Published online Nov 26, 2021. doi: 10.12998/wjcc.v9.i33.10279
Peer-review started: May 24, 2021
First decision: June 25, 2021
Revised: July 8, 2021
Accepted: August 19, 2021
Article in press: August 19, 2021
Published online: November 26, 2021
Processing time: 181 Days and 18 Hours
Cerebral hemorrhage secondary to cerebral embolism after mechanical throm
A 70-year-old woman presented to our emergency department with right-sided hemiplegia and mixed aphasia of 2.5 h duration. She was diagnosed with left cerebral embolism, left internal carotid artery occlusion, PE and left calf intramuscular vein thrombosis. Following mechanical thrombectomy, brain magnetic resonance imaging showed cerebral infarction with basal ganglia hemorrhage. We observed changes in cerebral hemorrhage on serial monitoring of brain computed tomography and adjusted the dose of anticoagulant drugs. After 3 wk of treatment, the patient’s neurological and respiratory symptoms signifi
Anticoagulation could be a potential option for PE accompanied by hemorrhagic transformation of an ischemic infarct.
Core Tip: Pulmonary embolism accompanied by cerebral hemorrhage secondary to cerebral embolism after mechanical thrombectomy is characterized by high disability and mortality. To manage this situation, we adopted a treatment strategy that involved adjustment of anticoagulant drugs according to the changes in cerebral hemorrhage after mechanical thrombectomy. The patient had a favorable prognosis.
- Citation: Chen XT, Zhang Q, Zhou CQ, Han YF, Cao QQ. Anticoagulant treatment for pulmonary embolism in patient with cerebral hemorrhage secondary to mechanical thrombectomy: A case report. World J Clin Cases 2021; 9(33): 10279-10285
- URL: https://www.wjgnet.com/2307-8960/full/v9/i33/10279.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i33.10279
Cerebral hemorrhage secondary to cerebral embolism after mechanical thrombectomy is characterized by high morbidity, disability and mortality[1]. If the patient also has severe pulmonary embolism (PE) at the same time, the prognosis may be poor. In this situation, the treatment choice is critical. We report a patient with PE and cerebral hemorrhage secondary to cerebral embolism after thrombectomy who was treated with anticoagulant drugs and her neurological and respiratory symptoms significantly improved. As far as we know, this complex situation has not been described in the literature.
A 70-year-old woman presented to our emergency department with right-sided hemiplegia and mixed aphasia.
This patient had a history of pulmonary hypertension for approximately 2 mo, but her shortness of breath was not relieved. Her right-sided hemiplegia and mixed aphasia started 2.5 h ago.
This patient had no history of allergies, denied tobacco and alcohol use, and was healthy with no history of hypertension, diabetes, coronary heart disease, hyperlipidemia, stroke, or cardiac risk factors.
This patient has no relevant family history in particular of clotting disorders.
On arrival, her blood pressure was 118/88 mmHg, heart rate was 93 bpm, and respiratory rate was 25 breaths/min. No pathological breath sounds or heart murmurs were noted and no edema in the lower extremities was observed. Neurological examination revealed mixed aphasia, right hemiplegia, and hypoesthesia. Right-side extremity weakness was noted and was graded 0/5 on the Medical Research Council Scale. Her National Institutes of Health Stroke Scale (NIHSS) score was 25.
Laboratory tests revealed high levels of N-terminal pro-brain natriuretic peptide (2308 pg/mL). Her D-dimer level was also elevated (6.23 mg/L). Results of arterial blood gas analysis indicated obvious hypoxemia (PaO2, 65 mmHg; PaCO2, 36 mmHg; pH, 7.44). Protein C, protein S, antithrombin III, lupus anticoagulant, and factor V Leiden, prothrombin gene mutation as well as anti-β2-glycoprotein-1 antibodies were within normal limits. Twelve-lead electrocardiography showed a normal sinus rhythm.
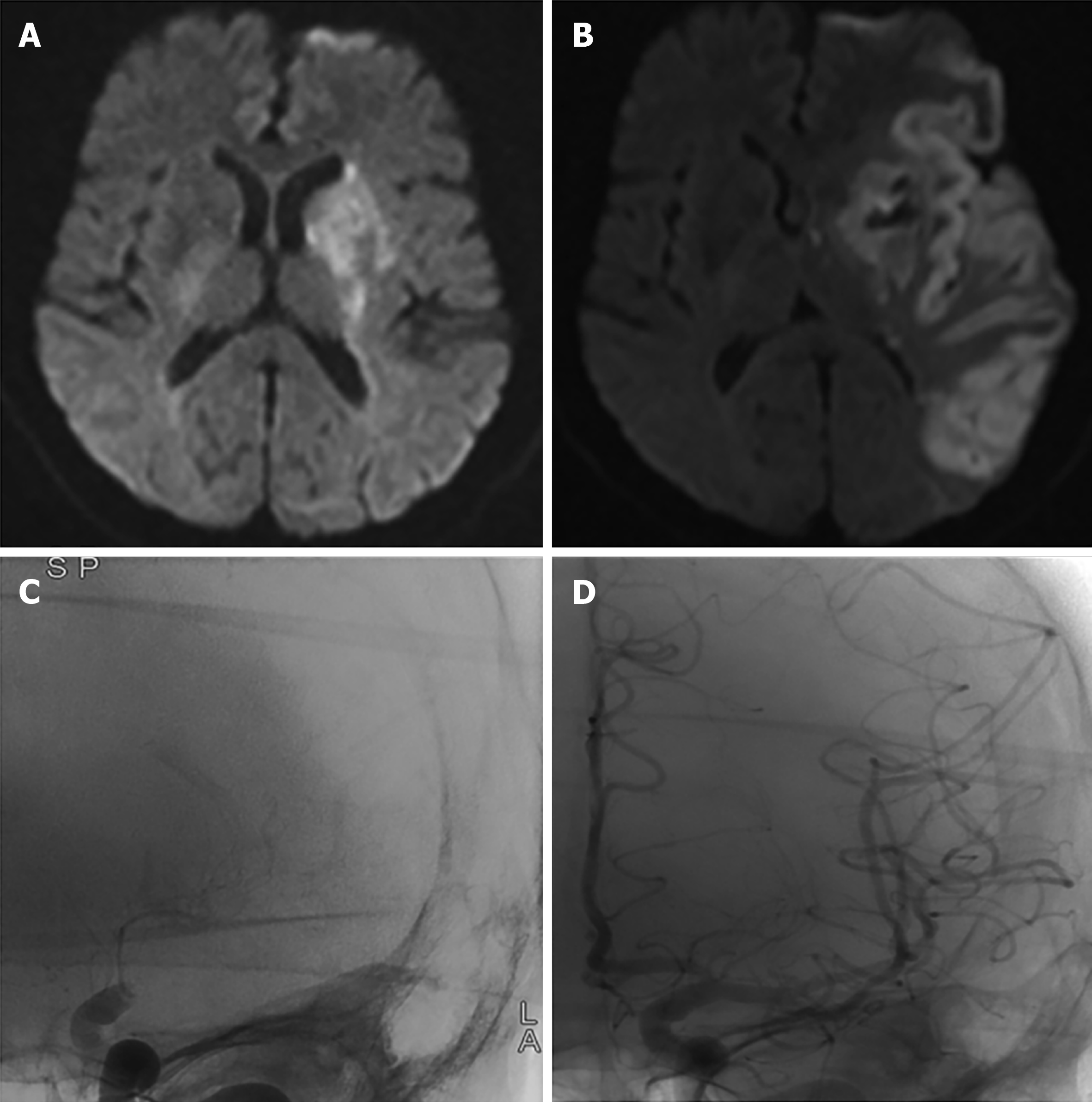
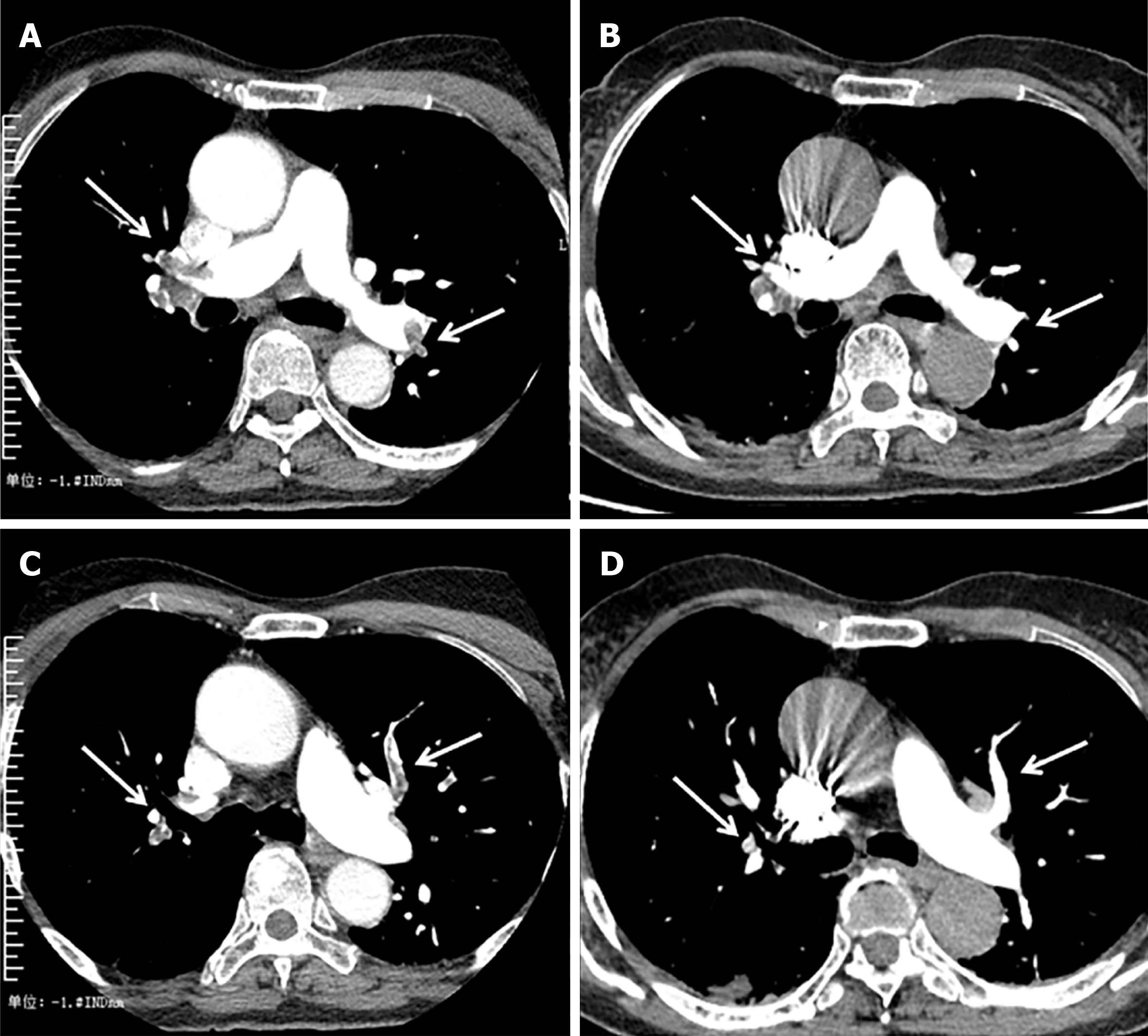
Brain computed tomography angiography (CTA) showed occlusions of the intracranial segment of the left internal carotid artery and the M1 segment of the left middle cerebral artery. The Alberta Stroke Program Early CT Score was 12. Brain magnetic resonance imaging (MRI) revealed acute multiple cerebral infarctions in the bilateral centrum semiovale, left lateral ventricle, and basal ganglia (Figure 1A). Pulmonary angiography showed that both main trunks and partial branches of bilateral pulmonary arteries were embolized (Figure 2A, 2C). Digital subtraction angiography (DSA) was performed and confirmed the CT findings (Figure 1C). Transesophageal echocardiography did not show any abnormalities. Ultrasound of both lower extremities showed thrombosis in the left muscle calf venous thrombosis (MCVT).
Based on these findings, she was diagnosed with left cerebral embolism, left internal carotid artery occlusion, PE, and left MCVT.
Mechanical thrombectomy was performed, and a large number of thrombi were aspirated with a Penumbra ACE suction catheter, and 100 000 U urokinase was administered locally for thrombolysis. Postoperative angiography showed that the left internal carotid artery, distal middle cerebral artery, and anterior cerebral artery were recanalized (Figure 1D), and the distal blood flow was significantly improved (thrombolysis in cerebral infarction; TICI 2b). After surgery, 4000 U enoxaparin solution was administered.
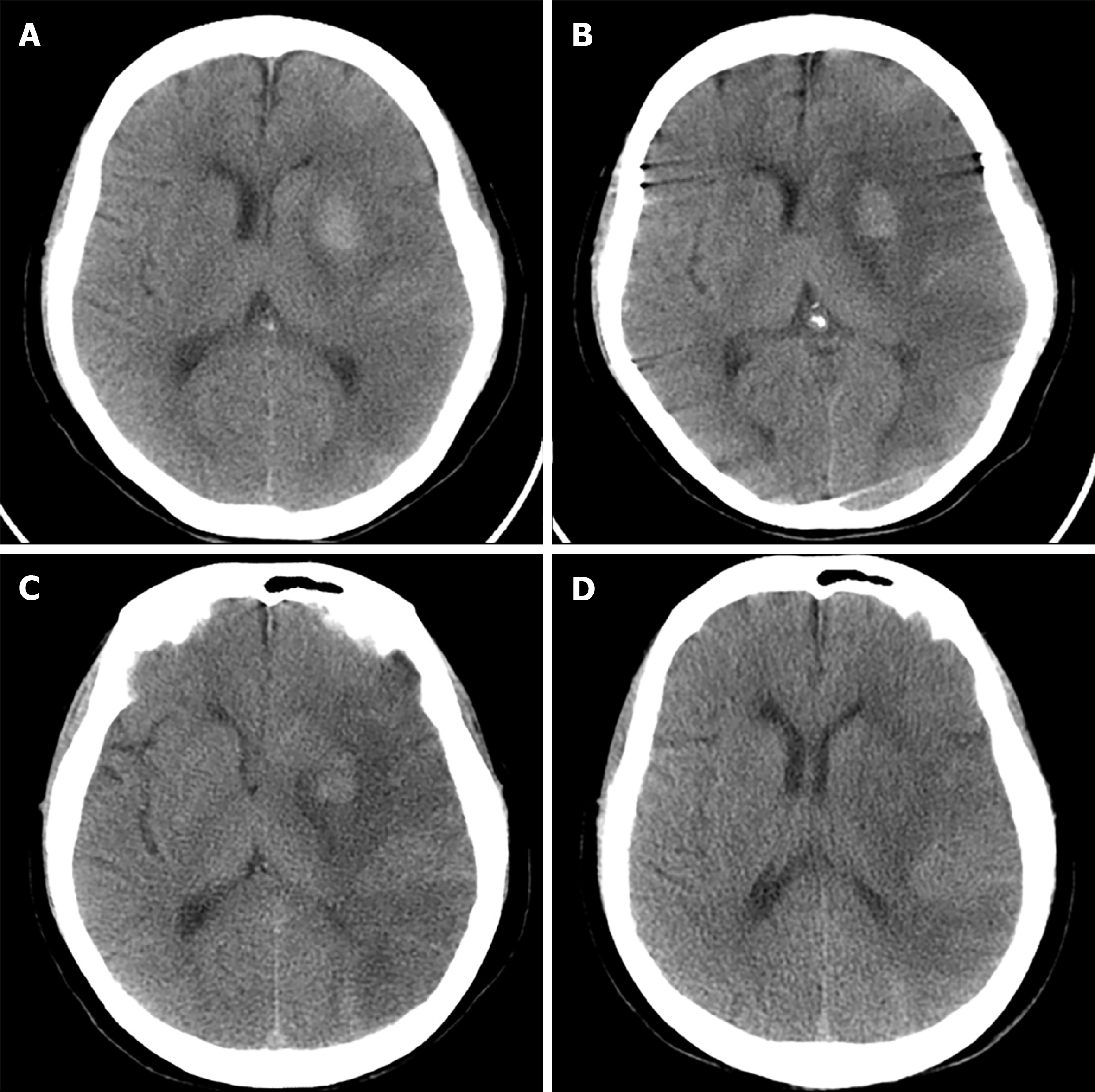
On the first day after surgery, the patient’s consciousness and symptoms of right hemiplegia improved (NIHSS 15 points). Postoperative brain MRI (Figure 1B) and follow-up brain CT (Figure 3A) showed that the left frontotemporal, occipital, parietal, insula, basal ganglia, and hippocampus had subacute large areas of cerebral infarction with basal ganglia hemorrhage. Anticoagulant therapy was stopped. On the second day after surgery, the follow-up CT scans showed that the cerebral hemorrhage had not enlarged markedly (Figure 3B) and the patient was given a subcutaneous injection of enoxaparin 2000 U twice daily as anticoagulant treatment. On the fourth day after surgery, brain CT scans showed that the cerebral hemorrhage had not enlarged and enoxaparin was changed to 4000 U twice daily. On day 20 after surgery, D-dimer, N-terminal pro-brain natriuretic peptide and blood gas analysis returned to normal levels. Dyspnea gradually resolved. There was no new evidence of cerebral infarction or hemorrhage on repeat CT of the brain (Figure 3C, 3D). Pulmonary angiography showed that the PE had improved (Figure 2B, 2D). Because the patient had left MCVT, combined with PE and cerebral hemorrhage, we suggest considering temporary inferior vena cava filter (IVCF) placement, but the patient’s family refused this treatment.
The patient was discharged to a rehabilitation center 3 wk after admission. The last brain CT scan showed no evidence of new cerebral infarction or hemorrhage. At the time of discharge, the patient showed slight fluid aphasia with right hemiplegia. There was right-sided upper extremity weakness graded 2/5 and lower extremity weakness graded 3/5 on the Medical Research Council Scale. Her NIHSS score was 9 and Modified Rankin Scale was 4. Dyspnea was not observed. The patient was discharged to an oral anticoagulant, namely warfarin, and no recurrence of cerebral infarction or cerebral hemorrhage was found after 6 mo of follow-up.
We present the unique case of a patient with PE and cerebral hemorrhage secondary to cerebral embolism after mechanical thrombectomy. However, after anticoagulant treatment, the neurological deficit and dyspnea symptoms gradually resolved, and the patient had a good prognosis. As far as we know, there are no similar case reports.
In this study, MRI revealed that the bilateral brain showed mostly scattered lesions, and the diagnosis of multiple cerebral infarctions was made. However, neither CTA nor DSA showed obvious atherosclerotic plaques. Therefore, it is unlikely that atherosclerotic plaques were present. In addition, the patient did not have common risk factors for stroke, such as diabetes, hyperlipidemia, or hypertension[2]. She was diagnosed with pulmonary hypertension in the other hospital, but because they did not further investigate the cause, this led to subsequent aggravation of the patient’s condition. The patient had cerebral embolism and PE, and both the venous and arterial systems were affected at the same time. Therefore, the patient may have had rare causes leading to chronic PE and further pulmonary hypertension. Pulmonary hypertension may cause a brief right-to-left shunt and emboli from pulmonary arteries to enter the left heart system, finally causing paradoxical cerebral embolism[3]. Although the patient’s cardiac examination showed no abnormal passage between the right heart and left heart, abnormal passages such as patent foramen ovale may be closed or healed as the PE improves[4]. This may be related to the pressure change between the right and left atria.
Based on these findings, combined with the patient’s lower extremity ultrasound, the possibility of PE caused by the left MCVT was considered. MCVT is a peripheral type of deep vein thrombosis (DVT) of the lower extremities and is considered to be the most common origin of DVT. There are related reports that MCVT can spread to the deep veins to form more serious DVT and cause chronic PE[5], or embolus may become detached and cause chronic PE[6], so we considered this possibility. At present, there is still a lack of robust evidence-based medical evidence to guide standardized treatment of MCVT; therefore, we still recommended the use of IVCFs to prevent the occurrence of another PE for this patient. It should be noted that the purpose of IVCF is to prevent PE and therefore to reduce associated morbidity and mortality, although randomized trials are needed[7,8]. In patients undergoing anticoagulation for DVT or PE in whom a contraindication to anticoagulation develops, many guidelines and expert consensus suggest[9] that an IVCF be considered in the setting of ongoing significant clinical risk for PE. Furthermore, we have not found the cause of venous thrombosis, so rare causes of venous thrombosis could not be excluded[10].
This patient had a large area of cerebral embolism caused by acute occlusion of the internal carotid artery and was treated with emergency mechanical thrombectomy. Postoperative CT showed hemorrhagic transformation of an ischemic infarct. However, the patient also had multiple emboli in both pulmonary aortic trunks, and both blood gas analysis and dyspnea indicated severe PE. Anticoagulation is indicated for the treatment of PE[11], but it may aggravate cerebral hemorrhage. However, if anticoagulation is not administered, PE may gradually worsen and threaten the patient’s life. Furthermore, the recanalized blood vessel may be occluded again. Cerebral hemorrhage secondary to mechanical thrombectomy is not always ag
It is unlikely that a specific treatment regimen will work for all patients. In patients with PE combined with cerebral embolism, especially those with cerebral hemorrhage secondary to mechanical thrombectomy, the benefit of anticoagulation and the risk of bleeding should be carefully evaluated to implement an individualized treatment strategy. Disease evolution should be closely monitored to adjust the treatment strategy at any time.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Specialty type: Clinical neurology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Konala VM S-Editor: Ma YJ L-Editor: Kerr C P-Editor: Yu HG
| 1. | Zi W, Wang H, Yang D, Hao Y, Zhang M, Geng Y, Lin M, Wan Y, Shi Z, Zhou Z, Wang W, Xu H, Tian X, Lv P, Wang S, Liu W, Wang Z, Liu X, Guo F, Zheng D, Li H, Tu M, Jin P, Xiao G, Liu Y, Xu G, Xiong Y; ACTUAL Investigators. Clinical Effectiveness and Safety Outcomes of Endovascular Treatment for Acute Anterior Circulation Ischemic Stroke in China. Cerebrovasc Dis. 2017;44:248-258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 54] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 2. | Chao TF, Lip GYH, Liu CJ, Lin YJ, Chang SL, Lo LW, Hu YF, Tuan TC, Liao JN, Chung FP, Chen TJ, Chen SA. Relationship of Aging and Incident Comorbidities to Stroke Risk in Patients With Atrial Fibrillation. J Am Coll Cardiol. 2018;71:122-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 150] [Article Influence: 21.4] [Reference Citation Analysis (0)] |
| 3. | Schäbitz WR, Köhrmann M, Schellinger PD, Minnerup J, Fisher M. Embolic Stroke of Undetermined Source: Gateway to a New Stroke Entity? Am J Med. 2020;133:795-801. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Ryoo S, Chung JW, Lee MJ, Kim SJ, Lee JS, Kim GM, Chung CS, Lee KH, Hong JM, Bang OY. An Approach to Working Up Cases of Embolic Stroke of Undetermined Source. J Am Heart Assoc. 2016;5:e002975. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 5. | Kret MR, Liem TK, Mitchell EL, Landry GJ, Moneta GL. Isolated calf muscular vein thrombosis is associated with pulmonary embolism and a high incidence of additional ipsilateral and contralateral deep venous thrombosis. J Vasc Surg Venous Lymphat Disord. 2013;1:33-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Su H, Liu H, Liu J, Wang X. Elderly patients with intertrochanteric fractures after intramedullary fixation : Analysis of risk factors for calf muscular vein thrombosis. Orthopade. 2018;47:341-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 7. | Turner TE, Saeed MJ, Novak E, Brown DL. Association of Inferior Vena Cava Filter Placement for Venous Thromboembolic Disease and a Contraindication to Anticoagulation With 30-Day Mortality. JAMA Netw Open. 2018;1:e180452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 47] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 8. | Kakkos SK, Gohel M, Baekgaard N, Bauersachs R, Bellmunt-Montoya S, Black SA, Ten Cate-Hoek AJ, Elalamy I, Enzmann FK, Geroulakos G, Gottsäter A, Hunt BJ, Mansilha A, Nicolaides AN, Sandset PM, Stansby G; Esvs Guidelines Committee; de Borst GJ, Bastos Gonçalves F, Chakfé N, Hinchliffe R, Kolh P, Koncar I, Lindholt JS, Tulamo R, Twine CP, Vermassen F, Wanhainen A, Document Reviewers, De Maeseneer MG, Comerota AJ, Gloviczki P, Kruip MJHA, Monreal M, Prandoni P, Vega de Ceniga M. Editor's Choice - European Society for Vascular Surgery (ESVS) 2021 Clinical Practice Guidelines on the Management of Venous Thrombosis. Eur J Vasc Endovasc Surg. 2021;61:9-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 385] [Article Influence: 77.0] [Reference Citation Analysis (0)] |
| 9. | Kaufman JA, Barnes GD, Chaer RA, Cuschieri J, Eberhardt RT, Johnson MS, Kuo WT, Murin S, Patel S, Rajasekhar A, Weinberg I, Gillespie DL. Society of Interventional Radiology Clinical Practice Guideline for Inferior Vena Cava Filters in the Treatment of Patients with Venous Thromboembolic Disease: Developed in collaboration with the American College of Cardiology, American College of Chest Physicians, American College of Surgeons Committee on Trauma, American Heart Association, Society for Vascular Surgery, and Society for Vascular Medicine. J Vasc Interv Radiol. 2020;31:1529-1544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 116] [Article Influence: 23.2] [Reference Citation Analysis (0)] |
| 10. | Hart RG, Diener HC, Coutts SB, Easton JD, Granger CB, O'Donnell MJ, Sacco RL, Connolly SJ; Cryptogenic Stroke/ESUS International Working Group. Embolic strokes of undetermined source: the case for a new clinical construct. Lancet Neurol. 2014;13:429-438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 980] [Cited by in RCA: 1173] [Article Influence: 106.6] [Reference Citation Analysis (0)] |
| 11. | Konstantinides SV, Meyer G, Becattini C, Bueno H, Geersing GJ, Harjola VP, Huisman MV, Humbert M, Jennings CS, Jiménez D, Kucher N, Lang IM, Lankeit M, Lorusso R, Mazzolai L, Meneveau N, Ní Áinle F, Prandoni P, Pruszczyk P, Righini M, Torbicki A, Van Belle E, Zamorano JL; ESC Scientific Document Group. 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS). Eur Heart J. 2020;41:543-603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1251] [Cited by in RCA: 2566] [Article Influence: 641.5] [Reference Citation Analysis (1)] |
| 12. | Charidimou A, Karayiannis C, Song TJ, Orken DN, Thijs V, Lemmens R, Kim J, Goh SM, Phan TG, Soufan C, Chandra RV, Slater LA, Haji S, Mok V, Horstmann S, Leung KT, Kawamura Y, Sato N, Hasebe N, Saito T, Wong LKS, Soo Y, Veltkamp R, Flemming KD, Imaizumi T, Srikanth V, Heo JH; International META-MICROBLEEDS Initiative. Brain microbleeds, anticoagulation, and hemorrhage risk: Meta-analysis in stroke patients with AF. Neurology. 2017;89:2317-2326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 77] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 13. | Sprügel MI, Sembill JA, Kuramatsu JB, Gerner ST, Hagen M, Roeder SS, Endres M, Haeusler KG, Sobesky J, Schurig J, Zweynert S, Bauer M, Vajkoczy P, Ringleb PA, Purrucker JC, Rizos T, Volkmann J, Muellges W, Kraft P, Schubert AL, Erbguth F, Nueckel M, Schellinger PD, Glahn J, Knappe UJ, Fink GR, Dohmen C, Stetefeld H, Fisse AL, Minnerup J, Hagemann G, Rakers F, Reichmann H, Schneider H, Wöpking S, Ludolph AC, Stösser S, Neugebauer H, Röther J, Michels P, Schwarz M, Reimann G, Bäzner H, Schwert H, Classen J, Michalski D, Grau A, Palm F, Urbanek C, Wöhrle JC, Alshammari F, Horn M, Bahner D, Witte OW, Guenther A, Hamann GF, Lücking H, Dörfler A, Schwab S, Huttner HB. Heparin for prophylaxis of venous thromboembolism in intracerebral haemorrhage. J Neurol Neurosurg Psychiatry. 2019;90:783-791. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |