Published online Oct 16, 2021. doi: 10.12998/wjcc.v9.i29.8812
Peer-review started: March 5, 2021
First decision: May 11, 2021
Revised: May 24, 2021
Accepted: August 23, 2021
Article in press: August 23, 2021
Published online: October 16, 2021
Processing time: 224 Days and 5.6 Hours
The floating spleen refers to the spleen moving away from the normal anatomical position to other parts of the abdominal cavity.
In this report, we describe two cases of torsion of floating spleen, which were successfully treated by laparoscopic partial splenectomy and retroperitoneal fixation of the residual spleen. The clinical characteristics of previously reported cases are also discussed.
In conclusion, laparoscopic partial resection of splenic volvulus infarction and extraperitoneal fixation of residual spleen are safe and reliable.
Core Tip: The floating spleen refers to the spleen moving away from the normal anatomical position to other parts of the abdominal cavity. Because the spleen lacks the support of its inherent attached ligaments, it is easy to cause splenic pedicle torsion and splenic infarction, which in turn leads to inflammatory fibrosis and peripheral inflammatory adhesion. Clinical diagnosis is very difficult. Therefore, we describe two cases of torsion of floating spleen, which were successfully treated by laparoscopic partial splenectomy and retroperitoneal fixation of residual spleen. The clinical characteristics of previously reported cases are also discussed.
- Citation: Sun C, Li SL. Successful treatment of floating splenic volvulus: Two case reports and a literature review . World J Clin Cases 2021; 9(29): 8812-8819
- URL: https://www.wjgnet.com/2307-8960/full/v9/i29/8812.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i29.8812
The floating spleen refers to the spleen moving away from the normal anatomical position to other parts of the abdominal cavity[1]. The wandering spleen is mostly caused by congenital splenic pedicle or long perisplenic ligament, the absence of perisplenic ligaments, loose ligament, or weak abdominal muscle caused by swollen spleen traction[2]. Moreover, a case of floating spleen caused by Epstein Barr virus has been reported[3]. Because the spleen lacks the support of its inherent attached ligaments, it is easy to cause splenic pedicle torsion and splenic infarction, which in turn leads to inflammatory fibrosis and peripheral inflammatory adhesion[4]. Clinical diagnosis is very difficult, because most patients are asymptomatic and lack a suf
In this report, we describe two cases of torsion of floating spleen, which were successfully treated by laparoscopic partial splenectomy and retroperitoneal fixation of residual spleen. The clinical characteristics of previously reported cases are also discussed.
Case 1: A 3-year-old girl was hospitalized with intermittent abdominal pain for 1 mo and fever for 0.5 mo.
Case 2: A 4-year-old girl was hospitalized with intermittent abdominal pain for 2 years and worsening for more than 1 mo.
Case 1: A 3-year-old girl was hospitalized with intermittent abdominal pain for 1 mo and fever for 0.5 mo.
Case 2: A 4-year-old girl was hospitalized with intermittent abdominal pain for 2 years and worsening for more than 1 mo.
Case 1: Cardiopulmonary examination showed no abnormality. In the left middle and lower abdomen, a tenderness and immobility mass with the size of 3 cm × 5 cm × 6 cm was found.
Case 2: Cardiopulmonary examination showed no abnormality. There were tenderness and unfixed mass in the left middle abdomen, with tympanitic note when percussion.
Case 1: Computed tomography (CT) examination showed no normal spleen image in the left upper abdomen, and vortex-like abnormal density shadow in the left lower abdomen. The shadow was cystic solid mass with uneven density. Some solid components had obvious enhanced imaging, but most areas had no enhanced imaging. Furthermore, the splenic vein connected with superior mesenteric vein rotated about 3 wk.
Case 2: CT angiogram showed that the spleen increased in size and moved to the left middle abdomen. The splenic pedicle (splenic artery) spirally twists downward from the rear of the pancreatic tail.
Case 1: Initially diagnosed as torsion of wandering spleen and infarction.
Case 2: Diagnosed as wandering spleen with splenic torsion and splenic infarction.
Case 1: Laparoscopic exploration was performed. The child was placed in the supine position. An incision was made on the right side of the umbilicus, and a 5 mm Trocar was inserted to establish a CO2 pneumoperitoneum. After inserting a 30° 5 mm laparoscope, it was found that the wandering spleen was torsion and adhered to the left middle and lower anterior abdominal wall. Then two 5 mm trocars were inserted under and above the umbilicus. The adhesive tissue around the spleen was cut by ultrasonic scalpel. After freeing the spleen, the spleen pedicle was turned clockwise for nearly 3 wk, and then it was reset. Furthermore, most of the spleen was infarcted, and only one blood vessel from the splenocolonic ligament supplied part lower pole tissues. He-o-lok was used to clamp the infarcted splenic artery and vein after freeing the main splenic pedicles. The infarcted spleen and the spleen with blood supply were cut off with ultrasonic scalpel, and the remaining vital spleen was retained about 20%. The peritoneum was cut at the left upper abdomen near the diaphragmatic attachment, and the lateral retroperitoneal space was separated. The residual spleen was put into this space, and the peritoneum was sutured. Finally, the fascia of abdominal wall between umbilicus and Trocar was cut, and the incision was expanded to 2 cm. Most of the resected infracted splenic tissues were pulled to the incision and taken them out after dividing into blocks. The operation lasted 90 min, with 10 mL bleeding during the operation, and the remaining vital spleen tissue about 3 cm × 2.5 cm × 2.5 cm in size.
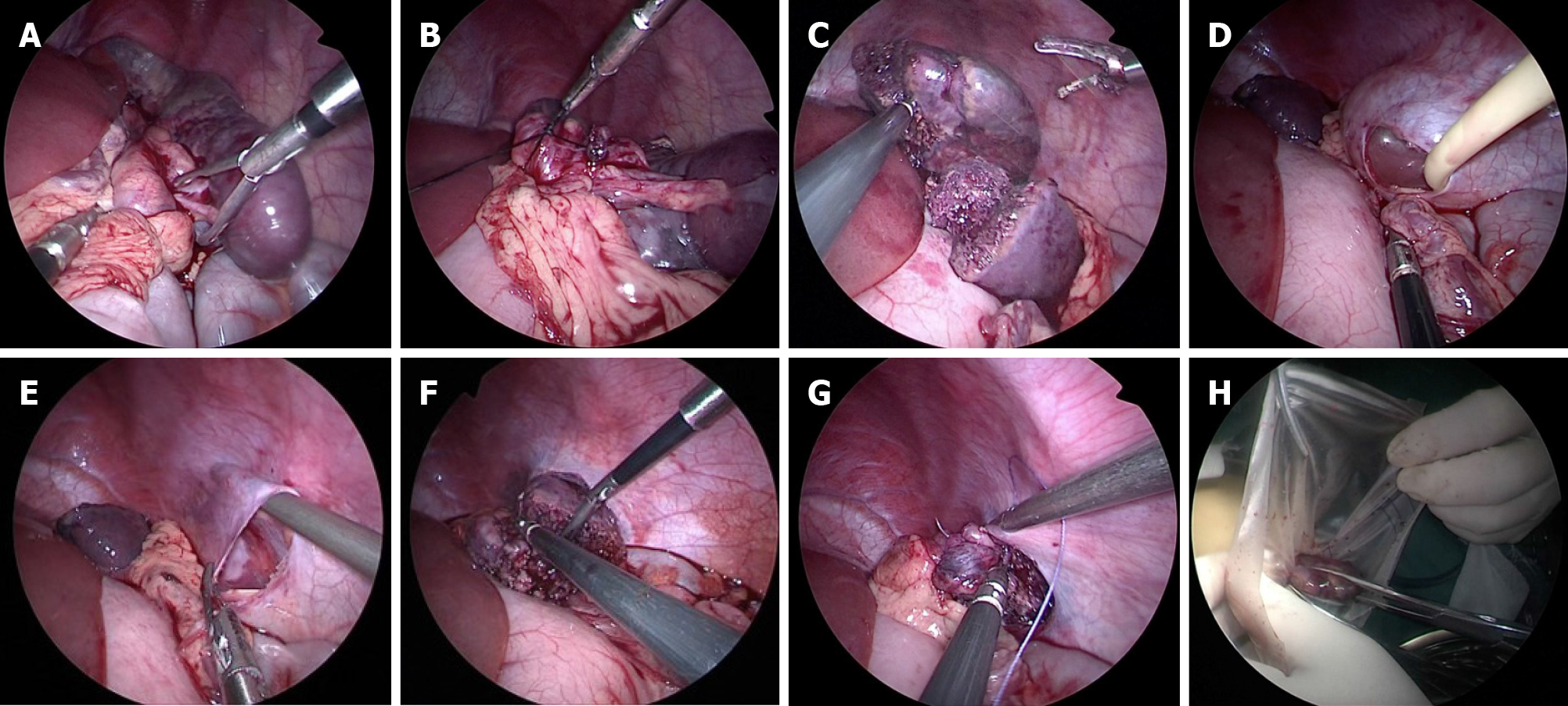
Case 2: Laparoscopic exploration was performed (Figure 1). TriPort was placed on the umbilicus. In addition, a 5 mm Trocar was inserted under the costal margin of the left anterior axillary line. The spleen was repositioned clockwise (5 wk). An ultrasonic scalpel was used to cut off the spleen along the boundary between the middle and lower poles of the spleen, leaving about 30% of the surviving spleen. The peritoneum was cut horizontally close to the lower edge of the posterolateral diaphragm of the splenic fossa. After bluntly separating the extraperitoneal space, a No. 14 Foley urinary catheter was inserted through the Trocar that was at left upper abdomen. The extraperitoneal space was formed by injecting 40 mL air balloon in vitro. The residual spleen tissue was placed in the expanded extraperitoneal space, and the peritoneal incision was sutured to complete the extraperitoneal splenic lower pole fixation. Place the collection bag through TriPort, put the excised necrotic spleen into the bag, crush the necrotic spleen tissue through the umbilical incision and take it out.
Case 1: The postoperative pathological examination of the resected spleen showed old anemic splenic thrombosis. On the 5th day after operation, the blood routine was reexamined. Platelets were increased from 184 × 109 cells/L before operation to 946 × 109 cells/L, and hemoglobin was increased from 82 g/L before operation to 108 g/L. The patient was cured and discharged from hospital. At 5 mo and 3 years after operation, B-ultrasound of spleen was reexamined twice, and both showed that the residual spleen had a uniform echo and a good blood supply.
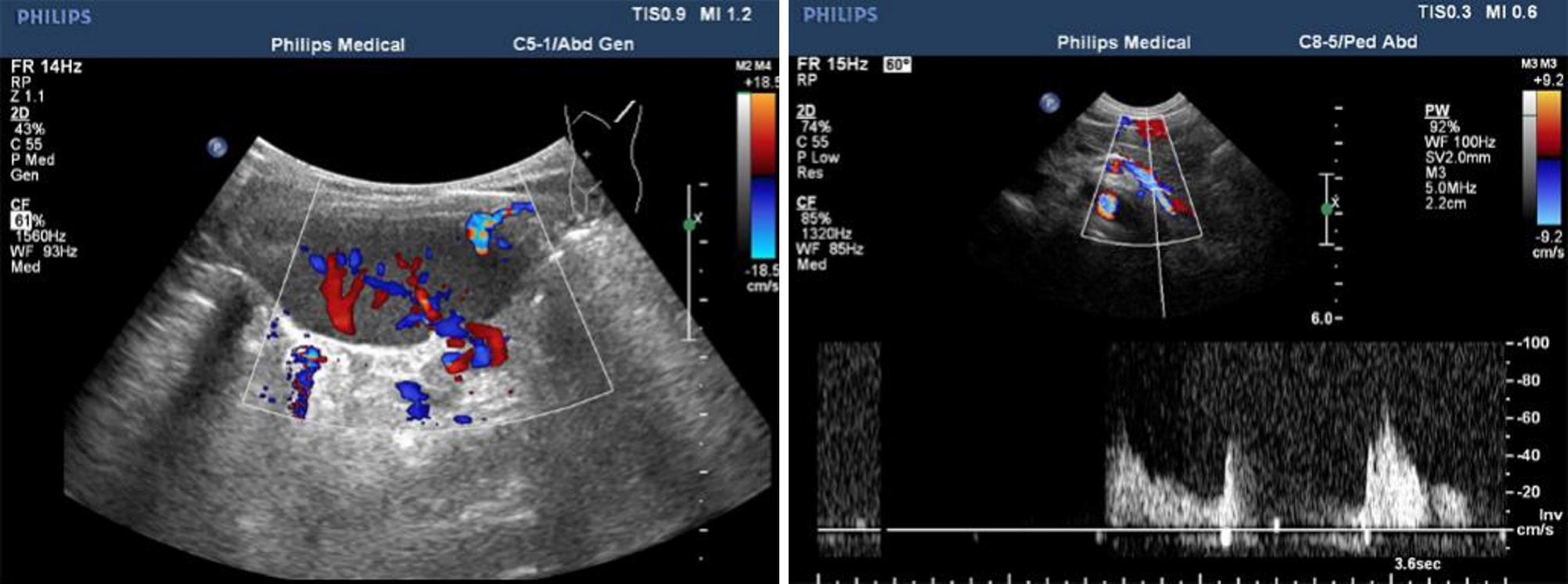
Case 2: The operation time was 105 min, the intraoperative blood loss was 20 mL, and there was about 4 cm × 3 cm × 2.5 cm spleen tissue remaining at the lower pole of the spleen. One accessory spleen was found during the operation and was reserved. On the 3rd day after operation, blood routine examination showed that platelets were 566 × 109 cells/L and hemoglobin was 107 g/L. The abdominal drainage tube was removed on the 3rd day after operation, and the patient was cured and discharged on the 5th day after operation. One month after the operation, the CT scan of the spleen showed no signs of ischemia in the residual spleen. Eight months after the operation, ultrasound examination showed that the size of the residual spleen was 5.3 cm × 3.5 cm × 2 cm, the blood picture was normal, the echo was homogeneous, and the blood supply was good (Figure 2).
Floating spleen is caused by abnormal embryonic development. In the embryonic stage, the spleen occurs in the interstitial cells of the dorsal mesangium of the stomach in the left upper abdomen. Splenorenal ligament hypoplasia and abnormal relaxation of the splenic and colon ligaments lead to poor fixation of the spleen and migration, which may be combined with intestinal malrotation, diaphragmatic hernia and other developmental abnormalities[6]. Floating spleen is more common in children under 10-years-old[7]. The previous case reports were shown in Table 1.
| Ref. | Age | Sex | Localization | Type of surgery | DOI |
| Hirose et al[24], 1998 | 2 | Female | Oita University, Japan | Elective laparoscopic splenopexy was performed by anchoring the spleen wrapped in absorbable mesh | 10.1016/s0022-3468(98)90503-6 |
| Schaarschmidt et al[35], 2005 | 9 | Female | Helios-Center for Pediatric Surgery, Germany | Retroperitoneal pocket created by using a self-made balloon | 10.1016/j.jpedsurg.2004.11.020 |
| Martínez-Ferro et al[27], 2005 | 4 | Male | National Pediatric Hospital, Argentina | Retroperitoneal pocket created by using a self-made balloon | 10.1016/j.jpedsurg.2005.02.009 |
| Kleiner et al[29], 2006 | 12 | Female | Ben Gurion University of the Negev, Israel. | Pexy by using a polyglactin mesh bag and endoscopic stapler to the left diaphragm | 10.1089/lap.2006.16.328 |
| Fukuzawa et al[28], 2006 | 11 | Male | Shizuoka Children’s Hospital, Japan | Retroperitoneal pocket created by using a preperitoneal distention balloon | 10.1007/s00383-006-1760-2 |
| Falchetti et al[36], 2007 | 14 | Female | Department of Pediatric Surgery, Spedali Civili, Italy | Pexy by using a polyglactin mesh bag to the left hypocondrium covered with omentum | 10.1016/j.jpedsurg.2007.03.063 |
| Upadhyaya et al[37], 2007 | 14 | Female | Children’s Mercy Hospital, United States | Pexy by using a polyglactin mesh bag to the left hypocondrium covered with omentum | 10.1016/j.jpedsurg.2007.03.001 |
| Rescorla et al[38], 2007 | 2 | N/A | Indiana University School of Medicine, United States | Pexy by using a polyglactin mesh bag and metal clip to the left diaphragm | 10.1097/SLA.0b013e318155abb9 |
The clinical manifestations of floating spleen are complicated. If there is no torsion of the spleen pedicle, it is generally asymptomatic, and a few may have compression or volvulus symptoms on adjacent organs. Severe activity, gastrointestinal dysfunction, trauma, and other reasons can cause torsion of splenic pedicle. Floating splenic volvulus includes acute torsion and chronic torsion. Complications of acute splenic volvulus include gangrene or splenic abscess formation, gastroesophageal vertical bleeding, acute or chronic diabetic inflammation, which showed spleen necrosis after pancreatic tail torsion, intestinal obstruction, gastric outlet obstruction, and partial or complete gastric volvulus[8]. Children with acute splenic volvulus are often prone to sudden severe abdominal pain or even shock after changing body position, and can also have sudden splenomegaly or abdominal hematocele. Chronic splenic volvulus leads to venous reflux obstruction, characterized by intermittent abdominal pain, gradually enlarged spleen and compression of adjacent organs, which can be fixed when adhering to surrounding tissues. In addition, because chronic splenic volvulus can make the spleen enlarged, the adjacent intestinal tract and mesentery can also be twisted. Compression of splenic portal vessels leads to stenosis, occlusion, thrombosis, and eventually left portal hypertension. And in rare cases, it can even manifest as gastric fundus, splenic vein, mesenteric vein stasis, and even rupture and bleeding of gastric fundus varicose veins[9,10].
Before the application of isotope angiography and angiography, the diagnosis of floating spleen was very difficult. In 1854, J ó ZEF first reported a case of floating spleen in child, which was provided by courtesy of the Polish National Digital Archives. Dietl[11,12] reported two cases of floating spleen in 1856 and 1863. With the development of imaging technology, the diagnostic methods of floating spleen mainly include CT, ultrasound, or angiography[13,14]. If CT shows absence of spleen and abnormal spleen-like mass in pelvic and abdominal cavity, physicians should be alerted to the possibility of floating spleen. According to Chauhan and Kumar[15], typical CT manifestations of wandering spleen include: the spleen disappearing in the left upper abdomen, unknown mass and ectopic swelling of the spleen; spiral appearance of splenic vessels; and secondary manifestations of the splenic pedicle volvulus (such as pancreatic tail necrosis and ascites)[13]. Ultrasound examination showed that there was an echo when there was abdominal mass, but there was no echo in normal splenic anatomy. Angiography can clearly show the blood supply of ectopic spleen and whether there is volvulus or infarction. In 1878, Martin[16] first reported a case of floating spleen in Berlin, Germany. In 1895, Rydygier[17] completed the splenic fixation for the first time. The spleen was fixed in the cavity formed by the abdominal posterior wall peritoneum to treat the floating spleen. Hall[18] reported that the lower pole of the spleen was fixed in the retroperitoneal space, while the spleen pedicle was fixed to the peritoneal incision, and the upper pole of the spleen was suspended and fixed to the ribs. At that time, without splenic reduction, splenic fixation had become the first choice for the treatment of floating spleen without infarction or hypersplenism[19].
With further research on the spleen function, most scholars believe that spleen preservation is of great significance for maintaining normal immunity, and that splenectomy will increase the risk of postoperative sepsis. In 2011, 19680 patients with splenectomy were retrospectively analyzed, including 3708 children[20]. The postoperative infection rate was 3.3%, the fatality rate was 1.7%, and there was a higher mortality rate in children than adults (1.7% vs 1.3%). Some scholars have shown that compared with healthy controls, the incidence of infection and fatal sepsis in patients with asplenia increased by 40 times and 17 times, respectively. Among them, age < 2 years and 2 years after operation are the risk factors leading to an increased incidence of infection and fatal sepsis[21]. Moreover, some studies have shown that the accessory spleen retained during splenectomy can appear secondary to enlargement and replace the original spleen function[22]. Therefore, surgery to preserve the spleen has gradually become the first choice of most surgeons. If there is splenic volvulus and infarction, the accessory spleen should be preserved when found.
With the gradual development of minimally invasive surgical equipment and technology, laparoscopic surgery can be used to diagnose and treat the floating spleen. It can thoroughly explore the abdominal cavity and clarify the position. At the same time, it can complete the spleen reduction and fixation, and the effect is equivalent to open surgery, and the operation time is short and the postoperative recovery is fast. Therefore, laparoscopic splenectomy has gradually become the mainstream operation for the treatment of floating spleen[23]. At the same time, the method of splenic fixation also gradually evolved over time. In 1998, Hirose et al[24] first reported a case of laparoscopic splenectomy for the treatment of 2-year-old girl with floating spleen[19]. Early spleen preservation surgery was mainly to straighten out the spleen pedicle and place the spleen in situ, but recurrence of spleen volvulus is prone to occur, leading to reoperation[25]. Peitgen et al[26] further improved the splenic fixation by using omental sac to wrap the spleen and fix the spleen at the left renal angle under laparoscope. Another laparoscopic splenectomy was reported in 2005 by Martínez-Ferro et al[27]. The skin was incised in the projection area of the left upper abdomen spleen, which was blunt separated to the peritoneal layer to form a small extraperitoneal space. The balloon was inserted to expand the capsule to form a bag. Then the peritoneum of the bag was opened from the abdominal cavity, and the spleen was placed into the bag to complete the splenic fixation. Fukuzawa et al[28] reported the same extraperitoneal splenectomy as before in 2006. It was also mentioned that ultrasound is more safe and accurate in locating the extraperitoneal space during inhalation. Kleiner et al[29] reported in 2006 that laparoscopic splenectomy was performed in a 12-year-old girl with splenic volvulus. In the operation, the spleen was put into a net bag made of absorbable materials and fixed to the diaphragm. The diaphragm colon ligament and lateral abdominal wall were used to form a support to help fix the spleen. In laparoscopic surgery, extraperitoneal space fixation is much more complicated, but it is easier to cover the spleen with absorbable mesh. At the same time, the mesh will cause adhesion of surrounding tissues and strengthen spleen fixation[30]. Montenovo et al[31] reported in 2010 that hybrid laparoscopic splenectomy was performed for the treatment of floating spleen. After the spleen was reset, the spleen was placed into the mesh pocket, and an extraperitoneal space was established on the lateral wall of the abdomen. The lower pole of the spleen was placed in the extraperitoneal space. The mesh bag covering the upper pole of the spleen was sutured with the greater curvature of the stomach, diaphragm, lateral abdominal wall and the splenic flexure of the colon to avoid twisting again. Okazaki et al[32] reported a 4-year-old boy with spleen volvulus who underwent laparoscopic splenectomy in 2011[27]. The spleen was placed into the left upper abdominal extraperitoneal space, and absorbable mesh was placed at the peritoneal incision for repair. This can not only prevent the extraperitoneal space from being too small to accommodate the spleen, but also reduce the risk of splenic vascular injury when suturing the peritoneal incision.
The postoperative complications of splenic fixation mainly include splenic ischemia, infarction and recurrent torsion. Magno et al[33] retrospectively analyzed 125 cases of patients who underwent splenectomy and splenic fixation, and found that the incidence of postoperative complications was about 5%, including splenic infarction, recurrent volvulus, splenic ischemia, pneumothorax[33]. Fiquet-Francois et al[34] retrospectively analyzed 14 cases of patients who underwent splenic vagrant surgery in multicenter. Among them, 5 patients underwent laparoscopic operation, and 3 patients were treated with mesh bag covered splenic fixation. Splenic ischemia occurred after operation in those 8 patients.
Combined with the literature, we summarize the experience as follows. After laparoscopic examination of splenic torsion, we should first try to reset and observe the recovery of splenic blood supply. Partial splenectomy and retroperitoneal fixation of the remaining spleen are feasible if the blood supply of part of the spleen is acceptable and independent blood supply exists. If the spleen is infarcted, complete splenectomy is necessary. If the accessory spleen is found during the operation, it is suggested to retain it, so as to preserve the immune function of the spleen to the greatest extent. The unique feature of this operation is complete partial splenectomy by laparoscopy and extraperitoneal fixation of residual spleen. No incision was made outside the abdominal wall. The operation is further simplified and the postoperative appearance is better.
In conclusion, children with acute abdominal pain and active tumor should be alert to the possibility of floating spleen. Laparoscopic partial resection of splenic volvulus infarction and extraperitoneal fixation of residual spleen are safe and reliable. The minimally invasive operation can retain the function of spleen with residual blood supply.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Yildirim M S-Editor: Fan JR L-Editor: Filipodia P-Editor: Liu JH
| 1. | Koliakos E, Papazarkadas X, Sleiman MJ, Rotas I, Christodoulou M. Wandering Spleen Volvulus: A Case Report and Literature Review of This Diagnostic Challenge. Am J Case Rep. 2020;21:e925301. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 2. | Guvendi B, Ogul H. Wandering spleen and intestinal malrotation. Cir Esp (Engl Ed). 2019;97:232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 3. | Tagliabue F, Chiarelli M, Confalonieri G, Pesenti G, Beretta S, Cappello A, Fumagalli LAM, Costa M. The Wandering Spleen. J Gastrointest Surg. 2018;22:546-547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Gorsi U, Bhatia A, Gupta R, Bharathi S, Khandelwal N. Pancreatic volvulus with wandering spleen and gastric volvulus: an unusual triad for acute abdomen in a surgical emergency. Saudi J Gastroenterol. 2014;20:195-198. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 5. | Karapolat B, Korkmaz HAA, Kocak G. Torsion of the Wandering Spleen. Am J Med Sci. 2019;357:e17-e18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Bouassida M, Sassi S, Chtourou MF, Bennani N, Baccari S, Chebbi F, Benali M, Mighri MM, Touinsi H. A wandering spleen presenting as a hypogastric mass: case report. Pan Afr Med J. 2012;11:31. [PubMed] |
| 7. | Köseoğlu H, Atalay R, Büyükaşık NŞ, Canyiğit M, Özer M, Solakoğlu T, Akın FE, Bolat AD, Yürekli ÖT, Ersoy O. An Unusual Reason for Gastric Variceal Hemorrhage: Wandering Spleen. Indian J Surg. 2015;77:750-751. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Lien CH, Lee HC, Yeung CY, Chan WT, Wang NL. Acute torsion of wandering spleen: report of one case. Pediatr Neonatol. 2009;50:177-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Wani S, Abdulkarim AB, Buckles D. Gastric variceal hemorrhage secondary to torsion of wandering spleen. Clin Gastroenterol Hepatol. 2008;6:A24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Sato M, Miyaki Y, Tochikubo J, Onoda T, Shiiya N, Wada H. Laparoscopic splenectomy for a wandering spleen complicating gastric varices: report of a case. Surg Case Rep. 2015;1:3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Dietl J. O ruchomej s´ledzionie, uwagi czerpane z ogle˛dzin pos´miertnych (About a wandering spleen from post mortem examination). Pamie˛tnik Towarzystwa Lekarskiego Warszawskiego. 1856;12:111-123. |
| 12. | Dietl J. We˛druja˛ca s´ledziona. Zapalenie otrzewnej. S´mierc´ (Wandering Spleen. Peritonitis. Death). Prz Lek. 1863;2:98-100. |
| 13. | Danaci M, Belet U, Yalin T, Polat V, Nurol S, Selçuk MB. Power Doppler sonographic diagnosis of torsion in a wandering spleen. J Clin Ultrasound. 2000;28:246-248. [PubMed] [DOI] [Full Text] |
| 14. | Guo LQ, Zhang XL, Liu YQ, Sun WD, Zhao ST, Yuan MZ. The application of laparoscopic Doppler ultrasound during laparoscopic varicocelectomy in infertile men. Asian J Androl. 2017;19:214-218. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Chauhan NS, Kumar S. Torsion of a Wandering Spleen Presenting as Acute Abdomen. Pol J Radiol. 2016;81:110-113. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 16. | Martin A. A Successful Case of Splenotomy. Br Med J. 1878;1:191-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 17. | Rydygier L. O przyszywaniu s´ledziony. Splenopexy (About sewing on of the spleen. Splenopexy). Prz Lek. 1895;34:65-66. |
| 18. | Hall JB. I. Splenopexy for Wandering Spleen: With Report of a Case. Ann Surg. 1903;37:481-485. [PubMed] |
| 19. | Misawa T, Yoshida K, Shiba H, Kobayashi S, Yanaga K. Wandering spleen with chronic torsion. Am J Surg. 2008;195:504-505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 20. | Bisharat N, Omari H, Lavi I, Raz R. Risk of infection and death among post-splenectomy patients. J Infect. 2001;43:182-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 296] [Cited by in RCA: 295] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 21. | Wester A, Co I. Wandering Spleen. N Engl J Med. 2020;383:2065. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 22. | Magowska A. Wandering spleen: a medical enigma, its natural history and rationalization. World J Surg. 2013;37:545-550. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 51] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 23. | Benevento A, Boni L, Dionigi G, Ferrari A, Dionigi R. Emergency laparoscopic splenectomy for "wandering" (pelvic) spleen: case report and review of the literature on laparoscopic approach to splenic diseases. Surg Endosc. 2002;16:1364-1365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 24. | Hirose R, Kitano S, Bando T, Ueda Y, Sato K, Yoshida T, Suenobu S, Kawano T, Izumi T. Laparoscopic splenopexy for pediatric wandering spleen. J Pediatr Surg. 1998;33:1571-1573. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 54] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 25. | Brown CV, Virgilio GR, Vazquez WD. Wandering spleen and its complications in children: a case series and review of the literature. J Pediatr Surg. 2003;38:1676-1679. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 65] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 26. | Peitgen K, Majetschak M, Walz MK. Laparoscopic splenopexy by peritoneal and omental pouch construction for intermittent splenic torsion ("wandering spleen"). Surg Endosc. 2001;15:413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 27. | Martínez-Ferro M, Elmo G, Laje P. Laparoscopic pocket splenopexy for wandering spleen: a case report. J Pediatr Surg. 2005;40:882-884. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 28. | Fukuzawa H, Urushihara N, Ogura K, Miyazaki E, Matsuoka T, Fukumoto K, Kimura S, Mitsunaga M, Hasegawa S. Laparoscopic splenopexy for wandering spleen: extraperitoneal pocket splenopexy. Pediatr Surg Int. 2006;22:931-934. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 29. | Kleiner O, Newman N, Cohen Z. Pediatric wandering spleen successfully treated by laparoscopic splenopexy. J Laparoendosc Adv Surg Tech A. 2006;16:328-330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 30. | Fonseca AZ, Ribeiro M Jr, Contrucci O. Torsion of a wandering spleen treated with partial splenectomy and splenopexy. J Emerg Med. 2013;44:e33-e36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 31. | Montenovo MI, Ahad S, Oelschlager BK. Laparoscopic splenopexy for wandering spleen: case report and review of the literature. Surg Laparosc Endosc Percutan Tech. 2010;20:e182-e184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 32. | Okazaki T, Ohata R, Miyano G, Lane GJ, Takahashi T, Yamataka A. Laparoscopic splenopexy and gastropexy for wandering spleen associated with gastric volvulus. Pediatr Surg Int. 2010;26:1053-1055. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 33. | Magno S, Nanni L, Retrosi G, Cina A, Gamba PG. An unusual case of acute pancreatitis and gastric outlet obstruction associated with wandering spleen treated by laparoscopic splenopexy. J Laparoendosc Adv Surg Tech A. 2011;21:467-470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 34. | Fiquet-Francois C, Belouadah M, Ludot H, Defauw B, Mcheik JN, Bonnet JP, Kanmegne CU, Weil D, Coupry L, Fremont B, Becmeur F, Lacreuse I, Montupet P, Rahal E, Botto N, Cheikhelard A, Sarnacki S, Petit T, Poli Merol ML. Wandering spleen in children: multicenter retrospective study. J Pediatr Surg. 2010;45:1519-1524. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 36] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 35. | Schaarschmidt K, Lempe M, Kolberg-Schwerdt A, Schlesinger F, Hayek I, Jaeschke U. The technique of laparoscopic retroperitoneal splenopexy for symptomatic wandering spleen in childhood. J Pediatr Surg. 2005;40:575-577. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 29] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 36. | Falchetti D, Torri F, Dughi S, Porto C, Manciana A, Boroni G, Ekema G. Splenic cyst in a wandering spleen: laparoscopic treatment with preservation of splenic function. J Pediatr Surg. 2007;42:1457-1459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 37. | Upadhyaya P, St Peter SD, Holcomb GW 3rd. Laparoscopic splenopexy and cystectomy for an enlarged wandering spleen and splenic cyst. J Pediatr Surg. 2007;42:E23-E27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 38. | Rescorla FJ, West KW, Engum SA, Grosfeld JL. Laparoscopic splenic procedures in children: experience in 231 children. Ann Surg. 2007;246:683-687; discussion 687. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 86] [Article Influence: 4.8] [Reference Citation Analysis (0)] |