Published online Dec 6, 2021. doi: 10.12998/wjcc.v9.i34.10681
Peer-review started: April 20, 2021
First decision: June 23, 2021
Revised: June 28, 2021
Accepted: September 14, 2021
Article in press: September 14, 2021
Published online: December 6, 2021
Intravascular papillary endothelial hyperplasia (IPEH) is a rare benign reactive vascular lesion that grows into an expansile compressing mass. It most commonly involves the skin and subcutaneous tissue. Spinal involvement is rare, with only 11 reported cases in the literature. We report, to our knowledge, the first case of IPEH in the cervicothoracic spinal canal and present a literature review.
A 27-year-old man presented with acute-onset neck pain, numbness, and weakness in his extremities. Magnetic resonance imaging showed an epidural mass in the cervicothoracic (C6-T1) spinal canal and vertebral hemangioma (VH) involving the C7 vertebral body. C6-T1 Laminectomy and radical excision of the mass were performed. Histopathological examinations revealed papillary proliferation of vascular endothelial cells with thrombus formation, and an IPEH diagnosis was made. By his 6-mo follow-up appointment, his symptoms were relieved without recurrence. The possible pathogenesis, clinical and imaging features, differential diagnosis, and management of IPEH were reviewed.
We report, to our knowledge, the first case of IPEH in the cervicothoracic spinal canal, treated via complete resection, and showing a favorable outcome. We found a causal relationship between spinal IPEH and VH; this partly explains the mechanism of IPEH.
Core Tip: Intravascular papillary endothelial hyperplasia (IPEH) is a rare benign reactive vascular lesion that grows into an expansile compressing mass. Spine involvement is rare, with only 11 case reports on its occurrence. We reported the first case of IPEH in the cervicothoracic spinal canal, which was treated via complete resection and had a good prognosis. We also found a causal relationship between spinal IPEH and vertebral hemangioma, and this partly explained the mechanism of IPEH.
- Citation: Gu HL, Zheng XQ, Zhan SQ, Chang YB. Intravascular papillary endothelial hyperplasia as a rare cause of cervicothoracic spinal cord compression: A case report. World J Clin Cases 2021; 9(34): 10681-10688
- URL: https://www.wjgnet.com/2307-8960/full/v9/i34/10681.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i34.10681
Intravascular papillary endothelial hyperplasia (IPEH) was first reported in 1923 by Pierre Masson in a case of an infected hemorrhoidal vein. Initial reports referred to the lesion as a “Masson tumor” or hemangioendotheliome vegetant intravasculaire[1]. In 1975, Clearkin and Enzinger described the lesion as an unusual and exaggerated thrombus reorganization, rather than a true tumor, and the condition was renamed IPEH[2]. IPEHs typically occur in the skin and subcutaneous tissues of the head and neck or limbs[3]; it rarely occurs in the spine. To our knowledge, only 11 cases of IPEH of the spine have been reported. We report the first case of IPEH of the cervicothoracic spinal canal and present a literature review.
A 27-year-old man presented to the Department of Spine Surgery of our hospital with complaints of neck pain, limb numbness, and weakness.
His symptoms started suddenly, 4 d prior to hospital presentation.
The patient had no trauma history. A similar episode of transient limb numbness and weakness occurred 6 years earlier.
He denied any personal or family history of other diseases.
Physical examination revealed tenderness of the paraspinal muscle of the C6-T1 spinous process, muted sensory responsiveness to touch along the T1 dermatome, and grade IV muscle strength in the four limbs.
The results of all blood analyses — including coagulation markers, inflammatory indicators, and tumor markers — were within normal limits.
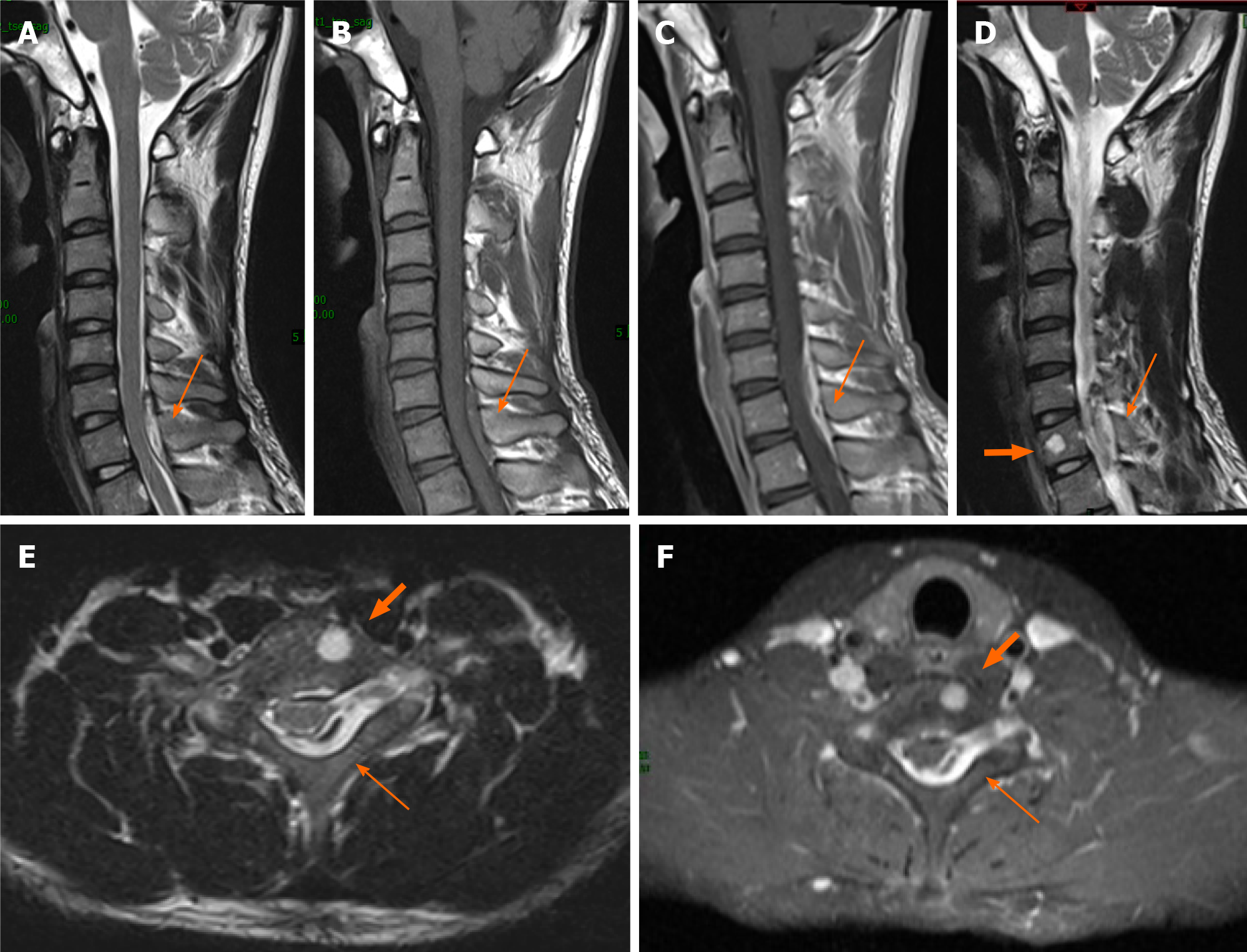
Spinal radiography and computed tomography demonstrated no obvious bone destruction. Enhanced cervical magnetic resonance imaging (MRI) showed a homogenously enhanced epidural mass in the C6-T1 spinal canal. The mass compressed the spinal cord and extended into the left C7-T1 foramen. It appeared hypointense on T1-weighted images (T1WIs) and hyperintense on T2WI. Moreover, a 0.5 cm × 0.5 cm × 0.6 cm-sized heterogeneously enhanced hyperintense mass was found in the C7 vertebral body on T2WI, which was suggestive of a benign vertebral hemangioma (VH) (Figure 1).
The mass was possibly an epidural schwannoma; however, we needed to exclude a nonneurogenic tumor diagnosis. The patient required surgical spinal cord decompression for symptom relief. The final diagnosis was confirmed histopathologically.
The final diagnosis was cervicothoracic spinal IPEH.
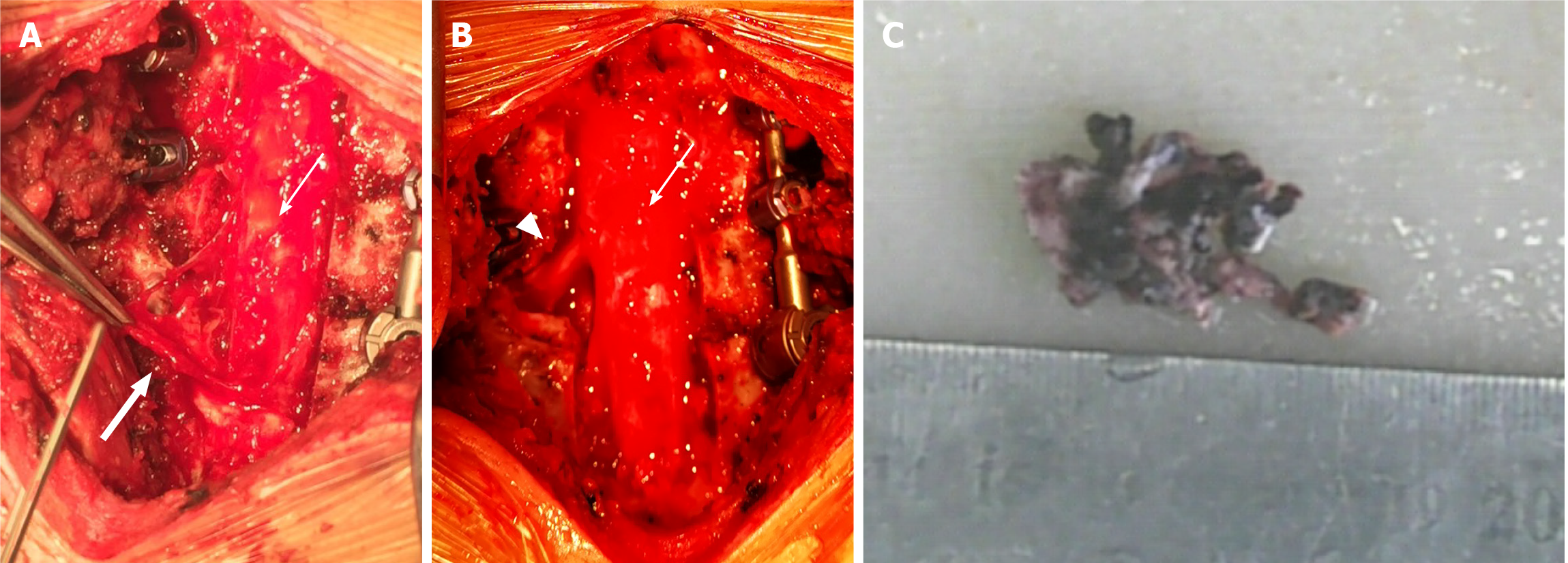
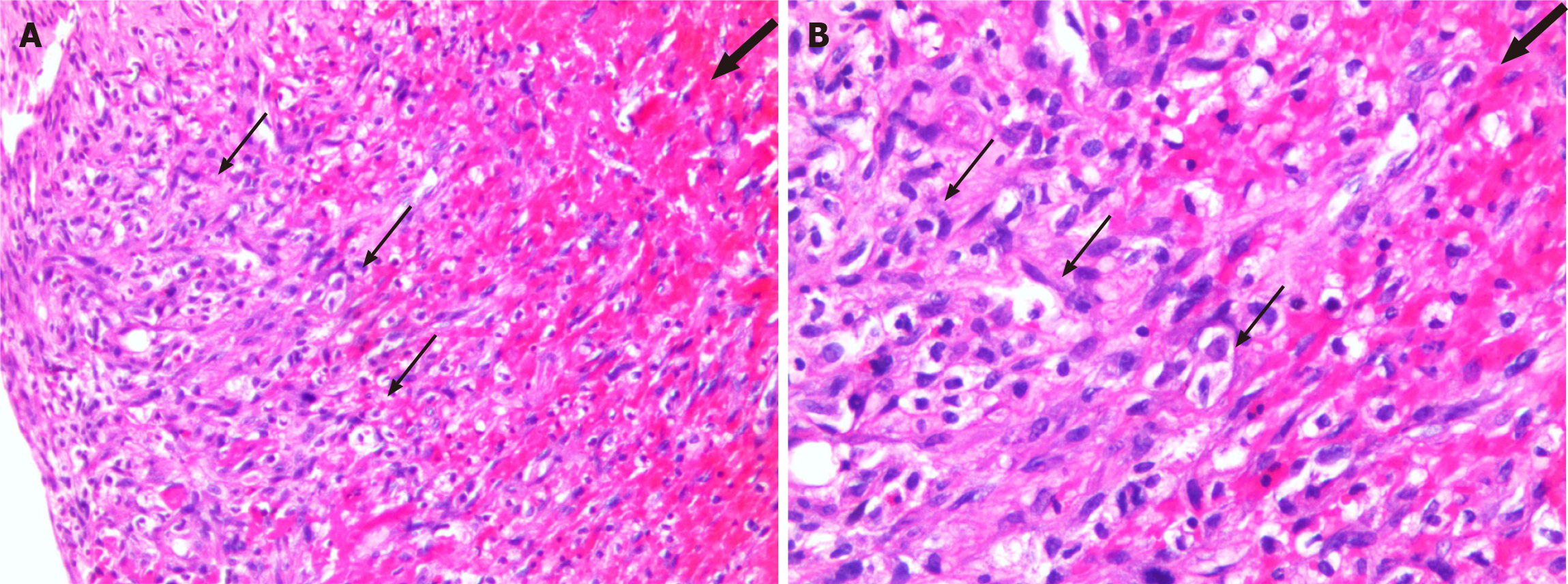
The patient underwent C6-T1 Laminectomy, left C7-T1 foramen decompression, and radical excision of the epidural mass. A C6-T1 posterior instrumented fusion was performed to stabilize the facetectomy at the spinal level, proximal to the cervicothoracic junction. We observed a dark red, nodular, highly vascularized 3 cm × 1.5 cm × 1 cm mass compressing the spinal cord and left C7 nerve root dorsally. The mass was subsequently excised (Figure 2), and an intraoperative frozen section revealed a diagnosis of benign neoplasm originating from blood vessels. Histopathological examination revealed papillary proliferation of vascular endothelial cells with thrombus formation, consistent with IPEH (Figure 3).
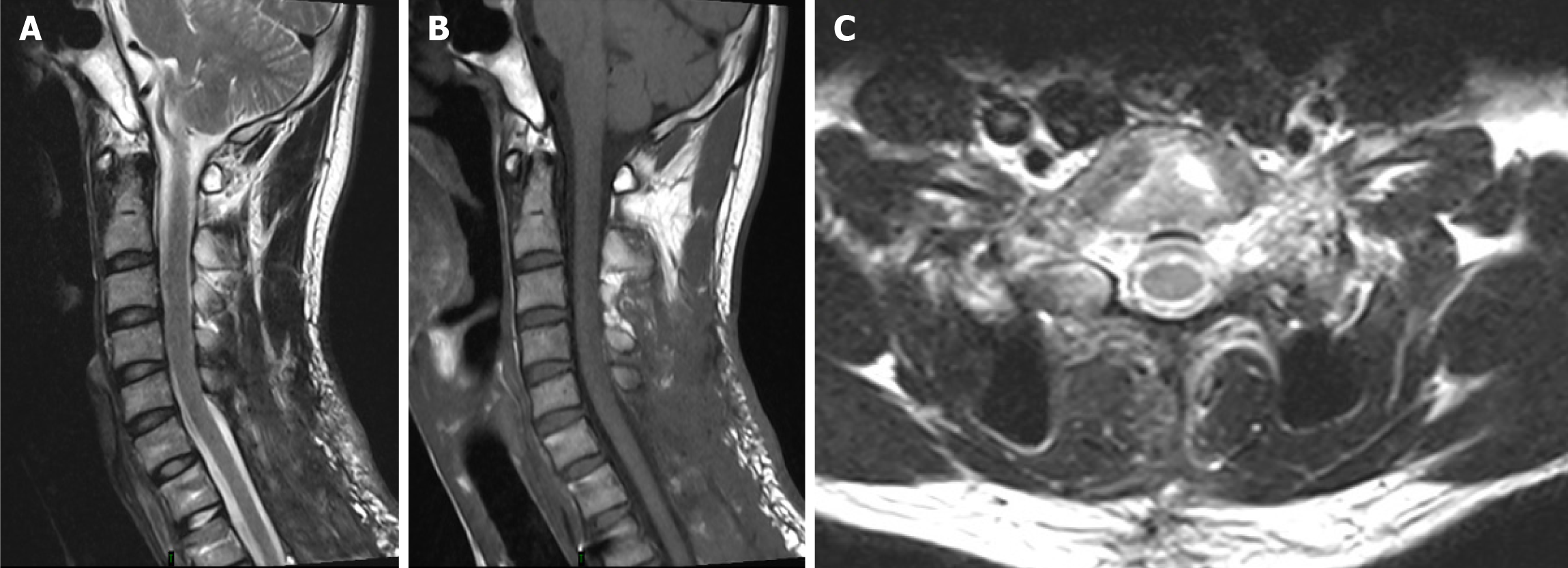
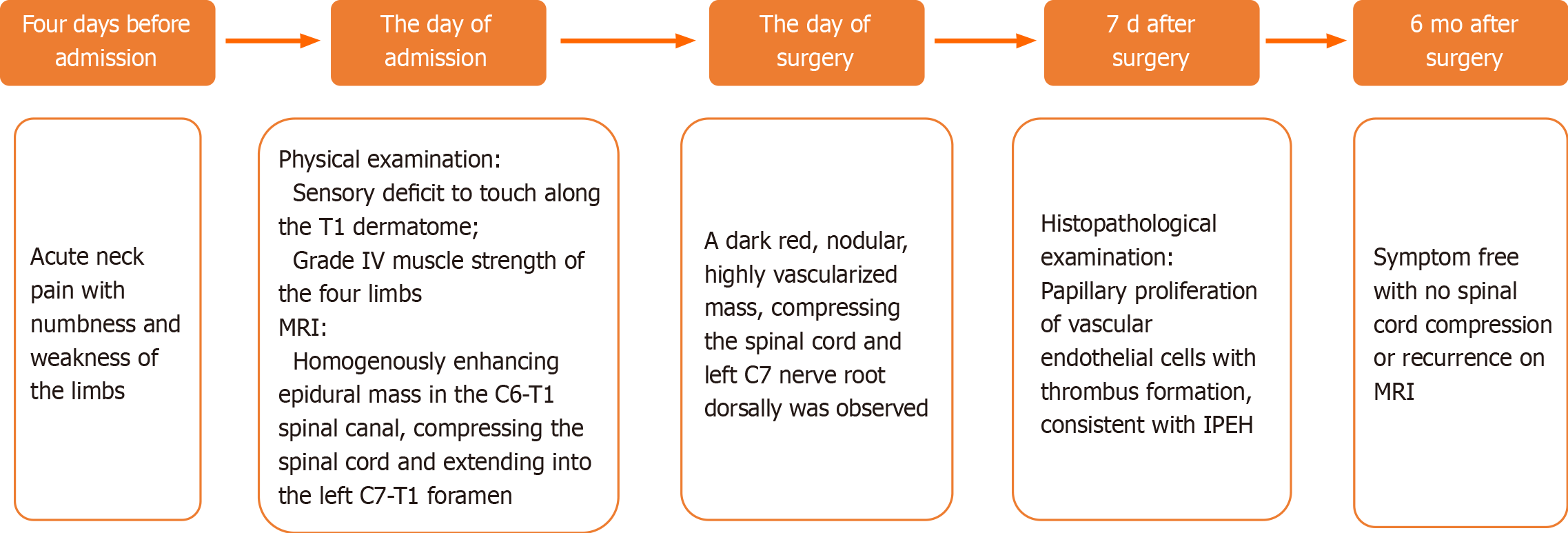
After the surgery, the patient showed gradual neurologic improvement. At his 6-mo follow-up, he was symptom-free, with no spinal cord compression or recurrence on MRI (Figure 4). The clinical timeline of the patient is depicted in Figure 5.
IPEH is a rare benign reactive vascular lesion that expands to form a compressing mass. There is no age predilection for IPEH, and its incidence is higher in women than in men[4], with a female-to-male ratio of 4:1 for intracranial lesions[5]. Although spinal presentations are rare, they occur more commonly in men[6]. IPEHs are commonly located in the skin and subcutaneous tissues of the head and neck or limbs[3] but have also been reported in the oral mucosa, lip, thyroid, maxillary sinus, parotid, lung, superior vena cava, adrenal gland, renal vein, forearm, foot, and intracranially[7-11]. There are 11 reported cases of spinal IPEH, including ten cases involving men and one case involving a woman, with patient age ranging from 16 years to 58 years (see Table 1 for details)[6,12-21]. Among these cases, in one case, the mass was located in the vertebral body and in the remaining ten cases, the mass was located in the spinal canal. Only one case of an intradural mass and nine cases of an epidural mass have been reported. The most common site of involvement was the thoracic spinal canal (n = 7). Of the three remaining cases, two cases involved the lumbar spine and one case involved the thoracolumbar junction. The mass in one case was multifocal, involving the cervical, thoracic, and lumbar vertebral bodies. The present report is the first report of cervicothoracic spinal IPEH.
| No. | Ref. | Year | Age (yr) | Sex | Primary location | Clinical features | RadiologicalFeatures | Treatment | Size (cm) |
| 1 | Ali et al[13] | 1994 | 42 | M | T8 posterior epidural mass | Paraplegia for 2 wk duration | MRI non-specific T1/T2 signal changes | Radical excision | 1.5 |
| 2 | Porter et al[14] | 1995 | 16 | M | T6 posterior epidural mass | Midthoracic radicular back pain with hesitancy for 1-wk duration | CT myelography: extradural thecal compression posteriorly with abnormal lamina | T6 laminectomy with T5-T6 right partial facetectomy | 4 × 2 × 1 |
| 3 | Taricco et al[15] | 1999 | 17 | M | T12-L1 posterior epidural mass | Pain, numbness, paresis of left lower limb with bladder dysfunction for 1 mo | Contrast-enhanced CT of spine: hyperdense lesion; MRI: T1-iso, T2-hyperintense with homogeneous contrast enhancement | T12-L1 laminectomy with radical excision of mass | Not mentioned |
| 4 | Petry et al[12] | 2009 | 47 | M | Multifocal lesions of the spine | Diffuse low back pain | MRI T1-iso, T2-hyperintense with homogeneous contrast enhancement | No surgery | Not mentioned |
| 5 | Lanotte et al[16] | 2010 | 33 | M | T6-T7 paraverte-bral mass extending epidural space | Back pain, hesitancy with paraparesis for 2 wk | MRI T1 hypo- T2 hyperintense mass | T6 laminectomy and excision of intracanal mass | 4.5 × 2.5 × 2.5 |
| 6 | Mozhdehi-panah et al[17] | 2013 | 58 | M | T4-6 posterior epidural mass | Spastic paraparesis and sensory deficit for 1 mo | MRI T2 hyperintense mass | Laminectomy and radical excision of mass | 3×1 |
| 7 | Bhalla et al[21] | 2013 | 51 | F | L1 centered on spinous process and involving pedicles | Back pain with paraparesis | MRI L1 centered on spinous process and involving pedicles causing cauda equina compression | Preoperative embolization, incomplete excision and Radiotherapy | 4.6×4.3×5.5 |
| 8 | Singla et al[18] | 2016 | 40 | M | T12-L1 dumbbell-shaped mass | Back pain and numbness of the right lower trunk for 2 yr | MRI dumbbell-shaped mass mimicking schwannoma | Radical excision | Not mentioned |
| 9 | Behera et al[19] | 2017 | 32 | M | T4-5 posterior epidural mass | Paraplegia for 4 mo | MRI T1 hypo- T2 hyperintense mass | Radical excision | 5 × 3 × 2 |
| 10 | Tanaka et al[20] | 2018 | 40 | M | L2-3 intradural mass | Low back pain and leg pain beginning approximately 5 yr ago and 1 mo ago | Isointense on T1 and hypointense with partial areas of high signal intensity on T2 without contrast enhancement | L2-3 laminectomy and durotomy with radical excision of mass | 2.5 × 1.5 × 1 |
| 11 | Oktar et al[6] | 2019 | 37 | M | T4-5 dumbbell-shaped mass | Dermatomal tingling burning pain with paresis of right lower limb for 1 mo | MRI dumbbell-shaped mass mimicking schwannoma | Radical excision | 5 × 2 × 3 |
| 12 | Present case | 2020 | 27 | M | C6-T1 posterior epidural mass | Neck pain and numbness and weakness of the extremities | MRI: T1-hypo-, T2-hyperintense with homogeneous contrast enhancement | C6-T1 laminectomy with C7-T1 left partial facetectomy and radical excision of the mass | 3 × 1.5 × 1 |
The pathogenesis of IPEH remains controversial. Some authors believe that IPEH is an excessive reaction to a normal thrombus reorganization process[2,22-24]. Others proposed that IPEH is a benign proliferation of endothelial cells with secondary thrombosis and fibrin deposition[25]. Few authors believe that there is a causal relationship between VH and spinal IPEH. Mozhdehipanah et al[17] reported a case of IPEH in the T4-T6 spinal canal. Two adjacent vertebral bodies (T4 and T5) demonstrated VH. The author speculated that bleeding within the spinal canal subsequently formed an organized thrombus, transformed into Masson's hemangioma and manifested symptoms[17]. According to Petry et al[12], IPEH of the vertebral body develops from underlying thrombosis of the basivertebral venous plexus or a preexisting VH. In the present case, spinal cord compression was most severe at the C7 Level. Additionally, a hemangioma was found in the C7 vertebral body, suggesting a possible relationship between spinal IPEH and VH. Therefore, the mechanism behind IPEH could be an excessive reaction to the normal thrombus reorganization process. However, it is difficult to make conclusions based on the few cases. Future, well-powered studies on the relationship between VH and IPEH in the spinal canal are needed.
Preoperative diagnosis of spinal IPEH is challenging because of its non-specific MRI features and the need to differentiate IPEH from arteriovenous malformations, schwannomas, or neurofibromas via imaging technology. Reported cases of spinal IPEH mostly exhibited isointensity or low signal intensity on T1WI and high or variable signal intensity on T2WI with contrast enhancement. Three cases presented as dumbbell-shaped masses, mimicking schwannoma[6]. The present patient was preoperatively diagnosed with epidural schwannoma, which typically features papillary proliferation of vascular endothelial cells, localized intravascularly, with normal thrombus formation in the entire papillary tissue[4,23,26]. The pathological findings in our case are consistent with a diagnosis of IPEH. However, IPEH must be distinguished from other benign and malignant lesions, including cavernous/capillary hemangioma, Kaposi sarcoma, endovascular papillary, and angioendothelioma. Importantly, IPEH should be differentiated from angiosarcoma to avoid unnecessary radiation and surgery[11].
Spinal manifestations of IPEH may be associated with chest or back pain, lower limb numbness, paralysis, and bladder dysfunction caused by spinal cord or cauda equina compression[6]. Treatment is only considered when pain or compression-related symptoms occur, and complete surgical resection is the preferred treatment. Prognosis after complete resection is good, with minimal recurrence. Nine of the 11 patients in the reported cases underwent radical resection, and no recurrence was noted during follow-up. Further, the patient in the present case — who presented with acute-onset numbness and weakness of the limbs owing to spinal cord compression — underwent complete surgical resection. His symptoms were relieved and had not recurred by the 6-mo follow-up visit. Adjuvant radiotherapy can be considered for lesions that cannot be completely removed or that are recurrent. To our knowledge, there is only one reported case of radiotherapy for incompletely resected spinal IPEH. This case showed the potential benefit of radiation following the recurrence of benign IPEH in a patient with epidural disease[21].
The main pathological change attributable to IPEH is benign vascular endothelial papillary hyperplasia with thrombosis; however, the mechanism of this relationship remains controversial. Spinal IPEH is rare, occurring more frequently in men, and is localized to the thoracic spine. Importantly, our findings suggest that spinal IPEH is related to VH. There are no prior reports of IPEH in the cervical spinal canal. To our knowledge, this is the first case of IPEH in the cervicothoracic spinal canal which was associated with a favorable outcome after complete resection.
The authors wish to thank the patient for his contributions to this report.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Specialty type: Neurosciences
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Cucuzza ME, Khanna V, Kung WM S-Editor: Gong ZM L-Editor: Filipodia P-Editor: Wang LYT
| 1. | Masson P. Hemangioendotheliome vegetant intravasculaire. Bull Soc Anat (Paris). 1923;93:517-532. [Cited in This Article: ] |
| 2. | Clearkin KP, Enzinger FM. Intravascular papillary endothelial hyperplasia. Arch Pathol Lab Med. 1976;100:441-444. [PubMed] [Cited in This Article: ] |
| 3. | Espinosa A, González J, García-Navas F. Intravascular Papillary Endothelial Hyperplasia at Foot Level: A Case Report and Literature Review. J Foot Ankle Surg. 2017;56:72-74. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Hashimoto H, Daimaru Y, Enjoji M. Intravascular papillary endothelial hyperplasia. A clinicopathologic study of 91 cases. Am J Dermatopathol. 1983;5:539-546. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 209] [Cited by in F6Publishing: 183] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 5. | Perez Prat G, Serrano Jimenez M, Cancela Caro P, Cardenas Ruiz-Valdepeñas E, Rivero Garvia M, Marquez Rivas FJ. Staged Management of Intracranial Masson Tumor: An Unexpected Gauntlet: Case Report and Review of the Literature. World Neurosurg. 2018;114:194-203. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Oktar N, M Ozer H, Demirtas E. Spinal intravascular papillary endothelial hyperplasia. Case report and review of the literature. Br J Neurosurg. 2019;1-3. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Mahapatra QS, Sahai K, Malik A, Mani NS. Intravascular papillary endothelial hyperplasia: An unusual histopathological entity. Indian Dermatol Online J. 2015;6:277-279. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Barritt AW, Merve A, Epaliyanage P, Aram J. Intracranial papillary endothelial hyperplasia (Masson's tumour) following gamma knife radiosurgery for temporal lobe epilepsy. Pract Neurol. 2017;17:214-217. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Narwal A, Sen R, Singh V, Gupta A. Masson's hemangioma: A rare intraoral presentation. Contemp Clin Dent. 2013;4:397-401. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Clifford PD, Temple HT, Jorda M, Marecos E. Intravascular papillary endothelial hyperplasia (Masson's tumor) presenting as a triceps mass. Skeletal Radiol. 2004;33:421-425. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 23] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 11. | Mardani P, Askari A, Shahriarirad R, Ranjbar K, Erfani A, Anbardar MH, Moradmand S. Masson's Tumor of the Hand: An Uncommon Histopathological Entity. Case Rep Pathol. 2020;2020:4348629. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Petry M, Brown MA, Hesselink JR, Imbesi SG. Multifocal intravascular papillary endothelial hyperplasia in the retroperitoneum and spine: a case report and review of the literature. J Magn Reson Imaging. 2009;29:957-961. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 15] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Ali SZ, Farmer PM, Black K, Rosenthal A. Masson's hemangioma of spinal meninges causing cord compression with paraplegia. Ann Clin Lab Sci. 1994;24:371-375. [PubMed] [Cited in This Article: ] |
| 14. | Porter DG, Martin AJ, Mallucci CL, Makunura CN, Sabin HI. Spinal cord compression due to Masson's vegetant intravascular hemangioendothelioma. Case report. J Neurosurg. 1995;82:125-127. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 19] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 15. | Taricco MA, Vieira JO Jr, Machado AG, Ito FY. Intravascular papillary endothelial hyperplasia causing cauda equina compression: case report. Neurosurgery. 1999;45:1478-1480. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 16. | Lanotte M, Molinaro L, Crudo V, Filosso PL, Crasto SG, Roncaroli F, Cassoni P. Spinal cord compression due to an extra-dural intra-vascular papillary endothelial hyperplasia of the thoracic spine. Acta Neurochir (Wien). 2010;152:877-880. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 17. | Mozhdehipanah H, Samiei F, Sayadnasiri M. Masson's hemangioma: A very rare cause of spinal cord compression. Neurol India. 2013;61:89-90. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 18. | Singla N, Kapoor A, Sodhi HB, Bal A, Chatterjee D. Straddling across the neural foramina with a leash of blood vessels: Mason's vegetant intravascular hemangioendothelioma mimicking a schwannoma. Neurol India. 2016;64:348-349. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 19. | Behera BR, Panda RN, Mishra S, Dhir MK. Masson Hemangioma-An Unusual Cause of Thoracic Compressive Myelopathy. World Neurosurg. 2017;98:876.e9-876.e13. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 20. | Tanaka M, Hiyama A, Sakai D, Katoh H, Sato M, Watanabe M. Intravascular Papillary Endothelial Hyperplasia (Masson's Tumor) Within Cauda Equina. J Am Acad Orthop Surg Glob Res Rev. 2018;2:e087. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 21. | Bhalla N, Husband DJ, Pillay R, Thorp N. Radiotherapy for a benign cause of cauda equina compression in a known case of breast carcinoma. BMJ Case Rep. 2013;2013. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 22. | Salyer WR, Salyer DC. Intravascular angiomatosis: development and distinction from angiosarcoma. Cancer. 1975;36:995-1001. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 23. | Akdur NC, Donmez M, Gozel S, Ustun H, Hucumenoglu S. Intravascular papillary endothelial hyperplasia: histomorphological and immunohistochemical features. Diagn Pathol. 2013;8:167. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 53] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 24. | Guledgud MV, Patil K, Saikrishna D, Madhavan A, Yelamali T. Intravascular papillary endothelial hyperplasia: diagnostic sequence and literature review of an orofacial lesion. Case Rep Dent. 2014;2014:934593. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 25. | Kuo T, Gomez LG. Papillary endothelial proliferation in cystic lymphangiomas. A lymphatic vessel counterpart of Masson's vegetant intravascular hemangioendothelioma. Arch Pathol Lab Med. 1979;103:306-308. [PubMed] [Cited in This Article: ] |
| 26. | Díaz-Flores L, Gutiérrez R, Madrid JF, García-Suárez MP, González-Álvarez MP, Díaz-Flores L Jr, Sáez FJ. Intravascular papillary endothelial hyperplasia (IPEH). Evidence supporting a piecemeal mode of angiogenesis from vein endothelium, with vein wall neovascularization and papillary formation. Histol Histopathol. 2016;31:1271-1279. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 4] [Reference Citation Analysis (0)] |