Published online Sep 26, 2021. doi: 10.12998/wjcc.v9.i27.8044
Peer-review started: April 15, 2021
First decision: April 27, 2021
Revised: May 8, 2021
Accepted: August 20, 2021
Article in press: August 20, 2021
Published online: September 26, 2021
Processing time: 153 Days and 19.5 Hours
Radial nerve palsy due to humeral shaft fracture is the most common peripheral nerve injury associated with long bone fractures. An antegrade nailing surgical technique is becoming popular for the fixation of these fractures with minimal invasiveness. We analyzed nerve recovery in patients with humeral shaft fracture and radial nerve palsy treated with humeral nail fixation without nerve exploration.
To assess the radial nerve recovery rate and time from humeral shaft fracture with surgical treatment using close nailing.
We retrospectively collected data of patients who underwent undergone surgical nail fixation for humeral shaft fractures between October 1, 2016, and March 31, 2020. Subsequently, we analyzed the primary or secondary radial nerve palsy recovery rate and radial nerve motor function recovery time.
The study included 70 patients who underwent surgical treatment for closed- or Gustilo type I open humeral shaft fractures using a nail fixation technique without radial nerve exploration. The patients suffered from primary (n = 5) and secondary (n = 5) radial nerve palsy. A 100% radial nerve recovery rate was achieved. The mean recovery time was 4.3 mo.
The study results indicate full recovery of radial nerve palsies from humeral shaft fracture using close nailing treatment. Surgeons need not be concerned about the occurrence of permanent nerve palsies.
Core Tip: The study results indicate full recovery of radial nerve palsies from humeral shaft fracture using close nailing treatment. Surgeons need not be concerned about the occurrence of permanent nerve palsies.
- Citation: Yeh KL, Liaw CK, Wu TY, Chen CP. Radial nerve recovery following closed nailing of humeral shaft fractures without radial nerve exploration: A retrospective study. World J Clin Cases 2021; 9(27): 8044-8050
- URL: https://www.wjgnet.com/2307-8960/full/v9/i27/8044.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i27.8044
Humeral shaft fractures account for about 3% of all adult fractures, and management includes conservative and surgical treatments. Conservative treatment involves wearing functional braces and is generally applied in a large proportion of patients, achieving a high union rate (94.5%) and a short union time (mean: 10.7 wk)[1,2]. However, the rapid development of locking nail and plate designs over the past few decades has resulted in an increasing number of surgical interventions for treating humeral shaft fractures. In the surgical treatment of humeral fractures using rigid fixation, early range of motion (ROM) training is recommended for patients to prevent prolonged immobilization associated with joint stiffness[3].
Humeral shaft fractures are often complicated by radial nerve palsy, which has a reported incidence of 11.8% to 25.4%, representing the most common peripheral nerve injury associated with bone fractures[1,4]. Humeral shaft fractures are mainly treated by plating or nail fixation techniques.
There is no clear consensus on whether and when the nerve should be intraoperatively explored during plating for fixation of humeral mid-shaft fractures[5]. In a previous retrospective study involving 151 humeral shaft fractures, secondary radial nerve palsy was reported in patients postoperatively (n = 9, 6%). In five of the nine patients investigated, the radial nerve was not exposed during the initial surgery, consequently requiring revision surgery[5]. Some surgeons propose that the radial nerve may be compressed by the plate during surgical fixation using a plate[6], whereby intraoperative nerve exploration can decrease the possibility of secondary radial nerve palsy.
Minimal invasiveness is a major advantage of nail fixation[7]. Closed nailing without nerve exploration causes less iatrogenic damage to the periosteum and thereby enables faster callus formation than using open nailing[8]. However, there have been no reports to date on the recovery rate and recovery time for primary or secondary radial nerve palsies. This study is a retrospective analysis of the prevalence and recovery outcomes of radial nerve palsies associated with humeral shaft fractures treated using humeral closed nailing without radial nerve exploration.
A retrospective study was conducted using data collected from the orthopedic department of our institution involving patients whose trauma episodes occurred between October 2016 and March 2020. Patients with sustained humeral shaft fractures that were treated with humeral nails were included in the study. This study was approved by the institutional review board of Shin Kong Wu Ho-Su Memorial Hospital on August 4, 2020 (Approval number: 20200706R). The study was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. The requirement for informed consent was waived owing to the retrospective study design.
The fractures were classified according to the AO-Müller/Orthopedic Trauma Association (AO/OTA) classification. Fractures at the mid-shaft categorized within the AO/OTA classification as spiral (12 A1, B1), oblique (12 A2, B2), transverse (12 A3), or comminuted (12 C3) were included in the study. Only these four fracture patterns, in line with closed- or Gustilo type I open fractures, were considered for closed humeral nailing.
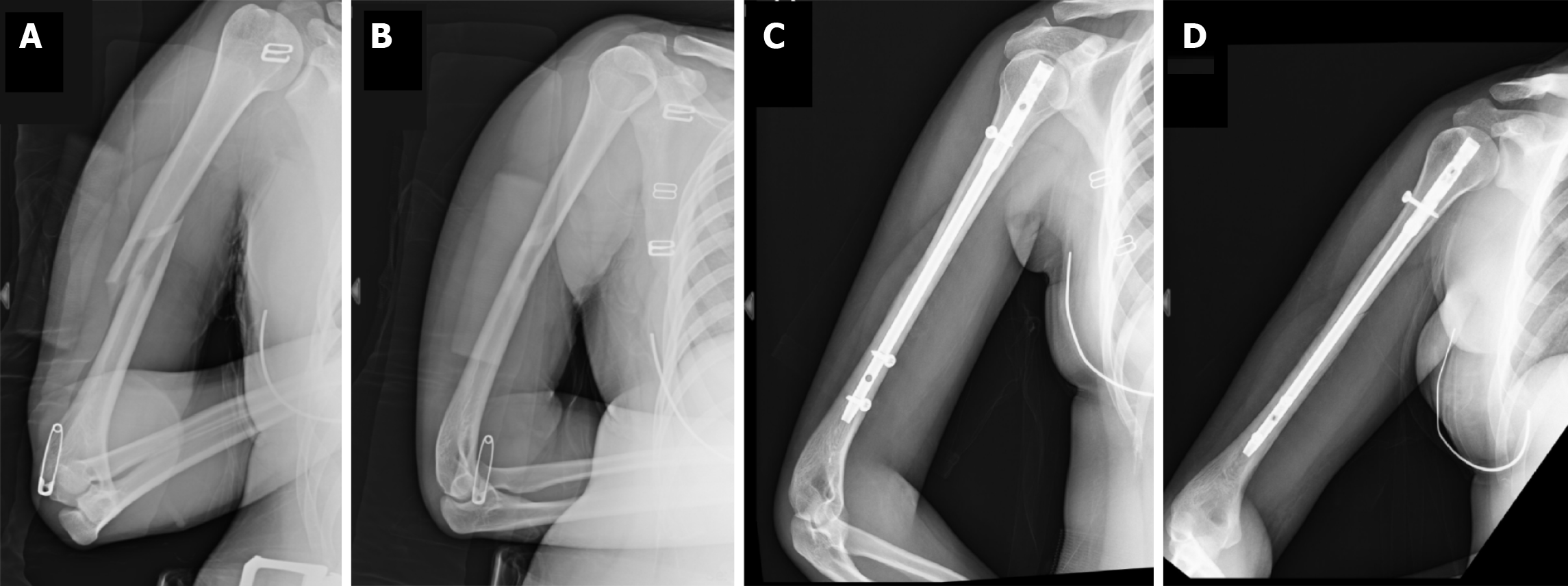
All surgeries were performed by experienced surgeons, that is, either attending physicians or senior resident physicians under the supervision of attending physicians. A skin incision was made, the exact nail entry point was located, and an awl was passed. Subsequently, a guidewire was placed under biplanar c-arm guidance, and closed reduction was performed. Reaming or unreaming was performed based on the patients’ humeral canal size and bone quality, followed by the insertion of MultiLoc humeral implants (Figure 1). The patients were treated at our hospital using the closed nailing technique.
We routinely examined wrist and thumb function preoperatively and postoperatively for all humeral shaft fractures. The Medical Research Council (MRC) scale of muscle strength (Grade 0: No movement; Grade 5: Normal muscle contraction against full resistance) was used to evaluate the strength of the muscles (wrist and digit extensors and extensor pollicis longus and brevis)[9]. If the MRC grade was below Grade 2, we considered the patient to have primary or secondary (postoperative onset) radial nerve palsy.
Patients with radial nerve palsies were required to visit our outpatient clinic every 2 wk postoperatively until recovery. The data of one patient who did not visit our outpatient department postoperatively were excluded from our analysis. Initial radial nerve assessment was performed using electromyography (EMG) and documented. Subsequently, EMG was performed once every 3 mo, as permitted by our public health insurance. Thus, radial nerve recovery was evaluated using two methods of assessment: active ROM of the wrist and an EMG test.
Patients were considered to have recovered from nerve palsy when the radial nerve motor function returned to normal (i.e., the patient regained a muscle strength of grade 4 or 5 for wrist and thumb extension, indicating that the patient could move the joint and had full ROM under moderate resistance).
The MultiLoc nailing system (Synthes, Umkirch, Germany) was used for nail fixation. No other products for humeral nail implants were available at our hospital.
Seventy-two patients with closed- or Gustilo type I open humeral shaft fracture, with a spiral (12 A1, B1), oblique (12 A2, B2), transverse (12 A3), or comminuted (12 C3) AO classification, underwent closed humeral nail fixation between October 2016 and March 2020. We excluded the data of two patients who died within a month following surgery. Participants included 35 males and 35 females aged 18 to 82 years. Of the 70 patients, three had pathological fractures.
Of the 70 patients, five (7.1%) reported primary radial nerve palsy. Secondary radial nerve palsy was also observed in five patients (7.1%). Both patients with primary and secondary nerve palsy achieved 100% radial nerve recovery (Table 1).
| Patient number | Sex | Age (yr) | Primary nerve palsy | Secondary nerve palsy | Recovery time (mo) | Mechanism of injury |
| 1 | Female | 21 | - | + | 3 | Fall from a 1.5-m height |
| 2 | Male | 20 | + | + | 4 | Fall from a 2-m height |
| 3 | Male | 18 | + | + | 4.5 | Motor vehicle accident |
| 4 | Male | 65 | + | + | 4.5 | Fall from a 1-m height |
| 5 | Female | 47 | + | + | 5 | Slippage and fall |
| 6 | Male | 53 | - | + | 5 | Motor vehicle accident |
| 7 | Male | 40 | - | + | 4 | Motor vehicle accident |
| 8 | Female | 62 | - | + | 6 | Motor vehicle accident |
| 9 | Male | 22 | - | + | 3 | Motor vehicle accident |
| 10 | Female | 24 | + | + | 4 | Motor vehicle accident |
The mean time to 80% functional recovery was 4.4 ± 0.4 mo and 4.2 ± 1.3 mo in patients with primary and secondary radial nerve palsy, respectively. The overall average recovery time was 4.3 mo.
The nailing surgical technique for humeral shaft fracture is a minimally invasive procedure. In our experience, stab wounds often result in humeral fractures in patients. The surgical wounds are typically 1 cm to 1.5 cm in size. We have observed that reduced damage to the periosteum, soft tissue, and blood supply at the fracture site resulting from closed nailing decreases the time for bone healing compared to open nailing. Closed humeral nailing produces better cosmetic outcomes and causes less damage to the blood supply of the periosteum than open nailing. However, no studies have been published thus far on the primary or secondary radial nerve recovery rate following the use of the closed nailing technique.
Neuropraxia is the most common radial nerve palsy following humeral shaft fracture and is caused by transient nerve conduction interruption due to traction or compression of the radial nerve. Recovery from neuropraxia is expected to be spontaneous[10]. Axonotmesis, however, is more severe because direct pressure on the axons results in mechanical extrusion of myelin, Wallerian degeneration, and late recovery[11]. Neurotmesis refers to the complete destruction of the axons and Schwann cells, from which there is no chance of recovery without surgical intervention[12]. Fortunately, neurotmesis seldom occurs in humeral mid-shaft fractures complicated with radial nerve palsy.
A previous study revealed that a mean time to full recovery for primary radial nerve palsy of 6.1 mo, which is longer than that observed in our study (4.4 ± 0.4 mo and 4.2 ± 1.3 mo in primary and secondary nerve palsy, respectively) and a mean spontaneous nerve recovery rate of 70.7%[13], which is much lower than that observed in our study (100%). In the aforementioned study[13], patients with humeral shaft fractures were conservatively treated. In these patients, callus formation may have impeded recovery from radial nerve palsies[1]. We could not control the area of callus formation, and this factor contributed to an extended spontaneous radial nerve recovery time and a lower spontaneous radial nerve recovery rate.
No studies have been performed to determine the mean radial nerve recovery time for primary and secondary radial nerve palsies in patients with humeral fractures. However, Shao et al[13] concluded that the rate of spontaneous nerve recovery after secondary radial neuropathy was similar to that after primary radial neuropathy. These findings are in accordance with those reported by Wang et al[14]. Our comparative analysis revealed similar recovery times for primary and secondary radial nerve palsies.
In our study, secondary radial nerve palsy was observed in five patients (7.1%) following humeral shaft fractures. To the best of our knowledge, there have been no previous reports of the incidence of secondary radial nerve palsy in patients with humeral shaft fractures.
Note that neurotmesis affects spontaneous nerve recovery[2]. This condition is caused by direct trauma or iatrogenic damage. Once we eliminated the incidence of neurotmesis, the spontaneous radial nerve recovery rate increased. Radial nerve vulnerability is associated with the lateral intermuscular septum at the lower lateral aspect of the humerus and fractures at the posterior mid-shaft of the humerus where the nerve lies in contact with the bone[11,15-17]. If the trauma involves external rotation and the fracture site is at the proximal-distal or distal end of the humeral shaft based on dividing the shaft into fifths, primary radial nerve injury caused by direct radial nerve entrapment may occur[18]. In these situations, using the closed antegrade nailing technique to treat patients may increase the risk of failure of radial nerve spontaneous recovery.
Given the high incidence of secondary radial nerve palsy in patients undergoing nailing fixation, we emphasize surgical strategies to prevent iatrogenic radial nerve transection due to the potential impact on spontaneous nerve recovery. Distal locking screws for the MultiLoc nailing system are inserted using a free-hand fluoroscopic method. Overpenetration of the medial cortex with distal locking screws using anterior-posterior and lateral-medial locking techniques has been reported to be associated with an increased risk of neurovascular complications, including radial and lateral cutaneous nerve injuries[19,20]. White et al[21] suggested that posterior-to-anterior drilling for distal locking screws can prevent neurovascular injury. Moreover, adequate soft tissue dissection before drilling and the use of drilling protectors can reduce the occurrence of neurovascular complications. However, iatrogenic nerve damage is sometimes unpredictable.
The incidence of humeral shaft fractures is 3%, and some surgeons in our hospitals treat humeral shaft fractures using the plating technique. These factors contributed to the small sample size. Despite the small cohort studied, we concluded that surgeons need not be concerned about permanent radial nerve damage in cases of primary or secondary radial nerve palsies when managing patients with humeral shaft fractures. We will collect further data on patients treated with closed nail fixation for humeral shaft fractures. The results of the present observational study can provide guidance to surgeons regarding the radial nerve recovery rate and the time to recovery and to patients in terms of expectations for recovery.
Primary or secondary radial nerve palsy is a common peripheral nerve injury complication in patients with closed- or Gustilo type I open humeral shaft fractures. In this single-hospital case series, primary and secondary radial nerve palsy occurred at equal incidences of 7.1% of humeral shaft fractures treated using closed nail fixation. Despite the high incidence of radial nerve palsies, a 100% radial nerve recovery rate was achieved following closed nail fixation of humeral shaft fractures. The mean recovery time and the recovery rate are crucial for guiding protocols regarding the expected waiting periods to be followed by surgeons in clinical settings.
Humeral shaft fractures are commonly associated with radial nerve palsies. The emergence of innovative implants has made the minimally invasive nailing procedure increasingly popular. In this study, we surveyed the recovery time and recovery rate of patients with primary or secondary radial nerve palsies.
No studies have been published on radial nerve recovery after nailing fixation treatment for humeral shaft fractures.
The aim of this study was to evaluate the radial nerve recovery time and rate in primary or secondary radial nerve palsy patients treated for humeral shaft fracture with a nailing fixation technique.
In this observational study, we enrolled patients with sustained close or Gustilo open type I humeral shaft fractures who received close nailing fixation treatment between October 2016 and March 2020. We examined the wrist and thumb function preoperatively and postoperatively for all humeral shaft fractures.
The study results demonstrated that all patients who suffered from radial nerve palsies recovered functionally (100%). The mean recovery time was 4.3 mo.
This observational study revealed that all patients with radial nerve palsies who underwent close nailing treatment for humeral shaft fracture achieved full recovery.
Although this observational study was conducted on a small sample, the high radial nerve recovery rate demonstrated that surgeons need not be concerned about permanent nerve injuries.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country/Territory of origin: Taiwan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Cao X, Chisthi MM, Samara AA S-Editor: Liu M L-Editor: A P-Editor: Wang LYT
| 1. | Sarmiento A, Kinman PB, Galvin EG, Schmitt RH, Phillips JG. Functional bracing of fractures of the shaft of the humerus. J Bone Joint Surg Am. 1977;59:596-601. [PubMed] |
| 2. | Papasoulis E, Drosos GI, Ververidis AN, Verettas DA. Functional bracing of humeral shaft fractures. A review of clinical studies. Injury. 2010;41:e21-e27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 82] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 3. | Rämö L, Taimela S, Lepola V, Malmivaara A, Lähdeoja T, Paavola M. Open reduction and internal fixation of humeral shaft fractures vs conservative treatment with a functional brace: a study protocol of a randomised controlled trial embedded in a cohort. BMJ Open. 2017;7:e014076. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 4. | Holstein A, Lewis GM. Fractures of the humerus with radial-nerve paralysis. J Bone Joint Surg Am. 1963;45:1382-1388. [PubMed] |
| 5. | Schwab TR, Stillhard PF, Schibli S, Furrer M, Sommer C. Radial nerve palsy in humeral shaft fractures with internal fixation: analysis of management and outcome. Eur J Trauma Emerg Surg. 2018;44:235-243. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 76] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 6. | Reichert P, Wnukiewicz W, Witkowski J, Bocheńska A, Mizia S, Gosk J, Zimmer K. Causes of Secondary Radial Nerve Palsy and Results of Treatment. Med Sci Monit. 2016;22:554-562. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 7. | Garnavos C. Diaphyseal humeral fractures and intramedullary nailing: Can we improve outcomes? Indian J Orthop. 2011;45:208-215. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 8. | Tahririan MA, Andalib A. Is there a place for open intramedullary nailing in femoral shaft fractures? Adv Biomed Res. 2014;3:157. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Paternostro-Sluga T, Grim-Stieger M, Posch M, Schuhfried O, Vacariu G, Mittermaier C, Bittner C, Fialka-Moser V. Reliability and validity of the Medical Research Council (MRC) scale and a modified scale for testing muscle strength in patients with radial palsy. J Rehabil Med. 2008;40:665-671. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 335] [Cited by in RCA: 405] [Article Influence: 23.8] [Reference Citation Analysis (0)] |
| 10. | Nakamichi K, Tachibana S. Radial nerve entrapment by the lateral head of the triceps. J Hand Surg Am. 1991;16:748-750. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 26] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Lin J. Locked nailing of spiral humeral fractures with or without radial nerve entrapment. Clin Orthop Relat Res. 2002;(403):213-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Latef TJ, Bilal M, Vetter M, Iwanaga J, Oskouian RJ, Tubbs RS. Injury of the Radial Nerve in the Arm: A Review. Cureus. 2018;10:e2199. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 13. | Shao YC, Harwood P, Grotz MR, Limb D, Giannoudis PV. Radial nerve palsy associated with fractures of the shaft of the humerus: a systematic review. J Bone Joint Surg Br. 2005;87:1647-1652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 283] [Cited by in RCA: 262] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 14. | Wang JP, Shen WJ, Chen WM, Huang CK, Shen YS, Chen TH. Iatrogenic radial nerve palsy after operative management of humeral shaft fractures. J Trauma. 2009;66:800-803. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 62] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 15. | Seigerman DA, Choung EW, Yoon RS, Lu M, Frank MA, Gaines LC, Liporace FA. Identification of the radial nerve during the posterior approach to the humerus: a cadaveric study. J Orthop Trauma. 2012;26:226-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 16. | Rocchi M, Tarallo L, Mugnai R, Adani R. Humerus shaft fracture complicated by radial nerve palsy: Is surgical exploration necessary? Musculoskelet Surg. 2016;100:53-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 17. | Moattari M, Kouchesfehani HM, Kaka G, Sadraie SH, Naghdi M. Evaluation of nerve growth factor (NGF) treated mesenchymal stem cells for recovery in neurotmesis model of peripheral nerve injury. J Craniomaxillofac Surg. 2018;46:898-904. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 23] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 18. | Ekholm R, Ponzer S, Törnkvist H, Adami J, Tidermark J. The Holstein-Lewis humeral shaft fracture: aspects of radial nerve injury, primary treatment, and outcome. J Orthop Trauma. 2008;22:693-697. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 47] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 19. | Rupp RE, Chrissos MG, Ebraheim NA. The risk of neurovascular injury with distal locking screws of humeral intramedullary nails. Orthopedics. 1996;19:593-595. [PubMed] |
| 20. | Vural M, Arslantaş A. Delayed radial nerve palsy due to entrapment of the nerve in the callus of a distal third humerus fracture. Turk Neurosurg. 2008;18:194-196. [PubMed] |
| 21. | White WJ, Hawken RM, Giles NC. Posterior to anterior distal locking of humeral intramedullary nails. Ann R Coll Surg Engl. 2012;94:603. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |