Published online Oct 16, 2021. doi: 10.12998/wjcc.v9.i29.8946
Peer-review started: July 10, 2021
First decision: July 26, 2021
Revised: July 27, 2021
Accepted: August 18, 2021
Article in press: August 18, 2021
Published online: October 16, 2021
Processing time: 97 Days and 0.9 Hours
Autonomic dysreflexia (AD) can be a life-threatening condition in patients with spinal cord injury. It is important to prevent bladder overdistension in these patients as it may trigger AD. Sensation-dependent bladder emptying (SDBE), as a method of bladder management, improves the quality of life and allows physiologic voiding. In this study, we report disruption of the SDBE habit after bladder overdistension leading to AD with chest pain.
A 47-year-old male with a diagnosis of C4 American Spinal Cord Injury Association impairment scale A had been emptying his bladder using the clean intermittent catheterization method with an itchy sensation in the nose as a sensory indication for a full bladder for 23 years, and the usual urine volume was about 300-400 mL. At the time of this study, the patient had delayed catheterization for approximately five hours. He developed severe abdominal pain and headache and had to visit the emergency room for bladder overdistension (800 mL) and a high systolic blood pressure (205 mmHg). After control of AD, a hypersensitive bladder was observed despite using anticholinergic agents. The sensation indicating bladder fullness changed from nose itching to pain in the abdomen and precordial area. Moreover, the volume of the painful bladder filling sensation became highly variable and was noted when the bladder urine volume exceeded only 100 mL. The patient refused intermittent clean catheterization. Finally, a cystostomy was performed, which relieved the symptoms.
Patients using physiologic feedback, such as SDBE, for bladder management are recommended to avoid bladder overdistension.
Core Tip: In this report, sensation-dependent bladder emptying (SDBE), which had been maintained for 23 years, was disrupted after bladder overdistension that led to autonomic dysreflexia (AD) in a patient with complete spinal cord injury (SCI). After the AD due to bladder overdistension, the bladder was oversensitive to even a small amount of urine, resulting in unbearable discomfort. Cystostomy was later performed. Patients using physiologic feedback, such as SDBE, for bladder management should follow a strict bladder emptying regimen. In addition, by considering the effect of AD on bladder filling sensation in this case, we provide additional information about the mechanism of AD and "discomplete SCI.”
- Citation: Yoon JY, Kim DS, Kim GW, Won YH, Park SH, Ko MH, Seo JH. Disruption of sensation-dependent bladder emptying due to bladder overdistension in a complete spinal cord injury: A case report. World J Clin Cases 2021; 9(29): 8946-8952
- URL: https://www.wjgnet.com/2307-8960/full/v9/i29/8946.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i29.8946
Neurogenic bladder is common in patients with spinal cord injury (SCI). Until recently, studies on the neurogenic bladder of patients with SCI, have been conducted in a search for the optimal treatment option. Because each patient's physical condition and methods of urination are different, a wider range of possible methods, both traditional and new, should be considered[1,2].
There are two main methods of bladder emptying in patients with SCI. First, time-dependent bladder emptying, by clean intermittent catheterization (CIC) at intervals of 4 to 6 h[3], is a commonly used method that facilitates bladder emptying. Second, sensation-dependent bladder emptying (SDBE) is a method in which bladder emptying is performed according to the filling sensation of the bladder using remaining sensory ability[4,5].
In SDBE, by reflecting the amount of urine produced according to fluid intake or temperature change, unnecessary catheterization can be avoided when the bladder is not adequately full. Overdistension can also be prevented even if unexpectedly rapid urine production occurs. In addition, there are reports that SDBE helps improve the quality of life[6] and reduces the probability of lower urinary tract infections[7].
In this case, we report disruption of bladder filling sensation after one event of autonomic dysreflexia (AD) due to bladder overdistension in a patient with complete SCI who had maintained SDBE for a long time.
A 47-year-old male presented to the emergency department with severe abdominal pain and headache.
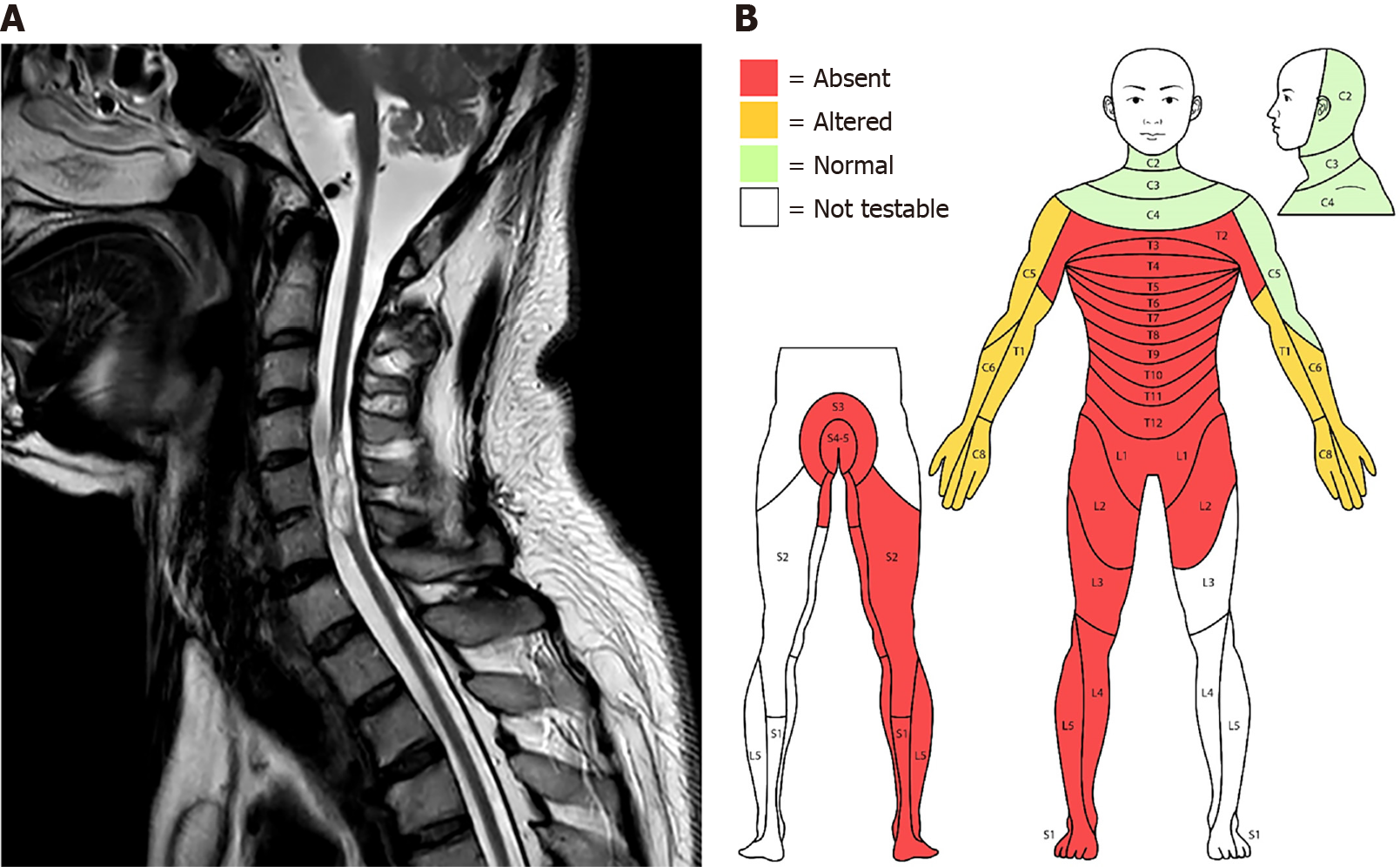
The patient was diagnosed with C4 American Spinal Cord Injury Association (ASIA) impairment scale A due to a car accident 23 years prior. The patient had a good motor grade at the C5 (elbow flexion) and C6 levels (wrist extensor), and zero grade at all levels below C6. For sensory grade, there was altered sensation below the C4 level on right side and C5 on left side, and no sensation below the T1 level (Figure 1). The patient had been using the CIC method for management of neurogenic bladder. He was able to sense bladder fullness by an itching sensation in the nose, at which time a caregiver would empty the bladder with CIC. This was maintained for approximately 23 years. The urine volume emptied by the bladder filling sense was usually 300-400 mL, and the discomfort of nasal itchiness was mild and measured two points on a visual analog scale (VAS). One day, the patient's catheterization was delayed for about five hours since the feeling of bladder fullness. Subsequently, he had to visit an emergency room for severe abdominal pain and headache.
At the time of the car accident with cervical cord injury 23 years earlier, the patient had a fracture of the left femur and underwent fixation surgery. Subsequently the patient underwent transfemoral amputation of the left lower extremity 7 years later due to malunion of the left distal femur fracture.
The patient had an unremarkable family history.
Bladder overdistension (800 mL) and high systolic blood pressure (SBP, 205 mmHg) were noted. An indwelling catheter was inserted, and blood pressure was controlled with a calcium channel blocker (nifedipine 80 mg/d) and nitrates (isosorbide dinitrate 2.5 mg).
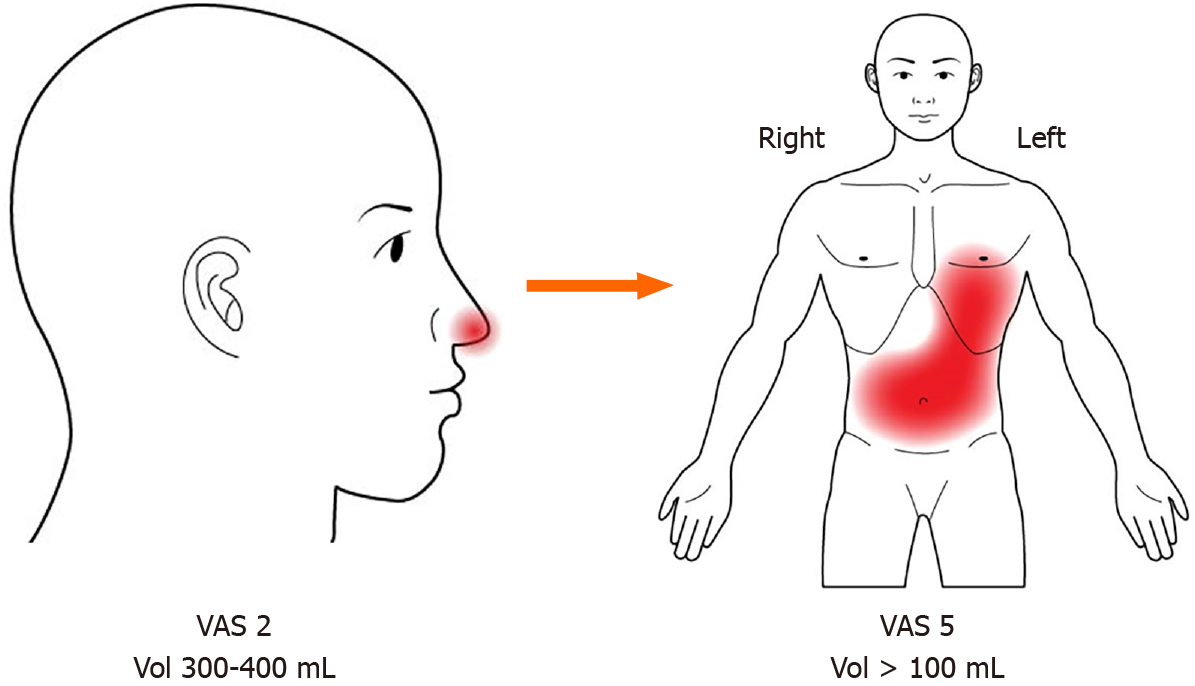
After the emergency treatment, the indwelling catheter was removed. Normal SDBE was expected as before the AD event. However, instead of the itching sensation in the nose, there was pain in the abdomen and precordial area (VAS 5), and the filling sensation did not result with a bladder volume of 300-400 mL as before. Instead, it fluctuated significantly between 100 and 400 mL (Figure 2). The patient wanted to restart the SDBE, but the change in the bladder filling sensation was very uncomfortable and unpredictable. Pain killers, including narcotics (tramadol, gabapentin, acetaminophen, celecoxib, and fentanyl), and anticholinergics (solifenacin 5 mg/d, propiverine 20 mg/d, and mirabegron 50 mg/d) did not relieve the pain or address the problem with the bladder volume. The patient underwent an urodynamic study (UDS) to examine the condition of the bladder.
ECG and cardiac echocardiogram were performed for the precordial area pain, but no abnormal findings were observed. Urinalysis did not show pyuria or hematuria. A UDS was performed and in comparison with the UDS findings before the AD event, bladder capacity was reduced, and hypersensitivity was observed even with the use of anticholinergics (Table 1).
Abdominal computed tomography (CT) was performed for abdominal pain, and chest CT was performed on the precordial area. No abnormal findings were observed. Cystoscopy was performed to rule out bladder injuries due to overdistension. The patient did not show any abnormal findings other than chronic cystitis. The patient’s cervical Magnetic resonance imaging (MRI) after the car accident is shown in Figure 1A.
The final diagnosis was complete SCI (C4 ASIA impairment scale A), with neurogenic bladder and persistent bladder hypersensitivity following bladder overdistension, which led to AD.
According to the results of UDS, additional anticholinergics (solifenacin 10 mg/d, propiverine 40 mg/d and mirabegron 50 mg/d) were administered, and lidocaine instillation was performed to reduce afferent noxious stimuli, but only minor improvement was observed. Timed bladder emptying with a Foley catheter at 1-2 h intervals was recommended at discharge.
At the three-month follow-up, the bladder filling sensation was still uncomfortable (VAS 5) and was unpredictable. The patient finally underwent cystostomy and the discomfort in the abdomen and precordial area improved slightly (VAS 5 to 4).
In this case report, a patient was diagnosed with C4 ASIA impairment scale A and maintained SDBE for approximately 23 years. An episode of AD with bladder overdistension caused detrimental changes to the bladder filling sensation (the position and intensity of the discomfort of the bladder filling changed; and fluctuation of the threshold of the bladder filling was observed), and SDBE could no longer be maintained. The patient wanted physiologic voiding through SDBE with CIC rather than surgical treatment, but ultimately cystostomy was performed.
In patients with complete SCI, SDBE is fundamentally possible under the premise that the patient is aware of bladder fullness[5]. A previous study using fMRI suggested that the perception of bladder fullness in patients with complete SCI is possible through extraspinal sensory pathways[8,9]. Furthermore, in recent studies, the concept of “discomplete SCI” has emerged. According to the ASIA impairment scale classification of SCI, the existence of a reproducible ambiguous sense can be referred to as sensory discomplete SCI, which might exist between ‘complete SCI’ and ‘incomplete SCI’. This has been proven in several studies using somatosensory evoked potential and fMRI[8,10,11]. These results provide a rationale for performing SDBE even in patients with complete SCI, such as this case.
AD is a clinical emergency that often occurs in patients with SCI above the T6 level. Among various symptoms, an increase in SBP is the most common, and clinical guidelines define it as an increase of more than 20-40 mmHg of SBP from the baseline[1,12]. Additionally, symptoms such as headache, sweating, flushing of skin, piloerection, nasal congestion, blurred vision, and anxiety may accompany elevated SBP. Headache and night sweats are observed in 88% of patients with AD[12]. Several studies have identified loss of supraspinal control, reorganization of sympathetic neurons, propriospinal plasticity, primary afferent sprouting, and peripheral adrenergic hypersensitivity as mechanisms for AD[12,13]. These mechanisms can be fundamentally interpreted as hypersensitivity and overactivity of the sympathetic spinal circuitry.
Therefore, it is necessary to elucidate how AD and bladder overdistension in this patient affected SDBE. It might be thought that the symptoms of AD are ‘directly’ reflected in the bladder filling sensation because the activation threshold of the circuit is decreased or residual activation occurs repeatedly after one AD episode. However, in this case, it is unlikely that AD directly affected the senses as there was no usual increase in SBP, even with the altered sense of bladder filling. It is unreasonable to think that the bladder filling sensation maintained for 23 years was caused by AD.
Therefore, we focused on how the AD and bladder overdistension events may have affected the sensory pathway of SDBE and proposed possible hypotheses. First, hyperactivation of the bladder afferent pathway, a common cause of AD, may affect SDBE. Bladder overdistension causes micro-damage to the bladder's urothelial cells (bladder barrier) and increases permeability, lowering the c-fiber activation threshold and consequently delivering more nociceptive stimulation[14]. As a result, the c-fibers can be activated even with a small amount of urine in the bladder. This was shown in the UDS findings of this case, as there was lower bladder capacity and hypersensitivity (Table 1). For the same reason, there is a possibility that the previous bladder fullness sensation may become perceived as pain (Figure 2; VAS 2 to 5), and fluctuations in the urine volume threshold for bladder fullness sensation may have occurred due to inconsistent activation of the c-fibers (Figure 2; bladder urine volume > 100 mL).
Second, the reorganization of several spinal pathways after AD affects the sensory pathways of SDBE. Reorganization of the sympathetic preganglionic neurons and propriospinal neurons is an established mechanism of AD[12,13], and it has been reported that activation of these pathways may affect sensory neurons[12,15]. This may be a clue to the changes of the body part reflecting bladder filling and the worsening of the discomfort level shown in this case (Figure 2; nose to precordial area & abdomen).
Third, as extraspinal sensory pathways, maladaptation of the vagus nerve after AD may affect SDBE. Kruhut et al[9] suggested that a sensory extraspinal pathway may develop following complete SCI, and the vagus nerve may play an important role in bladder re-innervation. The vagus nerve innervates the visceral sensory parts of the esophagus, lungs, heart, and most of the digestive system[16]. In this case, the fact that the sensory location reflecting bladder filling moved to the abdominal and precordial regions (Figure 2), which receive sensory innervation through the vagus nerve, supports this hypothesis. In addition, the vagus nerve has parasympathetic properties and is in a compensatory relationship with the sympathetic system. Overactivation or maladaptation of the vagal pathway might occur due to an overcompensatory response of the parasympathetic system to the overactivation of the sympathetic system such as in AD.
In a single episode of bladder overdistension causing AD, the pattern of SDBE, which had been well-maintained for many years, was disrupted in a patient with complete SCI. Therefore, we emphasize that avoidance of bladder overdistension in patients with SCI, especially with the use of SDBE.
The authors thank all members of the Department of Physical Medicine & Rehabilitation and Translational Research and Clinical Trials Center for Medical Devices, Jeonbuk National University Hospital.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mizuno H, Sikiric P S-Editor: Yan JP L-Editor: A P-Editor: Li X
| 1. | Krassioukov A, Warburton DE, Teasell R, Eng JJ; Spinal Cord Injury Rehabilitation Evidence Research Team. A systematic review of the management of autonomic dysreflexia after spinal cord injury. Arch Phys Med Rehabil. 2009;90:682-695. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 324] [Cited by in RCA: 246] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 2. | Wyndaele JJ. The management of neurogenic lower urinary tract dysfunction after spinal cord injury. Nat Rev Urol. 2016;13:705-714. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 57] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 3. | Goldmark E, Niver B, Ginsberg DA. Neurogenic bladder: from diagnosis to management. Curr Urol Rep. 2014;15:448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 4. | Ersoz M, Akyuz M. Bladder-filling sensation in patients with spinal cord injury and the potential for sensation-dependent bladder emptying. Spinal Cord. 2004;42:110-116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 5. | Shin JC, Chang WH, Jung TH, Yoo JH, Park SN. The determination of sensation-dependent bladder emptying time in patients with complete spinal cord injury above T11. Spinal Cord. 2008;46:210-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Adriaansen JJ, van Asbeck FW, Tepper M, Faber WX, Visser-Meily JM, de Kort LM, Post MW. Bladder-emptying methods, neurogenic lower urinary tract dysfunction and impact on quality of life in people with long-term spinal cord injury. J Spinal Cord Med. 2017;40:43-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 52] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 7. | Ersöz M, Sayılır S. Protective effect of preserved bladder-filling sensation on upper urinary tract in patients with spinal cord injury. Neurol Sci. 2014;35:1549-1552. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Finnerup NB, Gyldensted C, Fuglsang-Frederiksen A, Bach FW, Jensen TS. Sensory perception in complete spinal cord injury. Acta Neurol Scand. 2004;109:194-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 44] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 9. | Krhut J, Tintera J, Bilkova K, Holy P, Zachoval R, Zvara P, Blok B. Brain activity on fMRI associated with urinary bladder filling in patients with a complete spinal cord injury. Neurourol Urodyn. 2017;36:155-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 10. | Awad A, Levi R, Waller M, Westling G, Lindgren L, Eriksson J. Preserved somatosensory conduction in complete spinal cord injury: Discomplete SCI. Clin Neurophysiol. 2020;131:1059-1067. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 11. | Wrigley PJ, Siddall PJ, Gustin SM. New evidence for preserved somatosensory pathways in complete spinal cord injury: A fMRI study. Hum Brain Mapp. 2018;39:588-598. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 43] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 12. | Eldahan KC, Rabchevsky AG. Autonomic dysreflexia after spinal cord injury: Systemic pathophysiology and methods of management. Auton Neurosci. 2018;209:59-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 152] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 13. | Linsenmeyer TA, Gibbs K, Solinsky R. Autonomic Dysreflexia After Spinal Cord Injury: Beyond the Basics. Curr Physical Med Rehabilitat Rep. 2020;8:1-9. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 14. | Apodaca G, Kiss S, Ruiz W, Meyers S, Zeidel M, Birder L. Disruption of bladder epithelium barrier function after spinal cord injury. Am J Physiol Renal Physiol. 2003;284:F966-F976. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 90] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 15. | Schramm LP. Spinal sympathetic interneurons: their identification and roles after spinal cord injury. Prog Brain Res. 2006;152:27-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 36] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 16. | Craig AD. Interoception: the sense of the physiological condition of the body. Curr Opin Neurobiol. 2003;13:500-505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1605] [Cited by in RCA: 1634] [Article Influence: 74.3] [Reference Citation Analysis (0)] |