Copyright
©2011 Baishideng Publishing Group Co.
World J Gastroenterol. Sep 28, 2011; 17(36): 4076-4089
Published online Sep 28, 2011. doi: 10.3748/wjg.v17.i36.4076
Published online Sep 28, 2011. doi: 10.3748/wjg.v17.i36.4076
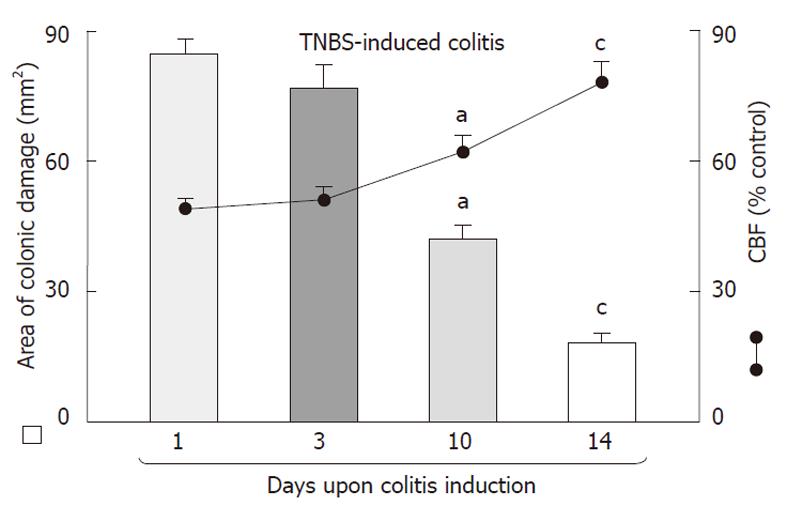
Figure 1 Time-sequence of the healing of trinitrobenzenesulfonic acid-induced colonic lesions, and accompanying changes in the colonic blood flow following day 1, 3, 10 and 14 upon induction of colitis.
The area of trinitrobenzenesulfonic acid-induced lesions was maximal on day 1 and then it significantly declined on day 10 and day 14, respectively. Mean ± SE of 6-8 rats. aP < 0.05 vs values obtained on day 3; cP < 0.05 vs values on day 3 and day 10. TNBS: Trinitrobenzenesulfonic acid; CBF: Colonic blood flow.
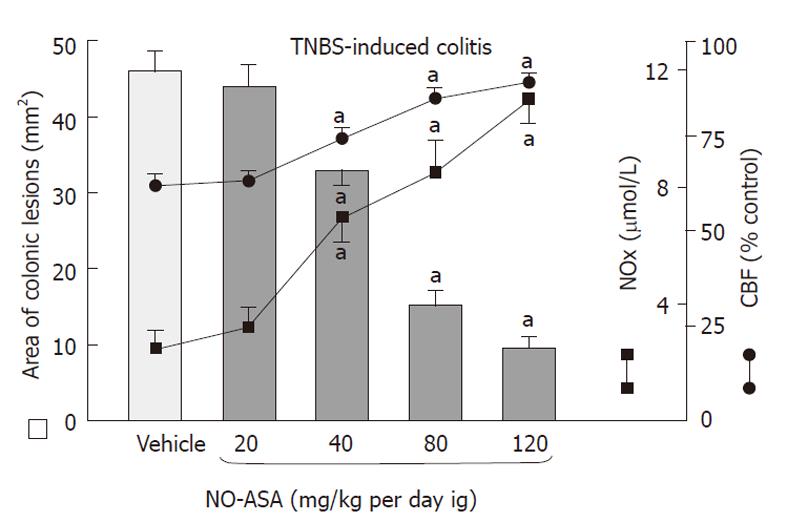
Figure 2 The effect of 10 d administration of nitric oxide-aspirin, applied ig in gradual concentrations ranging from 20 mg/kg up to 120 mg/kg on the area of colonic lesions, alterations in colonic blood flow and plasma NOx concentrations in rats with trinitrobenzenesulfonic acid-induced colitis on day 10.
Mean ± SE of 6-8 rats. aP < 0.05 vs vehicle (control) and animals treated with a dose of 20 mg/kg nitric oxide-aspirin (NO-ASA). TNBS: Trinitrobenzenesulfonic acid; CBF: Colonic blood flow.
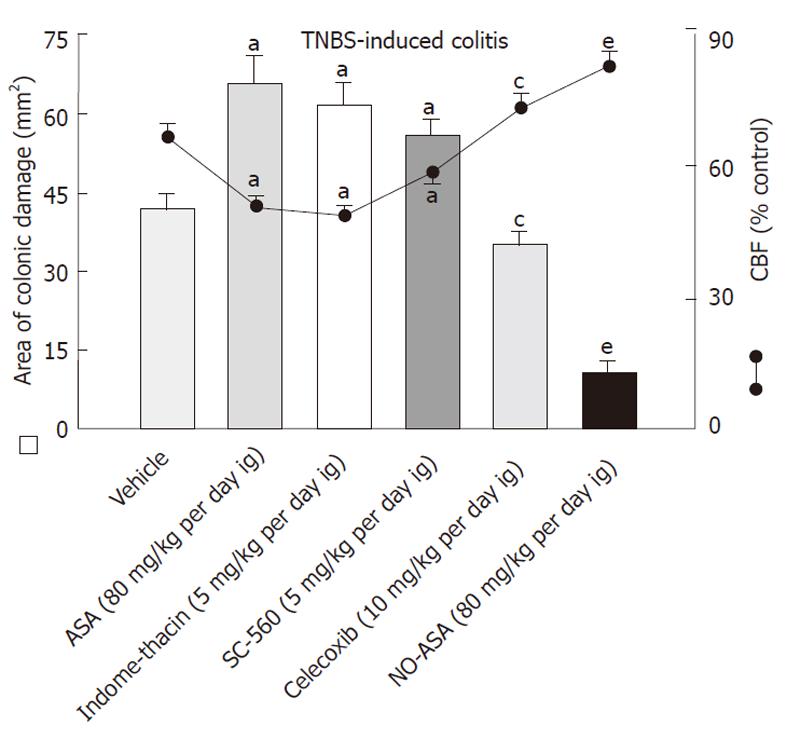
Figure 3 Effect of administration of vehicle, aspirin or indomethacin, non-selective cyclooxygenase inhibitors, a selective cyclooxygenase-1 inhibitor 5-(4-chlorophenyl)-1-(4-methoxyphenyl)-3-(trifluoromethyl)-1H-pyrazole, a selective cyclooxygenase-2 inhibitor (celecoxib) and nitric oxide releasing aspirin, on the area of colonic lesions and alterations in colonic blood flow on day 10 after colitis induction.
Mean ± SE of 6-8 rats. aP < 0.02 vs vehicle (control); cP < 0.05 vs aspirin (ASA)-, indomethacin- and 5-(4-chlorophenyl)-1-(4-methoxyphenyl)-3-(trifluoromethyl)-1H-pyrazole (SC-560) groups; eP < 0.02 vs vehicle, ASA, indomethacin, SC-560 and celecoxib groups. TNBS: Trinitrobenzenesulfonic acid; CBF: Colonic blood flow; NO-ASA: Nitric oxide-ASA.
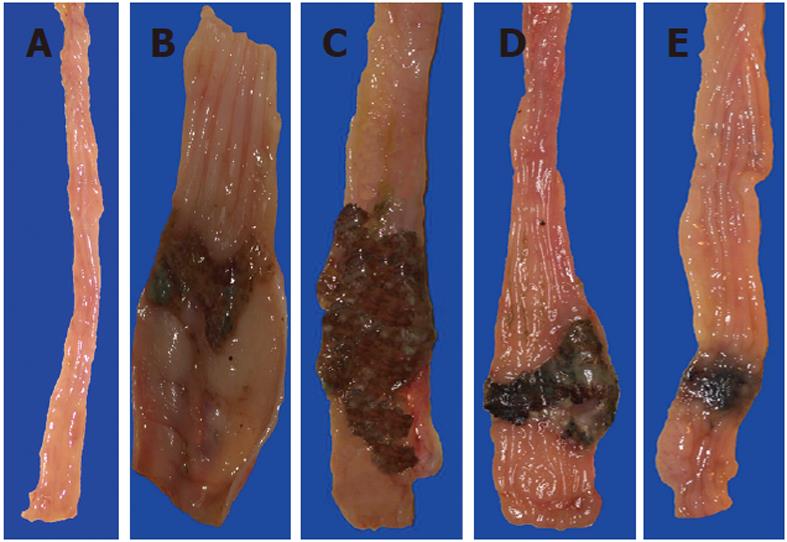
Figure 4 Gross appearance of the intact colon (A), and that of trinitrobenzenesulfonic acid-induced colitis rats treated with vehicle (B), aspirin (C), celecoxib (D) and nitric oxide-aspirin (E) at day 10 of colitis induction.
In aspirin-treated rats (C) the area of colonic damage was larger than in the control trinitrobenzenesulfonic acid rats, which were treated with vehicle (B). In the celecoxib group (D), the area of colonic damage was significantly smaller when compared to the aspirin (ASA) and vehicle groups. The healing of colonic lesions was significantly improved in nitric oxide-ASA treated rats as documented by the small ulceration area and scar formation.
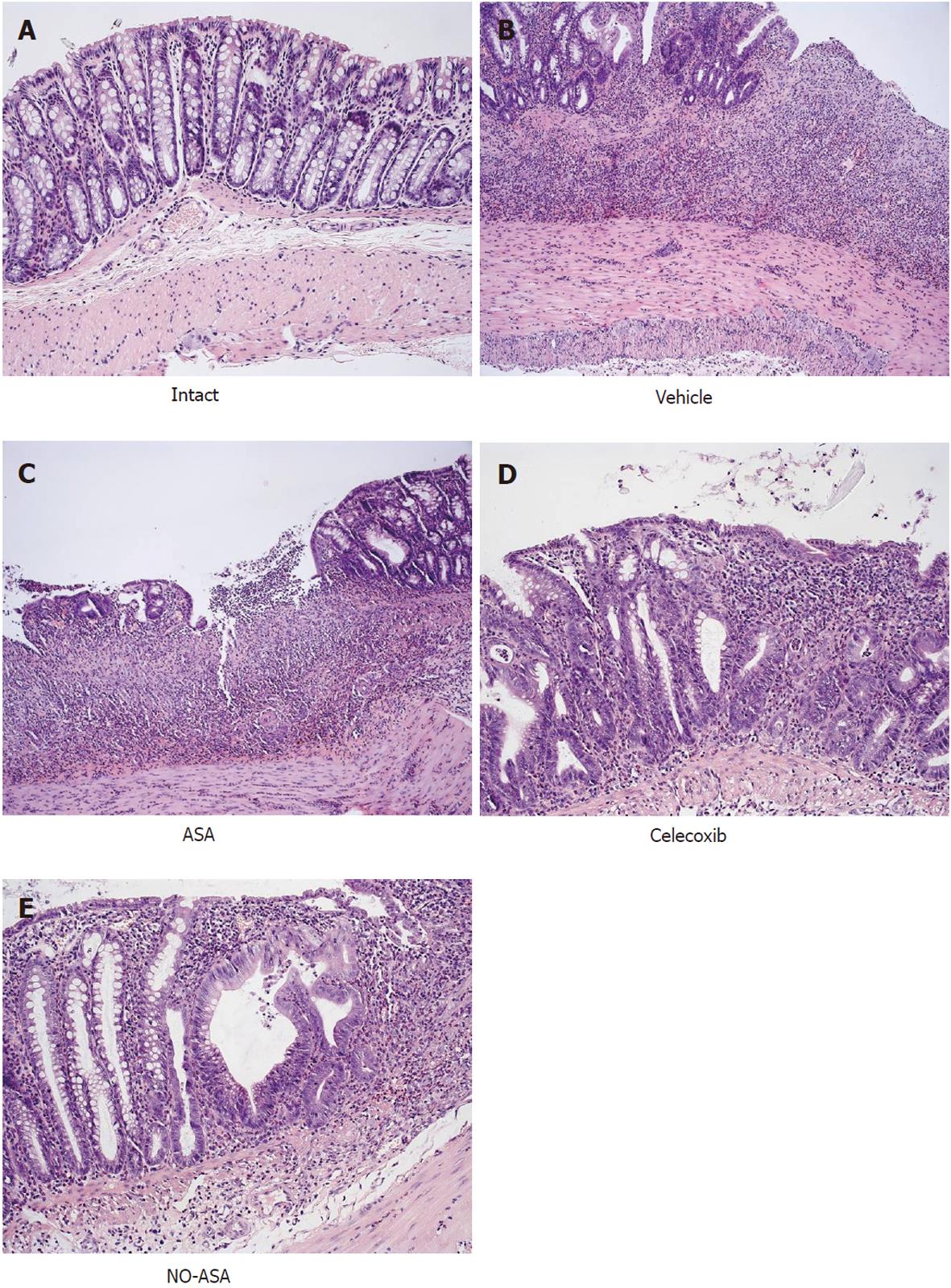
Figure 5 Histological appearance of the intact colonic mucosa (A) and that treated with vehicle (B), aspirin (C), celecoxib (D) and nitric oxide releasing aspirin on day 10 in rats with trinitrobenzenesulfonic acid-induced colitis.
Intact rat colon shows regular colonic architecture and normal colonic mucosa continuity with no signs of inflammation (A). In trinitrobenzenesulfonic acid rats treated with vehicle, deep ulceration and an intense neutrophil infiltration with the presence of numerous neutrophils penetrating the muscularis mucosa and submucosa were observed. The features of regeneration adjacent to the ulcer margin are clearly visible. In aspirin (ASA)-treated rats with colitis (C), there is deep ulceration with necrosis and an intense inflammation followed by severe neutrophil infiltration and the formation of granulation tissue penetrating the muscle layer of the muscularis propria. Less regeneration is observed with ASA (C) than vehicle (control) animals (B). The partially healed epithelium and abnormal crypt architecture with much more pronounced regeneration was observed in the colonic mucosa of rats with colitis treated with celecoxib (D) as compared with other cyclooxygenase inhibitors. In nitric oxide (NO)-ASA treated rats with colitis (E), the most advanced healing process of colonic ulcers as reflected by scar formation, epithelial regeneration and significantly smaller neutrophil infiltration was observed. Part of the colonic crypts distant to the scar already shows a normal appearance.
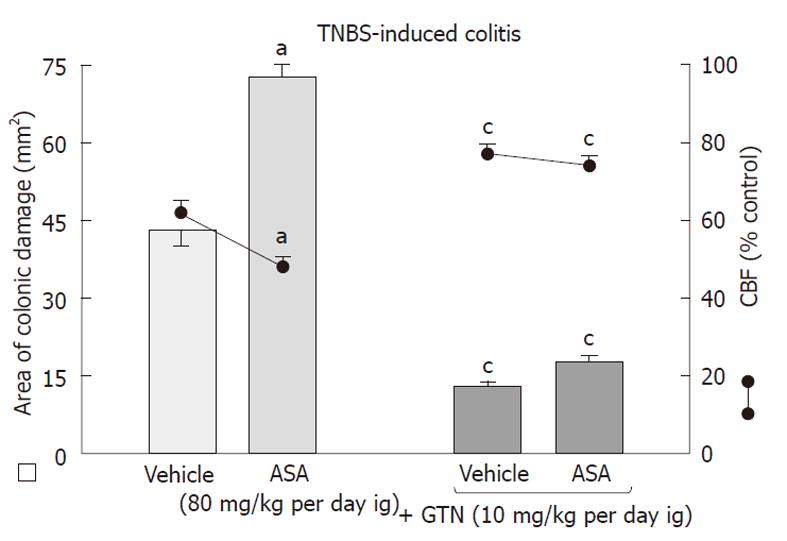
Figure 6 The effect of concurrent administration of nitric oxide donor glyceryl trinitrate on the area of colonic damage and alterations in colonic blood flow in rats with trinitrobenzenesulfonic acid-induced colitis, treated with vehicle or aspirin, on day 10.
Mean ± SE of 6-8 rats. aP < 0.02 vs vehicle (control); cP < 0.02 vs vehicle or aspirin alone. TNBS: Trinitrobenzenesulfonic acid; ASA: Aspirin; GTN: Glyceryl trinitrate; CBF: Colonic blood flow.
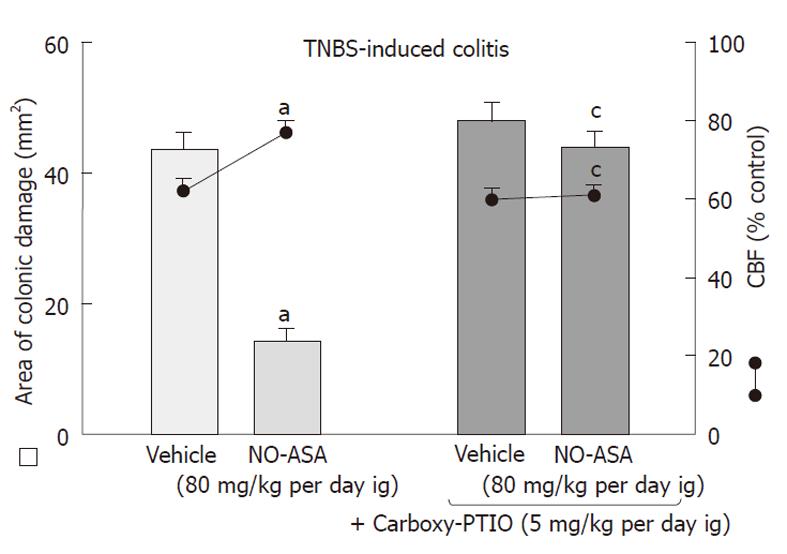
Figure 7 The effect of concurrent administration of nitric oxide scavenger 2-(4-carboxyphenyl)-4,5-dihydro-4,4,5,5-tetramethyl-1H-imidazolyl-1-oxy-3-oxide, monopotassium salt on the area of colonic damage and alterations in colonic blood flow in rats with trinitrobenzenesulfonic acid-induced colitis, treated with vehicle or nitric oxide-aspirin (80 mg/kg per day ig) on day 10.
Mean ± SE of 6-8 rats. aP < 0.05 vs vehicle group (control); cP < 0.05 vs vehicle or nitric oxide-aspirin (NO-ASA) without 2-(4-carboxyphenyl)-4,5-dihydro-4,4,5,5-tetramethyl-1H-imidazolyl-1-oxy-3-oxide, monopotassium salt. TNBS: Trinitrobenzenesulfonic acid; CBF: Colonic blood flow.
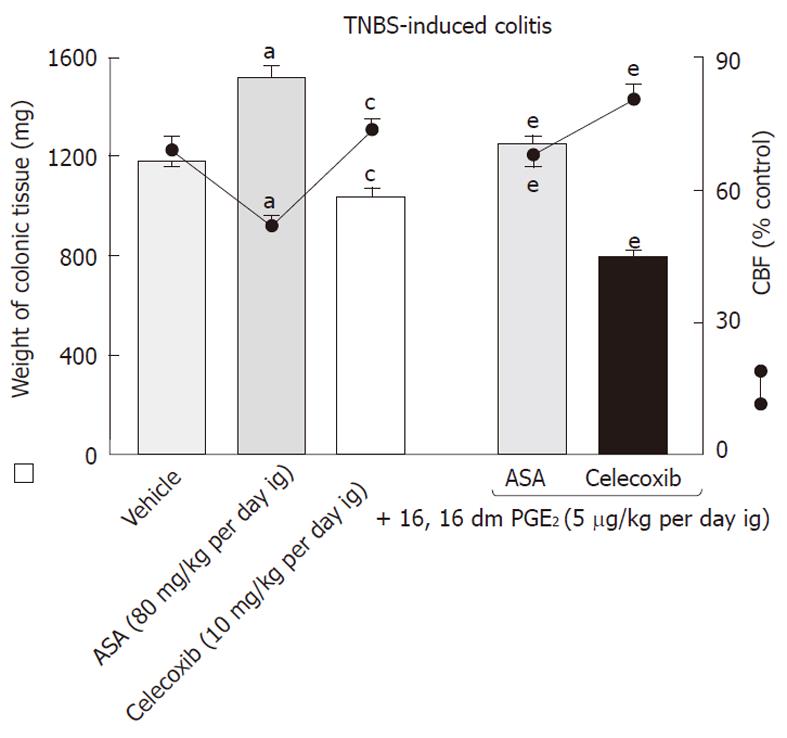
Figure 8 The weight of colonic tissue and alterations in colonic blood flow on day 10 after induction of trinitrobenzenesulfonic acid colitis in rats treated with aspirin or celecoxib with or without 16, 16 dm prostaglandin E2 (5 μg/kg per day ig).
Mean ± SE of 6-8 rats. aP < 0.02 vs vehicle (control); cP < 0.05 vs vehicle (control) and aspirin (ASA) groups; eP < 0.05 vs ASA and celecoxib groups without concurrent prostaglandin E2 (PGE2) administration. TNBS: Trinitrobenzenesulfonic acid; CBF: Colonic blood flow.
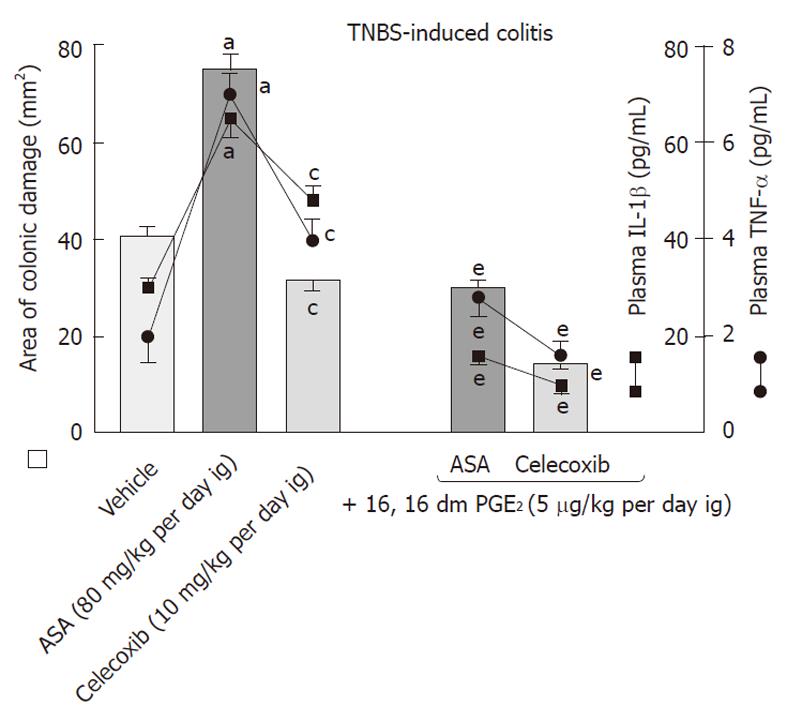
Figure 9 The area of colonic lesions and plasma levels of proinflammatory cytokines IL-1β and tumor necrosis factor-α on day 10 after induction of colitis in rats treated with aspirin or celecoxib with or without 16, 16 dm prostaglandin E2 (5 μg/kg per day ig).
Mean ± SE of 6-8 rats. aP < 0.02 vs vehicle (control); cP <0.02 vs vehicle-treated and aspirin (ASA)-treated groups; eP < 0.02 vs ASA and celecoxib groups without concurrent prostaglandin E2 (PGE2) administration. TNBS: Trinitrobenzenesulfonic acid; TNF: Tumor necrosis factor.
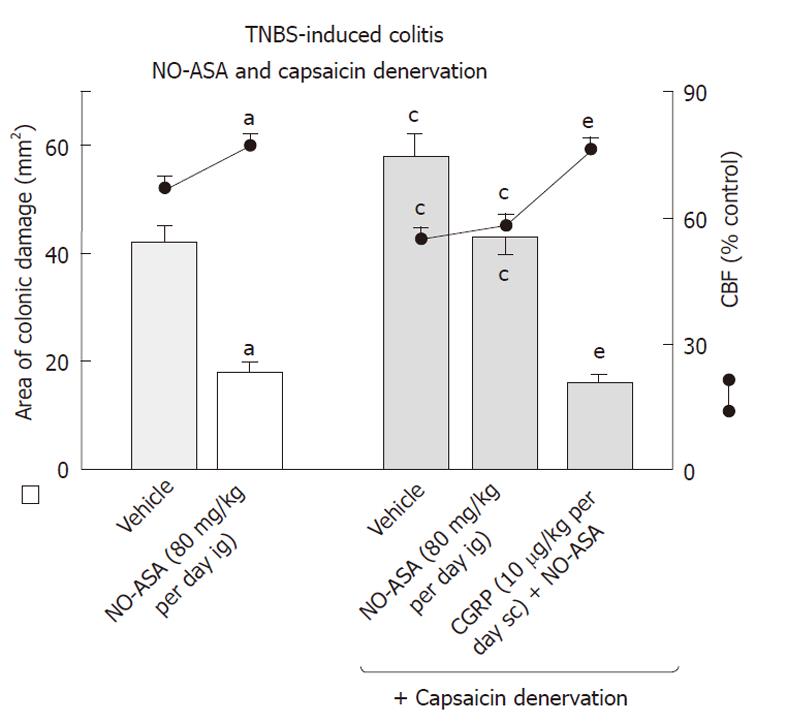
Figure 10 The area of colonic damage and changes in colonic blood flow on day 10 after colitis induction in rats with intact sensory nerves and in those with capsaicin-sensory denervation treated with vehicle (saline) or nitric oxide-aspirin (80 mg/kg per day ig) with or without administration of calcitonin gene related peptide (10 μg/kg per day sc).
Mean ± SE of 6-8 rats. aP < 0.05 vs vehicle (control); cP < 0.05 vs trinitrobenzenesulfonic acid (TNBS) rats without capsaicin denervation; eP < 0.02 vs rats with TNBS colitis treated with nitric oxide-aspirin (NO-ASA). CGRP: Calcitonin gene related peptide; CBF: Colonic blood flow.
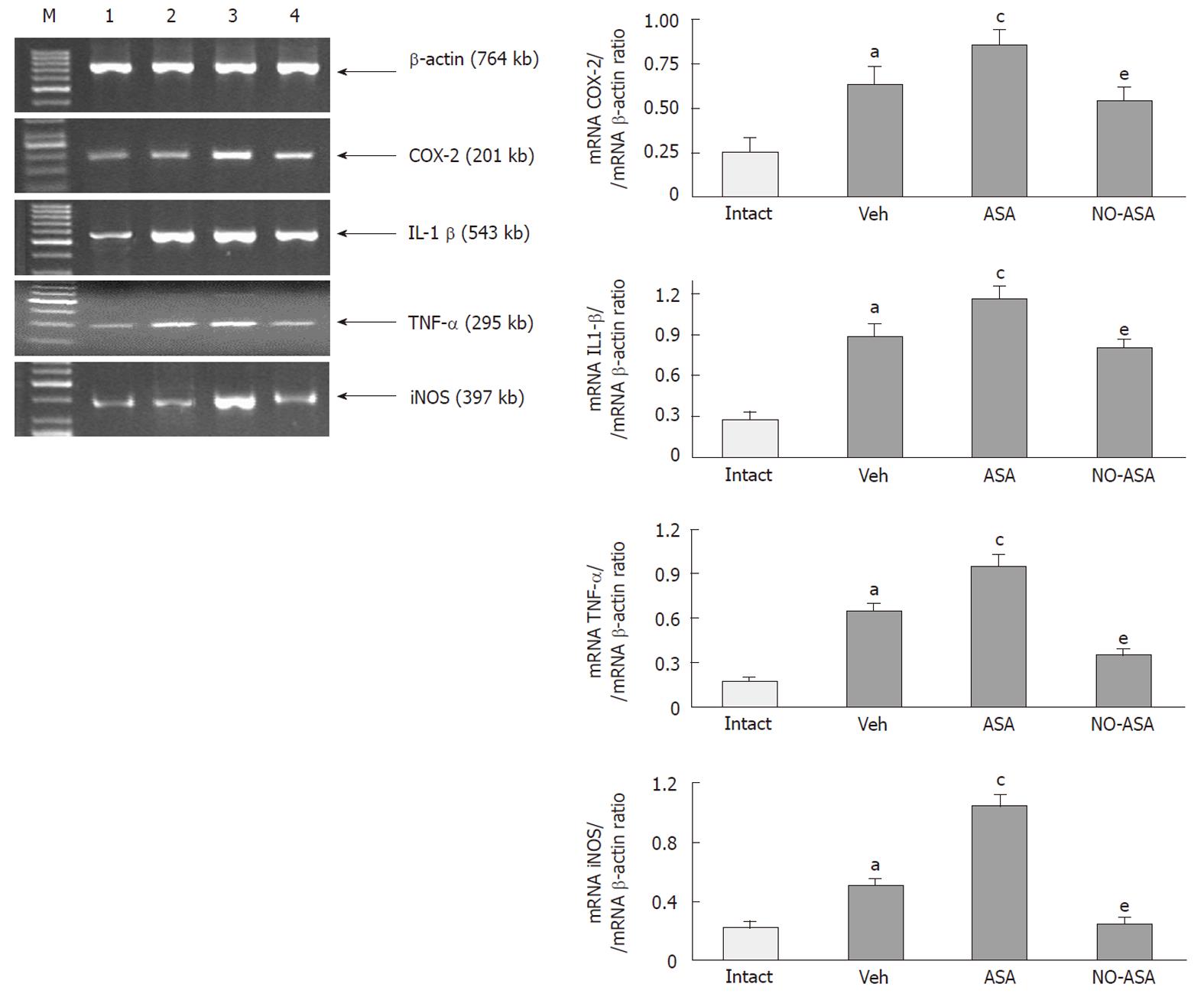
Figure 11 The expression of mRNA for cyclooxygenase-2, IL-1β, tumor necrosis factor-α and inducible form of nitric oxide synthase in colonic mucosa of intact rats (lane 1) those treated with vehicle (lane 2), aspirin (lane 3) and nitric oxide-aspirin (lane 4) at day 10 after induction of colitis.
Mean ± SE of 4 determinations in 4 rats. aP < 0.05 vs intact colonic mucosa; cP < 0.05 vs rats with trinitrobenzenesulfonic acid colitis administered with vehicle (Veh); eP < 0.05 vs vehicle and aspirin (ASA) groups. COX: Cyclooxygenase; TNF: Tumor necrosis factor; iNOS: Inducible form of nitric oxide synthase; M: Marker.
- Citation: Zwolinska-Wcislo M, Brzozowski T, Ptak-Belowska A, Targosz A, Urbanczyk K, Kwiecien S, Sliwowski Z. Nitric oxide-releasing aspirin but not conventional aspirin improves healing of experimental colitis. World J Gastroenterol 2011; 17(36): 4076-4089
- URL: https://www.wjgnet.com/1007-9327/full/v17/i36/4076.htm
- DOI: https://dx.doi.org/10.3748/wjg.v17.i36.4076