Published online Sep 26, 2021. doi: 10.12998/wjcc.v9.i27.8082
Peer-review started: May 11, 2021
First decision: June 15, 2021
Revised: June 29, 2021
Accepted: July 16, 2021
Article in press: July 16, 2021
Published online: September 26, 2021
Processing time: 128 Days and 0.4 Hours
Lumbar disc herniation (LDH) has emerged as one of the most common causes of low back pain. The routine treatment approach involves chemonucleolysis therapy, discectomy by percutaneous endoscopy, and percutaneous laser disc decompression. Unfortunately, all of these methods carry inherent risk of causing harm to the patient and, as such, there is an unmet but urgent need for an effective and safe noninvasive treatment for LDH. The purpose of this report is to describe a non-invasive method for re-absorption of LDH.
A 34-year-old woman was admitted with a complaint of waist pain that she reported as having become acutely aggravated over the past 3 d and accompanied by discomfort in the right lower limb. Her self-reported medical history included persistent postpartum low back pain from 7 years prior. Physical exam showed positivity for neck flexion test (Lindner sign) and supine abdomen test; the straight leg-raising test showed right 60(+) and left 80(-). Findings from standard imaging (magnetic resonance) and collective physical examinations indicated a L5/S1 herniated lumbar disc. Treatment consisted of three-dimensional (balanced regulating) spinal manipulation and acupuncture, upon which the LDH resolved by retraction.
Following L5/S1 herniated lumbar disc diagnosis, three-dimensional (balanced regulating) spinal manipulation combined with acupuncture therapy is an effective treatment.
Core Tip: In view of the risks associated with surgical treatment of lumbar disc herniation (LDH), this case report describes the successful treatment of a disc herniation by means of three-dimensional (balanced regulating) spinal manipulation. The steps involved in this technique are as follows: (1) Relaxation and stiffening; (2) three-dimensional spine manipulation; and (3) relaxation. Ultimately, this treatment effectively cured the patient’s LDH and provided a safe noninvasive alternative to the current invasive methods, overcoming their inherent risks.
- Citation: Wang P, Chen C, Zhang QH, Sun GD, Wang CA, Li W. Retraction of lumbar disc herniation achieved by noninvasive techniques: A case report. World J Clin Cases 2021; 9(27): 8082-8089
- URL: https://www.wjgnet.com/2307-8960/full/v9/i27/8082.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i27.8082
Low back pain has become an extremely common problem, with most people experiencing it to some degree at least once in their life. Indeed, the reported lifetime prevalence is 40% among the adult general population[1]. While the mechanism of low back pain remains to be fully elucidated, data from evidence-based medicine have revealed an appreciable prevalence among patients with lumbar disc herniation (LDH), as compared to other asymptomatic patients (57% vs 20%-28%)[2], making herniated disc the most common cause of low back pain. For LDH, neither the cause nor its relation to back pain and sciatica has been fully elucidated, but it is considered most likely to involve a complex combination of mechanical and biological processes[3]. Protrusion of a lumbar intervertebral disc represents a syndrome with clinical manifestations of pain and paresthesia in the innervation area. Mechanistically, these symptoms are due to rupture of the lumbar intervertebral disc annulus in response to various external forces, such as degeneration; when the nucleus pulposus protrudes to the rear, it produces compression and stimulation of adjacent spinal nerve roots and cauda equina[4]. Focused research has uncovered significant associations between LDH and age, sex, occupation, and body mass index[5]. One study showed that the number of individuals diagnosed with LDH increases with age and that the incidence of LDH is higher in women than in men[6]. In addition to direct causes of chronic/acute low back pain, LDH has been found to be closely related to non-physical factors, such as depression, insomnia, and smoking[7-9]. Consideration of all these factors is necessary for optimizing the treatment of LDH.
LDH can be effectively addressed by lumbar surgery, and is one of the most common indications for such. Modern society has seen a change in the workplace towards a more sedentary situation, paralleling the greater amount of time that the average worker spends using computers. Accordingly, although LDH has been historically characterized as a geriatric degenerative disease, it is now showing an increasing incidence among younger individuals[10]. The current treatment approach for LDH is largely conservative, involving such modalities as physical manipulation, acupuncture, and anti-inflammatory and analgesic drugs[11]. However, for persistent or more severe cases, the methods are invasive in nature, such as chemonucleolysis therapy[12], discectomy by percutaneous endoscopy, or percutaneous laser disc decompression[13], and carry inherent risk to the patient. Currently, there are many surgical treatment methods available for LDH, based upon open surgery as well as minimally invasive surgery[14]. Traditional open surgery is characterized by many drawbacks, such as substantial trauma, a large amount of intraoperative blood loss, and the need to dissect soft tissues, ligaments, and muscles around the lumbar spine, the latter of which also carries an appreciable risk of infection[15]; in addition, postoperative recovery is slow. While minimally invasive surgeries are safer, they are not free of risk. In micro-invasive surgery, the use of computed tomography and other auxiliary positioning techniques further increases its safety[16]. One example of this is the transforaminal spinal endoscopic technique; while it has helped optimize patient positioning, its use of fluoroscopy exposes both the patient and doctor to radiation, thereby increasing the well-known and inherent risks of such. For doctors, especially, there is a real risk of cumulative effects from radiation exposure related to long-term surgical practice[17].
Herein, we report a case of long-standing LDH that was cured by noninvasive conservative treatment.
A 34-year-old woman complained of lumbar pain accompanied by right lower extremity discomfort.
The patient self-reported that starting 3 d prior, the waist pain had acutely aggravated.
The patient self-reported having experienced persistent low back pain for the past 7 years, which had been initiated after giving birth.
The curvature of the patient’s lumbar spine appeared to be slightly straightened, and the muscle of the lower back was stiff. The angles of the lumbar vertebra were measured with a goniometer, and upon forward bending and backward stretching were 10 and 5, respectively. The angles upon flexion and rotation to the left and right were roughly 10 each. The L4-L5 bilateral spine showed prominent side tenderness and percussion pain was apparent. The neck flexion test (Lindner sign) was positive, as was the supine abdomen test. The straight leg-raising test showed right 60(+) and left 80(-). The right knee tendon reflex was weakened but the ankle reflex was normal. The ankle and patellar clonus tests showed negativity. Visual analogue scale (VAS) score was 8. According to the Fukuda method for measuring the rate of intervertebral disc herniation[1], the patient scored 84.5%.
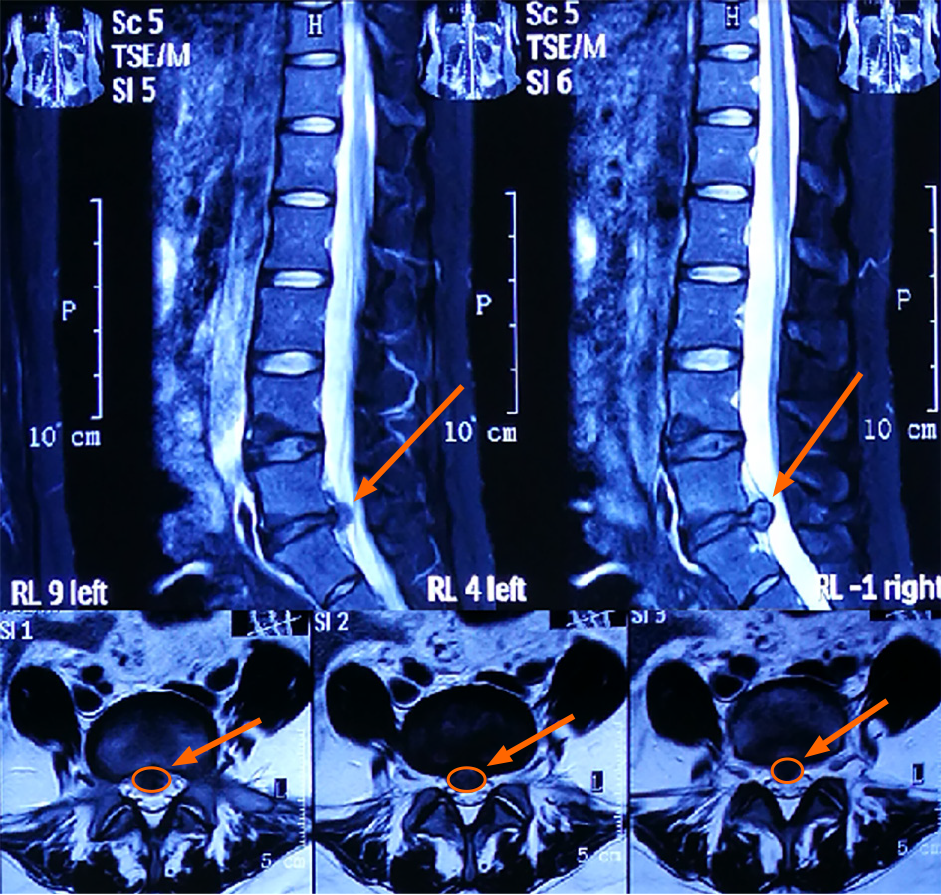
Magnetic resonance imaging (MRI) was undertaken and showed L5/S1 intervertebral disc herniation (giant) (Figure 1).
L5/S1 LDH.
L5/S1 LDH.
A 30-d treatment course was designed and implemented as follows: (1) Physical mechanical manipulation to relieve muscle spasm (each day); (2) acupuncture to clear the meridians, qi, and blood with the assistance of voltaren to relieve pain and inflammation (each day); and (3) three-dimensional (balanced regulating) spinal manipulation to correct facet joint disorder and improve the overall stress on the spine (each day). The acupuncture site encompassed the Shenshu, Sanjiaoshu, Guanyuanshu, Qihaishu, Huantiao, Fengshi, Yanglingquan, Weizhong, Chengshan, Kunlun, and Ashi. The acupuncture procedure involved disinfecting of the acupoint regional skin with iodophor routinely and vertical insertion of a filiform needle (0.45 mm-75 mm) into the acupoint (except for special acupoints). This was followed by tonifying and relieving, which were adopted to make the local or meridian circulation area produce needle sensations, such as acid, numbness, distension, and pain. For all instances, the needle was kept in place for 20-30 min. The steps of three-dimensional (balanced regulating) spinal manipulation are as follows: (1) Relaxing, which is composed of massage, delivered to the waist and affected limbs as pressing, pushing, rolling, and other muscle management techniques for 5-10 min to relax the muscles; (2) Three-dimensional spine manipulation, which involves first laying the patient on his/her side, then initiating flexion of his/her upper leg and straightening of the lower leg. In this procedure, the doctor holds the patient's forearm with one hand and pushes the joint of the patient's shoulder and the upper arm with the forearm, while, at the same time, using the other hand to push the thumb inward at the protruding part, fixing the hip joint with the elbow, and twisting the waist to a certain extent. As such, the elbow and thumb are suddenly exerted in the opposite direction simultaneously. When the characteristic effect sound is heard and finger movement is achieved, the reset is deemed to have been successful; and (3) Relaxation, which uses a top-to-bottom pushing type massage along the sacral spinous muscle with palm root, applied for 3-5 min, followed by a straight wiping motion of the bladder meridian on both sides of the waist and back and then across the lumbosacral part with the hypothenar to the degree of local heat. While the patient is prone, the massager pulls the patient's ankles to elongate the patient’s waist to a certain extent, when he/she then shakes the appendage(s) strongly, using both hands, to overextend the patient’s waist; the strength point should fall on the protruding lumbar vertebrae three times.
After completion of the treatment course described above, the patient’s waist pain and discomfort in the right lower limb disappeared almost completely.
On physical examination at 1 mo after discharge, we noted that the curvature of the lumbar spine remained slightly straightened but the stiffness in the back muscles had improved markedly. The angles of the lumbar vertebra upon forward bending and backward stretching were improved, to 40° and 25°, respectively. The angles of flexion and rotation to the left and right were also improved, to roughly 25°. The L4-L5 bilateral paracanth tenderness and waist percussion pain had completely disappeared. The neck flexion test (Lindner sign) and supine abdomen test were both negative. The straight leg raising test showed right 80(-) and left 80(-). The right knee tendon and ankle reflexes were unaffected, remaining weakened and normal, respectively. The ankle and patellar clonus tests remained negative. The VAS score decreased to 2.
After discharge, the patient attended twice monthly appointments to receive the three-dimensional (balanced regulating) spinal manipulation.
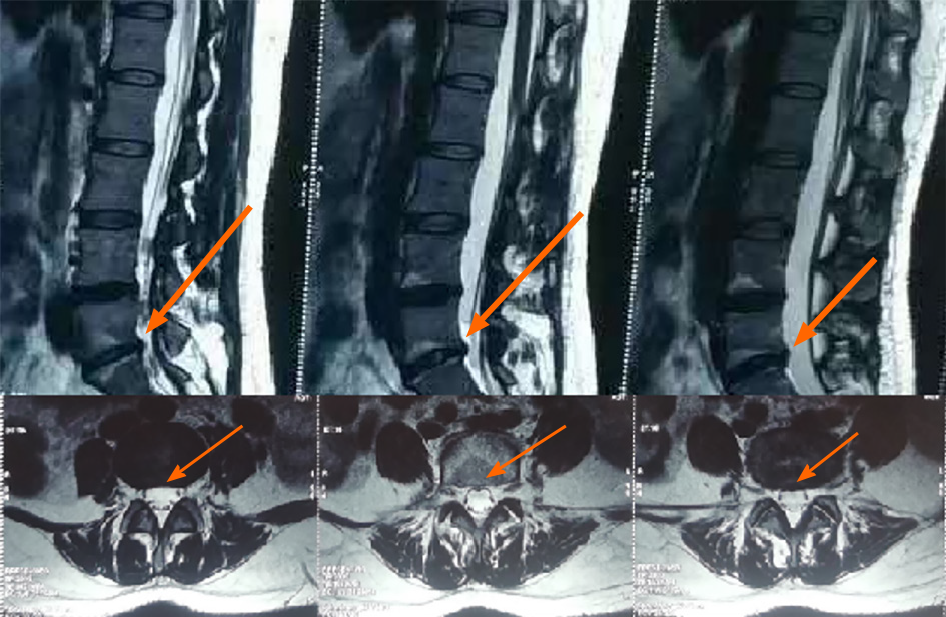
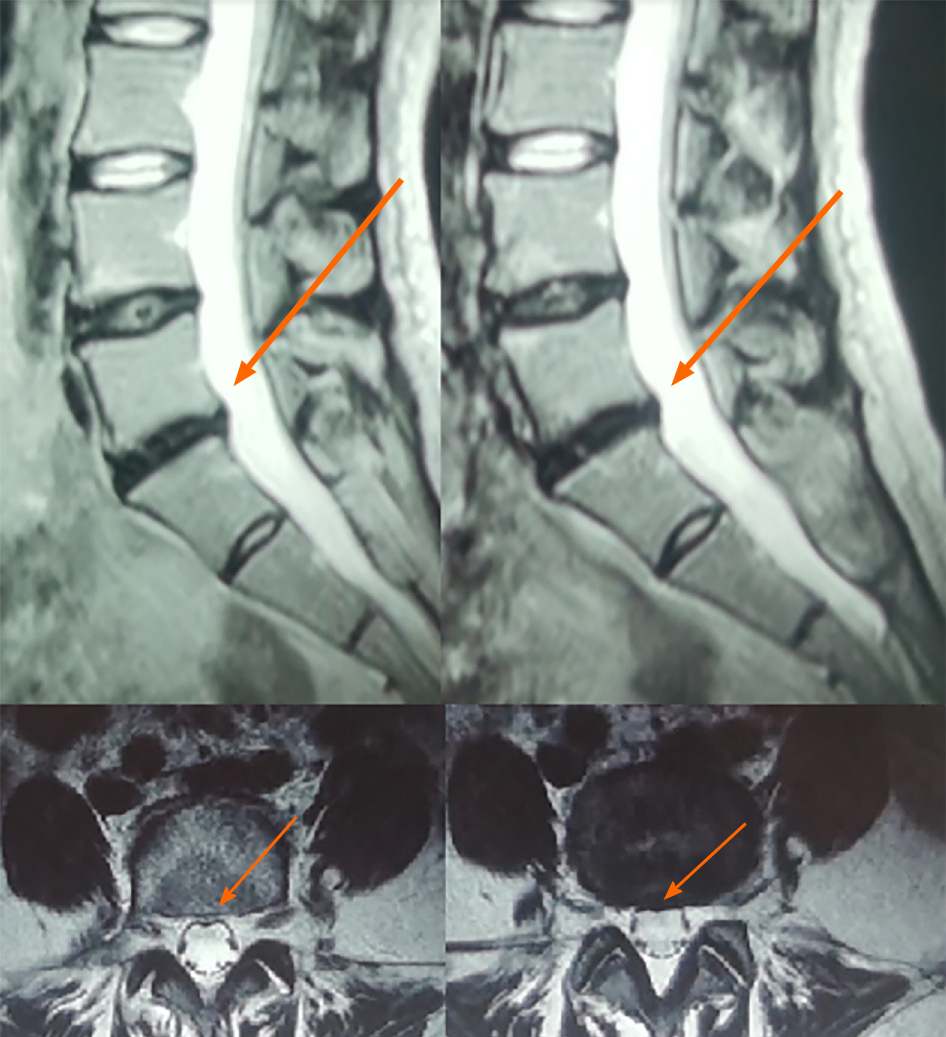
Fifteen months later, re-assessment by MRI showed that the L5/S1 had only mild bulging and the protrusion had basically disappeared (Figure 2), with a post-treatment protrusion rate of 11.3% and an absorption rate of 75%. The patient's discomfort symptoms had generally disappeared, and she reported having already been able to live and work normally. A further MRI scan at 44 mo after discharge confirmed the previous findings of resolution (Figure 3). The patient stated that her waist pain had completely gone and that she had no obvious discomfort after prolonged sitting and walking.
This case report describes a 34-year-old woman who was admitted with a complaint of waist pain following a 7-year history of persistent postpartum low back pain. Standard imaging (MRI) and physical examinations indicated a L5/S1 herniated lumbar disc. Treatment consisted of three-dimensional (balanced regulating) spinal manipulation and acupuncture, upon which the LDH resolved by retraction.
As mentioned in the Introduction, treatment options for disc herniation include both surgical and non-surgical interventions[18,19]. Surgical treatment includes percutaneous endoscopic lumbar discectomy and microsurgery. The former is a kind of minimally invasive surgery which focuses on the intervertebral disc (instead of the entire disc tissue), and aims to thoroughly remove intervertebral disc tissue that can cause lumbar iatrogenic instability. This therapeutic procedure not only alleviates the symptoms but it does so while necessitating only a small incision, causing little blood loss and quickly relieving pain; the recovery is also relatively quick, among other advantages[20]. For surgeons, however, there is a steep learning curve from novice to mastery of this technically demanding surgical procedure which relies upon complex instruments[18,21]. Early complications include nerve root injury, dural tear, inadequate decompression due to herniated disc residue, and postoperative recur
Microsurgery has remarkable benefits. With the assistance of an imaging system, it can enlarge the nerve root, dural sac, and herniated disc nucleus pulposus tissue; this helps the operator to avoid damage to these tissues while completely removing the herniated disc nucleus pulposus tissue, ultimately resolving the L5/S1 disc herniation[22]. Similar to the percutaneous endoscopic discectomy, microsurgical excision requires a long operative time and has a steep learning curve. Of note, although surgical treatment of lumbar intervertebral discs can eliminate the herniation and relieve pain quickly, its invasive nature can put great psychological pressure on patients, and there is an appreciable risk of accidental damage occurring during the surgical process. Relevant studies have also shown that the satisfactory degree to treatment effect gradually decreases in the course of 3 mo to 1 year after the surgery[23].
It was suspected that the patient had LDH due to previous pregnancy/giving birth according to her chief complaint and her actual situation. Back pain/LDH during pregnancy has been reported frequently in the domestic as well as international literature. Indeed, it was reported that more than 50% of pregnant women experience low back pain, typically between the 5th and 7th mo of gestation; in addition, LDH was reported to affect 1 in 10000 pregnant women[24]. In our case, the imaging examination confirmed our assumption.
This study adopts a three-dimensional balance ridge technique, which combines pulling force, torque, and shear force. The widened intervertebral disc gradually narrows after the adjustment to its pre-widened state. This causes a negative pressure within the intervertebral disc, whereby the protrusions have an obvious sucking force, and displacement of the protrusions then reduces or eliminates the oppression of the nerve[25]. In addition, when the manipulation is applied to the vertebral body in the three-dimensional spatial structure, the posterior longitudinal ligament will suddenly undergo a state of tension. That tension will push forward the protrusion and accelerate the retraction of the nucleus pulposus, ultimately improving the relative position of the protrusion and the compressed nerve. In this non-invasive way, the patient does not have to bear the great psychological stress caused by invasive surgery. Our case underwent treatment of LDH by three-dimensional (balanced regulating) spinal manipulation, showing it to be a feasible option for non-surgical treatment of such patients.
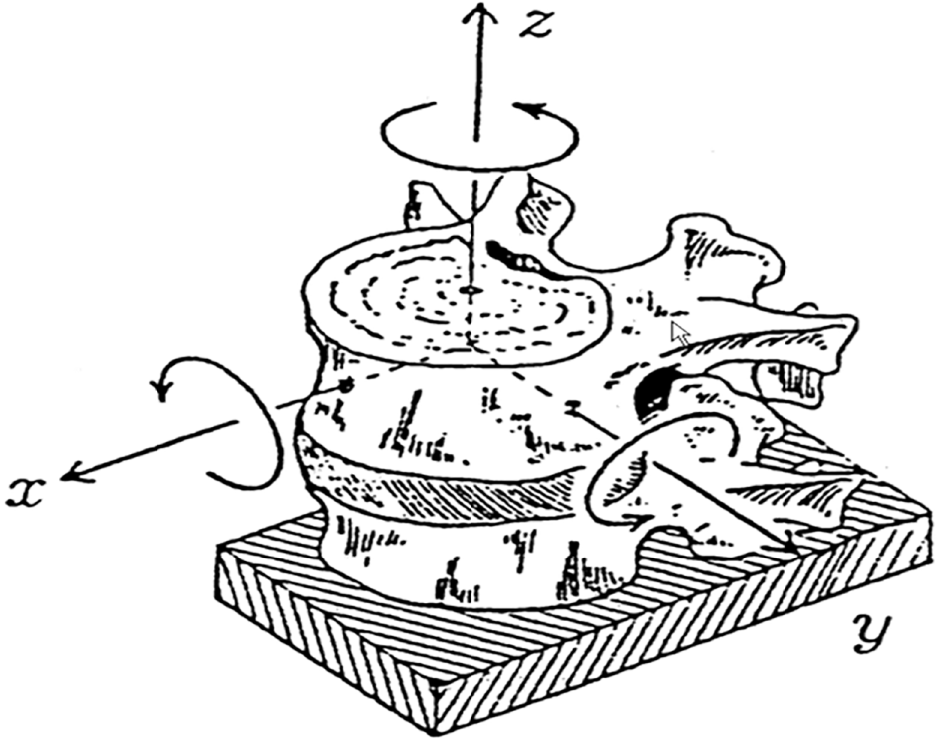
The resolution of LDH through the noninvasive methods of acupuncture and massage was achieved in our case. Herniated nucleus pulposus and ruptured annulus fibrosus could contribute to prolapsed lumbar discs, which will cause a three-dimensional displacement of the lumbar spine and soft tissue injury of the lumbar spine. We deduce that the three-dimensional balanced chiropractic manipulation combined with acupuncture mediated the retraction of our patient’s LDH. The mechanism of three-dimensional balanced chiropractic manipulation considers, first, the position of the herniated lumbar disc in relation to the nerve root, serving to adjust it. As shown in Figure 4, spinal motion has three-dimensional directions (i.e. front and back, left and right, rotational). Displacement of the three-dimensional direction of the spine and the normal force change of the spinal soft tissue are caused by the imbalance of spinal mechanics. As such, three-dimensional balanced chiropractic manipulation aims to and can correct spinal displacement[26,27]. Second, the herniated disc becomes released under pressure, and adherent nerve roots can be temporarily or durably released, alleviating the pathologic inflammatory changes that have occurred around the nerve roots. Ultimately, this method has the important advantage of being noninvasive (particularly non–surgical), overcoming the major inherent risks of the other surgical-based treatments.
One potentially limiting aspect of treating a disc herniation in this non-invasive way, to prompt re-absorption, is the longer period of time needed for the situation to resolve, compared to a surgical treatment. However, we believe that this non-invasive treatment is still a beneficial alterative to surgery, as it reduces the real psychological burden on patients and avoids the risks inherent to other well-known invasive procedures.
This case report describes a 34-year-old woman who was admitted with a complaint of waist pain following a 7-year history of persistent postpartum low back pain. Standard imaging (magnetic resonance) and physical examinations indicated a L5/S1 herniated lumbar disc. Treatment consisted of three-dimensional (balanced regulating) spinal manipulation and acupuncture, upon which the LDH resolved by retraction.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Abdelbasset WK S-Editor: Fan JR L-Editor: Wang TQ P-Editor: Guo X
| 1. | Manchikanti L, Singh V, Falco FJ, Benyamin RM, Hirsch JA. Epidemiology of low back pain in adults. Neuromodulation. 2014;17 Suppl 2:3-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 291] [Cited by in RCA: 355] [Article Influence: 35.5] [Reference Citation Analysis (0)] |
| 2. | Comer C, Conaghan PG. Tackling persistent low back pain in primary care. Practitioner. 2009;253:32-34, 3. [PubMed] |
| 3. | Awad JN, Moskovich R. Lumbar disc herniations: surgical versus nonsurgical treatment. Clin Orthop Relat Res. 2006;443:183-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 90] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 4. | Li Y, Fredrickson V, Resnick DK. How should we grade lumbar disc herniation and nerve root compression? Clin Orthop Relat Res. 2015;473:1896-1902. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 58] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 5. | Chen XL, Hai Y, Guan L, Liu YZ, Yang JC, Su QJ, Kang N, Meng XL, Yang L, Wang Y. [Topping-off surgery versus double-segment fusion for treatment of lumbar degenerative disease with mid-long term follow-up]. Zhonghua Yi Xue Za Zhi. 2017;97:857-863. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 6. | Kim YK, Kang D, Lee I, Kim SY. Differences in the Incidence of Symptomatic Cervical and Lumbar Disc Herniation According to Age, Sex and National Health Insurance Eligibility: A Pilot Study on the Disease's Association with Work. Int J Environ Res Public Health. 2018;15. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 65] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 7. | Koçak FA, Tunç H, Tomruk Sütbeyaz S, Akkuş S, Köseoğlu BF, Yılmaz E. Comparison of the short-term effects of the conventional motorized traction with non-surgical spinal decompression performed with a DRX9000 device on pain, functionality, depression, and quality of life in patients with low back pain associated with lumbar disc herniation: A single-blind randomized-controlled trial. Turk J Phys Med Rehabil. 2018;64:17-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Lener S, Wipplinger C, Hartmann S, Thomé C, Tschugg A. The impact of obesity and smoking on young individuals suffering from lumbar disc herniation: a retrospective analysis of 97 cases. Neurosurg Rev. 2020;43:1297-1303. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 9. | Kim MG, Ahn YS. Associations between lower back pain and job types in South Korean male firefighters. Int J Occup Saf Ergon. 2021;27:570-577. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 10. | Wilder DG, Pope MH, Frymoyer JW. The biomechanics of lumbar disc herniation and the effect of overload and instability. J Spinal Disord. 1988;1:16-32. [PubMed] |
| 11. | Gugliotta M, da Costa BR, Dabis E, Theiler R, Jüni P, Reichenbach S, Landolt H, Hasler P. Surgical versus conservative treatment for lumbar disc herniation: a prospective cohort study. BMJ Open. 2016;6:e012938. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 77] [Cited by in RCA: 120] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 12. | Chiba K, Matsuyama Y, Seo T, Toyama Y. Condoliase for the Treatment of Lumbar Disc Herniation: A Randomized Controlled Trial. Spine (Phila Pa 1976). 2018;43:E869-E876. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 59] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 13. | Momenzadeh S, Koosha A, Kazempoor Monfared M, Bairami J, Zali A, Ommi D, Hosseini B, Hashemi M, Sayadi S, Aryani R, Nematollahi F, Nematollahi L, Barati M. The Effect of Percutaneous Laser Disc Decompression on Reducing Pain and Disability in Patients With Lumbar Disc Herniation. J Lasers Med Sci. 2019;10:29-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 14. | Previnaire JG, De Bont N, Bordi H, Senal N, Mortier PE. Open surgery for haemorrhoids in persons with spinal cord injury. Spinal Cord Ser Cases. 2018;4:35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 15. | II, Pasechnik IN, Gubaidullin RR, Reshetnikov EA, Berezenko MN. [Accelerated postoperative rehabilitation: multidisciplinary issue (Part 1)]. Khirurgiia (Mosk). 2015;(9):4-8. Russian. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 16. | Fan G, Guan X, Zhang H, Wu X, Gu X, Gu G, Fan Y, He S. Significant Improvement of Puncture Accuracy and Fluoroscopy Reduction in Percutaneous Transforaminal Endoscopic Discectomy With Novel Lumbar Location System: Preliminary Report of Prospective Hello Study. Medicine (Baltimore). 2015;94:e2189. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 29] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 17. | Choi G, Modi HN, Prada N, Ahn TJ, Myung SH, Gang MS, Lee SH. Clinical results of XMR-assisted percutaneous transforaminal endoscopic lumbar discectomy. J Orthop Surg Res. 2013;8:14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 40] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 18. | Rogerson A, Aidlen J, Jenis LG. Persistent radiculopathy after surgical treatment for lumbar disc herniation: causes and treatment options. Int Orthop. 2019;43:969-973. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 55] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 19. | Postacchini F, Postacchini R. Operative management of lumbar disc herniation : the evolution of knowledge and surgical techniques in the last century. Acta Neurochir Suppl. 2011;108:17-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 50] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 20. | Ahn Y, Lee SH, Park WM, Lee HY, Shin SW, Kang HY. Percutaneous endoscopic lumbar discectomy for recurrent disc herniation: surgical technique, outcome, and prognostic factors of 43 consecutive cases. Spine (Phila Pa 1976). 2004;29:E326-E332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 199] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 21. | Pan M, Li Q, Li S, Mao H, Meng B, Zhou F, Yang H. Percutaneous Endoscopic Lumbar Discectomy: Indications and Complications. Pain Physician. 2020;23:49-56. [PubMed] |
| 22. | Heider FC, Mayer HM. [Surgical treatment of lumbar disc herniation]. Oper Orthop Traumatol. 2017;29:59-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 23. | Delgado-López PD, Rodríguez-Salazar A, Martín-Alonso J, Martín-Velasco V. [Lumbar disc herniation: Natural history, role of physical examination, timing of surgery, treatment options and conflicts of interests]. Neurocirugia (Astur). 2017;28:124-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 38] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 24. | Di Martino A, Russo F, Denaro L, Denaro V. How to treat lumbar disc herniation in pregnancy? Eur Spine J. 2017;26:496-504. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 25. | Zhang QH. Clinical Study of Three-dimensional Balanced Spine Manipulation Combined with Acupuncture in the Treatment of cervical spondylotic radiculopathy. Jinan University, 2019. |
| 26. | Han DT. [Biomechanical relation of the intervertebral disk, intervertebral foramen and vertebral canal: an experimental study on autopsy specimens]. Zhonghua Wai Ke Za Zhi. 1989;27:581-584, 637. [PubMed] |
| 27. | Zhang SY, Huang P, Huang X, Chen T, Zhao X, Liang CM, Li LX, Tan HZ. [Study on risk factors and predictive model for lumbar intervertebral disc herniation in the rural population]. Zhonghua Liu Xing Bing Xue Za Zhi. 2009;30:1152-1155. [PubMed] |