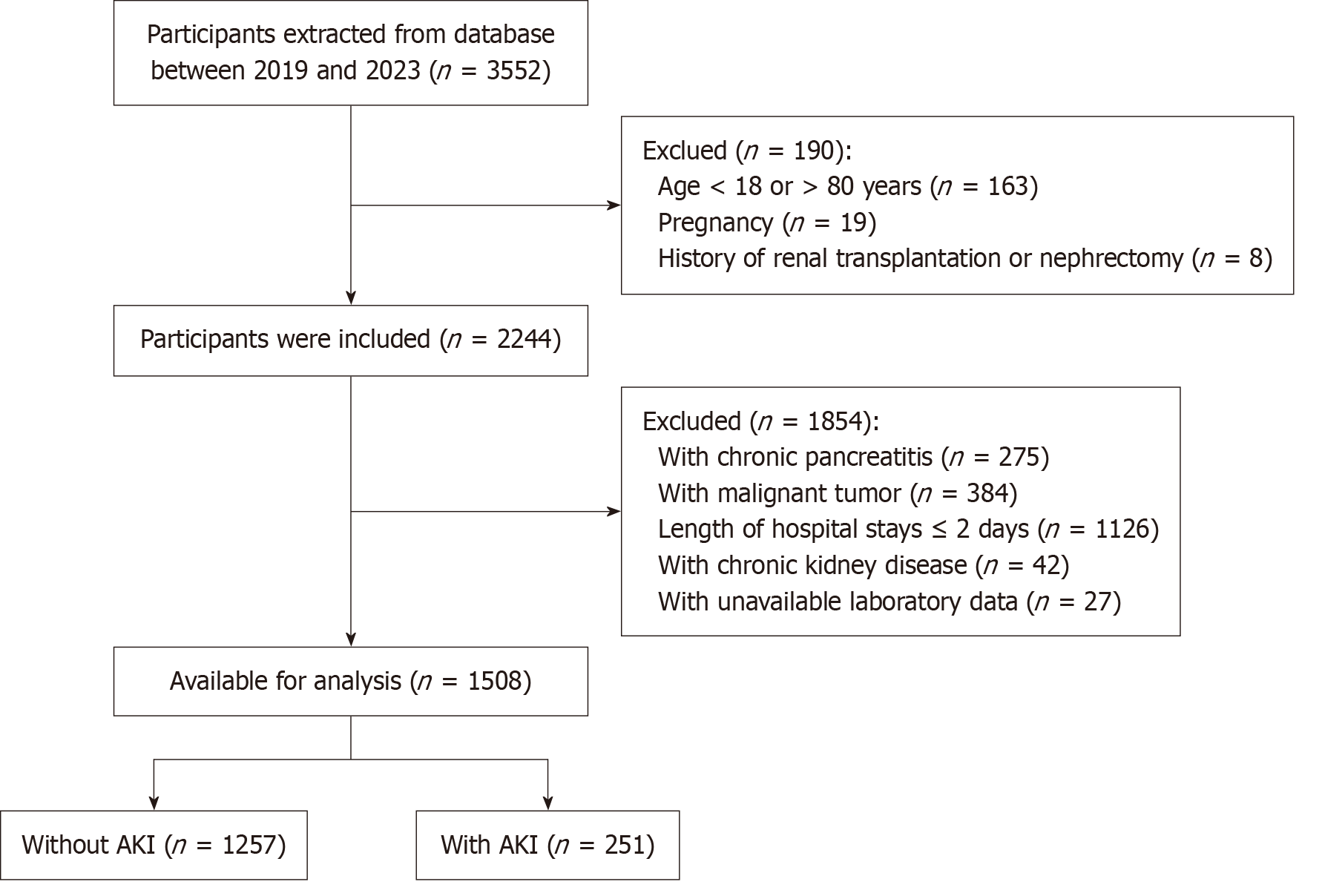
Patients who satisfied the criteria below were included: Inpatients from the First College of Clinical Medical Science of China Three Gorges University; and AP cases. The following patients were excluded: Those aged < 18 or > 80 years; Women during pregnancy or breastfeeding; Those with a hospital stay of ≤ 2 days; Patients with chronic kidney disease; Cancer cases; Those developing chronic pancreatitis; Those undergoing nephrectomy or renal transplantation; Patients with insufficient medical information. Figure 1 shows the patient collection and review process.
The ePVS was performed based on the following two different methodologies: (1) Duarte formula-based ePVS (D-ePVS)[13]: This method employs a single equation: D-ePVS = [100 - hematocrit (%)]/hemoglobin (g/dL); and (2) Kaplan-Hakim formula-based ePVS (KH-ePVS)[11,14,15]: This approach involves the calculation of actual and PVs (aPV and iPV, respectively), and ePVS using the below equations: aPV = [1 - hematocrit (%)] × [a + b × weight (kg)], a = 1530, b = 41 for males, whereas a = 864, b = 47.9 for females; iPV = c × weight (kg), For males: c = 39, for females: c = 40; KH-ePVS = [(aPV - iPV) / iPV] × 100%.
The diagnosis of AP was performed according to symptoms, physical examinations, laboratory results, medical history, and imaging findings (including abdominal ultrasound, contrast-enhanced computed tomography, or magnetic reso
AP severity could be classified according to the revised Atlanta classification. AP with no local/systemic complication or organ failure was deemed as mild, while that accompanied by local/systemic complications, and transient rather than persistent organ failure (which resolved in 2 days) was considered as moderate[21], and AP accompanied by persistent organ failure (single or multiple) lasting for over 48 hours was regarded as severe.
Following the KIDGO guidelines (2012), AKI was diagnosed and classified[22], with the serum creatinine standard as the increase in serum creatinine level ≥ 0.3 mg/dL (≥ 26.4 μmol/L) or the percentage increase by ≥ 50% in 48 hours. In addition, the lowest serum creatinine concentration detected in 48 hours prior to hospital admission was considered as its baseline content. If serum creatinine was not determined, we regarded the concentration during the initial measurement in 48 hours after hospital admission as its level.
General data were collected, including age, gender, body mass index (BMI), history of hypertension, coronary heart disease (CHD), diabetes mellitus (DM), the length of hospital stays (LOS), respiratory rate (RR), heart rate (HR), pulse oxygen saturation (SpO2), and systolic blood pressure (SBP), necessity of blood transfusion, mechanical ventilation (MV) and continuous renal replacement treatment (CRRT), bedside index of severity in AP (BISAP) score, and sequential organ failure assessment (SOFA) score in 24 hours after admission. Blood routine factors were extracted, including hemoglobin (HGB) level, white blood cell count, and hematocrit. Biochemical factors like blood urea nitrogen, ALB, fasting plasma glucose (FPG), serum creatinine, calcium ion level (Ca2+), sodium ion level, aspartate aminotransferase (AST), alanine aminotransferase, C-reactive protein (CRP), triglyceride (TG), and procalcitonin (PCT), were collected. AP severity was assessed using BISAP score[23,24] and SOFA score[25]. Our endpoint was AP-induced AKI during hospital stay.
Normally-distributed continuous data were indicated by means ± SDs and analyzed by one-way analysis of variance, while non-normally-distributed continuous data were explored by Kruskal-Wallis H test. In addition, categorical counterparts were indicated by frequencies or percentages and analyzed by Fisher’s exact and χ2 tests.
Patients were classified according to ePVS level in tertiles (D-ePVS < 4.231, 4.231 ≤ D-ePVS < 5.358, D-ePVS ≥ 5.358; KH-ePVS < -7.425, -7.425 ≤ KH-ePVS < 2.669, KH-ePVS ≥ 2.669). Subsequently, the association of ePVS with AKI was analyzed by multivariate logistic regression and smooth curve fitting. Based on the strengthening the reporting of observational studies statement[26], models not adjusted or adjusted for multiple variables were simultaneously ana
Free Statistics software versions 1.9 and statistical software packages R (http://www.R-project.org, The R Foundation) were used for analysis. P < 0.05 (two-sided) represented statistical significance.
Totally 1508 cases were included, including 251 (16.6%) developing AKI. We classified those included AP cases as AKI (n = 251) or non-AKI group (n = 1257) based on whether they developed AKI or not. BMI, the history of DM, chronic obstructive pulmonary disease, HGB, hematocrit, AST and D-ePVS were not of significance difference between two groups (P > 0.05). By contrast, age, gender, LOS, necessity of blood transfusion, MV and CRRT, PCT, ALB, TG, CRP, serum creatinine, and KH-ePVS were significantly different (P < 0.05). Median KH-ePVS was 0.9% in AKI group, re
| Variables | Non-AKI (n = 1257) | AKI (n = 251) | P value |
| Male | 642 (51.1) | 164 (65.3) | < 0.001 |
| Age (years), median (IQR) | 53.0 (41.0, 64.0) | 56.0 (44.0, 69.0) | 0.002 |
| Hypertension | 304 (24.2) | 88 (35.1) | < 0.001 |
| DM | 177 (14.1) | 47 (18.7) | 0.059 |
| CHD | 77 (6.1) | 26 (10.4) | 0.015 |
| COPD | 48 (3.8) | 15 (6) | 0.119 |
| Weight (kg), median (IQR) | 64.0 (56.0, 75.0) | 66.0 (55.0, 75.0) | 0.675 |
| Height (cm), median (IQR) | 163.0 (158.0, 170.0) | 166.0 (158.0, 172.0) | 0.003 |
| BMI (kg/m2), median (IQR) | 24.1 (21.8, 26.7) | 24.2 (20.9, 26.9) | 0.534 |
| HR (bpm), median (IQR) | 78.0 (72.0, 90.0) | 90.0 (76.0, 109.5) | < 0.001 |
| SBP (mmHg), median (IQR) | 130.0 (119.0, 143.0) | 123.0 (110.0, 140.5) | < 0.001 |
| DBP (mmHg), median (IQR) | 80.0 (74.0, 90.0) | 80.0 (66.0, 89.0) | 0.001 |
| RR (bpm), median (IQR) | 20.0 (19.0, 20.0) | 20.0 (19.0, 21.0) | 0.010 |
| SpO2 (%), median (IQR) | 99.0 (98.0, 100.0) | 98.0 (96.0, 100.0) | < 0.001 |
| Mechanical ventilation | 73 (5.8) | 83 (33.1) | < 0.001 |
| Transfusion | 70 (5.6) | 93 (37.1) | < 0.001 |
| CRRT | 21 (1.7) | 66 (26.3) | < 0.001 |
| WBC (× 109/L), median (IQR) | 9.6 (6.4, 13.2) | 11.2 (7.8, 15.8) | < 0.001 |
| HGB (g/L), median (IQR) | 129.0 (116.0, 144.0) | 128.0 (106.0, 150.5) | 0.255 |
| HCT (%), median (IQR) | 38.7 (34.9, 42.3) | 37.6 (32.2, 43.2) | 0.057 |
| PLT (× 109/L), median (IQR) | 181.0 (139.0, 234.0) | 172.0 (111.0, 226.5) | 0.005 |
| PCT (ng/mL), median (IQR) | 0.1 (0.0, 0.6) | 1.1 (0.2, 6.2) | < 0.001 |
| CRP (mg/L), median (IQR) | 31.4 (5.9, 119.0) | 90.8 (17.2, 198.6) | < 0.001 |
| AST (U/L), median (IQR) | 41.0 (23.0, 143.0) | 44.0 (25.0, 132.5) | 0.422 |
| ALB (g/dL), median (IQR) | 39.1 (34.9, 42.7) | 34.9 (28.6, 39.7) | < 0.001 |
| FPG (mmol/L), median (IQR) | 6.6 (5.3, 8.9) | 7.5 (5.7, 11.2) | < 0.001 |
| AMY (U/L), median (IQR) | 163.0 (64.5, 716.0) | 193.0 (90.0, 580.0) | 0.124 |
| TG (mmol/L), median (IQR) | 1.5 (1.0, 3.4) | 1.8 (1.2, 6.4) | < 0.001 |
| Na+ (mmol/L), median (IQR) | 139.7 (137.1, 141.8) | 137.9 (135.0, 141.1) | < 0.001 |
| Ca2+ (mmol/L), median (IQR) | 2.2 (2.1, 2.4) | 2.1 (1.9, 2.3) | < 0.001 |
| BUN (mmol/L), median (IQR) | 5.0 (3.8, 6.3) | 9.6 (5.9, 15.1) | < 0.001 |
| CREA (mmol/L), median (IQR) | 71.0 (59.0, 83.0) | 95.5 (84.0, 187.0) | < 0.001 |
| D-ePVS (dL/g), median (IQR) | 4.7 (4.0, 5.6) | 4.9 (3.8, 6.4) | 0.181 |
| KH-ePVS (%), median (IQR) | -2.5 (-10.0, 4.5) | 0.9 (-10.7, 13.1) | 0.002 |
| Death | 5 (0.4) | 18 (7.2) | < 0.001 |
| LOS (day), median (IQR) | 13.0 (10.0, 18.0) | 16.0 (10.0, 26.0) | < 0.001 |
| ICU | 115 (9.1) | 127 (50.6) | < 0.001 |
| SOFA (score) | 2.2 ± 1.9 | 5.0 ± 3.6 | < 0.001 |
| BISAP (score) | 1.2 ± 1.1 | 2.0 ± 1.3 | < 0.001 |
| Biliary | 887 (70.6) | 130 (51.8) | |
| Hyperlipidemic | 289 (23) | 64 (25.5) | |
| Alcoholic | 42 (3.3) | 8 (3.2) | |
| Others | 39 (3.1) | 49 (19.5) | |
| Severity of AP (%) | < 0.001 | ||
| Mild and moderate | 800 (63.6) | 90 (35.9) | |
| Severe | 457 (36.4) | 161 (64.1) |
Table 2 presents the basic patient demographic data classified based on ePVS tertiles. All patients had a median age of 53.0 (41.0, 65.0) years, including 53.4% males and 46.6% females. Among patients in the second tertile of ePVS levels, the length of intensive care unit (ICU) stays was lower, the demand for ventilation, transfusion and CRRT was lower, the HR, PCT and BISAP score were lower and the AKI patient proportion decreased relative to those in the ePVS higher and lower tertiles. Table 2 displays the distribution of PVS.
| Characteristics | D-ePVS formula | KH-ePVS formula | ||||||
| T1 (n = 505) (< 4.231 dL/g) | T2 (n = 504) (4.231-5.358 dL/g) | T3 (n = 505) (≥ 5.358 dL/g) | P value | T1 (n = 505) (< -7.425) | T2 (n = 504) (-7.425-2.669) | T3 (n = 505) (≥ 2.669) | P value | |
| Male | 401 (79.7) | 239 (47.6) | 166 (33) | < 0.001 | 363 (72.2) | 211 (42) | 232 (46.1) | < 0.001 |
| Age (years), median (IQR) | 46.0 (36.0, 57.0) | 55.0 (44.0, 65.0) | 59.0 (48.0, 69.0) | < 0.001 | 45.0 (35.0, 56.0) | 54.0 (46.0, 66.0) | 60.0 (50.0, 70.0) | < 0.001 |
| Death | 9 (1.8) | 2 (0.4) | 12 (2.4) | 0.031 | 493 (98) | 500 (99.6) | 492 (97.8) | 0.04 |
| ICU | 75 (14.9) | 51 (10.2) | 116 (23.1) | < 0.001 | 75 (14.9) | 51 (10.2) | 116 (23.1) | < 0.001 |
| LOS (day), median (IQR) | 12.0 (10.0, 17.0) | 13.0 (10.0, 18.0) | 14.0 (10.0, 22.0) | < 0.001 | 12.0 (10.0, 17.0) | 12.0 (10.0, 18.0) | 14.0 (10.0, 23.0) | < 0.001 |
| Hypertension | 119 (23.7) | 132 (26.3) | 141 (28) | 0.281 | 118 (23.5) | 149 (29.7) | 125 (24.9) | 0.062 |
| DM | 85 (16.9) | 62 (12.4) | 77 (15.3) | 0.121 | 95 (18.9) | 60 (12) | 69 (13.7) | 0.006 |
| CHD | 477 (94.8) | 473 (94.2) | 455 (90.5) | 0.012 | 26 (5.2) | 32 (6.4) | 45 (8.9) | 0.053 |
| SBP (mmHg), median (IQR) | 130.0 (120.0, 144.0) | 130.0 (118.0, 144.0) | 125.0 (112.0, 140.0) | < 0.001 | 130.0 (120.0, 146.0) | 130.0 (118.0, 142.0) | 125.0 (111.0, 140.0) | < 0.001 |
| DBP (mmHg), median (IQR) | 85.0 (78.0, 94.0) | 80.0 (72.0, 90.0) | 78.0 (69.0, 85.5) | < 0.001 | 86.0 (78.0, 95.0) | 80.0 (72.0, 90.0) | 77.0 (69.0, 85.0) | < 0.001 |
| HR (bpm), median (IQR) | 82.0 (75.0, 100.0) | 78.0 (72.0, 90.0) | 80.0 (72.0, 92.0) | < 0.001 | 82.0 (75.0, 99.0) | 78.0 (72.0, 89.8) | 80.0 (72.0, 94.0) | < 0.001 |
| RR (bpm), median (IQR) | 20.0 (19.0, 20.0) | 20.0 (19.0, 20.0) | 20.0 (18.0, 20.0) | 0.002 | 20.0 (19.0, 20.0) | 20.0 (19.0, 20.0) | 20.0 (18.0, 20.0) | < 0.001 |
| SpO2 (%), median (IQR) | 99.0 (97.0, 100.0) | 99.0 (97.0, 100.0) | 99.0 (98.0, 100.0) | 0.464 | 99.0 (97.0, 100.0) | 99.0 (97.0, 100.0) | 99.0 (97.0, 100.0) | 0.318 |
| Mechanical ventilation (%) | 52 (10.3) | 37 (7.4) | 67 (13.3) | 0.008 | 46 (9.1) | 31 (6.2) | 79 (15.7) | < 0.001 |
| Transfusion (%) | 41 (8.2) | 30 (6) | 92 (18.3) | < 0.001 | 35 (7) | 27 (5.4) | 101 (20.1) | < 0.001 |
| CRRT (%) | 38 (7.6) | 12 (2.4) | 37 (7.4) | < 0.001 | 37 (7.4) | 12 (2.4) | 38 (7.6) | < 0.001 |
| WBC (× 109/L), median (IQR) | 11.9 (8.4, 15.2) | 9.6 (6.5, 12.8) | 8.3 (5.6, 11.9) | < 0.001 | 11.8 (8.5, 14.8) | 9.3 (6.5, 12.9) | 8.3 (5.6, 12.3) | < 0.001 |
| HGB (g/L), median (IQR) | 152.0 (144.0, 162.0) | 129.0 (125.0, 134.0) | 108.0 (98.0, 114.0) | < 0.001 | 151.0 (141.0, 161.0) | 128.0 (120.0, 136.0) | 109.0 (98.0, 119.0) | < 0.001 |
| HCT (%), median (IQR) | 44.5 (42.5, 47.2) | 38.6 (37.2, 40.0) | 32.8 (30.0, 34.6) | < 0.001 | 44.3 (42.0, 47.2) | 38.0 (36.4, 40.1) | 33.0 (30.0, 35.6) | < 0.001 |
| PCT (ng/mL), median (IQR) | 0.2 (0.1, 0.9) | 0.1 (0.0, 0.6) | 0.3 (0.1, 1.2) | < 0.001 | 0.2 (0.1, 0.7) | 0.1 (0.0, 0.5) | 0.3 (0.1, 1.4) | < 0.001 |
| CRP (mg/L), median (IQR) | 37.3 (7.3, 130.7) | 27.4 (4.1, 123.2) | 53.3 (7.6, 139.0) | 0.007 | 34.7 (7.1, 138.1) | 32.8 (5.3, 134.7) | 45.9 (7.2, 133.4) | 0.194 |
| AST (U/L), median (IQR) | 38.0 (23.2, 121.5) | 44.2 (24.0, 152.5) | 41.0 (22.0, 143.5) | 0.435 | 38.0 (23.0, 134.0) | 42.0 (22.7, 143.8) | 42.0 (22.0, 137.4) | 0.919 |
| ALB (g/dL), median (IQR) | 41.1 (37.4, 44.3) | 38.9 (35.3, 42.5) | 35.0 (29.6, 39.2) | < 0.001 | 41.4 (37.9, 44.4) | 38.4 (34.9, 41.9) | 35.2 (29.6, 39.4) | < 0.001 |
| FPG (mmol/L), median (IQR) | 7.5 (6.0, 11.5) | 6.5 (5.3, 8.7) | 6.1 (5.0, 7.8) | < 0.001 | 7.8 (6.0, 11.9) | 6.4 (5.2, 8.4) | 6.2 (5.0, 7.8) | < 0.001 |
| TG (mmol/L), median (IQR) | 2.4 (1.2, 7.7) | 1.4 (0.9, 2.7) | 1.3 (0.9, 2.2) | < 0.001 | 2.5 (1.2, 7.4) | 1.4 (1.0, 2.7) | 1.2 (0.9, 2.2) | < 0.001 |
| Na+ (mmol/L), median (IQR) | 138.8 (135.5, 141.1) | 139.8 (137.2, 142.2) | 139.9 (137.3, 141.9) | < 0.001 | 139.1 (135.8, 141.2) | 139.9 (137.3, 142.4) | 139.6 (136.9, 141.8) | < 0.001 |
| Ca2+ (mmol/L), median (IQR) | 2.3 (2.1, 2.4) | 2.2 (2.1, 2.4) | 2.1 (2.0, 2.3) | < 0.001 | 2.2 (2.1, 2.4) | 2.2 (2.1, 2.4) | 2.1 (2.0, 2.3) | < 0.001 |
| AMY (U/L), median (IQR) | 236.0 (85.0, 875.5) | 193.0 (68.3, 650.8) | 117.0 (59.0, 433.0) | < 0.001 | 251.0 (78.2, 921.0) | 182.7 (68.3, 574.0) | 128.0 (60.0, 466.0) | < 0.001 |
| CREA (μmol/L), median (IQR) | 80.0 (69.0, 92.0) | 71.1 (59.0, 84.1) | 71.0 (58.0, 88.0) | < 0.001 | 79.0 (67.0, 91.0) | 70.0 (58.7, 81.8) | 75.0 (60.0, 90.0) | < 0.001 |
| AKI | 91 (18.1) | 55 (11) | 105 (20.9) | < 0.001 | 81 (16.1) | 62 (12.4) | 108 (21.5) | < 0.001 |
| Etiology | < 0.001 | < 0.001 | ||||||
| Biliary | 276 (54.9) | 367 (73.1) | 374 (74.4) | 272 (54.1) | 372 (74.1) | 373 (74.2) | ||
| Hyperlipidemic | 186 (37) | 97 (19.3) | 70 (13.9) | 189 (37.6) | 99 (19.7) | 65 (12.9) | ||
| Alcoholic | 28 (5.6) | 13 (2.6) | 9 (1.8) | 29 (5.8) | 12 (2.4) | 9 (1.8) | ||
| Others | 13 (2.6) | 25 (5) | 50 (9.9) | 13 (2.6) | 19 (3.8) | 56 (11.1) | ||
| SOFA (score) | 2.5 ± 2.4 | 2.5 ± 2.2 | 3.1 ± 2.8 | < 0.001 | 2.4 ± 2.2 | 2.5 ± 2.2 | 3.2 ± 2.9 | < 0.001 |
| BISAP (score) | 1.3 ± 1.1 | 1.2 ± 1.2 | 1.4 ± 1.2 | 0.004 | 1.3 ± 1.1 | 1.2 ± 1.1 | 1.5 ± 1.2 | < 0.001 |
| Severity of AP | 0.006 | < 0.001 | ||||||
| Mild and moderate | 434 (86.3) | 467 (93.0) | 439 (87.3) | 442 (87.9) | 472 (94.0) | 426 (84.7) | ||
| Severe | 69 (13.7) | 35 (7.0) | 64 (12.7) | 61 (12.1) | 30 (6.0) | 77 (15.3) | ||
Univariate regression identified age, gender, CHD, hypertension, SBP, HR, RR, SpO2, blood transfusion, MV, CRRT, BISAP score, SOFA score, ALB, white blood cell count, CRP, PCT, FPG, and Ca2+ as obvious confounders which affect AKI occurrence (P < 0.001) (Supplementary Table 1).
Using multivariate logistic regression (Table 3), relative to the D-ePVS reference tertile (T2: 4.231-5.358), the adjusted ORs for D-ePVS lower tertile (T1 < 4.231) and higher tertile (T3 ≥ 5.358) were determined to be 1.56 [95% confidence interval (CI): 1.01-2.41, P = 0.045] and 1.87 (95%CI: 1.20-2.91, P = 0.005), respectively, which were associated with an increased AKI risk. At the same time, relative to the KH-ePVS reference tertile (T2: -7.425 to 2.669), we determined the adjusted ORs for KH-ePVS lower tertile (T1 < -7.425) and higher tertile (T3 ≥ 2.669) to be 1.11 (95%CI: 0.72-1.72, P = 0.629) and 1.51 (95%CI: 1.00-2.29, P = 0.05), respectively, after adjusting for covariates.
| Non-adjusted model | Adjusted model 1 | Adjusted model 2 | Adjusted model 3 | |||||
| OR (95%CI) | P value | OR (95%CI) | P value | OR (95%CI) | P value | OR (95%CI) | P value | |
| D-ePVS, tertiles | ||||||||
| T1 | 1.8 (1.25-2.57) | 0.001 | 1.65 (1.13-2.41) | 0.01 | 1.54 (1.04-2.29) | 0.032 | 1.56 (1.01-2.41) | 0.045 |
| T2 | Ref. | Ref. | Ref. | Ref. | ||||
| T3 | 2.14 (1.51-3.05) | < 0.001 | 2.32 (1.61-3.35) | < 0.001 | 2.31 (1.57-3.38) | < 0.001 | 1.87 (1.2-2.91) | 0.005 |
| P for trend | 0.236 | 0.043 | 0.028 | 0.469 | ||||
| KH-ePVS, tertiles | ||||||||
| T1 | 1.36 (0.95-1.95) | 0.089 | 1.28 (0.87~1.89) | 0.211 | 1.18 (0.79-1.77) | 0.414 | 1.11 (0.72-1.72) | 0.629 |
| T2 | Ref. | Ref. | Ref. | Ref. | ||||
| T3 | 1.94 (1.38-2.73) | < 0.001 | 1.83 (1.28-2.62) | 0.001 | 1.4 (1.19-2.54) | 0.004 | 1.51 (1-2.29) | 0.05 |
| P for trend | 0.023 | 0.051 | 0.05 | 0.167 | ||||
When covariates from model 3 were adjusted, the nonlinear relations of D-ePVS and KH-ePVS with AKI were detected, exhibiting the U-shaped and J-shaped curves in the restricted cubic spline model, respectively (P for non-linearity < 0.01) (Figure 2).
In threshold analysis, the data were fitted into the piecewise multiple logistic regression model using 2 distinct slopes (Table 4). An inflection point at 4.3 dL/g (D-ePVS) and -2.8% (KH-ePVS) was found in the population. AKI was positively related to ePVS above the inflection point for both D-ePVS (OR = 1.235, 95%CI: 1.079-1.413, P = 0.002) and KH-ePVS (OR = 1.032, 95%CI: 1.005-1.060, P = 0.019). By contrast, below the inflection point, a negative correlation was observed between AKI and D-ePVS (OR = 0.579, 95%CI: 0.335-0.998, P = 0.049), while AKI was not significantly related to KH-ePVS (OR = 0.990, 95%CI: 0.953-1.028, P = 0.601).
| Two-piecewise linear regression model | D-ePVS | KH-ePVS | ||
| OR (95%CI) | P value | OR (95%CI) | P value | |
| Inflection point (K) | 4.3 | -2.8 | ||
| ePVS < K | 0.579 (0.335-0.998) | 0.049 | 0.990 (0.953-1.028) | 0.601 |
| ePVS ≥ K | 1.235 (1.079-1.413) | 0.002 | 1.032 (1.005-1.06) | 0.019 |
| Likelihood ratio test | 0.002 | 0.006 | ||
| Non-linear test | 0.021 | 0.025 | ||
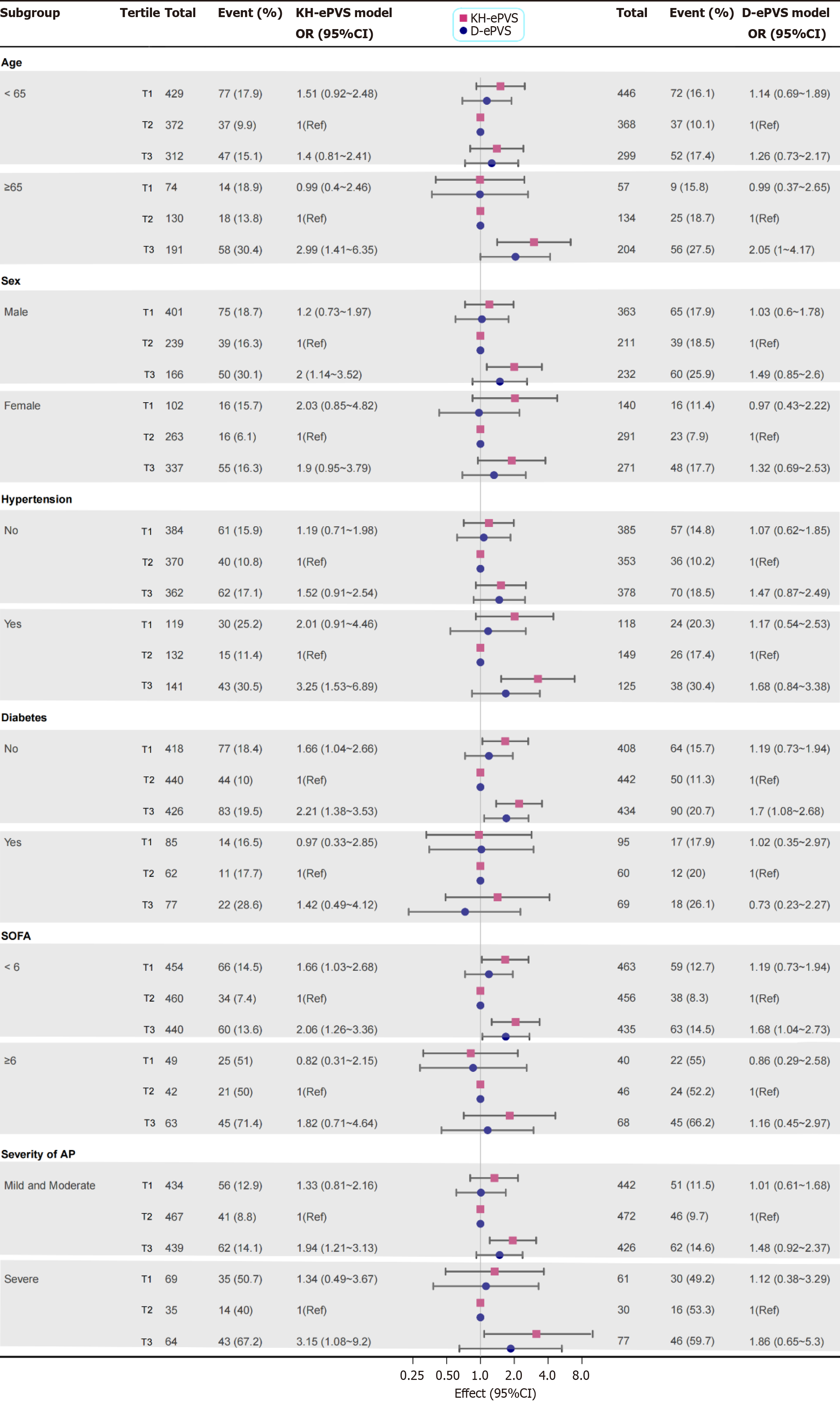
Our exploratory subgroup analyses, using two different formulae, consistently revealed an association between ePVS and AKI across various stratified variables including age, sex, hypertension, DM, SOFA score, and AP severity, and signi
Fluid management is a crucial and manageable risk factor related to AKI, especially for critical cases. Our study assessed the calculated PVS as the fluid status indicator in a large cohort with AP, showing several key results. At first, most AKI patients show the PVS on admission with KH-ePVS, suggesting excessive PV. Secondly, the U-shaped and J-shaped curves for ePVS corresponded with a graded increase in AKI risk in AP, with the optimal serum ePVS for minimal AKI risk identified at 4.3 dL/g using the Duarte formula and -2.8% with the Kaplan-Hakim formula, respectively. Finally, both formulae indicated the same nonlinear association, and subgroup analysis demonstrated the robust relationship between ePVS and AKI. Our findings indicate that ePVS is the valuable predictor for AKI risk among AP patients and warrants further investigation as a potential therapeutic target.
ePVS has been shown to associate with actual PV based on the 125Iodine-labeled human serum ALB method[28] or Technetium (99Tc)-labeled red blood cells[15] techniques, which is a key factor suggesting fluid status in chronic heart failure patients. Expansion of PV is correlated with dismal clinical results for heart failure patients[28-30]. In addition, ePVS has been used in the non-cardiovascular settings. Kurokawa et al[31] suggested the association of ePVS with the severity and unfavorable results of lower extremity artery disease. Gao et al[32] identified a J-shaped relationship between extracellular fluid volume (ePVS) and 28-day mortality in septic patients at the time of ICU admission, reporting a sig
AKI and AP are both characterized by significant inflammatory responses. Elevated levels of pro-inflammatory cytokines, such as tumor necrosis factor-α and interleukin-6, can lead to complications including endothelial dysfunction and microvascular injury in both the kidneys and the pancreas[36,37]. Endothelial dysfunction may result from impaired nitric oxide production and increased vascular permeability, which can contribute to fluctuations in fluid status, poten
Our study has first investigated the association of ePVS with AKI among AP, concentrating on volume status as a key factor in AKI development[1,38,39]. In early AP, capillary leak and fluid retention in the “third space” may result in hemodynamic instability, notable hypovolemia and hypotension, impairing renal perfusion and increasing the risk of pre-renal AKI, accompanied by a reduction in ePVS. Aggressive volume resuscitation is often necessary to reverse AKI. By contrast, volume overload can increase ePVS, potentially triggered by reduced urine output, inadequately fluid administered for over-resuscitation. The excess circulating volume can cause renal congestion, renal interstitial oedema, renal compartment syndrome and intra-abdominal hypertension[38], which may further impair renal function[40-42]. Therefore, both volume overload and depletion adversely impact renal function, which can highlight the complex interplay of factors affecting renal outcomes in AP.
Managing fluid balance in AP patients is challenging, and ePVS provides a valuable supplementary measure. Point-of-care ultrasound (POCUS) is the main non-invasive method for the assessment of volume status in the critical care settings[43]. However, its use in AP patients can be challenging owing to complications including acute dyspnea, abdominal distension, ascites, abdominal pain and bowel gas obstruction. In addition, POCUS is not widely used to manage AKI in most centers worldwide. Furthermore, it is of note that, as a tertiary teaching hospital, our medical center usually receives AP patients who have already undergone initial fluid resuscitation elsewhere before transfer, complicating the evaluation of fluid status. Considering these challenges, we believe ePVS can easily and quickly assess volume status upon hospital admission, especially for critical AP cases.
This study examined ePVS using two methods for the calculation of PV: D-ePVS and KH-ePVS. The D-ePVS formula, based on the Strauss formula[44], uses hematocrit and HGB for an ‘instantaneous’ PV measurement, as described by Duarte et al[45] in 2015. By contrast, the KH-ePVS formula (expressed as a percentage deviation from iPV) calculates hematocrit and patient body dry weight[28,46], while these two values can hardly be obtained in fluid-overload patients[35], and weight estimation among critical cases is usually unreliable. Severe AP patients are more vulnerable to develop AKI owing to insufficient blood volume and overload. Therefore, D-ePVS may be more dependable and practical for critically ill patients compared with KH-ePVS. Furthermore, D-ePVS follows a U-shaped curve, aligning closely with pathophysiology of AKI and clinical characteristics, which indicates that both lower and higher volumes can cause AP-AKI, whereas KH-ePVS is represented as a J-shaped curve. Our study suggests that D-ePVS of 4.3 dL/g may serve as a promising complement to other fluid status evaluation methods in AP, like physical examinations, biomarkers, ultra
To conclude, this study reveals the obvious nonlinear relation of serum ePVS with AKI, with the inflection points at 4.3 dL/g (Duarte formula) and -2.8% (Kaplan-Hakim formula). Given its wide availability, low cost, rapid quantification, and routine use in hemogram prescriptions, ePVS can serve as the important approach to diagnose and stratify AKI patients. Furthermore, more investigations are needed to validate our findings and explore mechanisms related to the ePVS-AKI relationship.
| 1. | Crosignani A, Spina S, Marrazzo F, Cimbanassi S, Malbrain MLNG, Van Regenmortel N, Fumagalli R, Langer T. Intravenous fluid therapy in patients with severe acute pancreatitis admitted to the intensive care unit: a narrative review. Ann Intensive Care. 2022;12:98. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 30] [Reference Citation Analysis (0)] |
| 2. | Kaplan M, Ates I, Akpinar MY, Yuksel M, Kuzu UB, Kacar S, Coskun O, Kayacetin E. Predictive value of C-reactive protein/albumin ratio in acute pancreatitis. Hepatobiliary Pancreat Dis Int. 2017;16:424-430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 95] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 3. | Silva-Vaz P, Abrantes AM, Castelo-Branco M, Gouveia A, Botelho MF, Tralhão JG. Murine Models of Acute Pancreatitis: A Critical Appraisal of Clinical Relevance. Int J Mol Sci. 2019;20:2794. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 30] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 4. | van Dijk SM, Hallensleben NDL, van Santvoort HC, Fockens P, van Goor H, Bruno MJ, Besselink MG; Dutch Pancreatitis Study Group. Acute pancreatitis: recent advances through randomised trials. Gut. 2017;66:2024-2032. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 221] [Cited by in RCA: 297] [Article Influence: 37.1] [Reference Citation Analysis (0)] |
| 5. | Kes P, Vucicević Z, Ratković-Gusić I, Fotivec A. Acute renal failure complicating severe acute pancreatitis. Nephron. 1996;73:488-489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Almeida N, Fernandes A, Casela A. Predictors of Severity and In-Hospital Mortality for Acute Pancreatitis: Is There Any Role for C-Reactive Protein Determination in the First 24 Hours? GE Port J Gastroenterol. 2015;22:187-189. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Petejova N, Martinek A. Acute kidney injury following acute pancreatitis: A review. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2013;157:105-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 54] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 8. | Kobayashi M, Girerd N, Duarte K, Chouihed T, Chikamori T, Pitt B, Zannad F, Rossignol P. Estimated plasma volume status in heart failure: clinical implications and future directions. Clin Res Cardiol. 2021;110:1159-1172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 36] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 9. | Maznyczka AM, Barakat MF, Ussen B, Kaura A, Abu-Own H, Jouhra F, Jaumdally H, Amin-Youssef G, Nicou N, Baghai M, Deshpande R, Wendler O, Kolvekar S, Okonko DO. Calculated plasma volume status and outcomes in patients undergoing coronary bypass graft surgery. Heart. 2019;105:1020-1026. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 28] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 10. | Fudim M, Miller WL. Calculated Estimates of Plasma Volume in Patients With Chronic Heart Failure-Comparison With Measured Volumes. J Card Fail. 2018;24:553-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 70] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 11. | Kobayashi M, Huttin O, Donal E, Duarte K, Hubert A, Le Breton H, Galli E, Fournet M, Mabo P, Schnell F, Leclercq C, Rossignol P, Girerd N. Association of estimated plasma volume status with hemodynamic and echocardiographic parameters. Clin Res Cardiol. 2020;109:1060-1069. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 12. | Grodin JL, Philips S, Mullens W, Nijst P, Martens P, Fang JC, Drazner MH, Tang WHW, Pandey A. Prognostic implications of plasma volume status estimates in heart failure with preserved ejection fraction: insights from TOPCAT. Eur J Heart Fail. 2019;21:634-642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 44] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 13. | Huang CY, Lin TT, Wu YF, Chiang FT, Wu CK. Long-term Prognostic Value of Estimated Plasma Volume in Heart Failure with Preserved Ejection Fraction. Sci Rep. 2019;9:14369. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 14. | Kobayashi M, Rossignol P, Ferreira JP, Aragão I, Paku Y, Iwasaki Y, Watanabe M, Fudim M, Duarte K, Zannad F, Girerd N. Prognostic value of estimated plasma volume in acute heart failure in three cohort studies. Clin Res Cardiol. 2019;108:549-561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 43] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 15. | Martens P, Nijst P, Dupont M, Mullens W. The Optimal Plasma Volume Status in Heart Failure in Relation to Clinical Outcome. J Card Fail. 2019;25:240-248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 34] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 16. | Turcato G, Zaboli A, Ciccariello L, Pfeifer N. Estimated plasma volume status (ePVS) could be an easy-to-use clinical tool to determine the risk of sepsis or death in patients with fever. J Crit Care. 2020;58:106-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 17. | Adlbrecht C, Piringer F, Resar J, Watzal V, Andreas M, Strouhal A, Hasan W, Geisler D, Weiss G, Grabenwöger M, Delle-Karth G, Mach M. The impact of subclinical congestion on the outcome of patients undergoing transcatheter aortic valve implantation. Eur J Clin Invest. 2020;50:e13251. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 18. | Otaki Y, Watanabe T, Konta T, Watanabe M, Asahi K, Yamagata K, Fujimoto S, Tsuruya K, Narita I, Kasahara M, Shibagaki Y, Iseki K, Moriyama T, Kondo M, Watanabe T. Impact of calculated plasma volume status on all-cause and cardiovascular mortality: 4-year nationwide community-based prospective cohort study. PLoS One. 2020;15:e0237601. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 19. | Beyer G, Hoffmeister A, Lorenz P, Lynen P, Lerch MM, Mayerle J. Clinical Practice Guideline—Acute and Chronic Pancreatitis. Dtsch Arztebl Int. 2022;119:495-501. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 20] [Reference Citation Analysis (0)] |
| 20. | Zhou W, Dong S, Chen Z, Li X, Jiang W. New challenges for microRNAs in acute pancreatitis: progress and treatment. J Transl Med. 2022;20:192. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 20] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 21. | Banks PA, Bollen TL, Dervenis C, Gooszen HG, Johnson CD, Sarr MG, Tsiotos GG, Vege SS; Acute Pancreatitis Classification Working Group. Classification of acute pancreatitis--2012: revision of the Atlanta classification and definitions by international consensus. Gut. 2013;62:102-111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4932] [Cited by in RCA: 4337] [Article Influence: 361.4] [Reference Citation Analysis (45)] |
| 22. | Khwaja A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract. 2012;120:c179-c184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1436] [Cited by in RCA: 3342] [Article Influence: 257.1] [Reference Citation Analysis (0)] |
| 23. | Annane D, Renault A, Brun-Buisson C, Megarbane B, Quenot JP, Siami S, Cariou A, Forceville X, Schwebel C, Martin C, Timsit JF, Misset B, Ali Benali M, Colin G, Souweine B, Asehnoune K, Mercier E, Chimot L, Charpentier C, François B, Boulain T, Petitpas F, Constantin JM, Dhonneur G, Baudin F, Combes A, Bohé J, Loriferne JF, Amathieu R, Cook F, Slama M, Leroy O, Capellier G, Dargent A, Hissem T, Maxime V, Bellissant E; CRICS-TRIGGERSEP Network. Hydrocortisone plus Fludrocortisone for Adults with Septic Shock. N Engl J Med. 2018;378:809-818. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 471] [Cited by in RCA: 608] [Article Influence: 86.9] [Reference Citation Analysis (0)] |
| 24. | Hagjer S, Kumar N. Evaluation of the BISAP scoring system in prognostication of acute pancreatitis - A prospective observational study. Int J Surg. 2018;54:76-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 81] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 25. | Ferreira FL, Bota DP, Bross A, Mélot C, Vincent JL. Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA. 2001;286:1754-1758. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1597] [Cited by in RCA: 1829] [Article Influence: 76.2] [Reference Citation Analysis (0)] |
| 26. | von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370:1453-1457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6805] [Cited by in RCA: 11759] [Article Influence: 653.3] [Reference Citation Analysis (0)] |
| 27. | Zhang Z. Multiple imputation with multivariate imputation by chained equation (MICE) package. Ann Transl Med. 2016;4:30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 278] [Reference Citation Analysis (0)] |
| 28. | Ling HZ, Flint J, Damgaard M, Bonfils PK, Cheng AS, Aggarwal S, Velmurugan S, Mendonca M, Rashid M, Kang S, Papalia F, Weissert S, Coats CJ, Thomas M, Kuskowski M, Cohn JN, Woldman S, Anand IS, Okonko DO. Calculated plasma volume status and prognosis in chronic heart failure. Eur J Heart Fail. 2015;17:35-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 119] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 29. | Nogi K, Ueda T, Nakamura T, Nogi M, Ishihara S, Nakada Y, Hashimoto Y, Nakagawa H, Nishida T, Seno A, Onoue K, Watanabe M, Saito Y. New Classification for the Combined Assessment of the Fractional Excretion of Urea Nitrogen and Estimated Plasma Volume Status in Acute Heart Failure. J Am Heart Assoc. 2023;12:e025596. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 30. | Kobayashi M, Girerd N, Duarte K, Preud'homme G, Pitt B, Rossignol P. Prognostic impact of plasma volume estimated from hemoglobin and hematocrit in heart failure with preserved ejection fraction. Clin Res Cardiol. 2020;109:1392-1401. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 31. | Kurokawa T, Otaki Y, Takahashi H, Watanabe T, Shikama T, Tamura H, Kato S, Nishiyama S, Arimoto T, Watanabe M. Impact of estimated plasma volume status on clinical outcomes in patients with lower extremity artery disease who underwent endovascular therapy. Hypertens Res. 2023;46:2005-2015. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 32. | Gao B, Chen R, Zhao H, Zhang H, Wang X, Liu D. Estimated plasma volume status as a simple and accessible predictor of 28-day mortality in septic shock: insights from a retrospective study of the MIMIC-IV database. Front Med (Lausanne). 2024;11:1416396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 33. | Laou E, Papagiannakis N, Ntalarizou N, Choratta T, Angelopoulou Z, Annousis K, Sakellakis M, Kyriakaki A, Ragias D, Michou A, Chalkias A. The Relation of Calculated Plasma Volume Status to Sublingual Microcirculatory Blood Flow and Organ Injury. J Pers Med. 2023;13. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 34. | Marawan A, Qayyum R. Estimated plasma volume and mortality: analysis from NHANES 1999-2014. Clin Res Cardiol. 2020;109:1148-1154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 35. | Chouihed T, Rossignol P, Bassand A, Duarte K, Kobayashi M, Jaeger D, Sadoune S, Buessler A, Nace L, Giacomin G, Hutter T, Barbé F, Salignac S, Jay N, Zannad F, Girerd N. Diagnostic and prognostic value of plasma volume status at emergency department admission in dyspneic patients: results from the PARADISE cohort. Clin Res Cardiol. 2019;108:563-573. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 35] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 36. | Gasiorowska A, Talar-Wojnarowska R, Kaczka A, Borkowska A, Czupryniak L, Małecka-Panas E. Subclinical Inflammation and Endothelial Dysfunction in Patients with Chronic Pancreatitis and Newly Diagnosed Pancreatic Cancer. Dig Dis Sci. 2016;61:1121-1129. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 37. | Dumnicka P, Maduzia D, Ceranowicz P, Olszanecki R, Drożdż R, Kuśnierz-Cabala B. The Interplay between Inflammation, Coagulation and Endothelial Injury in the Early Phase of Acute Pancreatitis: Clinical Implications. Int J Mol Sci. 2017;18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 117] [Cited by in RCA: 134] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 38. | Malbrain ML, Marik PE, Witters I, Cordemans C, Kirkpatrick AW, Roberts DJ, Van Regenmortel N. Fluid overload, de-resuscitation, and outcomes in critically ill or injured patients: a systematic review with suggestions for clinical practice. Anaesthesiol Intensive Ther. 2014;46:361-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 496] [Cited by in RCA: 384] [Article Influence: 34.9] [Reference Citation Analysis (0)] |
| 39. | Messmer AS, Zingg C, Müller M, Gerber JL, Schefold JC, Pfortmueller CA. Fluid Overload and Mortality in Adult Critical Care Patients-A Systematic Review and Meta-Analysis of Observational Studies. Crit Care Med. 2020;48:1862-1870. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 216] [Article Influence: 43.2] [Reference Citation Analysis (0)] |
| 40. | Prowle JR, Bellomo R. Fluid administration and the kidney. Curr Opin Crit Care. 2013;19:308-314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 41. | Schrier RW. Fluid administration in critically ill patients with acute kidney injury. Clin J Am Soc Nephrol. 2010;5:733-739. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 72] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 42. | De Laet I, Malbrain ML, Jadoul JL, Rogiers P, Sugrue M. Renal implications of increased intra-abdominal pressure: are the kidneys the canary for abdominal hypertension? Acta Clin Belg. 2007;62 Suppl 1:119-130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 41] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 43. | Bateman RM, Sharpe MD, Jagger JE, Ellis CG, Solé-Violán J, López-Rodríguez M, Herrera-Ramos E, Ruíz-Hernández J, Borderías L, Horcajada J, González-Quevedo N, Rajas O, Briones M, Rodríguez de Castro F, Rodríguez Gallego C, Esen F, Orhun G, Ergin Ozcan P, Senturk E, Ugur Yilmaz C, Orhan N, Arican N, Kaya M, Kucukerden M, Giris M, Akcan U, Bilgic Gazioglu S, Tuzun E, Riff R, Naamani O, Douvdevani A, Takegawa R, Yoshida H, Hirose T, Yamamoto N, Hagiya H, Ojima M, Akeda Y, Tasaki O, Tomono K, Shimazu T, Ono S, Kubo T, Suda S, Ueno T, Ikeda T, Hirose T, Ogura H, Takahashi H, Ojima M, Kang J, Nakamura Y, Kojima T, Shimazu T, Ikeda T, Suda S, Izutani Y, Ueno T, Ono S, Taniguchi T, O M, Dinter C, Lotz J, Eilers B, Wissmann C, Lott R, Meili MM, Schuetz PS, Hawa H, Sharshir M, Aburageila M, Salahuddin N, Chantziara V, Georgiou S, Tsimogianni A, Alexandropoulos P, Vassi A, Lagiou F, Valta M, Micha G, Chinou E, Michaloudis G, Kodaira A, Ikeda T, Ono S, Ueno T, Suda S, Izutani Y, Imaizumi H, De la Torre-Prados MV, Garcia-De la Torre A, Enguix-Armada A, Puerto-Morlan A, Perez-Valero V, Garcia-Alcantara A, Bolton N, Dudziak J, Bonney S, Tridente A, Nee P, Nicolaes G, Wiewel M, Schultz M, Wildhagen K, Horn J, Schrijver R, Van der Poll T, Reutelingsperger C, Pillai S, Davies G, Mills G, Aubrey R, Morris K, Williams P, Evans P, Gayat EG, Struck J, Cariou A, Deye N, Guidet B, Jabert S, Launay J, Legrand M, Léone M, Resche-Rigon M, Vicaut E, Vieillard-Baron A, Mebazaa A, Arnold R, Capan M, Linder A, Akesson P, Popescu M, Tomescu D, Sprung CL, Calderon Morales R, Munteanu G, Orenbuch-Harroch E, Levin P, Kasdan H, Reiter A, Volker T, Himmel Y, Cohen Y, Meissonnier J, Girard L, Rebeaud F, Herrmann I, Delwarde B, Peronnet E, Cerrato E, Venet F, Lepape A, Rimmelé T, Monneret G, Textoris J, Beloborodova N, Moroz V, Osipov A, Bedova A, Sarshor Y, Pautova A, Sergeev A, Chernevskaya E, Odermatt J, Bolliger R, Hersberger L, Ottiger M, Christ-Crain M, Mueller B, Schuetz P, Sharma NK, Tashima AK, Brunialti MK, Machado FR, Assuncao M, Rigato O, Salomao R, Cajander SC, Rasmussen G, Tina E, Söderquist B, Källman J, Strålin K, Lange AL, Sundén-Cullberg JS, Magnuson AM, Hultgren OH, Davies G, Pillai S, Mills G, Aubrey R, Morris K, Williams P, Evans P, Pillai S, Davies G, Mills G, Aubrey R, Morris K, Williams P, Evans P, Pillai S, Davies G, Mills G, Aubrey R, Morris K, Williams P, Evans P, Van der Geest P, Mohseni M, Linssen J, De Jonge R, Duran S, Groeneveld J, Miller R III, Lopansri BK, McHugh LC, Seldon A, Burke JP, Johnston J, Reece-Anthony R, Bond A, Molokhia A, Mcgrath C, Nsutebu E, Bank Pedersen P, Pilsgaard Henriksen D, Mikkelsen S, Touborg Lassen A, Tincu R, Cobilinschi C, Tomescu D, Ghiorghiu Z, Macovei R, Wiewel MA, Harmon MB, Van Vught LA, Scicluna BP, Hoogendijk AJ, Horn J, Zwinderman AH, Cremer OL, Bonten MJ, Schultz MJ, Van der Poll T, Juffermans NP, Wiersinga WJ, Eren G, Tekdos Y, Dogan M, Acicbe O, Kaya E, Hergunsel O, Alsolamy S, Ghamdi G, Alswaidan L, Alharbi S, Alenezi F, Arabi Y, Heaton J, Boyce A, Nolan L, Johnston J, Dukoff-Gordon A, Dean A, Molokhia A, Mann Ben Yehudah T, Fleischmann C, Thomas-Rueddel D, Haas C, Dennler U, Reinhart K, Suntornlohanakul O, Khwannimit B, Breckenridge F, Puxty A, Szturz P, Folwarzcny P, Svancara J, Kula R, Sevcik P, Caneva L, Casazza A, Bellazzi E, Marra S, Pagani L, Vetere M, Vanzino R, Ciprandi D, Preda R, Boschi R, Carnevale L, Lopez V, Aguilar Arzapalo M, Barradas L, Escalante A, Gongora J, Cetina M, Adamik B, Jakubczyk D, Kübler A, Radford A, Lee T, Singer J, Boyd J, Fineberg D, Williams M, Russell J, Scarlatescu E, Tomescu D, Droc G, Arama S, Müller M, Straat M, Zeerleder SS, Juffermans NP, Fuchs CF, Scheer CS, Wauschkuhn SW, Vollmer MV, Meissner KM, Kuhn SK, Hahnenkamp KH, Rehberg SR, Gründling MG, Yamamoto N, Ojima M, Hamaguchi S, Hirose T, Akeda Y, Takegawa R, Tasaki O, Shimazu T, Tomono K, Gómez-Sánchez E, Heredia-Rodríguez M, Álvarez-Fuente E, Lorenzo-López M, Gómez-Pesquera E, Aragón-Camino M, Liu-Zhu P, Sánchez-López A, Hernández-Lozano A, Peláez-Jareño MT, Tamayo E, Thomas-Rüddel DO, Fleischmann C, Haas C, Dennler U, Reinhart K, Adora V, Kar A, Chakraborty A, Roy S, Bandyopadhyay A, Das M, Mann Ben Yehudah T, BenYehudah G, Salim M, Kumar N, Arabi L, Burger T, Lephart P, Toth-martin E, Valencia C, Hammami N, Blot S, Vincent JL, Lambert ML, Brunke J, Riemann T, Roschke I, Tincu R, Cobilinschi C, Tomescu D, Ghiorghiu Z, Macovei R, Nimitvilai S, Jintanapramote K, Jarupongprapa S, Adukauskiene D, Valanciene D, Bose G, Lostarakos V, Carr B, Khedher S, Maaoui A, Ezzamouri A, Salem M, Chen J, Cranendonk DR, Van Vught LA, Wiewel MA, Cremer OL, Horn J, Bonten MJ, Schultz MJ, Van der Poll T, Wiersinga WJ, Day M, Penrice G, Roy K, Robertson P, Godbole G, Jones B, Booth M, Donaldson L, Kawano Y, Ishikura H, Al-Dorzi H, Almutairi M, Alhamadi B, Crizaldo Toledo A, Khan R, Al Raiy B, Arabi Y, Talaie H, Van Oers JA, Harts A, Nieuwkoop E, Vos P, Boussarsar Y, Boutouta F, Kamoun S, Mezghani I, Koubaji S, Ben Souissi A, Riahi A, Mebazaa MS, Giamarellos-Bourboulis E, Tziolos N, Routsi C, Katsenos C, Tsangaris I, Pneumatikos I, Vlachogiannis G, Theodorou V, Prekates A, Antypa E, Koulouras V, Kapravelos N, Gogos C, Antoniadou E, Mandragos K, Armaganidis A, Robles Caballero AR, Civantos B, Figueira JC, López J, Silva-Pinto A, Ceia F, Sarmento A, Santos L, Almekhlafi G, Sakr Y, Al-Dorzi H, Khan R, Baharoon S, Aldawood A, Matroud A, Alchin J, Al Johani S, Balkhy H, Arabi Y, Alsolamy S, Yousif SY, Alotabi BO, Alsaawi AS, Ang J, Curran MD, Enoch D, Navapurkar V, Morris A, Sharvill R, Astin J, Heredia-Rodríguez M, Gómez-Sánchez E, Peláez-Jareño MT, Gómez-Pesquera E, Lorenzo-López M, Liu-Zhu P, Aragón-Camino M, Hernández-Lozano A, Sánchez-López A, Álvarez-Fuente E, Tamayo E, Patel J, Kruger C, O’Neal J, Rhodes H, Jancik J, François B, Laterre PF, Eggimann P, Torres A, Sánchez M, Dequin PF, Bassi GL, Chastre J, Jafri HS, Ben Romdhane M, Douira Z, Kamoun S, Bousselmi M, Ben Souissi A, Boussarsar Y, Riahi A, Mebazaa MS, Vakalos A, Avramidis V, Craven TH, Wojcik G, Kefala K, McCoubrey J, Reilly J, Paterson R, Inverarity D, Laurenson I, Walsh TS, Mongodi S, Bouhemad B, Orlando A, Stella A, Via G, Iotti G, Braschi A, Mojoli F, Haliloglu M, Bilgili B, Kasapoglu U, Sayan I, Süzer Aslan M, Yalcın A, Cinel I, Vakalos A, Avramidis V, Ellis HE, Bauchmuller K, Miller D, Temple A, Chastre J, François B, Torres A, Luyt CE, Sánchez M, Singer M, Jafri HS, Nassar Y, Ayad MS, Trifi A, Abdellatif S, Daly F, Nasri R, Ben Lakhal S, Bilgili B, Haliloglu M, Gul F, Cinel I, Kuzovlev A, Shabanov A, Polovnikov S, Moroz V, Kadrichu N, Dang T, Corkery K, Challoner P, Bassi GL, Aguilera E, Chiurazzi C, Travierso C, Motos A, Fernandez L, Amaro R, Senussi T, Idone F, Bobi J, Rigol M, Torres A, Hodiamont CJ, Juffermans NP, Janssen JM, Bouman CS, Mathôt RA, De Jong MD, Van Hest RM, Payne L, Fraser GL, Tudor B, Lahner M, Roth G, Krenn C, Talaie H, Jault P, Gabard J, Leclerc T, Jennes S, Que Y, Rousseau A, Ravat F, Al-Dorzi H, Eissa A, Al-Harbi S, Aldabbagh T, Khan R, Arabi Y, Trifi A, Abdellatif. S, Daly F, Nasri R, Ben Lakhal S, Paramba F, Purayil N, Naushad V, Mohammad O, Negi V, Chandra P, Kleinsasser A, Witrz MR, Buchner-Doeven JF, Tuip-de Boer AM, Goslings JC, Juffermans NP, Van Hezel M, Straat M, Boing A, Van Bruggen R, Juffermans N, Markopoulou D, Venetsanou K, Kaldis V, Koutete D, Chroni D, Alamanos I, Koch L, Jancik J, Rhodes H, Walter E, Maekawa K, Hayakawa M, Kushimoto S, Shiraishi A, Kato H, Sasaki J, Ogura H, Matauoka T, Uejima T, Morimura N, Ishikura H, Hagiwara A, Takeda M, Tarabrin O, Shcherbakow S, Gavrychenko D, Mazurenko G, Ivanova V, Chystikov O, Plourde C, Lessard J, Chauny J, Daoust R, Shcherbakow S, Tarabrin O, Gavrychenko D, Mazurenko G, Chystikov O, Vakalos A, Avramidis V, Kropman L, In het Panhuis L, Konings J, Huskens D, Schurgers E, Roest M, De Laat B, Lance M, Durila M, Lukas P, Astraverkhava M, Jonas J, Budnik I, Shenkman B, Hayami H, Koide Y, Goto T, Iqbal R, Alhamdi Y, Venugopal N, Abrams S, Downey C, Toh CH, Welters ID, Bombay VB, Chauny JM, Daoust RD, Lessard JL, Marquis MM, Paquet JP, Siemens K, Sangaran D, Hunt BJ, Durward A, Nyman A, Murdoch IA, Tibby SM, Ampatzidou F, Moisidou D, Dalampini E, Nastou M, Vasilarou E, Kalaizi V, Chatzikostenoglou H, Drossos G, Spadaro S, Fogagnolo A, Fiore T, Schiavi A, Fontana V, Taccone F, Volta C, Chochliourou E, Volakli E, Violaki A, Samkinidou E, Evlavis G, Panagiotidou V, Sdougka M, Mothukuri R, Battle C, Guy K, Mills G, Evans P, Wijesuriya J, Keogh S, Docherty A, O’Donnell R, Brunskill S, Trivella M, Doree C, Holst L, Parker M, Gregersen M, Almeida J, Walsh T, Stanworth S, Moravcova S, Mansell J, Rogers A, Smith RA, Hamilton-Davies C, Omar A, Allam M, Bilala O, Kindawi A, Ewila H, Ampatzidou F, Moisidou D, Nastou M, Dalampini E, Malamas A, Vasilarou E, Drossos G, Ferreira G, Caldas J, Fukushima J, Osawa EA, Arita E, Camara L, Zeferino S, Jardim J, Gaioto F, Dallan L, Jatene FB, Kalil Filho R, Galas F, Hajjar LA, Mitaka C, Ohnuma T, Murayama T, Kunimoto F, Nagashima M, Takei T, Tomita M, Omar A, Mahmoud K, Hanoura S, Sudarsanan S, Sivadasan P, Othamn H, Shouman Y, Singh R, Al Khulaifi A, Mandel I, Mikheev S, Suhodolo I, Kiselev V, Svirko Y, Podoksenov Y, Jenkins SA, Griffin R, Tovar Doncel MS, Lima A, Aldecoa C, Ince C, Taha A, Shafie A, Mostafa M, Syed N, Hon H, Righetti F, Colombaroli E, Castellano G, Righetti F, Colombaroli E, Hravnak M, Chen LC, Dubrawski AD, Clermont GC, Pinsky MR, Gonzalez S, Macias D, Acosta J, Jimenez P, Loza A, Lesmes A, Lucena F, Leon C, Tovar Doncel MS, Ince C, Aldecoa C, Lima A, Bastide M, Richecoeur J, Frenoy E, Lemaire C, Sauneuf B, Tamion F, Nseir S, Du Cheyron D, Dupont H, Maizel J, Shaban M, Kolko R, Salahuddin N, Sharshir M, AbuRageila M, AlHussain A, Mercado P, Maizel J, Kontar L, Titeca D, Brazier F, Riviere A, Joris M, Soupison T, De Cagny B, Slama M, Wagner J, Körner A, Kubik M, Kluge S, Reuter D, Saugel B, Colombaroli E, Righetti F, Castellano G, Tran T, De Bels D, Cudia A, Strachinaru M, Ghottignies P, Devriendt J, Pierrakos C, Martínez González Ó, Blancas R, Luján J, Ballesteros D, Martínez Díaz C, Núñez A, Martín Parra C, López Matamala B, Alonso Fernández M, Chana M, Huber W, Eckmann M, Elkmann F, Gruber A, Klein I, Schmid RM, Lahmer T, Moller PW, Sondergaard S, Jakob SM, Takala J, Berger D, Bastoni D, Aya H, Toscani L, Pigozzi L, Rhodes A, Cecconi M, Ostrowska C, Aya H, Abbas A, Mellinghoff J, Ryan C, Dawson D, Rhodes A, Cecconi M, Cronhjort M, Wall O, Nyberg E, Zeng R, Svensen C, Mårtensson J, Joelsson-Alm E, Aguilar Arzapalo M, Barradas L, Lopez V, Cetina M, Parenti N, Palazzi C, Amidei LA, Borrelli FB, Campanale SC, Tagliazucchi FT, Sedoni GS, Lucchesi DL, Carella EC, Luciani AL, Mackovic M, Maric N, Bakula M, Aya H, Rhodes A, Grounds RM, Fletcher N, Cecconi M, Avard B, Zhang P, Mezidi M, Charbit J, Ould-Chikh M, Deras P, Maury C, Martinez O, Capdevila X, Hou P, Linde-Zwirble WZ, Douglas ID, Shapiro NS, Ben Souissi A, Mezghani I, Ben Aicha Y, Kamoun S, Laribi B, Jeribi B, Riahi A, Mebazaa MS, Pereira C, Marinho R, Antunes R, Marinho A, Crivits M, Raes M, Decruyenaere J, Hoste E, Bagin V, Rudnov V, Savitsky A, Astafyeva M, Korobko I, Vein V, Kampmeier T, Arnemann P, Hessler M, Wald A, Bockbreder K, Morelli A, Van Aken H, Rehberg S, Ertmer C, Arnemann P, Hessler M, Kampmeier T, Rehberg S, Van Aken H, Ince C, Ertmer C, Reddy S, Bailey M, Beasley R, Bellomo R, Mackle D, Psirides A, Young P, Reddy S, Bailey M, Beasley R, Bellomo R, Mackle D, Young P, Venkatesh H, Ramachandran S, Basu A, Nair H, Egan S, Bates J, Oliveira S, Rangel Neto NR, Reis FQ, Lee CP, Lin XL, Choong C, Eu KM, Sim WY, Tee KS, Pau J, Abisheganaden J, Maas K, De Geus H, Lafuente E, Marinho R, Moura J, Antunes R, Marinho A, Doris TE, Monkhouse D, Shipley T, Kardasz S, Gonzalez I, Stads S, Groeneveld AJ, Elsayed I, Ward N, Tridente A, Raithatha A, Steuber A, Pelletier C, Schroeder S, Michael E, Slowinski T, Kindgen-Milles D, Ghabina S, Turani F, Belli A, Busatti S, Barettin G, Candidi F, Gargano F, Barchetta R, Falco M, Demirkiran O, Kosuk M, Bozbay S, Weber V, Hartmann J, Harm S, Linsberger I, Eichhorn T, Valicek G, Miestinger G, Hoermann C, Faenza S, Ricci D, Mancini E, Gemelli C, Cuoghi A, Magnani S, Atti M, Laddomada T, Doronzio A, Balicco B, Gruda MC, O’Sullivan P, Dan VP, Guliashvili T, Scheirer A, Golobish TD, Capponi VJ, Chan PP, Kogelmann K, Drüner M, Jarczak D, Turani F, Belli AB, Martni SM, Cotticelli VC, Mounajergi F, Barchetta R, Morimoto S, Ishikura H, Hussain I, Salahuddin N, Nadeem A, Ghorab K, Maghrabi K, Kloesel SK, Goldfuss C, Stieglitz A, Stieglitz AS, Krstevska L, Albuszies G, Aguilar Arzapalo M, Barradas L, Lopez V, Escalante A, Jimmy G, Cetina M, Izawa J, Iwami T, Uchino S, Takinami M, Kitamura T, Kawamura T, Powell-Tuck JG, Crichton S, Raimundo M, Camporota L, Wyncoll D, Ostermann M, Hana A, De Geus HR, De Geus HR, Hana A, Aydogdu M, Boyaci N, Yuksel S, Gursel G, Cayci Sivri AB, Meza-Márquez J, Nava-López J, Carrillo-Esper R, Dardashti A, Grubb A, Maizel J, Wetzstein M, Titeca D, Kontar L, Brazier F, De Cagny B, Riviere A, Soupison T, Joris M, Slama M, Peters E, Njimi H, Pickkers P, Vincent JL, Waraich M, Doyle J, Samuels T, Forni L, Desai N, Baumber R, Gunning P, Sell A, Lin S, Torrence H, O’Dwyer M, Kirwan C, Prowle J, Kim T, O’Connor ME, Hewson RW, Kirwan CJ, Pearse RM, Prowle J, Hanoura S, Omar A, Othamn H, Sudarsanan S, Allam M, Maksoud M, Singh R, Al Khulaifi A, O’Connor ME, Hewson RW, Kirwan CJ, Pearse RM, Prowle J, Uzundere O, Memis D, Ýnal M, Gultekin A, Turan N, Aydin MA, Basar H, Sencan I, Kapuagasi A, Ozturk M, Uzundurukan Z, Gokmen D, Ozcan A, Kaymak C, Artemenko VA, Budnyuk A, Pugh R, Bhandari S, Mauri T, Turrini C, Langer T, Taccone P, Volta CA, Marenghi C, Gattinoni L, Pesenti A, Sweeney L, O’Sullivan A, Kelly P, Mukeria E, MacLoughlin R, Pfeffer M, Thomas JT, Bregman GB, Karp GK, Kishinevsky EK, Stavi DS, Adi NA, Poropat T, Knafelj R, Llopart E, Batlle M, De Haro C, Mesquida J, Artigas A, Pavlovic D, Lewerentz L, Spassov A, Schneider R, De Smet S, De Raedt S, Derom E, Depuydt P, Oeyen S, Benoit D, Decruyenaere J, Gobatto A, Besen B, Tierno P, Melro L, Mendes P, Cadamuro F, Park M, Malbouisson LM, Civantos BC, Lopez JL, Robles A, Figueira J, Yus S, Garcia A, Oglinda A, Ciobanu G, Oglinda C, Schirca L, Sertinean T, Lupu V, Kelly P, O’Sullivan A, Sweeney L, MacLoughlin R, O’Sullivan A, Kelly P, Sweeney L, Mukeria E, Wolny M, MacLoughlin R, Pagano A, Numis F, Visone G, Saldamarco L, Russo T, Porta G, Paladino F, Bell C, Liu J, Debacker J, Lee C, Tamberg E, Campbell V, Mehta S, Silva-Pinto A, Sarmento A, Santos L, Kara Ý, Yýldýrým F, Zerman A, Güllü Z, Boyacý N, Basarýk Aydogan B, Gaygýsýz Ü, Gönderen K, Arýk G, Turkoglu M, Aydogdu M, Aygencel G, Ülger Z, Gursel G, Boyacý N, Isýkdogan Z, Özdedeoglu Ö, Güllü Z, Badoglu M, Gaygýsýz U, Aydogdu M, Gursel G, Kongpolprom N, Sittipunt C, Eden A, Kokhanovsky Y, Bursztein – De Myttenaere S, Pizov R, Neilans L, MacIntyre N, Radosevich M, Wanta B, Weber V, Meyer T, Smischney N, Brown D, Diedrich D, Fuller A, McLindon P, Sim K, Shoaeir M, Noeam K, Mahrous A, Matsa R, Ali A, Dridi C, Koubaji S, Kamoun S, Haddad F, Ben Souissi A, Laribi B, Riahi A, Mebazaa MS, Pérez-Calatayud A, Carrillo-Esper R, Zepeda-Mendoza A, Diaz-Carrillo M, Arch-Tirado E, Carbognin S, Pelacani L, Zannoni F, Agnoli A, Gagliardi G, Cho R, Adams A, Lunos S, Ambur S, Shapiro R, Prekker M, Thijssen M, Janssen L, Foudraine N, Voscopoulos CJ, Freeman J, Voscopoulos CJ, Freeman J, George E, Voscopoulos CJ, Eversole D, Freeman J, George E, Muttini S, Bigi R, Villani G, Patroniti N, Williams G, Voscopoulos CJ, Freeman J, George E, Waldmann A, Böhm S, Windisch W, Strassmann S, Karagiannidis C, Waldmann A, Böhm S, Windisch W, Strassmann S, Karagiannidis C, Karagiannidis CK, Waldmann AW, Böhm SB, Strassmann S, Windisch WW, Persson P, Lundin S, Stenqvist O, Porta G, Numis F, Serra CS, Pagano AP, Masarone MM, Rinaldi LR, Amelia AA, Fascione MF, Adinolfi LA, Ruggiero ER, Asota F, O’Rourke K, Ranjan S, Morgan P, DeBacker JW, Tamberg E, O’Neill L, Munshi L, Burry L, Fan E, Mehta S, Poo S, Mahendran K, Fowles J, Gerrard C, Vuylsteke A, Loveridge R, Chaddock C, Patel S, Kakar V, Willars C, Hurst T, Park C, Best T, Vercueil A, Auzinger G, Borgman A, Proudfoot AG, Grins E, Emiley KE, Schuitema J, Fitch SJ, Marco G, Sturgill J, Dickinson MG, Strueber M, Khaghani A, Wilton P, Jovinge SM, Sampson C, Harris-Fox S, Cove ME, Vu LH, Sen A, Federspiel WJ, Kellum JA, Mazo Torre C, Riera J, Ramirez S, Borgatta B, Lagunes L, Rello J, Kuzovlev AK, Moroz V, Goloubev A, Polovnikov S, Nenchuk S, Karavana V, Glynos C, Asimakos A, Pappas K, Vrettou C, Magkou M, Ischaki E, Stathopoulos G, Zakynthinos S, Spadaro S, Kozhevnikova I, Dalla Corte F, Grasso S, Casolari P, Caramori G, Volta C, Andrianjafiarinoa T, Randriamandrato T, Rajaonera T, El-Dash S, Costa ELV, Tucci MR, Leleu F, Kontar L, De Cagny B, Brazier F, Titeca D, Bacari-Risal G, Maizel J, Amato M, Slama M, Mercado P, Maizel J, Kontar L, Titeca D, Brazier F, Riviere A, Joris M, Soupison T, De Cagny B, El Dash S, Slama M, Remmington, Fischer A, Squire S, Boichat M, Honzawa H, Yasuda H, Adati T, Suzaki S, Horibe M, Sasaki M, Sanui M, Marinho R, Daniel J, Miranda H, Marinho A, Milinis K, Cooper M, Williams GR, McCarron E, Simants S, Patanwala I, Welters I, Su Y, Fernández Villanueva J, Fernández Garda R, López Lago A, Rodríguez Ruíz E, Hernández Vaquero R, Tomé Martínez de Rituerto S, Varo Pérez E, Lefel N, Schaap F, Bergmans D, Olde Damink S, Van de Poll M, Tizard K, Lister C, Poole L, Ringaitiene D, Gineityte D, Vicka V, Norkiene I, Sipylaite J, O’Loughlin A, Maraj V, Dowling J, Velasco MB, Dalcomune DM, Dias EB, Fernandes SL, Oshima T, Graf S, Heidegger C, Genton L, Karsegard V, Dupertuis Y, Pichard C, Friedli N, Stanga Z, Mueller B, Schuetz P, Vandersteen L, Stessel B, Evers S, Van Assche A, Jamaer L, Dubois J, Marinho R, Castro H, Moura J, Valente J, Martins P, Casteloes P, Magalhaes C, Cabral S, Santos M, Oliveira B, Salgueiro A, Marinho A, Marinho R, Santos M, Lafuente E, Castro H, Cabral S, Moura J, Martins P, Oliveira B, Salgueiro A, Duarte S, Castro S, Melo M, Casteloes P, Marinho A, Gray S, Maipang K, Bhurayanontachai R, Grädel LG, Schütz P, Langlois P, Manzanares W, Tincu R, Cobilinschi C, Tomescu D, Ghiorghiu Z, Macovei R, Manzanares W, Langlois P, Lemieux M, Elke G, Bloos F, Reinhart K, Heyland D, Langlois P, Lemieux M, Aramendi I, Heyland D, Manzanares W, Su Y, Marinho R, Babo N, Marinho A, Hoshino M, Haraguchi Y, Kajiwara S, Mitsuhashi T, Tsubata T, Aida M, Rattanapraphat T, Bhurayanontachai R, Kongkamol C, Khwannimit B, Marinho R, Santos M, Castro H, Lafuente E, Salgueiro A, Cabral S, Martins P, Moura J, Oliveira B, Melo M, Xavier B, Valente J, Magalhaes C, Casteloes P, Marinho A, Moisidou D, Ampatzidou F, Koutsogiannidis C, Moschopoulou M, Drossos G, Taskin G, Çakir M, Güler AK, Taskin A, Öcal N, Özer S, Yamanel L, Wong JM, Fitton C, Anwar S, Stacey S, Aggou M, Fyntanidou B, Patsatzakis S, Oloktsidou E, Lolakos K, Papapostolou E, Grosomanidis V, Suda S, Ikeda T, Ono S, Ueno T, Izutani Y, Gaudry S, Desailly V, Pasquier P, Brun PB, Tesnieres AT, Ricard JD, Dreyfuss D, Mignon A, White JC, Molokhia A, Dean A, Stilwell A, Friedlaender G, Peters M, Stipulante S, Delfosse A, Donneau AF, Ghuysen A, Feldmann C, Freitag D, Dersch W, Irqsusi M, Eschbach D, Steinfeldt T, Wulf H, Wiesmann T, Kongpolprom N, Cholkraisuwat J, Beitland S, Nakstad E, Stær-Jensen H, Drægni T, Andersen G, Jacobsen D, Brunborg C, Waldum-Grevbo B, Sunde K, Hoyland K, Pandit D, Hayakawa K, Oloktsidou E, Kotzampassi K, Fyntanidou B, Patsatzakis S, Loukipoudi L, Doumaki E, Grosomanidis V, Yasuda H, Admiraal MM, Van Assen M, Van Putten MJ, Tjepkema-Cloostermans M, Van Rootselaar AF, Horn J, Ragusa F, Marudi A, Baroni S, Gaspari A, Bertellini E, Taha A, Abdullah T, Abdel Monem S, Alcorn S, McNeill S, Russell S, Eertmans W, Genbrugge C, Meex I, Dens J, Jans F, De Deyne C, Cholkraisuwat J, Kongpolprom N, Avard B, Burns R, Patarchi A, Spina T, Tanaka H, Otani N, Ode S, Ishimatsu S, Cho J, Moon JB, Park CW, Ohk TG, Shin MC, Won MH, Dakova S, Ramsheva Z, Ramshev K, Cho J, Moon JB, Park CW, Ohk TG, Shin MC, Cho J, Moon JB, Park CW, Ohk TG, Shin MC, Marudi A, Baroni S, Gaspari A, Bertellini E, Orhun G, Senturk E, Ozcan PE, Sencer S, Ulusoy C, Tuzun E, Esen F, Tincu R, Cobilinschi C, Tomescu D, Ghiorghiu Z, Macovei R, Van Assen M, Admiraal MM, Van Putten MJ, Tjepkema-Cloostermans M, Van Rootselaar AF, Horn J, Fallenius M, Skrifvars MB, Reinikainen M, Bendel S, Raj R, Abu-Habsa M, Hymers C, Borowska A, Sivadhas H, Sahiba S, Perkins S, Rubio J, Rubio JA, Sierra R, English S, Chasse M, Turgeon A, Lauzier F, Griesdale D, Garland A, Fergusson D, Zarychanski R, Tinmouth A, Van Walraven C, Montroy K, Ziegler J, Dupont Chouinard R, Carignan R, Dhaliwal A, Lum C, Sinclair J, Pagliarello G, McIntyre L, English S, Chasse M, Turgeon A, Lauzier F, Griesdale D, Garland A, Fergusson D, Zarychanski R, Tinmouth A, Van Walraven C, Montroy K, Ziegler J, Dupont Chouinard R, Carignan R, Dhaliwal A, Lum C, Sinclair J, Pagliarello G, McIntyre L, Groza T, Moreau N, Castanares-Zapatero D, Hantson P, Carbonara M, Ortolano F, Zoerle T, Magnoni S, Pifferi S, Conte V, Stocchetti N, Carteron L, Suys T, Patet C, Quintard H, Oddo M, Rubio JA, Rubio J, Sierra R, Spatenkova V, Pokorna E, Suchomel P, Ebert N, Jancik J, Rhodes H, Bylinski T, Hawthorne C, Shaw M, Piper I, Kinsella J, Kink AK, Rätsep IR, Boutin A, Moore L, Chasse M, Zarychanski R, Lauzier F, English S, McIntyre L, Lacroix J, Griesdale D, Lessard-Bonaventure P, Turgeon AF, Boutin A, Moore L, Green R, Lessard-Bonaventure P, Erdogan M, Butler M, Lauzier F, Chasse M, English S, McIntyre L, Zarychanski R, Lacroix J, Griesdale D, Desjardins P, Fergusson DA, Turgeon AF, Goncalves B, Vidal B, Valdez C, Rodrigues AC, Miguez L, Moralez G, Hong T, Kutz A, Hausfater P, Amin D, Struja T, Haubitz S, Huber A, Mueller B, Schuetz P, Brown T, Collinson J, Pritchett C, Slade T, Le Guen M, Hellings S, Ramsaran R, Alsheikhly A, Abe T, Kanapeckaite L, Abu-Habsa M, Bahl R, Russell MQ, Real KJ, Abu-Habsa M, Lyon RM, Oveland NP, Penketh J, Mcdonald M, Kelly F, Alfafi M, Alsolamy S, Almutairi W, Alotaibi B, Van den Berg AE, Schriel Y, Dawson L, Meynaar IA, Talaie H, Silva D, Fernandes S, Gouveia J, Santos Silva J, Foley J, Kaskovagheorgescu A, Evoy D, Cronin J, Ryan J, Huck M, Hoffmann C, Renner J, Laitselart P, Donat N, Cirodde A, Schaal JV, Masson Y, Nau A, Leclerc T, Howarth O, Davenport K, Jeanrenaud P, Raftery S, MacTavish P, Devine H, McPeake J, Daniel M, Kinsella J, Quasim T, Alrabiee S, Alrashid A, Alsolamy S, Gundogan O, Bor C, Akýn Korhan E, Demirag K, Uyar M, Frame F, Ashton C, Bergstrom Niska L, Dilokpattanamongkol P, Suansanae T, Suthisisang C, Morakul S, Karnjanarachata C, Tangsujaritvijit V, Mahmood S, Al Thani H, Almenyar A, Vakalos A, Avramidis V, Sharvill R, Penketh J, Morton SE, Chiew YS, Pretty C, Chase JG, Shaw GM, Knafelj R, Kordis P, Patel S, Grover V, Kuchyn I, Bielka K, Aidoni Z, Grosomanidis V, Kotzampassi K, Stavrou G, Fyntanidou B, Patsatzakis S, Skourtis C, Lee SD, Williams K, Weltes ID, Berhane S, Arrowsmith C, Peters C, Robert S, Caldas J, Panerai RB, Robinson TG, Camara L, Ferreira G, Borg-Seng-Shu E, De Lima Oliveira M, Mian NC, Santos L, Nogueira R, Zeferino SP, Jacobsen Teixeira M, Galas F, Hajjar LA, Killeen P, McPhail M, Bernal W, Maggs J, Wendon J, Hughes T, Taniguchi LU, Siqueira EM, Vieira Jr JM, Azevedo LC, Ahmad AN, Abu-Habsa M, Bahl R, Helme E, Hadfield S, Loveridge R, Shak J, Senver C, Howard-Griffin R, Wacharasint P, Fuengfoo P, Sukcharoen N, Rangsin R, Sbiti-Rohr D, Schuetz P, Na H, Song S, Lee S, Jeong E, Lee K, Cooper M, Milinis K, Williams G, McCarron E, Simants S, Patanwala I, Welters ID, Zoumpelouli E, Volakli EA, Chrysohoidou V, Georgiou S, Charisopoulou K, Kotzapanagiotou E, Panagiotidou V, Manavidou K, Stathi Z, Sdougka M, Salahuddin N, AlGhamdi B, Marashly Q, Zaza K, Sharshir M, Khurshid M, Ali Z, Malgapo M, Jamil M, Shafquat A, Shoukri M, Hijazi M, Abe T, Uchino S, Takinami M, Rangel Neto NR, Oliveira S, Reis FQ, Rocha FA, Moralez G, Ebecken K, Rabello LS, Lima MF, Hatum R, De Marco FV, Alves A, Pinto JE, Godoy M, Brasil PE, Bozza FA, Salluh JI, Soares M, Krinsley J, Kang G, Perry J, Hines H, Wilkinson KM, Tordoff C, Sloan B, Bellamy MC, Moreira E, Verga F, Barbato M, Burghi G, Soares M, Silva UV, Azevedo LC, Torelly AP, Kahn JM, Angus DC, Knibel MF, Brasil PE, Bozza FA, Salluh JI, Velasco MB, Dalcomune DM, Marshall R, Gilpin T, Tridente A, Raithatha A, Mota D, Loureiro B, Dias J, Afonso O, Coelho F, Martins A, Faria F, Al-Dorzi H, Al Orainni H, AlEid F, Tlaygeh H, Itani A, Hejazi A, Arabi Y, Gaudry S, Messika J, Ricard JD, Guillo S, Pasquet B, Dubief E, Dreyfuss D, Tubach F, Battle C, James K, Temblett P, Davies L, Battle C, Lynch C, Pereira S, Cavaco S, Fernandes J, Moreira I, Almeida E, Seabra Pereira F, Malheiro M, Cardoso F, Aragão I, Cardoso T, Fister M, Knafelj R, Muraray Govind P, Brahmananda Reddy N, Pratheema R, Arul ED, Devachandran J, Velasco MB, Dalcomune DM, Knafelj R, Fister M, Chin-Yee N, D’Egidio G, Thavorn K, Heyland D, Kyeremanteng K, Murchison AG, Swalwell K, Mandeville J, Stott D, Guerreiro I, Devine H, MacTavish P, McPeake J, Quasim T, Kinsella J, Daniel M, Goossens C, Marques MB, Derde S, Vander Perre S, Dufour T, Thiessen SE, Güiza F, Janssens T, Hermans G, Vanhorebeek I, De Bock K, Van den Berghe G, Langouche L, Devine H, MacTavish P, Quasim T, Kinsella J, Daniel M, McPeake J, Miles B, Madden S, Devine H, Weiler M, Marques P, Rodrigues C, Boeira M, Brenner K, Leães C, Machado A, Townsend R, Andrade J, MacTavish P, McPeake J, Devine H, Kinsella J, Daniel M, Kishore R, Fenlon C, Quasim T, Fiks T, Ruijter A, Te Raa M, Spronk P, Chiew YS, Docherty P, Dickson J, Moltchanova E, Scarrot C, Pretty C, Shaw GM, Chase JG, Hall T, Ngu WC, Jack JM, Morgan P, Avard B, Pavli A, Gee X, Bor C, Akin Korhan E, Demirag K, Uyar M, Shirazy M, Fayed A, Gupta S, Kaushal A, Dewan S, Varma A, Ghosh E, Yang L, Eshelman L, Lord B, Carlson E, Helme E, Broderick R, Hadfield S, Loveridge R, Ramos J, Forte D, Yang F, Hou P, Dudziak J, Feeney J, Wilkinson K, Bauchmuller K, Shuker K, Faulds M, Raithatha A, Bryden D, England L, Bolton N, Tridente A, Bauchmuller K, Shuker K, Tridente A, Faulds M, Matheson A, Gaynor J, Bryden D; S South Yorkshire Hospitals Research Collaboration, Ramos J, Peroni B, Daglius-Dias R, Miranda L, Cohen C, Carvalho C, Velasco I, Forte D, Kelly JM, Neill A, Rubenfeld G, Masson N, Min A, Boezeman E, Hofhuis J, Hovingh A, De Vries R, Spronk P, Cabral-Campello G, Aragão I, Cardoso T, Van Mol M, Nijkamp M, Kompanje E, Ostrowski P, Omar A, Kiss K, Köves B, Csernus V, Molnár Z, Hoydonckx Y, Vanwing S, Stessel B, Van Assche A, Jamaer L, Dubois J, Medo V, Galvez R, Miranda JP, Stone C, Wigmore T, Arunan Y, Wheeler A, Bauchmuller K, Bryden D, Wong Y, Poi C, Gu C, Molmy P, Van Grunderbeeck N, Nigeon O, Lemyze M, Thevenin D, Mallat J, Ramos J, Correa M, Carvalho RT, Forte D, Fernandez A, McBride C, Koonthalloor E, Walsh C, Webber A, Ashe M, Smith K, Jeanrenaud P, Marudi A, Baroni S, Ragusa F, Bertellini E, Volakli EA, Chochliourou E, Dimitriadou M, Violaki A, Mantzafleri P, Samkinidou E, Vrani O, Arbouti A, Varsami T, Sdougka M, Bollen JA, Van Smaalen TC, De Jongh WC, Ten Hoopen MM, Ysebaert D, Van Heurn LW, Van Mook WN, Sim K, Fuller A, Roze des Ordons A, Couillard P, Doig C, Van Keer RV, Deschepper RD, Francke AF, Huyghens LH, Bilsen JB, Nyamaizi B, Dalrymple C, Molokhia A, Dobru A, Marrinan E, Ankuli A, Molokhia A, McPeake J, Struthers R, Crawford R, Devine H, Mactavish P, Quasim T, Morelli P, Degiovanangelo M, Lemos F, MArtinez V, Verga F, Cabrera J, Burghi G, Rutten A, Van Ieperen S, De Geer S, Van Vugt M, Der Kinderen E, Giannini A, Miccinesi G, Marchesi T, Prandi E. 36th International Symposium on Intensive Care and Emergency Medicine : Brussels, Belgium. 15-18 March 2016. Crit Care. 2016;20:94. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 261] [Cited by in RCA: 300] [Article Influence: 33.3] [Reference Citation Analysis (0)] |
| 44. | Strauss MB, Davis RK, Rosenbaum JD, Rossmeisl EC. Water diuresis produced during recumbency by the intravenous infusion of isotonic saline solution. J Clin Invest. 1951;30:862-868. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 198] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 45. | Duarte K, Monnez JM, Albuisson E, Pitt B, Zannad F, Rossignol P. Prognostic Value of Estimated Plasma Volume in Heart Failure. JACC Heart Fail. 2015;3:886-893. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 113] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 46. | Yoshihisa A, Abe S, Sato Y, Watanabe S, Yokokawa T, Miura S, Misaka T, Sato T, Suzuki S, Oikawa M, Kobayashi A, Yamaki T, Kunii H, Saitoh SI, Takeishi Y. Plasma volume status predicts prognosis in patients with acute heart failure syndromes. Eur Heart J Acute Cardiovasc Care. 2018;7:330-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 35] [Article Influence: 4.4] [Reference Citation Analysis (0)] |