Published online Feb 26, 2021. doi: 10.12998/wjcc.v9.i6.1461
Peer-review started: October 31, 2020
First decision: December 8, 2020
Revised: December 21, 2020
Accepted: December 30, 2020
Article in press: December 30, 2020
Published online: February 26, 2021
Processing time: 97 Days and 17.9 Hours
In general, atlantoaxial dislocation is rare due to the stability of the C1-C2 complex. Traumatic atlantoaxial dislocations are usually anterior and accompanied by odontoid fractures. Posterior atlantoaxial dislocations are rare, and complete posterior dislocation without associated fracture is even more rare. A case of early recurrence of posterior atlantoaxial dislocation without fracture being in therapy of first closed reduction and then open reduction has not been previously reported.
A 45-year-old female presented with traumatic posterior atlantoaxial dislocation (TPAD) of C1-C2 without associated fractures, and Frankel Grade B spinal cord function. She was successfully managed by immediate closed reduction under skull traction. Unexpectedly, 17 d later, re-dislocation was discovered. On day 28, closed reduction was performed as before but failed. Then, open reduction and posterior internal fixation with autologous iliac bone grafts was performed. By 6 mo after surgery, atlantoaxial joint fusion was achieved, and neurological function had recovered to Frankel Grade E. At 12 mo follow-up, she had lost only 15° of cervical rotation, and atlantoaxial complex instability in joint flexing and extending were no longer observed under fluoroscopy.
Early assessment of transverse ligament is critical for TPAD without fracture avoiding re-dislocation after closed reduction.
Core Tip: Traumatic posterior atlantoaxial dislocations (TPADs) without fracture are rare. In this article, we present a 45-year-old female with early recurrence of TPAD of C1-C2 without associated fractures. The patient first underwent closed reduction and then open reduction, internal fixation, and interfacial fusion. Excellent results were achieved. In conclusion, early assessment of the condition of the transverse ligament is critical for the prevention and early discovery of the re-dislocation of TPADs.
- Citation: Sun YH, Wang L, Ren JT, Wang SX, Jiao ZD, Fang J. Early reoccurrence of traumatic posterior atlantoaxial dislocation without fracture: A case report. World J Clin Cases 2021; 9(6): 1461-1468
- URL: https://www.wjgnet.com/2307-8960/full/v9/i6/1461.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i6.1461
Atlantoaxial dislocations are classified as anteroposterior, rotatory, central, or mixed dislocations, based on the direction and plane of dislocation[1]. Traumatic atlantoaxial dislocations usually are anterior and accompanied by odontoid fractures[2-5]. Posterior atlantoaxial dislocations are rare, and complete posterior dislocation without fracture is rarer still[6-17]. Here, we present the first reported case of early recurrence of posterior atlantoaxial dislocation without fracture and the necessary treatments.
A 45-year-old female was admitted to our hospital with light coma and difficulty breathing 3 h after being struck in an automobile accident.
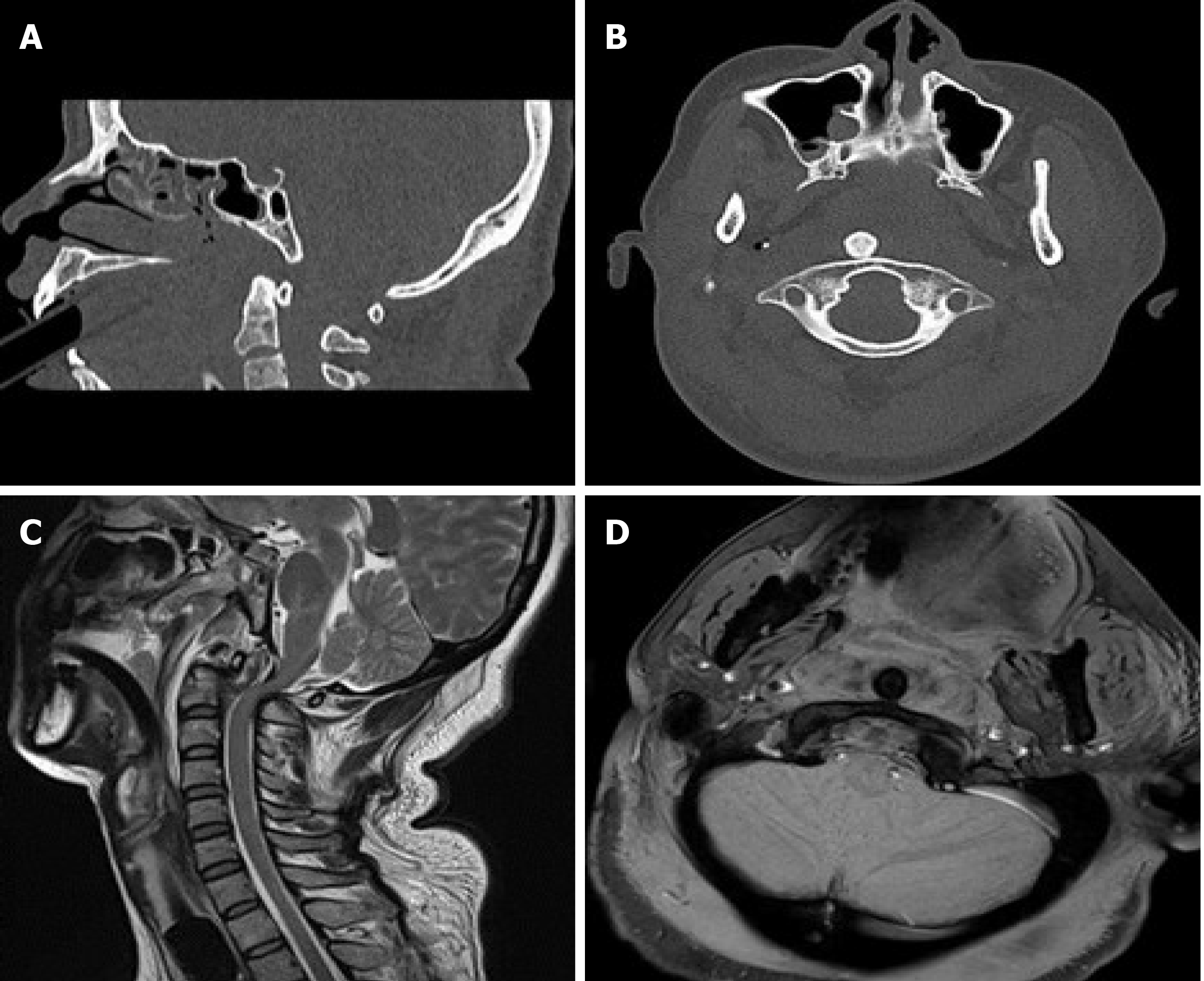
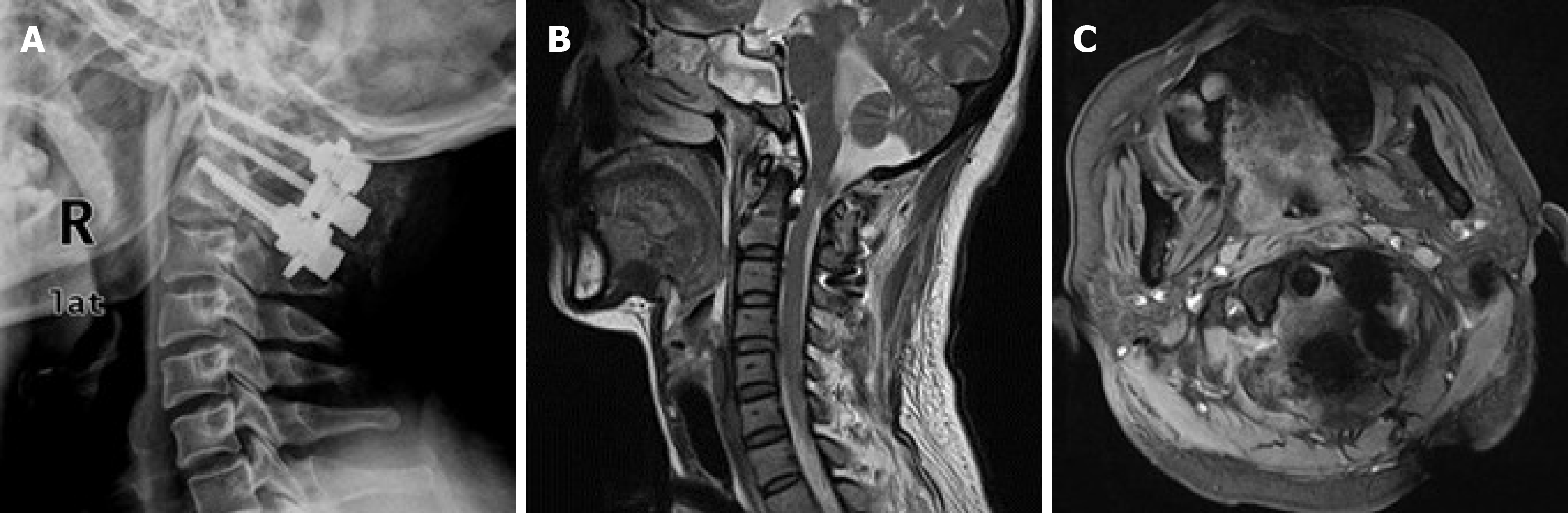
The patient, who was struck in the back by an automobile, was transferred from a local county clinic to our hospital 3 h after the accident. She presented with light coma, difficulty breathing, lacerations on the face and scalp and stiffness in the neck. Emergency intubation was performed, followed by computed tomography (CT) and magnetic resonance imaging (MRI) examinations. CT scans revealed posterior atlantoaxial dislocation (Figure 1). Hence, the patient was admitted to our hospital and was rescued immediately.
Neurological assessment showed cerebral brain stem injury and Frankel Grade B spinal cord function (only sensory function below the injury level)[18].
No abnormalities on preoperative examination.
CT scans revealed posterior atlantoaxial dislocation and no evidence of fracture. The odontoid process was situated anterolateral to the anterior arch of C1 with facet joint dislocation of C1-C2. The atlanto-occipital joint, body and posterior arch of C2, occipital condyles, and the remainder of the visualized cervical spine appeared normal. A T2W MRI midsagittal view of the cervical spine demonstrated no cord compression or intramedullary cord signal abnormality at the level of the atlantoaxial dislocation, with bending in the cervical spinal curvature. On a T1W MRI coronal view of the cervical spine, the membrana tectoria/apical and transverse ligaments at the lateral attachment of the odontoid and the superior transverse ligament were visibly torn (Figure 1).
Traumatic posterior atlantoaxial dislocation (TPAD) without associated fracture but with neurological deficit.
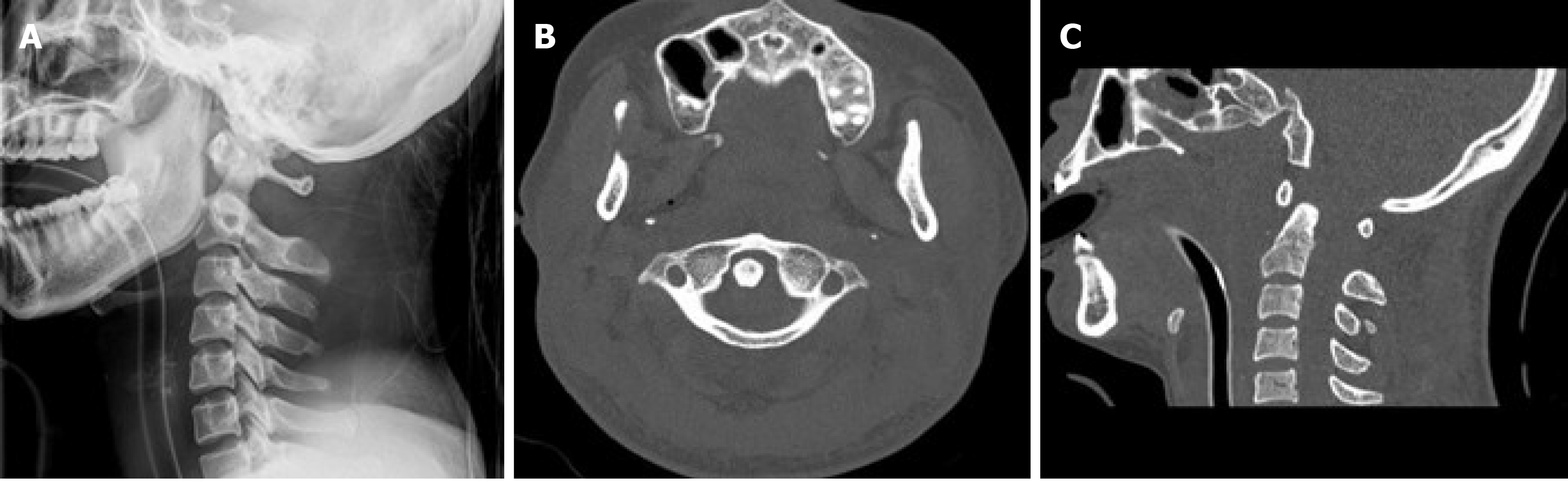
Under general anesthesia (GA), closed reduction under skull traction was attempted immediately, aided by fluoroscopic viewing and neurological monitoring according to the Wong three-step method as follows[11]. During the distraction phase, traction was applied in slight flexion to keep the C1 ring opposed to the posterior odontoid process. While maintaining 10° flexion, traction was increased from 3.0 to 5.0 kg at a rate of 0.5 kg every 15 min. During the realignment phase, the C1 ring had slipped back over the odontoid but was displaced forward because of the slightly excessive flexion angle of traction. During the release phase, traction was modified to slight extension, allowing the C1 ring to come closer to the anterior odontoid process. Then traction was released and a cervical collar was applied. Fluoroscopy imaging demonstrated that the odontoid process was reset in the osseo-ligamentous ring of C1, and lateral X-ray of the cervical spine showed an atlantodental interval (ADI) of 11 mm and atlantoaxial interval (AAI) of 32 mm. CT of coronal and midsagittal sections of the cervical spine revealed that the odontoid process returned to the C1 ring, but the lateral atlantodental space remained asymmetric (the right side was smaller than the left side; Figure 2).
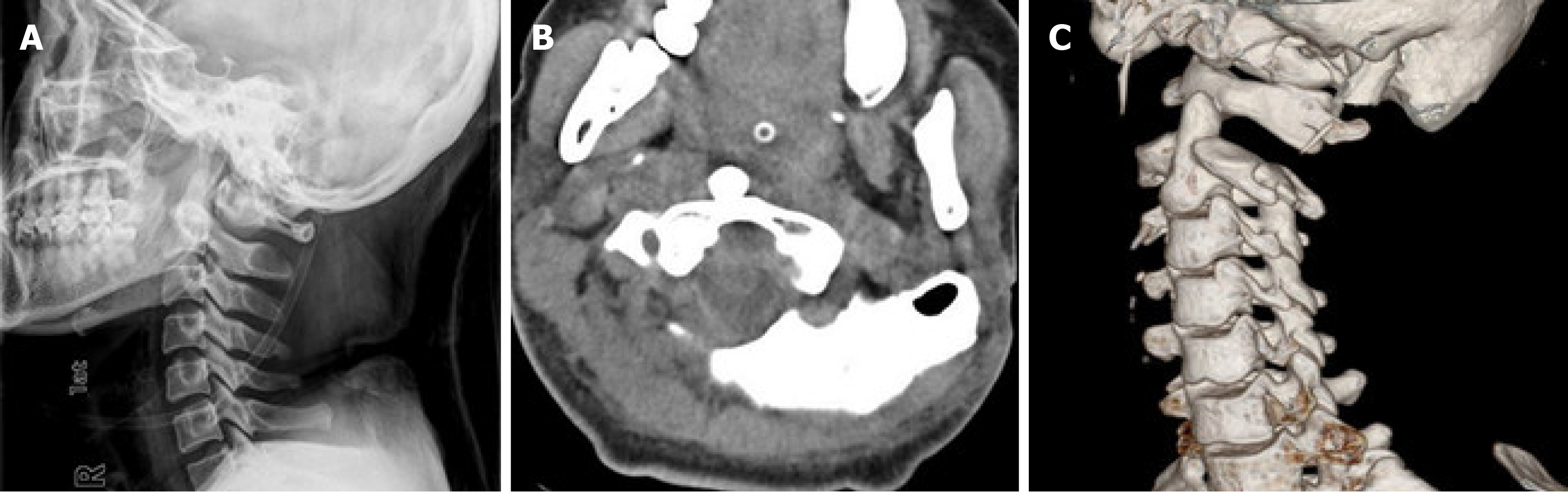
On day 2, the patient recovered consciousness but her respiration was blocked. Thus, a tracheotomy was performed. On days 3, 7, and 12, X-rays were taken and re-dislocation was not observed. Her neural function recovered to Frankel Grade C by day 10. However, her mental state deteriorated with obvious loss of muscle strength in the limbs on day 17. Re-dislocation was confirmed by X-ray and CT scans (Figure 3).
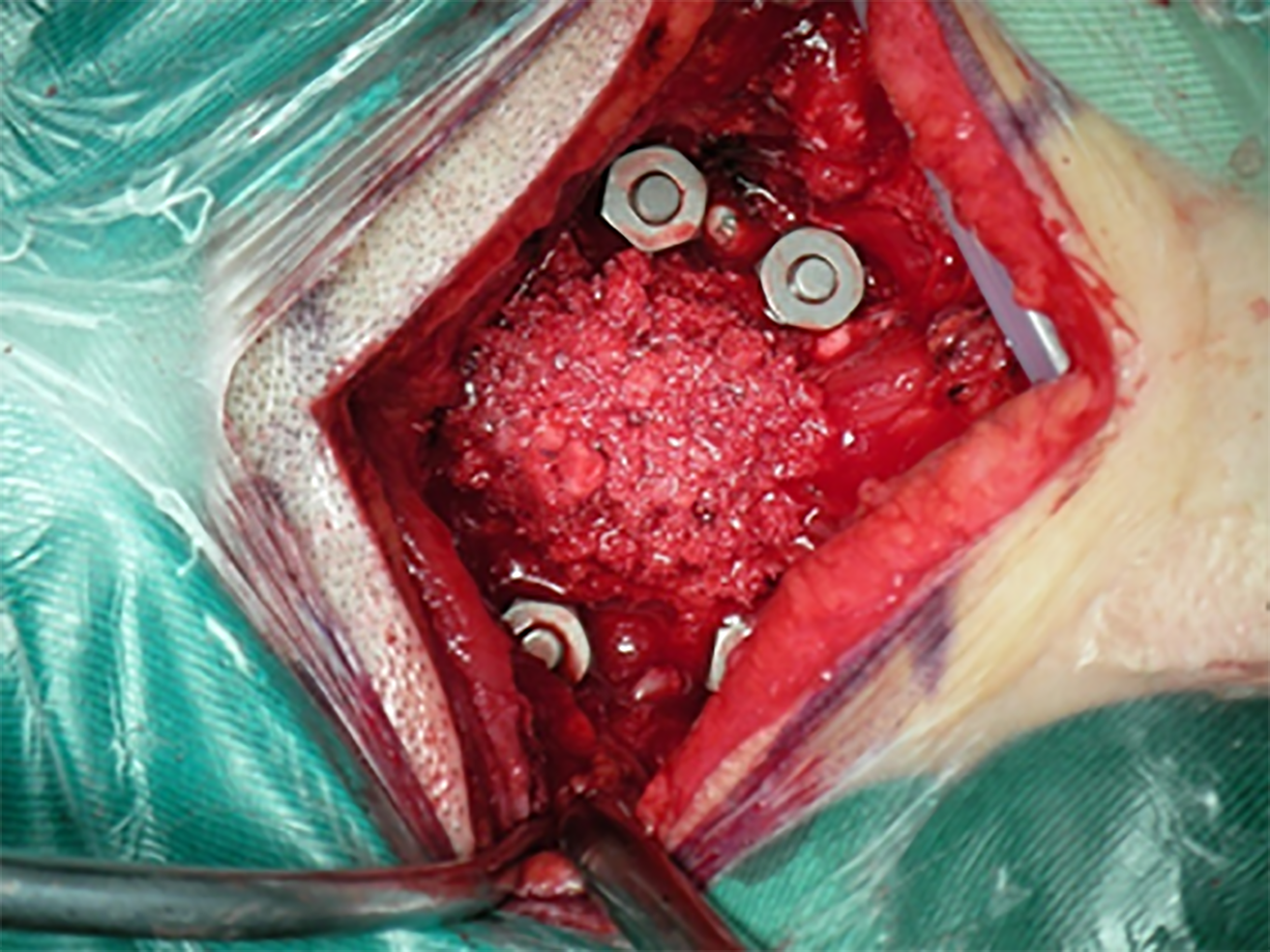
Due to the patient’s cerebral brain stem injury and poor respiration, reduction of the repeated dislocation was not possible until 28 d after the first reduction. Under GA, closed reduction was attempted as before but failed even with a traction weight of 10.0 kg. With the patient in the prone position under 10.0 kg traction, the facet joints of C1-C2 and C2-C3 were exposed, and as expected, the apical, alar, cruciate, posterior longitudinal, and transverse ligaments were torn. The spinous process of C2 was pulled back gently with a towel clamp, and the posterior arch of C1 was nudged forward by the surgeon’s thumb. A snapping sound indicated successful reduction without odontoidectomy and was confirmed fluoroscopically. Then traction was released. Under fluoroscopy, a cervical fixation system with a 3.5-mm-diameter pedicular screw (Tianjin New Medical Devices Co., Ltd., Tianjin, China) was applied in the C1-C2 pedicles, and interfacial fusion was performed using autologous iliac bone grafts (Figure 4). The cervical spine was immobilized using a rigid cervical collar for 1 mo postoperatively.
Rehabilitation therapy was started the first day after surgery, and the follow-up period was 12 mo. The patient’s neurological function recovered to Frankel Grade C by day 60 and Grade D by day 90. By 6 mo after surgery, atlantoaxial joint fusion was achieved, and neurological function had recovered to Frankel Grade E. After 12 mo, lateral X-ray of the cervical spine showed a normal atlantoaxial complex, with perfect positioning of the pedicular screws and good bone fusion. A T2W MRI midsagittal view of the cervical spine revealed that curvature had returned to normal without cord edema at the C1-C2 Level. A T1W MRI coronal view showed that the odontoid process had returned to the C1 ring (Figure 5). The patient had lost only 15° of cervical rotation, and atlantoaxial complex instability in joint flexing and extending were no longer observed under fluoroscopy. Moreover, an open mouth view with manual cervical traction showed no distraction at the C1-C2 joint.
In general, atlantoaxial dislocation is rare due to the stability of the C1-C2 complex. The odontoid process interlocks within the osseo-ligamentous ring formed ventrally by the anterior arch of the atlas and dorsally by the transverse ligament. Anterior movement of the axis vertebra (C2) is restricted by the anterior arch of the atlas when the odontoid is normal. Posterior movement is restricted by the cruciate ligaments, especially the transverse ligament, and rotatory movement is restricted by the alar ligaments[19,20]. Silbergeld et al[21] reported that posterior displacements of 5-10 mm can develop after isolated transverse ligament rupture, whereas further separation of C1 and C2 without fracture requires disruption of the apical, alar, cruciate, and posterior longitudinal ligaments. Therefore, only trauma tends to cause enough force to induce posterior dislocation, and the injury pattern is consistent with a high-grade hyperextension mechanism, as described by Haralson and Boyd[6]. This theory is supported by the fact that most previously reported cases of posterior atlantoaxial dislocation as well as the present case resulted from road traffic accidents[15].
All previously reported cases had either mild or no neurological deficit related to C1-C2 dislocation[6-17,22]. It seems that if the initial distraction of the atlantoaxial complex does not cause a neurological deficit, then a high degree of displacement can be tolerated in this region due to the large spinal canal[6]. Tucker et al[23] demonstrated that posterior dislocation without odontoid fracture reduced the canal area by only 36%, which avoids injury to the cord. Wong et al[11] proposed that the extra free space also allows a margin of error during reduction. Because patients seen in clinical practice likely represent those who avoided severe distraction injury to the spinal cord, suspicion of dislocation is warranted, especially in patients who have concomitant head injuries and altered mental state. In contrast to previous reports, the neurological deficit in the present case was severe with an unknown mechanism, but in addition to cervical spinal cord injury, cerebral brain stem damage cannot be ruled out as a possible cause.
Possible reduction techniques include closed manipulation under skull traction and open decompression and reduction. Controversy persists regarding whether internal fixation of such injury after closed reduction. Among the 12 previously reported cases in the English literature, seven were successfully treated initially with closed reduction via manipulation and skull traction[6-8,10,11,14,15]. However, stability was achieved without internal fixation in only four cases[7,8,14,15]. We propose that assessment of the transverse ligament is critical when planning treatment, because an intact transverse ligament may sufficiently stabilize the atlantoaxial complex after reduction of the odontoid peg into the osseo-ligamentous ring[6,14]. Zhen et al[17] reported that transverse ligament rupture in cases of anterior atlantoaxial dislocation without fracture can be diagnosed indirectly when radiographs show an ADI ≥ 5 mm. Dickman et al[24] reported that such ligamentous injuries can be directly seen on MRI. A compromised transverse ligament on MRI strongly suggests that internal fixation will be necessary[15,22]. Most commonly, posterior surgical fusion is necessary due to continuing C1-C2 instability or incomplete reduction. In fact, three of the previous seven cases of successful closed reduction eventually underwent posterior fusion and internal fixation[6,10,11].The choices for posterior fixation included wiring techniques and screw constructs[25,26]. The use of C1-C2 pedicle screws is recommended because they afford greater stiffness and are associated with a high fusion rate without postoperative halo vest immobilization. In our patient, dislocation reoccurred after the first closed reduction, and because the transverse ligament was torn, upper cervical spine stability could only be restored via open reduction and posterior stabilization.
Possible reasons for re-dislocation soon after closed reduction in this case include the following: First and most importantly, the C1-C2 complex was quite unstable due to complete rupture of the transverse ligament and disruption of the apical, alar, cruciate, and posterior longitudinal ligaments. This was verified by an ADI of 11 mm and AAI of 32 mm on lateral X-ray after closed reduction. Second, the cervical collar does not sufficiently immobilize C1-C2 and may even increase the AAI, thereby increasing the risk of re-dislocation. Third, excessive extension of the neck during tracheotomy operation or care also could have played a role in the re-dislocation. Finally, other inappropriate movements of cervical vertebra during nasal feeding, repositioning in the bed, and positioning for radiographic examination may have contributed to the re-dislocation.
We have the following recommendations based on treatment outcomes in this case. (1) Early MRI assessment of the transverse ligament after closed reduction is essential, and if the transverse ligament is compromised, internal fixation should be performed as soon as possible. (2) Reliable external fixation should be applied after closed reduction, using devices such as the Halo-vest rack and head-neck-chest brace or plaster, but not a cervical collar. (3) During intubation or tracheotomy, fiber-optic intubation with cervical immobilization is preferred to minimize neck extension. (4) Radiographic examination should be performed immediately if the patient’s mental state or muscle strength in the limbs quickly deteriorates soon after reduction, because these conditions may indicate spinal cord injury resulting from re-dislocation. And (5) Closed reduction should be attempted as soon as possible after re-dislocation. In this case, closed reduction was not attempted immediately following re-dislocation, and failure of the delayed closed reduction was likely due to scar tissue adhesions around the atlantoaxial joint and contracture of the anterior longitudinal ligament and longus capitis and longus colli muscles on both sides.
Closed reduction under fluoroscopic guidance with continuous spinal cord monitoring is preferred for repairing any atlantoaxial dislocation. However, determining the appropriate amount of traction can be difficult, and over-distraction of the C1-C2 complex is often fatal[27]. Alternatively, the flexion/extension maneuver, which is used for reinserting the odontoid process into the osteo-ligamentous ring of the atlas, poses a risk of injury to the spinal cord. Thus, extreme caution must be exercised when repairing any atlantoaxial dislocation.
TPAD without fracture with complete rupture of the transverse ligament can easily reoccur after closed reduction. Early assessment of transverse ligament is critical for TPAD without fracture avoiding re-dislocation.
Manuscript source: Unsolicited manuscript
Corresponding Author's Membership in Professional Societies: Department of Orthopaedic Traumatology, Disability Committee, Chinese Rehabilitation Association.
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Tanrivermis Sayit A S-Editor: Fan JR L-Editor: Filipodia P-Editor: Xing YX
| 1. | Jain VK. Atlantoaxial dislocation. Neurol India. 2012;60:9-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 51] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 2. | Adams VI. Neck injuries: II. Atlantoaxial dislocation--a pathologic study of 14 traffic fatalities. J Forensic Sci. 1992;37:565-573. [PubMed] |
| 3. | Tian NF, Xu HZ, Wu YS, Chi YL. Traumatic atlantoaxial dislocation with type II odontoid fracture. Spine J. 2014;14:1067-1069. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Zitouna K, Riahi H, Lassoued NB, Selmene MA, Barsaoui M, Drissi G. Traumatic Atlantoaxial Dislocation with an Odontoid Fracture: A Rare and Potentially Fatal Injury. Asian J Neurosurg. 2019;14:1249-1252. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Ahuja K, Kandwal P, Singh S, Jain R. Neglected Posttraumatic Atlantoaxial Spondyloptosis with Type 2 Odontoid Fracture: A Case Report. J Orthop Case Rep. 2019;9:80-83. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 6. | Haralson RH 3rd, Boyd HB. Posterior dislocation of the atlas on the axis without fracture. Report of a case. J Bone Joint Surg Am. 1969;51:561-566. [PubMed] |
| 7. | Sassard WR, Heinig CF, Pitts WR. Posterior atlanto-axial dislocation without fracture. Case report with successful conservative treatment. J Bone Joint Surg Am. 1974;56:625-628. [PubMed] |
| 8. | Patzakis MJ, Knopf A, Elfering M, Hoffer M, Harvey JP Jr. Posterior dislocation of the atlas on the axis; a case report. J Bone Joint Surg Am. 1974;56:1260-1262. [PubMed] |
| 9. | Fox JL, Jerez A. An unusual atlanto-axial dislocation. Case report. J Neurosurg. 1977;47:115-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Jamshidi S, Dennis MW, Azzam C, Karim N. Traumatic posterior atlantoaxial dislocation without neurological deficit: case report. Neurosurgery. 1983;12:211-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Wong DA, Mack RP, Craigmile TK. Traumatic atlantoaxial dislocation without fracture of the odontoid. Spine (Phila Pa 1976). 1991;16:587-589. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 31] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 12. | Sud S, Chaturvedi S, Buxi TB, Singh S. Posterior atlantoaxial dislocation without associated fracture. Skeletal Radiol. 2002;31:529-531. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 13. | Yoon DH, Yang KH, Kim KN, Oh SH. Posterior atlantoaxial dislocation without fracture. Case report. J Neurosurg. 2003;98:73-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | Neumann U, Urbanski H, Riedel K. Posterior atlantoaxial dislocation without fracture of the odontoid. A case report. J Bone Joint Surg Am. 2003;85:1343-1346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Chaudhary R, Chaudhary K, Metkar U, Rathod A, Raut A, Sanghvi D. Posterior atlantoaxial dislocation without odontoid fracture. Skeletal Radiol. 2008;37:361-366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 16. | Jiang LS, Shen L, Wang W, Wu H, Dai LY. Posterior atlantoaxial dislocation without fracture and neurologic deficit: a case report and the review of literature. Eur Spine J. 2010;19 Suppl 2:S118-S123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 17. | Zhen P, Lan X, Yang LW. Traumatic posterior atlantoaxial dislocation without associated fracture and neurological deficit. Arch Orthop Trauma Surg. 2011;131:681-685. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 18. | Frankel HL, Hancock DO, Hyslop G, Melzak J, Michaelis LS, Ungar GH, Vernon JD, Walsh JJ. The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. I. Paraplegia. 1969;7:179-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1028] [Cited by in RCA: 1054] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 19. | White AA 3rd, Panjabi MM. The clinical biomechanics of the occipitoatlantoaxial complex. Orthop Clin North Am. 1978;9:867-878. [PubMed] |
| 20. | Tulsi RS. Some specific anatomical features of the atlas and axis: dens, epitransverse process and articular facets. Aust N Z J Surg. 1978;48:570-574. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 21. | Silbergeld DL, Laohaprasit V, Grady MS, Anderson PA, Winn HR. Two cases of fatal atlantoaxial distraction injury without fracture or rotation. Surg Neurol. 1991;35:54-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 22. | Peterson R, Burkhardt E, Sin A. Traumatic Atlantoaxial Dislocation without Neurologic Deficit. World Neurosurg. 2020;140:188-190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 23. | Tucker SK, Taylor BA. Spinal canal capacity in simulated displacements of the atlantoaxial segment: a skeletal study. J Bone Joint Surg Br. 1998;80:1073-1078. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 24. | Dickman CA, Mamourian A, Sonntag VK, Drayer BP. Magnetic resonance imaging of the transverse atlantal ligament for the evaluation of atlantoaxial instability. J Neurosurg. 1991;75:221-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 132] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 25. | Farey ID, Nadkarni S, Smith N. Modified Gallie technique versus transarticular screw fixation in C1-C2 fusion. Clin Orthop Relat Res. 1999;(359):126-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 152] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 26. | Tfifha M, Gaha M, Mama N, Yacoubi MT, Abroug S, Jemni H. Atlanto-axial langerhans cell histiocytosis in a child presented as torticollis. World J Clin Cases. 2017;5:344-348. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 5] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 27. | Botelho RV, de Souza Palma AM, Abgussen CM, Fontoura EA. Traumatic vertical atlantoaxial instability: the risk associated with skull traction. Case report and literature review. Eur Spine J. 2000;9:430-433. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 1.1] [Reference Citation Analysis (0)] |