Published online Oct 26, 2021. doi: 10.12998/wjcc.v9.i30.9310
Peer-review started: July 10, 2021
First decision: July 26, 2021
Revised: August 8, 2021
Accepted: September 8, 2021
Article in press: September 8, 2021
Published online: October 26, 2021
Processing time: 103 Days and 5.3 Hours
While tuberculosis (TB) itself is a common disease, isolated TB of the liver is a rare entity. Tubercular involvement of the liver is more commonly a part of a disseminated disease of the hepatic parenchyma. In contrast, isolated hepatic TB spread through the portal vein from the gastrointestinal tract is seldom encountered in clinical practice, with only a few sporadic cases and short series available in the current literature. Vascular complications, such as portal vein thrombosis (PVT), have rarely been reported previously.
A 22-year-old man was hospitalized with complaints of a 3-mo history of fever and weight loss of approximately 10 kg. He had a 10-year hepatitis B virus (HBV) infection in his medical history. Contrast-enhanced computed tomography (CECT) confirmed hepatosplenomegaly, with hypodensity of the right lobe of the liver and 2.1 cm thrombosis of the right branch of the portal vein. A liver biopsy showed epithelioid granulomas with a background of caseating necrosis. Ziehl-Nelson staining showed acid-fast bacilli within the granulomas. The patient was diagnosed with isolated hepatic TB with PVT. Anti-TB therapy (ATT), including isoniazid, rifapentine, ethambutol, and pyrazinamide, was administered. Along with ATT, the patient was treated with entecavir as an antiviral medication against HBV and dabigatran as an anticoagulant. He remained asymptomatic, and follow-up sonography of the abdomen at 4 mo showed complete resolution of the PVT.
Upon diagnosis of hepatic TB associated with PVT and HBV coinfection, ATT and anticoagulants should be initiated to prevent subsequent portal hypertension. Antiviral therapy against HBV should also be administered to prevent severe hepatic injury.
Core Tip: Tubercular involvement of the liver is more commonly a part of a disseminated disease of the hepatic parenchyma. In contrast, isolated hepatic tuberculosis (TB) spread through the portal vein from the gastrointestinal tract is seldom encountered in clinical practice. Vascular complications, such as portal vein thrombosis, have rarely been reported previously. Patients with hepatitis B virus (HBV) and TB coinfection needing anti-TB therapy may have more risks for hepatic injury. We hereby describe a case with an unusual appearance of local hepatic TB associated with portal vein thrombosis and HBV coinfection who was successfully treated with anti-TB therapy, anti-coagulants, and antiviral treatment against HBV.
- Citation: Zheng SM, Lin N, Tang SH, Yang JY, Wang HQ, Luo SL, Zhang Y, Mu D. Isolated hepatic tuberculosis associated with portal vein thrombosis and hepatitis B virus coinfection: A case report and review of the literature. World J Clin Cases 2021; 9(30): 9310-9319
- URL: https://www.wjgnet.com/2307-8960/full/v9/i30/9310.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i30.9310
Mycobacterium tuberculosis usually infects the lungs, resulting in pulmonary tuberculosis (TB), but it can infect almost any organ in the body, causing extrapulmonary infection. Hepatic TB is an extrapulmonary manifestation of an active infection. Hepatic TB can be broadly divided into two types, the more common miliary type and the less common local type, each of which can be further divided into diffuse and nodular subtypes. The miliary or disseminated type characterized by diffuse hepatic involvement is caused by the hematogenous spread of the Mycobacterium tuberculosis by the hepatic artery, generally from the lungs. Such patients usually show evidence of miliary pulmonary TB, as well[1]. Isolated or local hepatic TB is the rarest form of local hepatic TB, which occurs through Mycobacterium tuberculosis spread through the portal vein from the gastrointestinal tract[2,3]. Among reported hepatic TB cases, the miliary form accounts for 79%, while local hepatic TB accounts for 21%[4]. Biliary TB is another form of TB in the liver and is considered rare[2,5].
Local hepatic TB associated with portal vein thrombosis (PVT) and hepatitis B virus (HBV) infection poses challenges in both diagnosis and treatment and has not, to our knowledge, been reported previously. We hereby describe a case with an unusual appearance of local hepatic TB associated with PVT and HBV coinfection.
A 22-year-old man was admitted to our hospital with a 3-mo history of fever and weight loss of approximately 10 kg.
The patient’s symptoms started 3 mo ago with chronic fever and progressive weight loss.
The patient had a 10-year HBV infection in his medical history. He had never taken antiviral treatment against HBV.
This patient had no special personal and family history.
On examination, the patient’s temperature was 39.5 °C, heart rate was 94 beats per minute, respiratory rate was 17 breaths per minute, and blood pressure was 100/70 mmHg, without any other pathological signs.
A laboratory workup revealed a hepatic injury pattern, with alanine aminotransferase of 137 IU/L (normal range, 9-60 IU/L), aspartate aminotransferase of 95 IU/L (15-45 IU/L), alkaline phosphatase of 290 IU/L (45-125 IU/L), and γ-glutamyltransferase of 172 IU/L (10-60 IU/L). The hepatitis panel showed positivity for hepatitis B surface antigen (HBsAg), hepatitis B e antigen (HBeAg), and hepatitis B core antibody. HBV-DNA level was 3.496 × 107 IU/mL (< 2.0 × 102 IU/mL). C-reactive protein was 46 mg/L (0-3 mg/L). Procalcitonin was 2.37 ng/mL (0-0.05 ng/mL). The purified protein derivative skin test, autoimmune, HIV, and ESR tests were within normal limits.
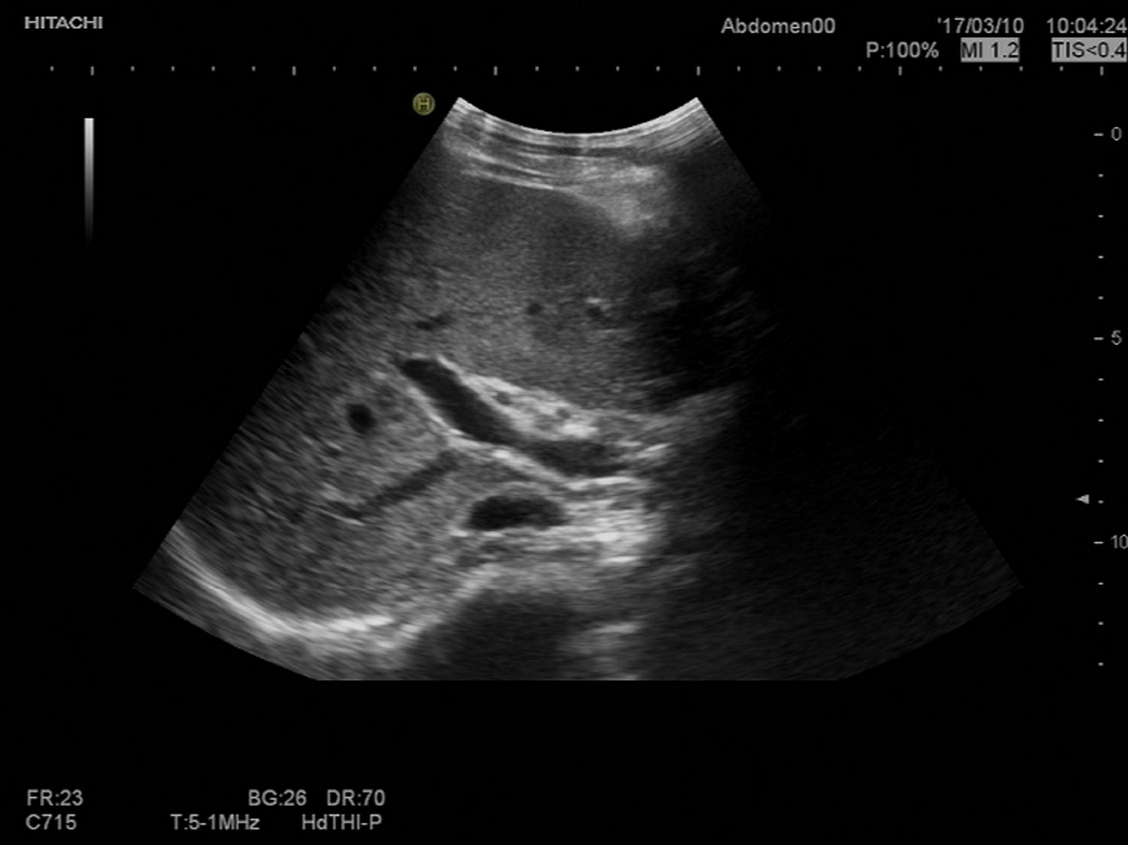
Abdominal ultrasound showed that the liver was enlarged, with a span of 15.2 cm with no other focal lesions. The spleen was enlarged with a span of 7.3 cm. The right branch of the portal vein showed evidence of a 2.1 cm thrombosis (Figure 1). All other abdominal viscera appeared normal with no free fluid.
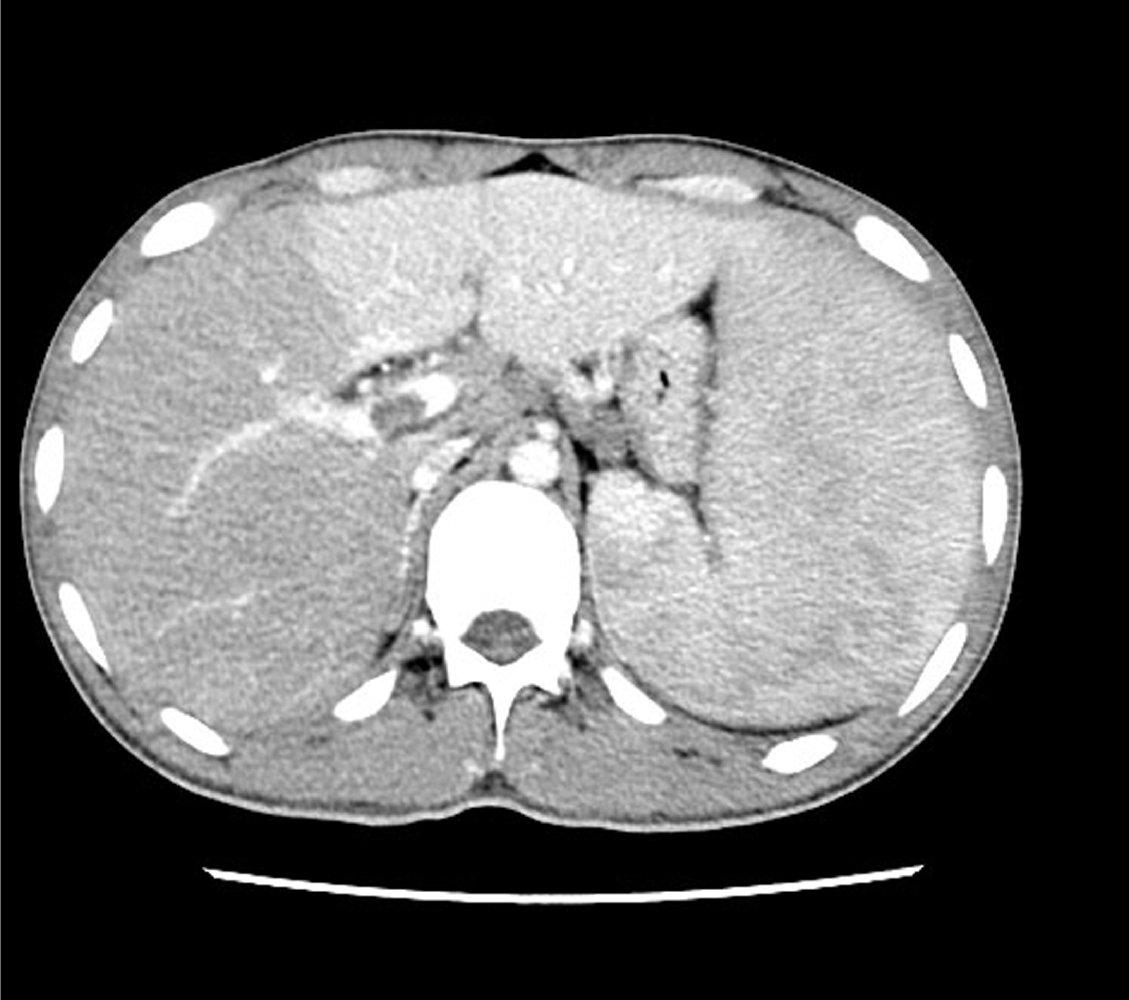
Contrast-enhanced computed tomography (CECT) of the thorax and abdomen was then performed to further assess the burden of the disease in the chest and to evaluate the portal vein. CECT confirmed hepatosplenomegaly, with hypodensity of the right lobe of the liver; thrombosis of the right branch of the portal vein (Figure 2); and enlargement of several hepatic portal, retroperitoneal, and para-aortic lymph nodes.
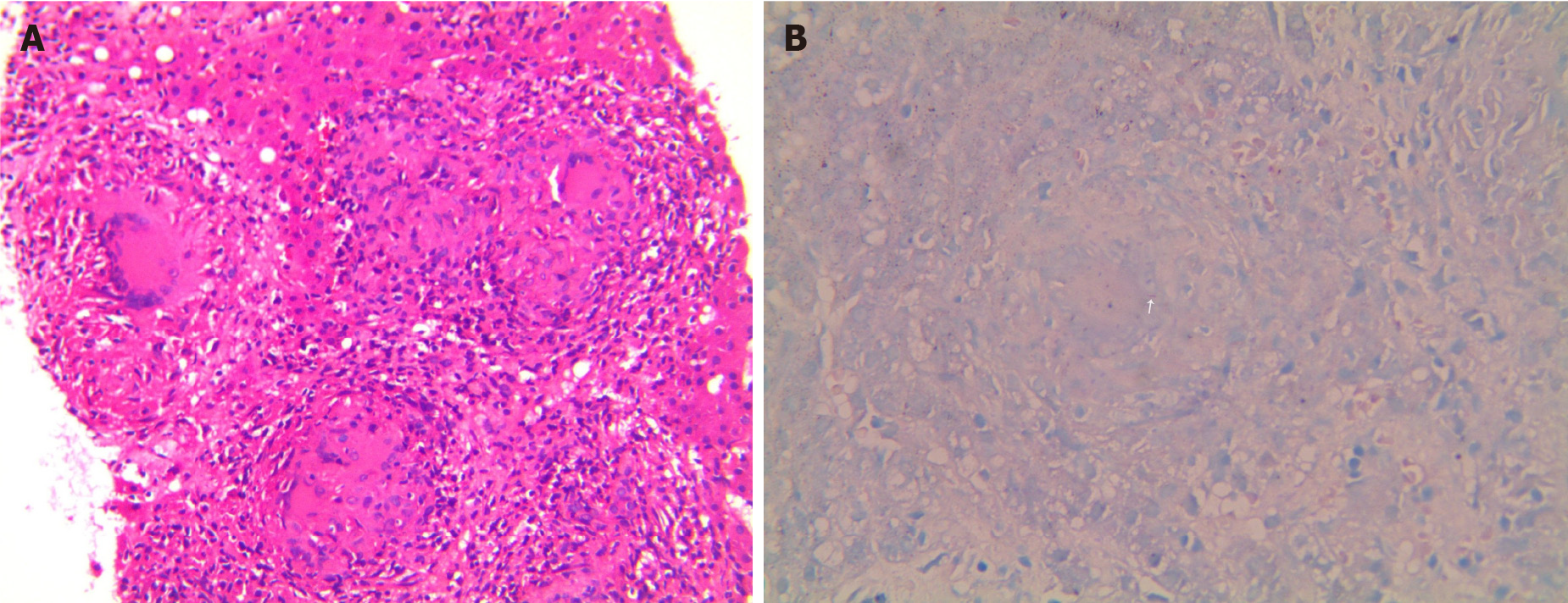
A bone marrow smear and biopsy were attempted with the result of slightly decreased whole cell counts. The subsequent esophagogastroduodenoscopy and colonoscopy results were normal. Although the possibility of viral, bacterial, and parasitic infestations was clinically considered, it was kept at a low priority due to the lack of significant results of laboratory examinations. Ultrasound-guided percutaneous liver biopsy was then performed. Histology of the liver biopsy showed entirely effaced architecture of hepatic parenchymal and portal areas by inflammation and necrosis. Central caseating necrosis was surrounded by lymphocytes, multinucleate giant cells, and epithelioid macrophages (Figure 3A). This revealed epithelioid granulomas with a background of caseating necrosis. Ziehl-Nelson staining showed acid-fast bacilli within the granulomas (Figure 3B).
Based on the histological, bacteriological, and laboratory findings, a final diagnosis of the present case was isolated hepatic TB associated with PVT and HBV coinfection.
Anti-TB medication, including isoniazid, rifapentine, ethambutol, and pyrazinamide, was administered. Along with ATT, the patient was treated with entecavir as an antiviral medication and dabigatran as an anticoagulant. One week after ATT, he was discharged from the hospital free of symptoms.
The patient had an uneventful clinical course. At 4 wk of therapy, repeat sonography of the abdomen showed regression of hepatosplenomegaly. At 4 mo of therapy, the sonography showed complete resolution of the PVT (Figure 4), so dabigatran was discontinued. ATT and antiviral therapies were administered for a total of 9 mo. The HBV-DNA level was under detection with normal liver function at the 2-year follow-up after therapy.
Although the prevalence of TB decreased quickly worldwide after the widespread use of anti-TB drugs in the 1940s, there has been a global resurgence of TB since the acquired immune deficiency syndrome epidemic of the 1980s, the development of multidrug-resistant TB strains, and an increased number of immunocompromised patients[6-8]. The global distribution of reported hepatic TB cases is concentrated in Sub-Saharan Africa and Southeast Asia, which is similar to the distribution of pulmonary TB[4]. A conservative estimate of the incidence of hepatic TB can be made using data from studies conducted by Essop et al[9] and Tai et al[10], who found hepatic TB in approximately 1% of all active TB cases.
Hematogenous dissemination via the hepatic artery from a pulmonary focus is the most common etiology of hepatic TB[2,5]. Other extrapulmonary sites, such as abdominal lymph nodes, may be a rare source of miliary dissemination. In local hepatic TB, dissemination primarily occurs via the portal vein from a focus in the gastrointestinal tract. Miliary hepatic TB is characterized by diffuse seeding of the liver, with tubercles less than 2 mm in size situated in lobules of the liver. Local hepatic TB is typically characterized by tubercles greater than 2 mm in diameter situated near the portal triad region[2]. Local hepatic TB tends to cause more hepatocellular damage than miliary hepatic TB[2].
Hepatic TB most commonly affects people in the 11 to 50-year-old age group, with the peak incidence of disease in the second decade of life. Isolated hepatic TB is more common in the fourth to sixth decades of life[12-14]. The disease has a 2:1 male preponderance[15]. The clinical features of hepatic TB are nonspecific, which often delays diagnosis. Analysis of hepatic TB case series revealed that the most common signs or symptoms were hepatomegaly (80%), fever (67%), respiratory symptoms (66%), abdominal pain (59.5%), and weight loss (57.5%)[4]. The less common signs included splenomegaly (30%), ascites (23%), and jaundice (20%)[4]. Local hepatic TB and miliary TB may differ in clinical presentation. Miliary hepatic TB may present with acute respiratory symptoms, such as a cough, with or without sputum production[2,10,15], while local hepatic TB may present primarily as diffuse abdominal pain. Jaundice is also more common in cases of local hepatic TB and biliary TB.
The imaging manifestation of tubercular hepatic disease can be wide ranging but can be broadly categorized into miliary patterns, nodular tuberculosis with serohepatic variants, and tubercular cholangitis. Ultrasound and CT scans are generally the most widely available and first imaging tests to be obtained, but they both lack diagnostic specificity. On CT, miliary lesions appear as microabscesses in the form of multiple small foci and may exhibit minimal peripheral enhancement following intravenous contrast administration[16,17]. In contrast, local hepatic TB generally appears on CT as one large solitary nodule or multiple variable-sized hepatic nodules. Hepatic TB may also reveal hepatomegaly without nodular intrahepatic lesions, or it may reveal abdominal lymphadenopathy with peripheral lymph node enhancement and/or calcifications[18-20]. Sonographically, hepatic TB lesions may appear hypoechoic to isoechoic relative to the background parenchyma; however, in rare instances, a hyperechoic pattern may be demonstrated[12,21-25]. Since the imaging appearances can be quite variable depending on the stage of the hepatic disease, it may often be difficult to distinguish hepatic TB from the more common neoplasm, other granulomatous diseases, vascular disorders, viral hepatitis, and systemic infections[26,27]. Isolated TB of the liver is a rare entity, in which vascular complications, such as PVT and subsequent portal hypertension, have rarely been reported[28]. The present case demonstrates the difficulty of diagnosis despite a complete investigation due to its nonspecific clinical and imaging findings.
The fact that isolated liver TB does not produce characteristic symptoms, clinical signs, or imaging appearances, makes diagnosis challenging. Histopathological or bacteriological confirmation is often required to reach diagnosis. A liver biopsy is recommended in any person with clinical, laboratory, and radiographic suspicion of hepatic TB. These may include but are not limited to hepatosplenomegaly of unknown origin, fever of unknown origin, and abnormal liver enzymes[29,30]. Liver biopsies should be sent for both histological and microbiological evaluation in such cases. The characteristic histological feature of both miliary and local forms of hepatic TB is the granuloma. Histological evidence of caseating granulomas had a median sensitivity of 68% among hepatic TB case series[4]. In TB endemic regions, the presence of a hepatic caseating granuloma on liver biopsy should suggest a TB etiology and may warrant a course of ATT. Liver biopsies should be sent for acid-fast bacilli (AFB) smear testing as well as mycobacterial culture. AFB smears have a median sensitivity of 25% among hepatic TB case series[4]. Mycobacterial culture provides specific evidence for hepatic TB, but the sensitivity has been reported to be less than 10%[31]. Since AFB smears and cultures have a low sensitivity, PCR assays have been recommended for diagnosing hepatic TB[31,32]. In a systemic review of 14 hepatic TB case series, Hickey et al[4] reported that PCR had a median sensitivity of 86% among hepatic TB cases. In another series of 43 liver biopsies with granulomas, Diaz et al[31] used PCR to amplify the IS6110 insertion sequence to detect TB and showed that PCR had a sensitivity of 53%, specificity of 96%, and positive and negative predictive values of 90% and 76%, respectively. These preliminary studies suggest that PCR may be more sensitive and specific for the diagnosis of TB than AFB smear or culture. This faster method for the diagnosis of hepatic TB may promote early detection and treatment.
It has been reported that the lifetime risk of PVT in the general population is 1%[33]. Venous thrombosis is a known but rare complication of pulmonary and extrapulmonary tuberculosis, occurring in 1.5%–3.4% of patients[34]. Intraabdominal TB, such as peritoneum, bowel, lymph node, and solid organ involvements, may be associated with PVT (Table 1)[28,35-41]. All the three parts of Virchow’s triad (hypercoagulability, venous stasis, and endothelial dysfunction) may play a role in the pathogenesis of thromboembolic complications in TB. It has been postulated that contiguous spread of inflammation and granulomas in the vessel wall with subintimal fibrosis may be other risk factors that contribute to PVT. Spontaneous resolution of the thrombosis did occur in some cases, but the frequency of partial or complete recanalization seemed to be higher in patients treated with anticoagulants. Based on a previous study, anticoagulants may be associated with recanalization of both acute and chronic thrombosis[42]. Low molecular weight heparins and vitamin K antagonists have long been the preferred anticoagulants in noncirrhotic PVT; however, direct oral anticoagulants are coming into increasing clinical use and have been shown to be safe and effective in retrospective studies[43,44]. Timely initiation of anticoagulants and ATT may lead to complete resolution of the PVT and thus prevent subsequent portal hypertension and complications, including ascites and life-threatening bleeding from varices.
| Ref. | Number | Age/Sex | Location of TB involvement | Site of thrombosis | Therapy | Recanalization |
| Venkatesh et al[28], 2005 | 1 | 31/F | Liver; ileo-cecum | PVT; PH | ATT | Not mentioned |
| Bhalla et al[35], 2010 | 6/183 | 27/M | Peri-pancreatic, coeliac axis adenopathy; cecum | PVT; SVT; SMVT | ATT | Persistent thrombosis |
| 36/M | Peri-pancreatic adenopathy; duodenum; lung | PVT | ATT | Lost to follow-up | ||
| 32/M | Duodenum | PVT | ATT | Recanalization | ||
| 25/F | Peri-pancreatic adenopathy; peritoneum; lung | PVT | ATT | Died of disseminated disease | ||
| 35/F | Peri-pancreatic, porta, left para-aortic adenopathy | PVT; PC | ATT | Persistent PC | ||
| 8/F | Peri-pancreatic, porta, left para-aortic adenopathy; mediastinum | PVT | ATT | Persistent PC | ||
| Ozşeker et al[36], 2012 | 1 | 43/M | Peritoneum | PVT; PC | ATT | Not mentioned |
| Ruttenberg et al[37], 1991 | 1/2 | 42/F | Pancreas | PVT; SVT; PH | ATT | Not mentioned |
| Liew et al[38],2011 | 1 | 26/F | Periporta TB | PVT; PC; PH | ATT | Not mentioned |
| Wariyapperuma et al[39], 2015 | 1 | 35/F | Peritoneum | PVT; PC | ATT; VKA | Not mentioned |
| Kumar et al[40], 2013 | 1 | 2/Not mentioned | Abdominal lymph nodes | PVT; PC | ATT | Persistent PC |
| Elleuch et al[41], 2020 | 1 | 60/M | Peritoneum | PVT; PC | ATT; VKA | Recanalization |
HBV infection is another serious global public health problem. It is estimated that 240 million people worldwide are chronic carriers of HBsAg[45]. The prevalence of HBV infection is highly heterogeneous throughout the world, with an intermediate to high prevalence in the Asia-Pacific region, representing three-quarters of chronic HBV-positive subjects worldwide. HBV infection has been reported to be a significant risk factor for hepatotoxicity related to ATT[46]. A higher proportion of inactive HBsAg carriers who received ATT evidenced moderate to severe drug-induced liver injury when compared with control subjects (8% vs 2%)[47]. Liver injury was also more severe by histological assessment in HBV carriers than in non-carriers[46]. Further research indicated that hepatotoxicity related to ATT was more common in HBV-positive patients who were seropositive for HBeAg than among those who were seronegative for HBeAg[48]. Most episodes of liver dysfunction are usually preceded by an increase in HBV-DNA levels[46]. To date, there have not been guidelines for antiviral therapy against HBV in active TB and inactive HBV coinfected patients needing ATT. Antiviral agents active against HBV have been shown to suppress HBV replication, prevent progression to cirrhosis, and reduce the risk of hepatocellular carcinoma and liver-related deaths[45]. Therefore, a case can be made for decreasing viral load using antiviral therapy against HBV with high potency, high genetic barrier drugs, such as entecavir or tenofovir, in patients with HBV infection needing ATT to prevent the development of liver dysfunction.
The incidence of TB has likely increased with the development of multidrug-resistant TB strains and an increased number of immunocompromised patients. Isolated hepatic TB poses diagnostic challenges due to its largely nonspecific clinical and imaging presentations. Liver biopsy is recommended for a definite diagnosis. Timely ATT and anticoagulants may be effective in preventing portal hypertension and serious complications in patients with hepatic TB associated with PVT. Since HBV and TB coinfected patients needing ATT may have a higher risk of hepatic injury, antiviral medication against HBV with high potency and high genetic barrier drugs should be initiated upon diagnosis to prevent liver dysfunction.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and Hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Akbulut S, Mocan T S-Editor: Wang JL L-Editor: Wang TQ P-Editor: Wu RR
| 1. | Ghossein RA, Ross DG, Salomon RN, Rabson AR. Rapid detection and species identification of mycobacteria in paraffin-embedded tissues by polymerase chain reaction. Diagn Mol Pathol. 1992;1:185-191. [PubMed] |
| 2. | Chien RN, Lin PY, Liaw YF. Hepatic tuberculosis: comparison of miliary and local form. Infection. 1995;23:5-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 45] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 3. | Culafic D, Boricic I, Vojinovic-Culafic V, Zdrnja M. Hepatic tuberculomas. A case report. Rom J Gastroenterol. 2005;14:71-74. [PubMed] |
| 4. | Hickey AJ, Gounder L, Moosa MY, Drain PK. A systematic review of hepatic tuberculosis with considerations in human immunodeficiency virus co-infection. BMC Infect Dis. 2015;15:209. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 68] [Cited by in RCA: 83] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 5. | Chong VH, Lim KS. Hepatobiliary tuberculosis. Singapore Med J. 2010;51:744-751. [PubMed] |
| 6. | Dye C, Scheele S, Dolin P, Pathania V, Raviglione MC. Consensus statement. Global burden of tuberculosis: estimated incidence, prevalence, and mortality by country. WHO Global Surveillance and Monitoring Project. JAMA. 1999;282:677-686. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1956] [Cited by in RCA: 1886] [Article Influence: 72.5] [Reference Citation Analysis (0)] |
| 7. | Valadas E, Antunes F. Tuberculosis, a re-emergent disease. Eur J Radiol. 2005;55:154-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 31] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 8. | WHO global tuberculosis control report 2010. Summary. Cent Eur J Public Health. 2010;18:237. [PubMed] |
| 9. | Essop AR, Posen JA, Hodkinson JH, Segal I. Tuberculosis hepatitis: a clinical review of 96 cases. Q J Med. 1984;53:465-477. [PubMed] |
| 10. | Tai WC, Kuo CM, Lee CH, Chuah SK, Huang CC, Hu TH, Wang JH, Chang KC, Tseng PL, Changchien CS, Lee CM. Liver tuberculosis in Southern Taiwan: 15-years clinical experience. J Intern Med Taiwan. 2008;19:410-417. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Chan HS, Pang J. Isolated giant tuberculomata of the liver detected by computed tomography. Gastrointest Radiol. 1989;14:305-307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 26] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 12. | Brauner M, Buffard MD, Jeantils V, Legrand I, Gotheil C. Sonography and computed tomography of macroscopic tuberculosis of the liver. J Clin Ultrasound. 1989;17:563-568. [PubMed] [DOI] [Full Text] |
| 13. | Epstein BM, Leibowitz CB. Ultrasonographic and computed tomographic appearance of focal tuberculosis of the liver. A case report. S Afr Med J. 1987;71:461-462. [PubMed] |
| 14. | Alvarez SZ, Carpio R. Hepatobiliary tuberculosis. Dig Dis Sci. 1983;28:193-200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 89] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 15. | Kok KY, Yapp SK. Isolated hepatic tuberculosis: report of five cases and review of the literature. J Hepatobiliary Pancreat Surg. 1999;6:195-198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 35] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 16. | Kakkar C, Polnaya AM, Koteshwara P, Smiti S, Rajagopal KV, Arora A. Hepatic tuberculosis: a multimodality imaging review. Insights Imaging. 2015;6:647-658. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 50] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 17. | Harisinghani MG, McLoud TC, Shepard JA, Ko JP, Shroff MM, Mueller PR. Tuberculosis from head to toe. Radiographics. 2000;20:449-70; quiz 528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 233] [Cited by in RCA: 188] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 18. | Mortelé KJ, Segatto E, Ros PR. The infected liver: radiologic-pathologic correlation. Radiographics. 2004;24:937-955. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 277] [Cited by in RCA: 203] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 19. | Yu RS, Zhang SZ, Wu JJ, Li RF. Imaging diagnosis of 12 patients with hepatic tuberculosis. World J Gastroenterol. 2004;10:1639-1642. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 78] [Cited by in RCA: 80] [Article Influence: 3.8] [Reference Citation Analysis (1)] |
| 20. | Mert A, Ozaras R, Tabak F, Ozturk R, Bilir M. Localized hepatic tuberculosis. Eur J Intern Med. 2003;14:511-512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 34] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 21. | Tan TC, Cheung AY, Wan WY, Chen TC. Tuberculoma of the liver presenting as a hyperechoic mass on ultrasound. Br J Radiol. 1997;70:1293-1295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 26] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 22. | Kawamori Y, Matsui O, Kitagawa K, Kadoya M, Takashima T, Yamahana T. Macronodular tuberculoma of the liver: CT and MR findings. AJR Am J Roentgenol. 1992;158:311-313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 56] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 23. | Thoeni RF, Margulis AR. Gastrointestinal tuberculosis. Semin Roentgenol. 1979;14:283-294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 83] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 24. | Jain R, Sawhney S, Gupta RG, Acharya SK. Sonographic appearances and percutaneous management of primary tuberculous liver abscess. J Clin Ultrasound. 1999;27:159-163. [PubMed] [DOI] [Full Text] |
| 25. | Chen HC, Chao YC, Shyu RY, Hsieh TY. Isolated tuberculous liver abscesses with multiple hyperechoic masses on ultrasound: a case report and review of the literature. Liver Int. 2003;23:346-350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 37] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 26. | Arora R, Sharma A, Bhowate P, Bansal VK, Guleria S, Dinda AK. Hepatic tuberculosis mimicking Klatskin tumor: a diagnostic dilemma. Indian J Pathol Microbiol. 2008;51:382-385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 27. | Vimalraj V, Jyotibasu D, Rajendran S, Ravichandran P, Jeswanth S, Balachandar TG, Kannan DG, Surendran R. Macronodular hepatic tuberculosis necessitating hepatic resection: a diagnostic conundrum. Can J Surg. 2007;50:E7-E8. [PubMed] |
| 28. | Venkatesh SK, Tan LK, Siew EP, Putti TC. Macronodular hepatic tuberculosis associated with portal vein thrombosis and portal hypertension. Australas Radiol. 2005;49:322-324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 29. | Grant A, Neuberger J. Guidelines on the use of liver biopsy in clinical practice. British Society of Gastroenterology. Gut. 1999;45 Suppl 4:IV1-IV11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 186] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 30. | Ferrari TC, Couto CM, Vilaça TS, Xavier MA. Localized hepatic tuberculosis presenting as fever of unknown origin. Braz J Infect Dis. 2006;10:364-367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 31. | Diaz ML, Herrera T, Lopez-Vidal Y, Calva JJ, Hernandez R, Palacios GR, Sada E. Polymerase chain reaction for the detection of Mycobacterium tuberculosis DNA in tissue and assessment of its utility in the diagnosis of hepatic granulomas. J Lab Clin Med. 1996;127:359-363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 58] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 32. | Alcantara-Payawal DE, Matsumura M, Shiratori Y, Okudaira T, Gonzalez R, Lopez RA, Sollano JD, Omata M. Direct detection of Mycobacterium tuberculosis using polymerase chain reaction assay among patients with hepatic granuloma. J Hepatol. 1997;27:620-627. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 33] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 33. | Ogren M, Bergqvist D, Björck M, Acosta S, Eriksson H, Sternby NH. Portal vein thrombosis: prevalence, patient characteristics and lifetime risk: a population study based on 23,796 consecutive autopsies. World J Gastroenterol. 2006;12:2115-2119. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 310] [Cited by in RCA: 323] [Article Influence: 17.0] [Reference Citation Analysis (2)] |
| 34. | Gupta A, Mrigpuri P, Faye A, Bandyopadhyay D, Singla R. Pulmonary tuberculosis - An emerging risk factor for venous thromboembolism: A case series and review of literature. Lung India. 2017;34:65-69. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 35. | Bhalla AS, Hari S, Chandrashekhara SH, Sinha A, Makhariab G, Gupta R. Tuberculose ganglionnaire abdominale et hypertension portale. Gastroentérologie Clinique et Biologique. 2010;34:696-701. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 36. | Ozşeker B, Ozşeker HS, Kav T, Shorbagi A, Karakoç D, Bayraktar Y. Abdominal tuberculosis leading to portal vein thrombosis, mimicking peritoneal carcinomatosis and liver cirrhosis. Acta Clin Belg. 2012;67:137-139. [PubMed] |
| 37. | Ruttenberg D, Graham S, Burns D, Solomon D, Bornman P. Abdominal tuberculosis--a cause of portal vein thrombosis and portal hypertension. Dig Dis Sci. 1991;36:112-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 31] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 38. | Liew E, Sutherland T, Slavin J, Darby J. Isolated periportal tuberculosis causing portal vein thrombosis. J Ultrasound Med. 2011;30:1599-1601. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 39. | Wariyapperuma UM, Jayasundera CI. Peritoneal tuberculosis presenting with portal vein thrombosis and transudative Ascites - a diagnostic dilemma: case report. BMC Infect Dis. 2015;15:394. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 40. | Kumar J, Chowdhury V, Rajeshwari K. Portal vein thrombosis resulting from tubercular lymphadenitis: an unusual scenario. Arab J Gastroenterol. 2013;14:85-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 41. | Elleuch N, Sabbek A, Hammami A, Ksiaa M, Jmaa A. Primary peritoneal tuberculosis, a forgotten etiology of portal vein thrombosis. J Med Vasc. 2020;45:96-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 42. | Intagliata NM, Caldwell SH, Tripodi A. Diagnosis, Development, and Treatment of Portal Vein Thrombosis in Patients With and Without Cirrhosis. Gastroenterology. 2019;156:1582-1599.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 247] [Article Influence: 41.2] [Reference Citation Analysis (0)] |
| 43. | Naymagon L, Tremblay D, Zubizarreta N, Moshier E, Troy K, Schiano T, Mascarenhas J. The efficacy and safety of direct oral anticoagulants in noncirrhotic portal vein thrombosis. Blood Adv. 2020;4:655-666. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 65] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 44. | Nery F, Valadares D, Morais S, Gomes MT, De Gottardi A. Efficacy and Safety of Direct-Acting Oral Anticoagulants Use in Acute Portal Vein Thrombosis Unrelated to Cirrhosis. Gastroenterology Res. 2017;10:141-143. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 33] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 45. | WHO Guidelines Review Committee. Guidelines for the Prevention, Care and Treatment of Persons with Chronic Hepatitis B Infection. Geneva: World Health Organization, 2015. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 46. | Wong WM, Wu PC, Yuen MF, Cheng CC, Yew WW, Wong PC, Tam CM, Leung CC, Lai CL. Antituberculosis drug-related liver dysfunction in chronic hepatitis B infection. Hepatology. 2000;31:201-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 149] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 47. | Lee BH, Koh WJ, Choi MS, Suh GY, Chung MP, Kim H, Kwon OJ. Inactive hepatitis B surface antigen carrier state and hepatotoxicity during antituberculosis chemotherapy. Chest. 2005;127:1304-1311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 38] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 48. | Patel PA, Voigt MD. Prevalence and interaction of hepatitis B and latent tuberculosis in Vietnamese immigrants to the United States. Am J Gastroenterol. 2002;97:1198-1203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 46] [Article Influence: 2.0] [Reference Citation Analysis (0)] |