Published online May 14, 2025. doi: 10.3748/wjg.v31.i18.103778
Revised: February 26, 2025
Accepted: April 16, 2025
Published online: May 14, 2025
Processing time: 163 Days and 5 Hours
Idiopathic myointimal hyperplasia of the mesenteric veins (IMHMV) is a rare disease characterized by narrowing of the lumen caused by mesenteric vein intimal hyperplasia, resulting in chronic intestinal ischemia. Although the colo
In this case report, we present a unique instance of IMHMV exclusively occurring in the small intestine. The patient experienced small intestinal perforation, infarction, and obstruction before receiving a clear diagnosis, which was achieved only during the third operation. In this review, we analyzed 84 reported cases to summarize the etiology, clinical manifestations, and diagnostic challenges of IMHMV, with the aim of raising awareness regarding this rare condition among clinicians.
Notably, IMHMV can also affect the small intestine alone. When refractory enteritis with endoscopic findings of nonspecific ischemic changes is encountered, IMHMV should be considered for potential diagnosis.
Core Tip: Idiopathic myointimal hyperplasia of the mesenteric veins (IMHMV) is a rare vascular disorder that typically affects the colorectum but can also involve the small intestine. We present a unique case of IMHMV exclusively affecting the small intestine, in which the patient experienced small intestinal perforation, infarction, and obstruction before a definitive diagnosis was made. This report emphasizes the importance of early recognition and highlights the diagnostic challenges faced by patients. A review of 84 cases helps increase awareness and understanding of the clinical presentation, diagnosis, and management of IMHMV.
- Citation: Jiang ZX, Yuan LW, Peng LX, Yang LC, Zhang YW, Wu Q, Yao BJ, Wang XH. Idiopathic myointimal hyperplasia of the mesenteric veins affecting the small intestine alone: A case report and review of literature. World J Gastroenterol 2025; 31(18): 103778
- URL: https://www.wjgnet.com/1007-9327/full/v31/i18/103778.htm
- DOI: https://dx.doi.org/10.3748/wjg.v31.i18.103778
Idiopathic myointimal hyperplasia of the mesenteric veins (IMHMV) is a rare disease characterized by narrowing or occlusion of the venous lumen due to mesenteric venous intimal hyperplasia, leading to chronic intestinal ischemia[1]. This condition is more prevalent in males, with the rectum and sigmoid being common sites of occurrence. It can occasionally affect the small intestine. To date, there have been only seven documented cases of IMHMV exclusively affecting the small intestine worldwide[2] (Table 1). Following radical surgical resection, the incidence of recurrence is exceedingly minimal. In this study, we present a case of IMHMV involving exclusively the small intestine, which was pathologically confirmed after three surgical interventions over an extended period of time.
| Case | Ref. | Age (year)/sex | Symptoms | Affected site | Clinical impression | Indication for surgery | Time to surgery | Follow-up |
| 1 | Current case | 50/F | Abdominal pain, abdominal distension | Terminal ileum | CD | Bowel obstruction | 6 years (this operation)/1 year (the first operation) | 1 month |
| 2 | Li et al[7] | 64/M | Abdominal pain, abdominal distension, weight loss | Terminal ileum | IBD | Bowel obstruction | 6 months | 1 year |
| 3 | Yamada et al[24] | 81/F | Abdominal pain, nausea and vomiting | Terminal ileum | Adhesive intestinal obstruction | Bowel obstruction | 1 year | 32 months |
| 4 | Guadagno et al[47] | 59/F | Abdominal pain, diarrhea, weight loss | Ileum | CD | Bowel obstruction | 6 months | 3 months |
| 5 | Laskaratos et al[25] | 62/F | Abdominal pain, diarrhea | Terminal ileum | IBD | Perforation | - | - |
| 6 | Lanitis et al[37] | 81/M | Abdominal pain, abdominal distension, constipation, weight loss, anorexia, bilateral lower limb edema | Terminal ileum | - | Appendiceal mucocoele and pseudomyxoma peritonei | 6 months | - |
| 7 | Bryant[30] | 42/F | Chest pain, seizures | Jejunum | - | - | - | - |
| 8 | Louie et al[27] | 57/F | Abdominal pain, nausea | Jejunum/ileum | - | CT scan showed bowel ischemia | - | 24 months |
| 9 | Martin et al[43] | 63/M | Diarrhea, hematochezia, weight loss, fever | Rectum - DC | IC | Persisting symptoms | 3.75 months | - |
| 10-13 | Lincango et al[42] | Mean 55 (range 45-61)/4 M | Abdominal pain (n = 3), diarrhea (n = 1), fever (n = 1), tenesmus (n = 2), rectal pain (n = 1), constipation and diarrhea alternated | Rectum - DC (n = 1), SC (n = 1), SC - DC (n = 1), RS (n = 1) | UC (n = 2), IC (n = 1), UC/IC (n = 1) | Medically refractory | > 10 days (n = 1) | Mean 69 months (range 12-144 months) |
| 14 | Al Ansari et al[18] | 63/M | Abdominal pain, diarrhea | SC - DC | Entamoeba histolytica colitis | Persisting symptoms | 41 days | 5 years |
| 15-26 | Kim et al[19] | Mean 66 (range 58-77)/11 M and 1F | Abdominal pain (n = 10), diarrhea (n = 9), constipation (n = 3), mucoid stools (n = 3), perianal pain | RS (n = 9), rectum - DC (n = 2), TC - terminal ileum | IC (n = 4); UC (n = 1), nonspecific colitis (n = 1), CMV colitis (n = 1), idiopathic phlebosclero colitis (n = 1), IMHMN (n = 3) | - | Mean 3 months (range 1-8 months) | Mean 29 months (range 2-125 months) |
| 27 | Chudy-Onwugaje et al[48] | 54/M | Abdominal pain, diarrhea, weight loss | TC | CMV colitis | Persisting symptoms | 4 months | - |
| 28 | Zhou et al[44] | 67/M | Abdominal pain, diarrhea, hematochezia, weight loss | Rectum - DC | UC | Persisting symptoms | 6.25 months | - |
| 29 | Han et al[31] | 74/M | Abdominal pain, diarrhea, hematochezia, weight loss | Rectum - TC | IMHMV | Persisting symptoms, IMHMV was suspected | 1 year | 5.5 months |
| 30 | Kelly et al[38] | 53/M | Abdominal pain, hematochezia, weight loss, tenesmus | Rectum - DC | UC/IMHMV | Persisting symptoms | 3 months | 3 months |
| 31 | Noujaim et al[49] | 66/M | Abdominal pain, diarrhea, hematochezia, weight loss, fever, night sweats | Rectum - DC | IBD/IMHMV/C. difficile infection | Acute abdomen | > 2 months | Died on postoperative day 4 |
| 32 | Yun et al[20] | 64/M | Abdominal pain, diarrhea, hematochezia | Rectum - TC | Non-thrombotic veno-occlusive disease, such as IMHMV | IMHMV was suspected | 2 years | 6 months |
| 33 | Almumtin et al[46] | 55/M | Abdominal pain, hematochezia, weight loss, constipation, fever | Rectum - TC | IBD | Perforation | 1 year | - |
| 34 | Shah et al[12] | 24/F | Abdominal pain, hematochezia | Rectum - DC | IC | Abdominal pain/perforation | > 1 month | - |
| 35 | Kawasaki et al[17] | 71/M | Abdominal pain, constipation | RS | IMHMV | IMHMV was suspected | 4 months | 8 months |
| 36 | Wong et al[21] | 72/M | Abdominal pain, diarrhea, hematochezia | Rectum - DC | IC/IMHMV | Acutely worsening abdominal pain with peritoneal signs | Several days | - |
| 37 | Dillione et al[50] | 47/M | Abdominal pain, hematochezia | RS | Ischemic proctitis | Persisting symptoms | Several weeks | - |
| 38 | Wangensteen et al[28] | 62/F | Abdominal pain, diarrhea, hematochezia | Rectum - DC | UC (initial)/IMHMV | Persisting symptoms, IMHMV was suspected | > 3 months | 1.5 years |
| 39-48 | Yantiss et al[35] | Mean 68 (range 25-83)/9 M and 1F | Abdominal pain (n = 6), diarrhea (n = 10), hematochezia (n = 9), weight loss (n = 2), Palpable mass | Rectum - DC (n = 7), SC (n = 1), SC - DC (n = 1) | IC/IBD (n = 1), IBD (n = 7), IC (n = 2) | Perforation (n = 5), obstruction and refractory colitic symptoms | - | - |
| 49 | AbiMansour et al[40] | 59/M | Abdominal pain, diarrhea, urgency | SC | Diverticulitis | Persisting symptoms | 1 year | - |
| 50 | Patel et al[51] | 65/M | Abdominal pain, rectal urgency, tenesmus | Rectum - DC | CD/IMHMV | Perforation | > 1.5 months | - |
| 51 | Morimura et al[11] | 44/M | Abdominal pain, constipation, fever | Rectum - TC | IBD/Eosinophilic enteritis | Bowel ischemia and necrosis with peritonitis | > 1 month | 1 year |
| 52 | Xie et al[52] | 21/F | Abdominal pain, diarrhea, hematochezia, fever, tenesmus | RS | Acute IBD | Massive hematochezia, shock | > 20 days | 2 years |
| 53 | Cauchois et al[53] | 48/M | Abdominal pain, diarrhea, hematochezia, fever, weight loss | RS | UC | Persistent symptoms | 5 months | - |
| 54 | Costa et al[33] | 47/M | Abdominal pain, diarrhea, hematochezia, fever, tenesmus, proctalgia, fecal incontinence | RS | IBD/IC | Persistent symptoms | 9 months | - |
| 55-62 | Anderson et al[34] | Median 62.5 (range 22-75)/6 M and 2F | Abdominal pain (n = 7), diarrhea (n = 5), hematochezia (n = 4) | SC (n = 6) | IBD (n = 3) | - | - | - |
| 63 | Mohtashami et al[45] | 61/M | Abdominal pain, diarrhea, hematochezia, abdominal distension | Rectum - DC | CD | Perforation | 3 weeks | - |
| 64 | Gonai et al[54] | 68/M | Abdominal distension, constipation, mucoid stools | SC - DC | Chronic venous ischemic disease | Persistent symptoms | - | - |
| 65 | Sahara et al[1] | 76/M | Abdominal pain, diarrhea | RS | UC/IC | Severe pain | 13 months | 3 months |
| 66 | García-Castellanos et al[32] | 32/F | Abdominal pain, diarrhea, hematochezia | Rectum - DC | Primary pneumatosis intestinalis, IC | Persistent rectal bleeding, severe pain | 3 months | 24 months |
| 67 | Feo et al[55] | 75/F | Abdominal pain, diarrhea, hematochezia, weight loss, tenesmus | RS | IC | Persistent symptoms | 6 months | - |
| 68 | Bhatt et al[29] | 82/M | Abdominal distension, diarrhea, erratic bowel movements, urgency, mucoid stools, weight loss | Rectum - DC | IC | Persistent symptoms | 3 months | > 1 year |
| 69 | Bhatt et al[29] | 59/M | Diarrhea, tenesmus | RS | Diverticulitis (initial)/IMHMV | Persistent symptoms/ MRI suggested IMHMV | - | > 1 year |
| 70 | Abbott et al[56] | 58/M | Abdominal pain, diarrhea, hematochezia | Rectum - DC | Entameba histolytica infection/IBD | Persistent symptoms | Several weeks | - |
| 71-74 | Genta and Haggitt[3] | Mean 40 (range 25-67)/4 M | Abdominal pain (n = 4), hematochezia | SC (n = 1), Rectum - DC (n = 1), RS (n = 2) | UC (n = 2), CD (n = 1), Stricture (n = 1) | Bowel obstruction (n = 1), toxic megacolon (n = 1), abdominal pain and hematochezia (n = 2) | Mean 3 months (range 1-6 months) | Mean 3.5 years (range 1-7 years) |
| 75 | Kao et al[9] | 38/M | Abdominal pain, rectalgia, constipation, hematochezia, mucoid stools, weight loss | RS | Idiopathic chronic IBD | Perforation | 5 months | 18 months |
| 76 | Yang et al[22] | 44/M | Abdominal pain, diarrhea, hematochezia | RS | UC/IC | Persistent symptoms | 2 months | - |
| 77 | Savoie et al[57] | 22/M | Abdominal pain, diarrhea, hematochezia, tenesmus | RS | UC | Persistent symptoms | > 2 weeks | 10 months |
| 78 | Abu-Alfa et al[4] | 58/M | Abdominal pain, diarrhea, hematochezia | SC | IBD/IC | Persistent bleeding, severe pain | 1 year | - |
| 79 | Chiang et al[39] | 60/M | Abdominal pain, diarrhea, hematochezia, weight loss | RS | UC | Persistent symptoms | 2 months | 4 months |
| 80 | Coombs et al[23] | 33/M | Abdominal pain, constipation, hematochezia | RS | IC | Persistent rectal bleeding and abdominal pain | 4 weeks | - |
| 81 | Uwah et al[36] | 37/M | Abdominal pain, constipation and diarrhea alternated, hematochezia | Rectum - DC | IBD/IC | Persistent symptoms/stricture | > 2 months | - |
| 82 | Uwah et al[36] | 49/M | Abdominal pain, diarrhea, hematochezia | Rectum - DC | Colitis of unknown etiology | Persistent symptoms | Several months | - |
| 83 | López et al[58] | 37/F | Abdominal pain, diarrhea | Rectum - terminal ileum | CD | Acute abdomen | 7 months | Died |
| 84 | Song et al[26] | 59/M | Abdominal pain, abdominal distension, constipation and diarrhea alternated, Incontinence | Rectum - terminal ileum | CD | Persistent symptoms | - | - |
| 85 | Louie et al[27] | 45/M | Lower gastrointestinal bleeding | RS | UC | - | - | - |
We conducted a literature review using the search term "Idiopathic Myointimal Hyperplasia of the Mesenteric Veins" or "IMHMV" in the PubMed database, which yielded 64 articles published between 1991 and 2024. After the titles and abstracts of these articles were screened, only 48 articles that contained actual case reports were included. A total of 84 reported cases of IMHMV were collected from these articles (Table 1). We conducted a detailed review of the full texts of these 48 articles. Based on the collected data, an updated overview of the etiology, clinical features, endoscopic findings, imaging characteristics, and pathological features of IMHMV is provided.
A 50-year-old female patient presented with a 6-year history of recurrent abdominal pain and distension, with exacerbation over the past 4 months.
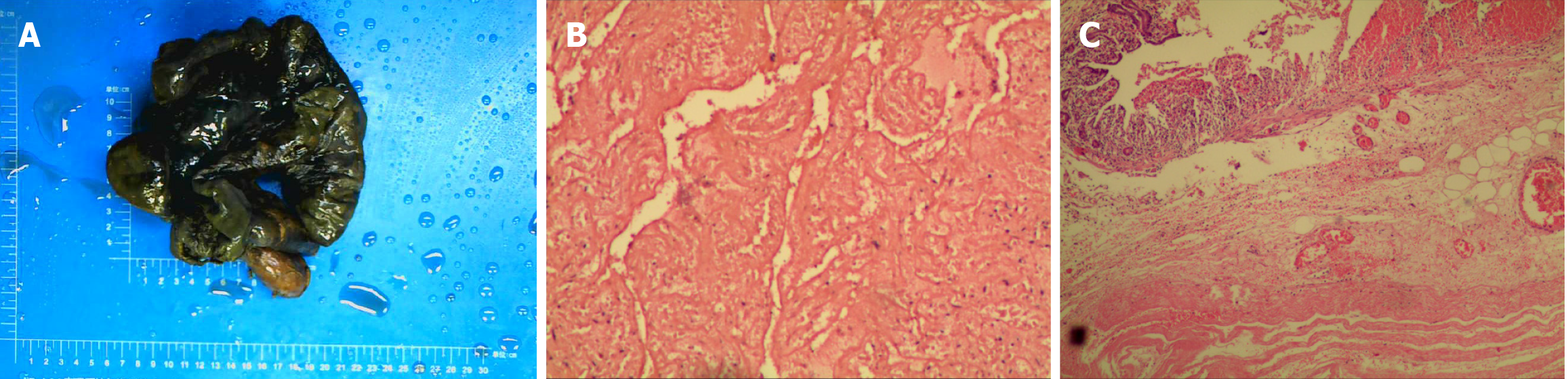
Six years prior, the patient experienced abdominal pain and was diagnosed with eosinophilic gastroenteritis at a local hospital. She was treated with prednisone (25 mg daily) for approximately 1 month before her medication was discontinued on her own. One year later, she experienced a sudden exacerbation of her abdominal pain. Suspecting intestinal perforation, surgeons performed emergency small bowel perforation repair. Small bowel perforation was found during surgery, and some small red nodules in the mesentery at the site of small bowel perforation were noted. Histopathological examination revealed that these nodules were fibroadipose tissue with inflammation. Two years later, the patient developed vomiting. Computed tomography (CT) imaging revealed small bowel wall thickening, edema, and intestinal dilation, leading to a diagnosis of incomplete intestinal obstruction. Conservative management failed to alleviate symptoms, necessitating exploratory laparotomy. Intraoperatively, approximately 80 cm of the jejunum exhibited ischemic necrosis, which was resected (Figure 1A), followed by small bowel anastomosis. Postoperative histopathology (Figure 1B and C) revealed small bowel infarction without specific features. After the operation, the patient still experienced recurrent abdominal pain and abdominal distension. Glucocorticoids were used intermittently, but they were ineffective and the symptoms continued to worsen. Therefore, the patient came to our unit for medical treatment.
Apart from the previously mentioned eosinophilic gastroenteritis, the patient has no history of chronic conditions including hypertension, diabetes mellitus, or cardiovascular disease.
The patient denied any family history or history of smoking, alcohol consumption, toxin exposure, or contact with contaminated water sources.
The patient weighed 33 kg and was 156 cm tall. Her vital signs were as follows: Temperature, 36.3 °C; blood pressure, 80/59 mmHg; heart rate, 80 beats per minute; and respiratory rate, 18 breaths per minute. Physical examination did not reveal any significant positive findings.
The hemoglobin levels were within normal limits. However, the fecal occult blood test was positive, and the serum albumin level decreased to 27.5 g/L. No problems related to the function of other organs or to infectious diseases were detected.
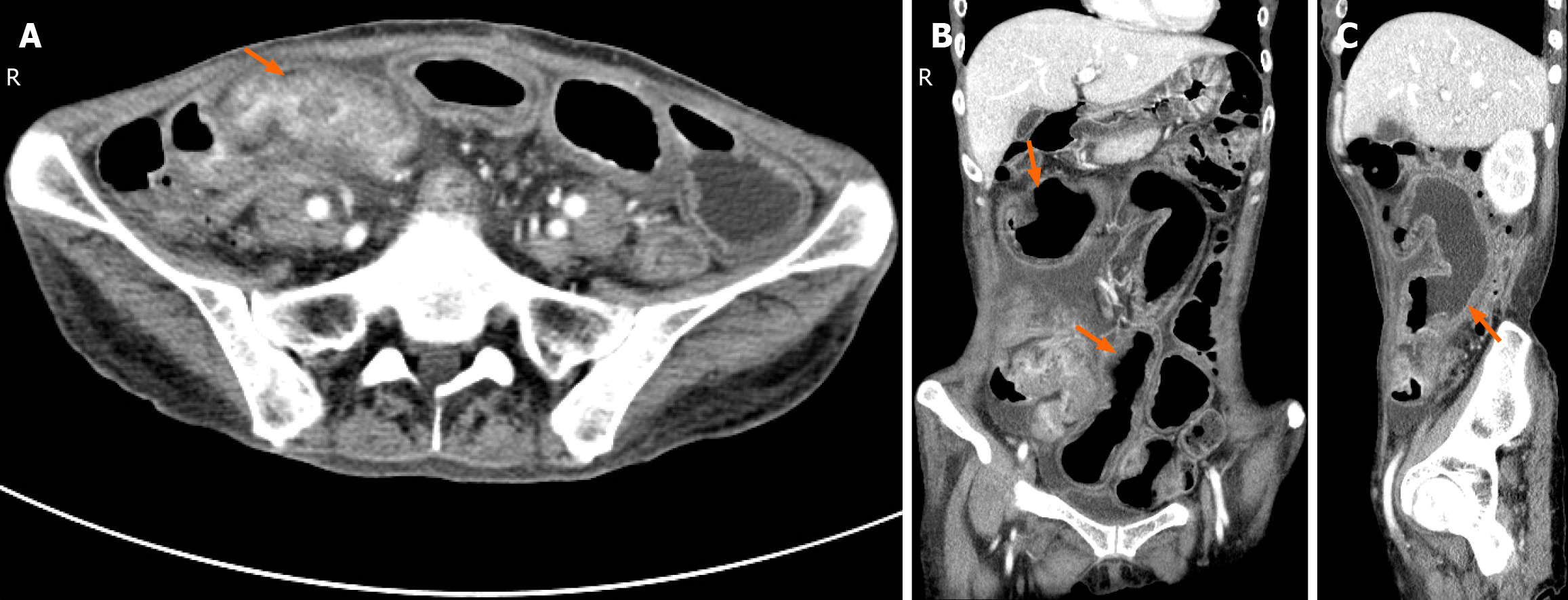
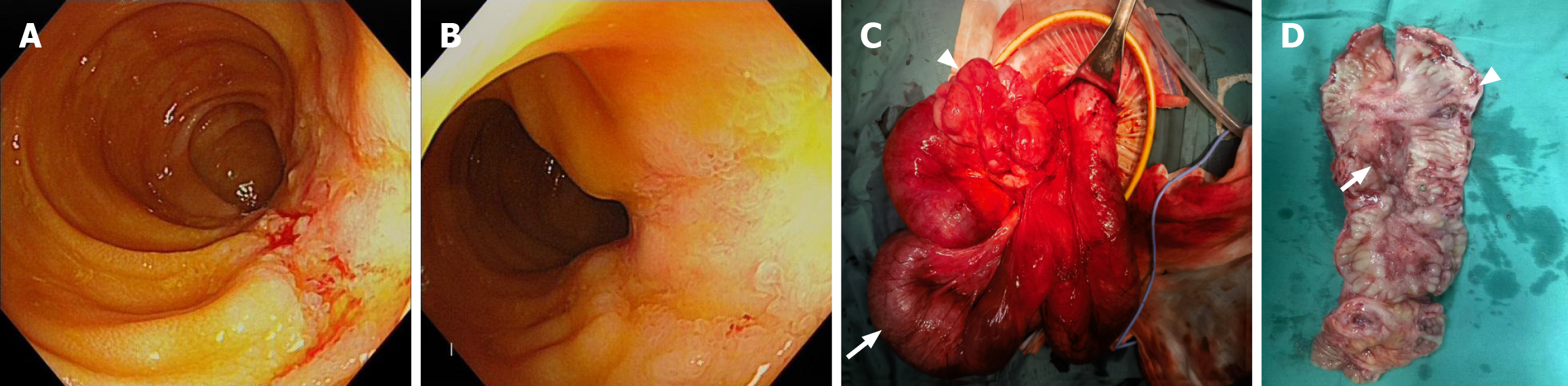
Contrast-enhanced abdominal CT revealed wall thickening of the terminal ileum, a narrow lumen, and proximal small bowel dilation (Figure 2). Electronic colonoscopy revealed a longitudinal ulcer approximately 8 cm long in the terminal ileum, and the ileocecal valve mucosa was congested and swollen (Figure 3A and B). No obvious abnormalities were found in the rest of the colorectum. Severe chronic inflammatory changes in the terminal ileum, ulceration, and crypt epitheliitis were observed microscopically. More lymphocytes and plasma cells infiltrated the lamina propria of the ileocecal valve. No obvious noncaseating granulomatous nodules were found in any part of the sample.
The final diagnoses included the following: (1) IMHMV; (2) Incomplete small bowel obstruction; (3) Status post-small bowel perforation repair; and (4) Status postpartial jejunal resection.
A multidisciplinary consultation initially considered the diagnosis of Crohn's disease. However, the evidence was insufficient. The patient had severe small bowel obstruction and required urgent surgical treatment to relieve the obstruction. During the operation, the ileum 50 cm away from the ileocecal region was tortuous and formed a mass. The intestinal wall was thickened, and it was close to complete obstruction. The small intestine before the obstruction site was severely dilated and edematous (Figure 3C). Therefore, the lesion was excised. Considering the patient's poor nutritional status and severe intestinal wall edema, ileostomy was performed. The specimens dissected during surgery showed marked constriction and ulceration (Figure 3D).
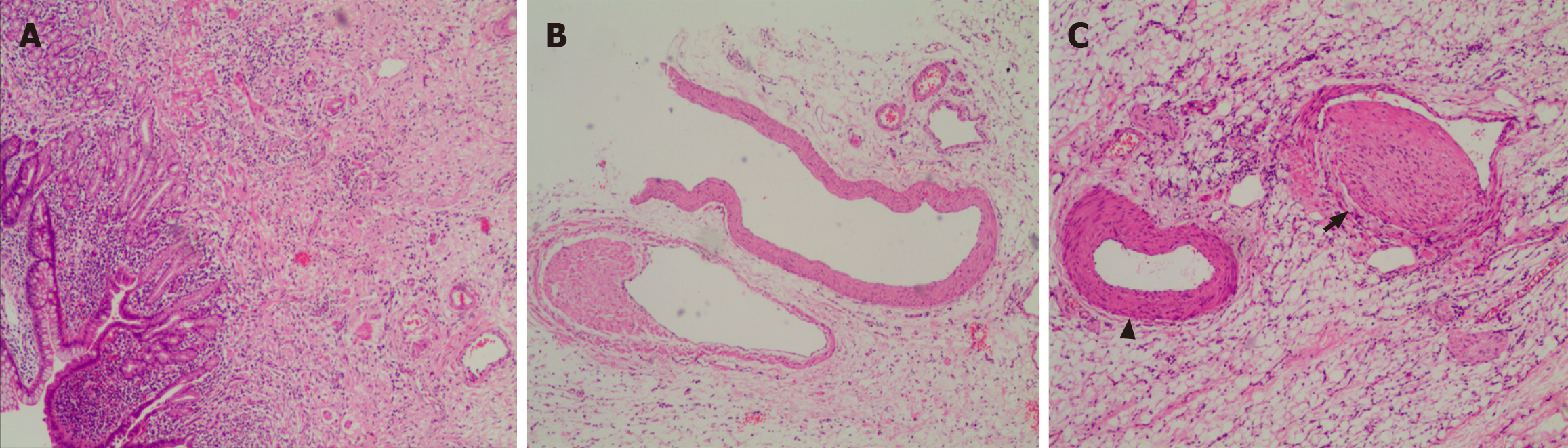
Pathology (Figure 4) revealed irregular hyperplasia of venous intimal smooth muscle cells in the subserosa of the intestinal wall and mesentery, a narrowed lumen, no vasculitis, and normal accompanying arteries. Ultimately, IMHMV was diagnosed.
Antibiotics and parenteral nutrition were administered after the operation. The patient was discharged from the hospital 1 week later. One month later, the patient experienced no recurrence of abdominal pain.
IMHMV is an extremely rare vascular disease of the intestine, and its precise etiology remains unclear. Currently, two main hypotheses prevail: The arteriovenous fistula (AVF) formation hypothesis and the mesenteric venous inflammation hypothesis.
AVF formation hypothesis: The hypothesis posits that intermittent torsion or stretching of the sigmoid mesentery could lead to the development of anomalous arteriovenous connections[3,4]. This process may increase venous blood flow and pressure, promoting intimal smooth muscle proliferation and luminal narrowing, which could subsequently precipitate IMHMV. This theory is based on the ease of mobility of the sigmoid colon and the noted resemblance between venous pathological alterations in IMHMV patients and those observed in patients with unsuccessful cardiac saphenous vein bypass grafts or AVF stenosis in individuals undergoing dialysis[5-7]. Additionally, a retrospective analysis indicated that individuals with prior abdominal trauma had a greater incidence of focal IMHMV-like alterations, lending indirect support to the notion that IMHMV might stem from torsional or stretching injuries to the sigmoid colon[8]. However, AVFs were not detected in postoperative pathology specimens from IMHMV patients reported in the literature or in our case; this may be attributed to the difficulty in identifying arteriovenous malformations in pathological samples[9]. Preoperatively, only one-third of patients underwent cross-sectional vascular imaging, and only 5% of patients underwent dynamic mesenteric angiography[10]. Furthermore, fistula detection remains highly challenging and is frequently overlooked, even with advanced imaging techniques such as specialized CT and magnetic resonance angiography. To date, only 2 patients with abnormal arteriovenous connections identified during preoperative angiography have been reported[11,12]. In one of these cases, endovascular embolization was performed on the suspected arteriovenous connection; however, the patient's pain recurred 11 days later and increased to pre-embolization levels approximately 26 days after the procedure. Ultimately, the arteriovenous connection in this patient was deemed a secondary, nonspecific alteration potentially associated with IMHMV and/or chronic thrombosis of the inferior mesenteric vein[12]. Therefore, further case studies and targeted studies are needed to substantiate this hypothesis. Additionally, this theory fails to account for cases involving intestinal segments beyond the sigmoid colon, particularly those involving IMHMV confined exclusively to the small intestine.
Mesenteric venous inflammation hypothesis: This hypothesis originates from a case report of enterocolic lymphocytic phlebitis (ELP) with marked myointimal hyperplasia, in which postoperative pathological findings demonstrated features common to both ELP and IMHMV[13]. This finding suggests a potential pathological spectrum linking IMHMV and ELP, with the venous injury observed in IMHMV potentially resulting from prolonged chronic inflammation, which is characteristic of ELP. Chronic ELP is characterized by relatively mild lymphocytic infiltration, slower disease progression, and a predilection for the right colon and terminal ileum-features that share some similarities with our case[14,15]. ELP and IMHMV were indeed previously categorized as the same entity. However, considering the distinct histological features and clinical presentations of IMHMV and ELP, they are generally regarded as two separate diseases[16]. Most importantly, neither our case nor the literature review revealed lymphocytic infiltrative inflammation in the affected veins of IMHMV patients using postoperative pathology. To date, only one surgical specimen reported by Kawasaki et al[17] demonstrated minimal perivascular lymphocytic infiltration in an IMHMV patient, but no evidence of phlebitis was found.
Other potential contributing factors: In addition to the aforementioned mechanisms, the pre-existing conditions and medication history of patients may also play a role in the development of IMHMV[9,18]. Most IMHMV patients were previously healthy. Among the 85 patients we reviewed, only 25 reported a history of chronic diseases, and these conditions did not appear to be significantly correlated with the occurrence of vascular abnormalities. Interestingly, 12 of these 25 patients had a history of hypertension, suggesting that microcirculatory abnormalities and hemodynamic changes associated with hypertension might increase their risk of IMHMV. Furthermore, some IMHMV patients had a history of abdominal surgeries or trauma, including colectomy for colonic adenocarcinoma (n = 3), ileostomy (n = 2), small bowel resection (n = 2), appendectomy alone (n = 1), combined appendectomy and cholecystectomy (n = 1), liver transplantation (n = 3), kidney transplantation (n = 1), radical prostatectomy (n = 2), and splenectomy (n = 1)[19-27]. Notably, the patient in our study also underwent two prior intestinal surgeries, including small bowel perforation repair and partial jejunal resection. A history of abdominal surgery may have similarly contributed to an increased risk of developing IMHMV[8].
IMHMV is an extremely rare disease. Since its first description by Genta and Haggitt[3] in 1991, only 85 cases have been reported in the literature. However, this number may underestimate the true incidence of the disease, as preoperative imaging and endoscopic findings are often nonspecific, and definitive diagnosis typically relies on histopathological analysis of surgically resected samples. Consequently, there may be a risk of underdiagnosis or misdiagnosis, particularly in mild cases that do not require surgical intervention[26].
IMHMV most commonly affects the colorectum, with 91% (77/85) of reported cases involving this region. In contrast, IMHMV of the small intestine is rare, with only seven cases documented in the literature to date. The case described in this study represents the eighth reported instance. The disease predominantly affects previously healthy middle-aged and elderly men, with an age range of 21 to 83 years and a mean onset age of 57.9 years. The male-to-female ratio is approximately 4.3:1. However, small bowel-type IMHMV appears to be more common in female patients, with females accounting for 75% (6/8) of the reported cases.
The clinical presentation of IMHMV lacks specificity and overlaps significantly with that of other common colonic diseases, such as inflammatory bowel disease (IBD) or ischemic colitis (IC), often leading to misdiagnosis or delayed diagnosis[28,29]. There are some differences in the clinical features between small bowel IMHMV and colorectal IMHMV (Table 2). Small bowel IMHMV primarily manifests as abdominal pain (7/8), abdominal distension (3/8), nausea and vomiting (2/8), diarrhea (2/8), constipation (1/8), and weight loss (3/8). Additionally, Bryant J reported a case of small bowel IMHMV in which the patient experienced sudden cardiac death while on propranolol therapy[30]. The main symptoms prior to death were chest pain and seizures. By contrast, colorectal IMHMV is characterized predominantly by abdominal pain (83.1%, 64/77), diarrhea (66.2%, 51/77), and hematochezia (63.6%, 49/77). Other reported symptoms include constipation, alternating diarrhea and constipation, tenesmus, mucus in the stool, fever, weight loss, perianal pain, rectal urgency, and fecal incontinence. The natural history of IMHMV is symptomatic progression, which occasionally leads to complications such as bowel obstruction, perforation, massive hematochezia requiring transfusion, or toxic megacolon[31]. Compared with its colorectal counterpart, small bowel IMHMV appears to be more prone to obstruction (50%, 4/8), likely due to the smaller diameter of the small intestine. Ischemia-induced changes in diameter may contribute to an increased risk of obstruction in small bowel IMHMV[24]. The clinical course of IMHMV is generally chronic. The average time from symptom onset to surgery is 8.4 months for small bowel IMHMV (data from only 5 cases of small bowel IMHMV are available) and 4.4 months for colorectal IMHMV.
| Clinical characteristics | Colonic IMHMV (n = 77) | Small intestinal IMHMV (n = 8) | ||
| Mean age, years (range) | 57 (21-82) | 62 (42-81) | ||
| Sex | ||||
| M | 67 | 2 | ||
| F | 10 | 6 | ||
| Symptoms and signs | Abdominal pain | 64 | Abdominal pain | 7 |
| Diarrhea | 51 | Diarrhea | 2 | |
| Hematochezia | 49 | |||
| Constipation | 8 | Constipation | 1 | |
| Tenesmus | 10 | |||
| Weight loss | 16 | Weight loss | 3 | |
| Fever | 10 | Nausea and vomiting | 2 | |
| Constipation and diarrhea alternated | 8 | Anorexia | 1 | |
| Abdominal distension | 5 | Abdominal distension | 3 | |
| Mucoid stools | 9 | Chest pain | 1 | |
| Rectal urgency | 3 | Seizures | 1 | |
| Fecal incontinence | 2 | Bilateral lower limb edema | 1 | |
| Perianal pain | 2 | |||
| Preoperative clinical impression | IBD | 33 | IBD | 4 |
| IC | 14 | |||
| IBD/IC | 7 | |||
| IMHMV | 9 | Adhesive intestinal obstruction | 1 | |
| Endoscopic findings | Congested, edematous, friable mucosa | 58 | Congested, edematous, friable mucosa | 2 |
| Ulcer | 44 | Ulcer | 3 | |
| Erythema | 34 | |||
| Intestinal stenosis | 19 | Intestinal stenosis | 1 | |
| Pseudopolyps | 5 | |||
| Affected site | Rectum - DC | 24 | Terminal ileum | 5 |
| Rectum - TC | 4 | Ileum | 1 | |
| RS | 26 | Jejunum | 1 | |
| SC | 11 | Jejunum/ileum | 1 | |
| SC - DC | 4 | |||
| DC | 1 | |||
| TC | 1 | |||
| Rectum - terminal ileum | 2 | |||
| TC - terminal ileum | 1 | |||
| Time to surgery (range); follow-up period (range), months | 4.4 (0.25, 24); 28.5 (2, 144) | 8.4 (6, 12); 14.4 (1, 32) | ||
| Indication for surgery | Clinical symptoms continued to worsen and medical treatment was ineffective | 23 | Appendiceal mucocoele and pseudomyxoma peritonei | 1 |
| IMHMV was suspected and surgery was performed to confirm the diagnosis | 7 | CT scan showed bowel ischemia | 1 | |
| Acute abdomen | 3 | |||
| Massive hematochezia and medical treatment was ineffective | 6 | |||
| Bowel obstruction | 2 | Bowel obstruction | 4 | |
| Perforation | 9 | Perforation | 1 | |
The endoscopic manifestations of IMHMV primarily consist of nonspecific ischemic changes in the intestine. Common endoscopic findings include mucosal hyperemia, edema, increased fragility, and a variety of ulcerations (which may appear volcano-like, cobblestone, annular, longitudinal, or patchy, with some cases even exhibiting features reminiscent of pseudomembranous colitis[32]), as well as erythema, luminal stenosis, and pseudopolypoid changes (Table 2). Because these endoscopic features are also frequently observed in patients with IBD and IC and given that the clinical symptoms lack specificity, IMHMV is often misdiagnosed preoperatively. In total, 37 cases have been reported to be misdiagnosed as IBD, 14 as IC, and 7 as IBD/IC.
In the past, endoscopic biopsy has been considered of limited diagnostic value for IMHMV, as conventional biopsy techniques often fail to obtain submucosal and deeper tissues, precluding direct observation of the characteristic concentric intimal hyperplasia of small veins[33]. Most preoperative biopsy reports described only nonspecific ischemic changes[19]. However, as our understanding of the disease has advanced, several studies have suggested the potential for preoperative diagnosis based on endoscopic mucosal biopsy[34]. Research indicates that the ischemic mucosal changes in IMHMV patients may be accompanied by abundant eosinophilic, fibrinous thrombi within vessels, with some cases also showing evidence of endothelial injury[35]. Further analysis revealed highly sensitive and specific pathological features, including microvascular dilation, closely arranged endothelial cells with "arterialization" changes, and subendothelial fibrin deposition[35]. These typical features suggest the possibility of the preoperative diagnosis of IMHMV. Unfortunately, such features were not observed in our biopsy samples. Recently, Kim et al[19] retrospectively analyzed colonoscopic biopsy samples from 7 IMHMV patients and proposed biopsy-based diagnostic criteria as follows: (1) Marked thickening of the capillary walls with fibrinous necrosis; and (2) Arterialization or thickening of the capillary walls accompanied by endothelial cell proliferation[19]. Using these criteria, they successfully preoperatively diagnosed 3 prospective cases between January 2019 and January 2020. It is important to note, however, that not all IMHMV patients exhibit these characteristic features. Importantly, when clinicians encounter difficult-to-treat enteritis cases with endoscopic biopsy showing ischemic changes without any specific findings for IBD, they should maintain a high index of suspicion for IMHMV[36].
IMHMV primarily involves the left colon, particularly the rectum and sigmoid colon. CT and magnetic resonance imaging (MRI) often reveal localized bowel wall thickening in affected regions. Thickening is typically pronounced but lacks the characteristic "target sign", distinguishing it from the bowel wall changes observed in IBD and other conditions[20]. In addition, CT may show increased fat density around the affected bowel segments, suggesting infiltration of the surrounding adipose tissue. Although this finding resembles inflammatory changes, it generally lacks prominent inflammatory signals. In patients with the small bowel subtype of IMHMV, CT findings often indicate ileal wall thickening, luminal narrowing, and proximal small bowel dilation[24,37], consistent with our observations.
Furthermore, venous dilation can occur in the affected regions due to blood flow obstruction caused by intimal proliferation in the mesenteric veins. Angiography may reveal filling defects within the veins or occlusion of the distal inferior mesenteric vein with peripheral venous dilation[20,29,32,38,39]. These findings mimic thrombosis but are essentially a result of abnormal intimal proliferation. Similarly, secondary vascular changes, such as mesenteric vein branch dilation and collateral vessel formation, can be observed in some patients on contrast-enhanced CT/MRI, suggesting chronic vascular disease[29,31]. In rare cases, contrast-enhanced imaging may reveal a cord-like or occluded inferior mesenteric vein[11,40]. Previous studies have also reported imaging findings suggestive of abnormal arteriovenous connections, including rapid venous filling observed on conventional angiography and significant enhancement of dilated mesenteric vein branches during the arterial phase of contrast-enhanced CT[11,12]. Similar to certain characteristic changes observed in endoscopic mucosal biopsies, these imaging features can provide preliminary diagnostic clues, improving the likelihood of a preoperative diagnosis of IMHMV. However, because IMHMV is relatively rare and venous ischemia of the bowel is seldom suspected, these subtle vascular abnormalities are often overlooked or identified only retrospectively during postoperative analysis[3,24].
To date, pathological examination of resected samples remains the only definitive method for confirming the diagnosis of IMHMV[19]. The most notable pathological feature of IMHMV is the abnormal proliferation of the myo-intimal layer of the mesenteric veins. The number of smooth muscle cells in the venous wall increases, leading to thickening of the myo-intimal layer. This proliferation is typically localized, predominantly affecting medium and small mesenteric veins, with the arteries remaining unaffected. Occasionally, the proliferated veins resemble arteries, making differentiation difficult. Elastic fiber staining can distinguish the proliferated veins. Smooth muscle actin staining reveals centripetal proliferation of smooth muscle in the mesenteric venous intima[41]. Due to myogenic proliferation, the lumen of the mesenteric veins becomes significantly narrowed and, in some cases, completely occluded. This venous obstruction leads to impaired venous return from the intestinal wall, causing localized ischemia and congestion without thrombus formation within the veins[42]. Pathological examination typically does not reveal significant inflammatory cell infiltration, which is an important differentiating feature of IMHMV compared with other intestinal diseases with prominent inflammatory responses, such as Crohn’s disease. Moreover, the vessel walls in IMHMV patients usually lack inflammatory cell infiltration, especially lymphocytes, distinguishing this condition from mesenteric inflammatory venous obstructive disease[31]. In tissue sections, in addition to the abnormal proliferation of the myo-intimal layer of the veins, other blood vessels in the affected area (especially arteries) typically do not show abnormal thickening or sclerosis, which is another distinguishing feature of IMHMV compared with other vascular diseases.
Due to impaired venous return, the mucosa and submucosa of the affected intestinal segment also exhibit localized ischemic and congestive changes, such as crypt atrophy, twisting, mucosal hyperplasia, fibrosis, focal ulceration, or submucosal edema with hemorrhage[18,20,42-44]. These pathological findings are typically nonspecific. However, in some cases, experienced pathologists may identify significant features suggestive of IMHMV in the ulcer base, submucosal layer, or even in areas where the mucosa remains intact, including: (1) Significant thickening of the capillary walls or capillary “arterialization”; (2) Focal subendothelial fibrin deposition in small vessels; and (3) Fibrin thrombi in small vessels[43-45].
Surgical intervention remains the most effective treatment for IMHMV. Although there are no specific guidelines, surgery typically involves resecting the affected bowel segment down to the normal mucosa and grossly normal vessels[29]. Common surgical approaches include Hartmann's procedure, segmental colon resection, or total colectomy[23,42]. After bowel resection, the recurrence rate is very low, at just 1% (1 patient). Among the cases reviewed in the literature, only one patient who underwent Hartmann’s procedure for bowel resection experienced recurrence of IMHMV 1 year postsurgery[19]. The authors attributed this recurrence to subclinical disease in the unresected segment rather than true disease recurrence. In the other 38 cases with postoperative follow-up data available, no recurrence of the disease was observed during the follow-up period (mean: 27 months, range: 3-144 months). Notably, our patient underwent three surgeries before a definitive diagnosis was made, and the three affected areas did not appear to be in the same region of the small intestine. No significant venous intimal hyperplasia was observed in the first two surgeries, which may be related to disease progression or insufficient diagnostic experience of the pathologist.
Pharmacological treatments are typically ineffective and may even be potentially harmful for IMHMV patients. Among the 10 patients in our review who underwent emergency surgery due to bowel perforation, 8 were initially treated with corticosteroids on the basis of suspected IBD[9,24,34,44-46]. Timely surgery not only alleviates patient suffering but also prevents progressive ischemia, malnutrition, and the complications inherent in prolonged use of antibiotics or corticosteroids[36]. Recently, several scholars have suggested that IMHMV patients should undergo early assessment for vascular abnormalities with CT angiography while also considering therapeutic embolization as a final intervention to minimize the need for surgical resection[10,11]. However, to date, only one case of an IMHMV patient who underwent endovascular embolization for suspected arteriovenous malformations has been reported[12]. The patient’s symptoms recurred shortly after embolization and returned to pre-embolization levels. She ultimately required surgical treatment. Therefore, whether interventional therapy can serve as an effective early intervention for IMHMV remains to be debated, and further case studies are needed to confirm its role.
IMHMV is an extremely rare vascular disorder of the intestine with an unknown etiology. Owing to overlapping clinical manifestations and endoscopic findings, IMHMV is frequently misdiagnosed as inflammatory or ischemic bowel disease. Advances in biopsy and angiographic techniques may improve the likelihood of preoperative identification; however, histopathological examination of resected samples remains the diagnostic gold standard. Surgical resection remains the definitive treatment, with no recurrence typically observed postoperatively. Nevertheless, further investigations are needed to better understand small intestinal IMHMV. The small intestinal IMHMV case we report here appears to differ in clinical presentation and disease course from previously documented cases, potentially contributing to a deeper understanding of its pathogenesis. This article provides a scoping review of the literature, combined with the latest case reports, to analyze the clinical characteristics of IMHMV and compare the differences between small intestinal and colonic IMHMV. The aim of this work was to enhance the clinical recognition of this rare disease. Importantly, the findings of this study are limited by the quality and completeness of the data in the reported cases.
We thank the Department of Pathology and Department of Radiology of the Second Xiangya Hospital of Central South University for their contributions to the diagnosis of this case.
| 1. | Sahara K, Yamada R, Fujiwara T, Koizumi K, Horiguchi S, Hishima T, Yamaguchi T. Idiopathic myointimal hyperplasia of mesenteric veins: Rare case of ischemic colitis mimicking inflammatory bowel disease. Dig Endosc. 2015;27:767-770. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 2. | Rozner R, Gisriel S, Damianos J, Grimshaw AA, Rizwan R, Nawaz A, Chan K, Wan D, Pantel H, Bhutta AQ, Fenster M, Brandt LJ, Barbieri A, Robert ME, Feuerstadt P, Li DK. Idiopathic myointimal hyperplasia of the mesenteric veins: A systematic review and individual patient data regression analysis. J Gastroenterol Hepatol. 2023;38:1040-1046. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 6] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 3. | Genta RM, Haggitt RC. Idiopathic myointimal hyperplasia of mesenteric veins. Gastroenterology. 1991;101:533-539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 77] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 4. | Abu-Alfa AK, Ayer U, West AB. Mucosal biopsy findings and venous abnormalities in idiopathic myointimal hyperplasia of the mesenteric veins. Am J Surg Pathol. 1996;20:1271-1278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 46] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 5. | Kern WH, Wells WJ, Meyer BW. The pathology of surgically excised aortocoronary saphenous vein bypass grafts. Am J Surg Pathol. 1981;5:491-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 28] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Stracke S, Konner K, Köstlin I, Friedl R, Jehle PM, Hombach V, Keller F, Waltenberger J. Increased expression of TGF-beta1 and IGF-I in inflammatory stenotic lesions of hemodialysis fistulas. Kidney Int. 2002;61:1011-1019. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 99] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 7. | Li H, Shu H, Zhang H, Cui M, Gao Y, Tian F. Idiopathic Myointimal Hyperplasia of the Mesenteric Veins: A Case Report and Scoping Review of Previously Reported Cases From Clinical Features to Treatment. Front Med (Lausanne). 2022;9:855335. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 8. | Sherman J, Kao PC, Brian West A, Blaszyk H. Focal myointimal hyperplasia of mesenteric veins is associated with previous trauma in surgical specimens. Pathol Res Pract. 2006;202:517-522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Kao PC, Vecchio JA, Hyman NH, West AB, Blaszyk H. Idiopathic myointimal hyperplasia of mesenteric veins: a rare mimic of idiopathic inflammatory bowel disease. J Clin Gastroenterol. 2005;39:704-708. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 38] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 10. | Huynh D, Hendy P, Mortimore M. Idiopathic myointimal hyperplasia of the mesenteric veins could be related to mesenteric arteriovenous malformation. J Gastroenterol Hepatol. 2024;39:2239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 11. | Morimura F, Edo H, Niwa T, Sugiura H, Suyama Y, Okazaki S, Narimatsu K, Ohno H, Okamoto K, Ueno H, Yoshimatsu S, Miyai K, Hamamoto K, Shinmoto H. Idiopathic myointimal hyperplasia of mesenteric veins: radiological evaluation using CT angiography. BJR Case Rep. 2024;10:uaad009. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 12. | Shah YB, Lee D, Khaddash TS. Endovascular approach in the management of idiopathic myointimal hyperplasia of the inferior mesenteric vein. CVIR Endovasc. 2021;4:88. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 13. | Nakaya M, Hashimoto H, Nagata R, Usui G, Kusakabe M, Harihara Y, Horiuchi H, Yao T, Morikawa T. Enterocolic lymphocytic phlebitis with marked myointimal hyperplasia and perivenous concentric fibrosis. Cardiovasc Pathol. 2019;40:68-71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 14. | Bao P, Welch DC, Washington MK, Herline AJ. Resection of mesenteric inflammatory veno-occlusive disease causing ischemic colitis. J Gastrointest Surg. 2005;9:812-817. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 15. | Ngo N, Chang F. Enterocolic lymphocytic phlebitis: clinicopathologic features and review of the literature. Arch Pathol Lab Med. 2007;131:1130-1134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 34] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 16. | Bowee S, Matter SB, Dawson H, Inglin RA. Enterocolic phlebitis: a rare cause of bowel ischemia and review of the literature. Gastroenterol Rep (Oxf). 2023;11:goad002. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 17. | Kawasaki K, Kawatoko S, Torisu T, Mizuuchi Y, Iura T, Ohtani H, Okamura K, Yamamoto H, Nakamura M, Kitazono T. Idiopathic myointimal hyperplasia of mesenteric veins depicted by barium enema examination, and conventional and magnifying colonoscopy. Clin J Gastroenterol. 2022;15:734-739. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 18. | Al Ansari A, Ahmed S, Mansour E, Abass MA. Idiopathic myointimal hyperplasia of the mesenteric veins. J Surg Case Rep. 2021;2021:rjaa453. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 19. | Kim SW, Ho Park S, Hyoung Park S, Sik Yoon Y, Kim J. Idiopathic Myointimal Hyperplasia of the Mesenteric Veins Is a Peculiar Venous Ischemia That May Be Diagnosed Before Surgery. Dis Colon Rectum. 2022;65:e707-e717. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 20. | Yun SJ, Nam DH, Kim J, Ryu JK, Lee SH. The radiologic diagnosis of idiopathic myointimal hyperplasia of mesenteric veins with a novel presentation: case report and literature review. Clin Imaging. 2016;40:870-874. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 21. | Wong R, Westerveld D, Yeo H, Jessurun J, Jesudian A. Ischemic Colitis From Idiopathic Myointimal Hyperplasia of the Mesenteric Veins in a Post-Liver Transplant Patient. ACG Case Rep J. 2021;8:e00692. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 22. | Yang KH, Kwon TH, Park KS, Kim ES, Cho KB, Baek SK, Hwang I. [Idiopathic Myointimal Hyperplasia of Mesenteric Veins]. Korean J Gastroenterol. 2016;67:54-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 23. | Coombs RA, Martin SA, Garg SK. An Unusual Case of Rectal Bleeding and Abdominal Pain in a Young Man. Gastroenterology. 2024;166:e16-e18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 24. | Yamada K, Hiraki M, Tanaka T, Mori D, Tanaka F, Manabe T, Aibe H, Kitahara K, Noshiro H. A case of idiopathic myointimal hyperplasia of the mesenteric veins presenting with small bowel obstruction. Surg Case Rep. 2021;7:17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 25. | Laskaratos FM, Hamilton M, Novelli M, Shepherd N, Jones G, Lawrence C, Mitchison M, Murray CD. A rare cause of abdominal pain, diarrhoea and GI bleeding. Idiopathic myointimal hyperplasia of the mesenteric veins (IMHMV). Gut. 2015;64:214, 350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 26. | Song SJ, Shroff SG. Idiopathic Myointimal Hyperplasia of Mesenteric Veins of the Ileum and Colon in a Patient with Crohn's Disease: A Case Report and Brief Review of the Literature. Case Rep Pathol. 2017;2017:6793031. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 27. | Louie CY, DiMaio MA, Charville GW, Berry GJ, Longacre TA. Gastrointestinal Tract Vasculopathy: Clinicopathology and Description of a Possible "New Entity" With Protean Features. Am J Surg Pathol. 2018;42:866-876. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 28. | Wangensteen KJ, Fogt F, Kann BR, Osterman MT. Idiopathic Myointimal Hyperplasia of the Mesenteric Veins Diagnosed Preoperatively. J Clin Gastroenterol. 2015;49:491-494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 23] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 29. | Bhatt H, Moreira RK, Shawki SF, Rumer KK. Atypical presentation of a rare disorder; idiopathic myointimal hyperplasia of mesenteric veins (IMHMV): Report of two cases. Int J Surg Case Rep. 2023;111:108839. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 30. | Bryant J. Unexpected sudden death during propranolol therapy in a patient with mild mesenteric venous myointimal hyperplasia. J Forensic Sci. 1998;43:905-907. [PubMed] |
| 31. | Han GR, Mehrotra AP, Gomez AJ, Romanucci E, Halpern VJ. Capturing the often-elusive diagnosis of idiopathic myointimal hyperplasia of mesenteric veins. J Vasc Surg Cases Innov Tech. 2022;8:520-533. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 32. | García-Castellanos R, López R, de Vega VM, Ojanguren I, Piñol M, Boix J, Domènech E, Cabré E. Idiopathic myointimal hyperplasia of mesenteric veins and pneumatosis intestinalis: a previously unreported association. J Crohns Colitis. 2011;5:239-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 33. | Costa MN, Saiote J, Pinheiro MJ, Duarte P, Bentes T, Ferraz Oliveira M, Ramos J. Segmental colitis caused by idiopathic myointimal hyperplasia of mesenteric veins. Rev Esp Enferm Dig. 2016;108:821-826. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 34. | Anderson B, Smyrk TC, Graham RP, Lightner A, Sweetser S. Idiopathic myointimal hyperplasia is a distinct cause of chronic colon ischaemia. Colorectal Dis. 2019;21:1073-1078. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 35. | Yantiss RK, Cui I, Panarelli NC, Jessurun J. Idiopathic Myointimal Hyperplasia of Mesenteric Veins: An Uncommon Cause of Ischemic Colitis With Distinct Mucosal Features. Am J Surg Pathol. 2017;41:1657-1665. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 36. | Uwah M, Bustamante-Lopez L, Devane L, Hoff J, Garcia-Henriquez N, Kline B, Monson JRT, Albert M. Idiopathic myointimal hyperplasia of the mesenteric veins-a report of two cases. AME Case Rep. 2024;8:84. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 37. | Lanitis S, Kontovounisios C, Karaliotas C. An extremely rare small bowel lesion associated with refractory ascites. Idiopathic myointimal hyperplasia of mesenteric veins of the small bowel associated with appendiceal mucocoele and pseudomyxoma peritonei. Gastroenterology. 2012;142:e5-e7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 38. | Kelly Wu W, Tombazzi CR, Howe CF, Kendall MA, Walton DB, Washington MK, Ford MM, Hopkins MB, Geiger TM, Hawkins AT, Muldoon RL. Idiopathic Myointimal Hyperplasia of the Mesenteric Veins: A Rare Imitator of Inflammatory Bowel Disease. Am Surg. 2023;89:1141-1143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 39. | Chiang CK, Lee CL, Huang CS, Huang SH, Wu CH. A rare cause of ischemic proctosigmoiditis: idiopathic myointimal hyperplasia of mesenteric veins. Endoscopy. 2012;44 Suppl 2 UCTN:E54-E55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 40. | AbiMansour J, Khanna S, Sweetser S. An Important Mimicker. Gastroenterology. 2022;162:1840-1843. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 41. | Korenblit J, Burkart A, Frankel R, Klinge M, Greenbau L, Goldstein S, Kastenberg D. Refractory pancolitis: a novel presentation of idiopathic myointimal hyperplasia of mesenteric veins. Gastroenterol Hepatol (N Y). 2012;8:696-700. [PubMed] |
| 42. | Lincango EP, Cheong JY, Prien C, Connelly TM, Hernandez Dominguez O, Tursun N, Liska D, Lipman J, Lightner A, Kessler H, Valente MA, Hull T, Steele SR, Holubar SD. Idiopathic myointimal hyperplasia of the mesenteric veins: A systematic review of surgical management. Surgery. 2023;174:473-479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 3] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 43. | Martin FC, Yang LS, Fehily SR, D'Souza B, Lim A, McKelvie PA. Idiopathic myointimal hyperplasia of the mesenteric veins: Case report and review of the literature. JGH Open. 2020;4:345-350. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 44. | Zhou L, Tian F, Zhang H, Shu H, Gao Y, Cui M, Xie Y. Idiopathic Myointimal Hyperplasia of the Mesenteric Veins: A Case Report. Inflamm Bowel Dis. 2022;28:e131-e133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 45. | Mohtashami A, Badiani S, Chui JN, De Silva K, Salama Y. Idiopathic myointimal hyperplasia of the mesenteric veins: a rare and poorly understood disease. ANZ J Surg. 2024;94:478-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 46. | Almumtin A, Al Sulais E, Elhag MA. Idiopathic Myointimal Hyperplasia of Mesenteric Veins (IMHMV) with two spontaneous bowel perforations: A case report and literature review. Int J Surg Case Rep. 2021;83:106022. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 47. | Guadagno E, Del Basso De Caro M, Del Prete E, D'Armiento FP, Campione S. Coexistence of Multiple Ileal Neuroendocrine Tumors and Idiopathic Myointimal Hyperplasia of Mesenteric Veins: Coincidence or Consequence? Case Report and Review of Literature. Int J Surg Pathol. 2016;24:627-630. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 48. | Chudy-Onwugaje K, Ali O, Umoren M. Idiopathic Myointimal Hyperplasia of the Mesenteric Veins of the Colon. Clin Gastroenterol Hepatol. 2020;18:A19-A20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 49. | Noujaim MG, Tang H, Kalisz K, Iranzad N, Wild D. Ischemic Colitis Due to Idiopathic Myointimal Hyperplasia of the Mesenteric Veins. ACG Case Rep J. 2023;10:e01125. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 50. | Dillione MR, Abrahamsen I, Ho D, Pak K, Fiore B, Sadowski B, Liu S, Foley S, Hogan P, Brandau J, Liebig J, Vicente D, Edson T, Bachmann A. Idiopathic Myointimal Hyperplasia of the Mesenteric Veins: A Rare Disorder Leading to Ischemic Proctitis. Am J Gastroenterol. 2024;119:610. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 51. | Patel AD, Schneider Y, Saumoy M, Maltz C, Yeo H, Jessurun J, Wan D. Idiopathic Myointimal Hyperplasia of the Mesenteric Veins. ACG Case Rep J. 2016;3:e84. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 52. | Xie H, Xu X. Radiological and clinical findings of idiopathic myointimal hyperplasia of mesenteric veins: Case report. Medicine (Baltimore). 2021;100:e27574. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 53. | Cauchois A, Desfourneaux V, Kammerer-Jacquet SF, Bouguen G, Rioux-Leclercq N, Henno S. [A case of idiopathic myointimal hyperplasia of mesenteric veins]. Ann Pathol. 2016;36:415-419. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 54. | Gonai T, Toya Y, Nakamura S, Kawasaki K, Yanai S, Fujita Y, Uesugi N, Kimura T, Otsuka K, Sugai T, Matsumoto T. Gastrointestinal: Idiopathic myointimal hyperplasia of mesenteric veins. J Gastroenterol Hepatol. 2018;33:1939. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 55. | Feo L, Cheeyandira A, Schaffzin DM. Idiopathic myointimal hyperplasia of mesenteric veins in the elderly. Int J Colorectal Dis. 2013;28:433-434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 56. | Abbott S, Hewett P, Cooper J, Ruszkiewicz A. Idiopathic myointimal hyperplasia of the mesenteric veins: a rare differential to be considered in idiopathic colitis. ANZ J Surg. 2018;88:242-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 57. | Savoie LM, Abrams AV. Refractory proctosigmoiditis caused by myointimal hyperplasia of mesenteric veins: report of a case. Dis Colon Rectum. 1999;42:1093-1096. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 58. | López Morales P, González Valverde FM, Giménez Francés C, Pastor Quirante F, Albarracín Marín-Blázquez A. Idiopathic myointimal hyperplasia of the mesenteric veins, an uncommon cause of intestinal ischemia. Rev Esp Enferm Dig. 2022;114:368-369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |