Published online Sep 16, 2021. doi: 10.12998/wjcc.v9.i26.7909
Peer-review started: April 26, 2021
First decision: June 6, 2021
Revised: June 15, 2021
Accepted: July 15, 2021
Article in press: July 15, 2021
Published online: September 16, 2021
Processing time: 136 Days and 16.9 Hours
Syphilis is a chronic, classic sexually transmitted disease caused by Treponema pallidum, which can invade almost all organs of the body and produce various symptoms and signs. Although there are some cases of colorectal bleeding caused by syphilis, small intestinal bleeding caused by syphilis is still rare.
A 58-year-old man had experienced recurrent abdominal pain and melena for 3 years. Repeated gastroenteroscopy and computed tomography angiography examinations failed to find bleeding lesions. During the same admission, multiple intestinal ulcers were found by capsule endoscopy, and syphilis was also diagnosed. With a history of atrial fibrillation and chronic pancreatitis, he had undergone mitral valve replacement and tricuspid valvuloplasty for valvular heart disease. After anti-syphilis treatment, the melena and abdominal pain disappeared and his hemoglobin gradually increased. It is considered that gastrointestinal bleeding, chronic pancreatitis, atrial fibrillation, and heart valvular disease may have been caused by syphilis.
This case report found that syphilis can mimic systemic disease and cause intestinal bleeding. In addition, treatment of the disease requires both sexual partners to be treated. Finally, although syphilis is easy to treat, it is more important to consider that bleeding could be caused by syphilis.
Core Tip: Syphilis is considered a sexually transmitted disease, which can affect all systems of the body and cause multiple clinical signs and symptoms. We report a rare case of gastrointestinal hemorrhage caused by Treponema pallidum. The case occurred in an adult male patient. The patient has not only suffered from atrial fibrillation, heart valvular disease, chronic pancreatitis, etc. for more than 10 years, but has also undergone heart valve replacement surgery. In recent years, the patient experienced recurrent unexplained gastrointestinal bleeding. Finally, based on careful analysis, syphilis was identified as the cause of intestinal ulcers that eventually led to gastrointestinal bleeding. This case shows that syphilis is a systemic disease and that it is important to treat syphilis as a couple.
- Citation: Sun DJ, Li HT, Ye Z, Xu BB, Li DZ, Wang W. Gastrointestinal bleeding caused by syphilis: A case report. World J Clin Cases 2021; 9(26): 7909-7916
- URL: https://www.wjgnet.com/2307-8960/full/v9/i26/7909.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i26.7909
Gastrointestinal bleeding is a common disease of the digestive tract. Hematemesis and blackness are its common manifestations. Most gastrointestinal bleeding can be diagnosed by gastroenteroscopy. Intestinal bleeding is often considered when the cause cannot be determined by repeated gastroenteroscopy, and capsule endoscopy, small colonoscopy, abdominal computed tomography angiography (CTA) or magnetic resonance angiography (MRA) can be used to identify lesions in the small intestine. Syphilis is a sexually transmitted infection that can cause systemic disease[1]. Some cases of intestinal bleeding have been reported to be caused by infection with syphilis[2]. Intestinal bleeding itself is uncommon, accounting for about 10% of all cases gastrointestinal bleeding[3], and syphilis is a rare cause of intestinal bleeding.
A 58-year-old man had experienced recurrent abdominal pain and melena for 3 years, but repeated gastroenteroscopy and CTA had failed to find bleeding lesions.
On June 30, 2020, the patient presented to our department with a history of recurrent abdominal pain and melena for 3 years. In June 2017, he developed recurrent localized and dark pain in the upper abdomen without obvious inducement. It was tolerable, lasted for about 1 h, occurred about 3 times a day and was accompanied by thin, textureless melena, dizziness, and fatigue. His symptoms occurred repeatedly. He had gone to major hospitals across the country many times, but there was no clear diagnosis, and conservative treatment was used for alleviation. Two months before admission, the above symptoms progressively worsened. Melena was passed 4-5 times a day, with a total volume of about 200 g, and the dizziness and fatigue were significantly worse than before. After symptomatic treatment of hemostasis in the local hospital, the symptoms were improved, but still existed.
He was diagnosed with syphilis in 2008. Multiple treatments were successful, but the disease recurred shortly afterward. Because of heart valve disease, he underwent a mitral valve replacement and tricuspid valvuloplasty at Fujian Provincial Hospital In 2010. In 2019, he was diagnosed with atrial fibrillation and chronic pancreatitis. Currently, he is taking Betaloc 23.75 mg qd orally.
The patient had a history of unprotected intercourse with multiple sexual partners, a smoking history for 40 years (20 cigarettes a day), and a drinking history for 30 years. There is no family history of infectious or heredity diseases.
On admission, his temperature was 36 ℃, pulse was 66 beats/min, respiration was 18 breaths/min, and blood pressure was 120/80 mmHg. He was conscious and could cooperate in the physical examination. The skin of the whole body was slightly pale. Systemic superficial lymph nodes were not enlarged or tender, the conjunctiva was pale, the lips were slightly pale, carotid artery pulsation was normal, jugular vein was normal, liver jugular vein return sign was negative, and lung physical examination was not remarkable. There was a postoperative scar of about 20 cm in length on the chest, which had healed well. The heart rate was 80 beats/min, the heart rhythm was absolutely uneven, the first heart sound varied in intensity, a systolic murmur was heard in the mitral valve auscultation area, no obvious pathological murmur was heard in the other auscultation area, the fricative consonant was unintentionally included, the abdomen was flat and soft without tenderness or rebound pain, and the abdomen was not lumped. The liver and spleen were not touched, Murphy’s sign was negative, and there was no mobile dullness. Intestinal sounds (4/min) were normal.
The initial hemoglobin of the patient was 78.0 g/L and fecal occult blood was present (++). The syphilis toluidine red unheated serum test (TRUST) was positive; the syphilis titer was 1:2 positive. The white blood cell count, platelets, coagulation function, antinuclear antibody, antinuclear antibody profile, fecal routine, urine routine, alpha fetoprotein, carcinoembryonic antigen, glycogen antigen 199, total iron binding capacity, serum iron, unsaturated iron binding capacity, ferritin, folic acid, vitamin B12, purified protein derivative (PPD tuberculin test, tuberculosis antibody, and tuberculosis T-cell test showed no obvious abnormalities.
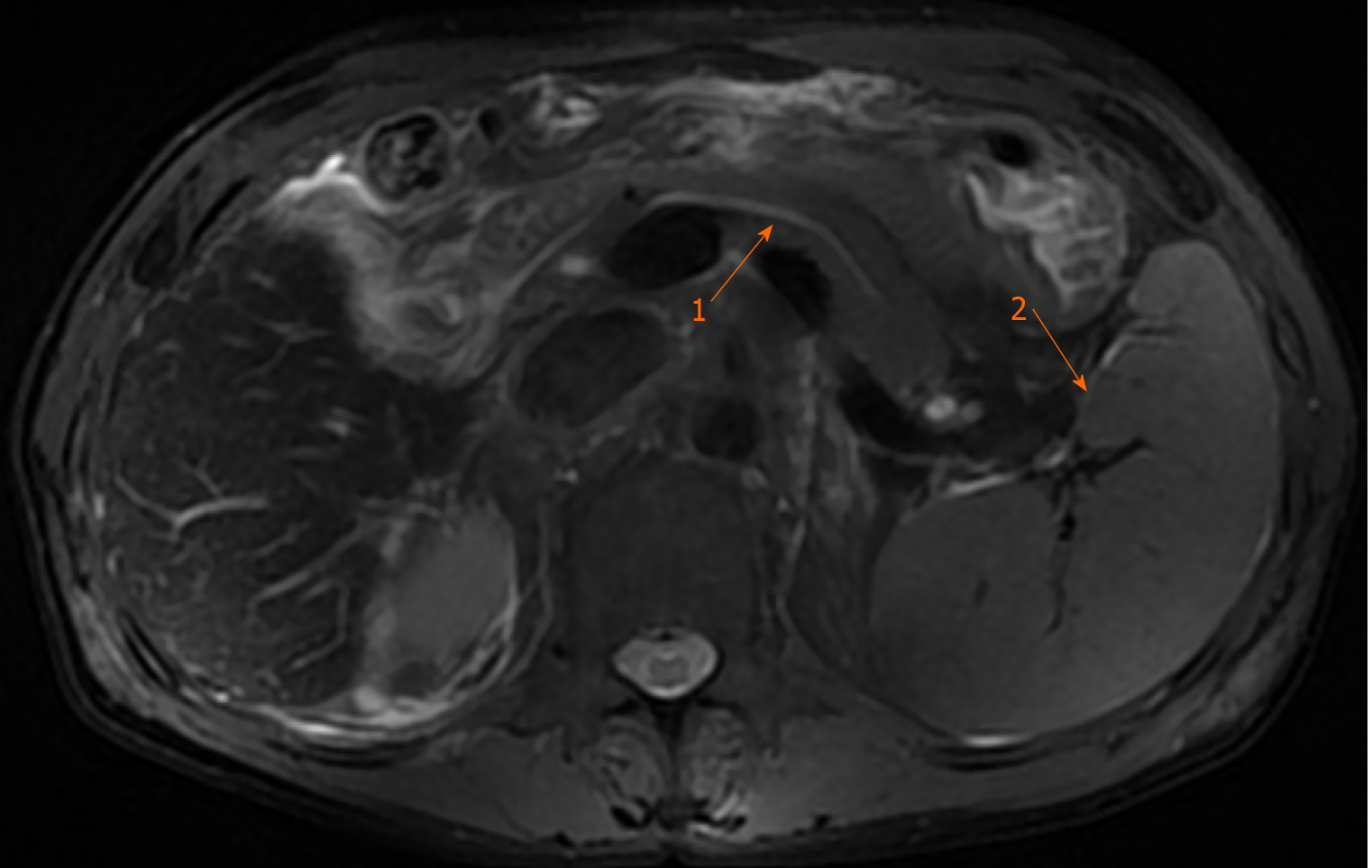
The patient’s upper abdominal magnetic resonance cholangiopancreatography revealed splenomegaly, and dilatation of the intrahepatic and extrahepatic bile ducts and pancreatic ducts (Figure 1).
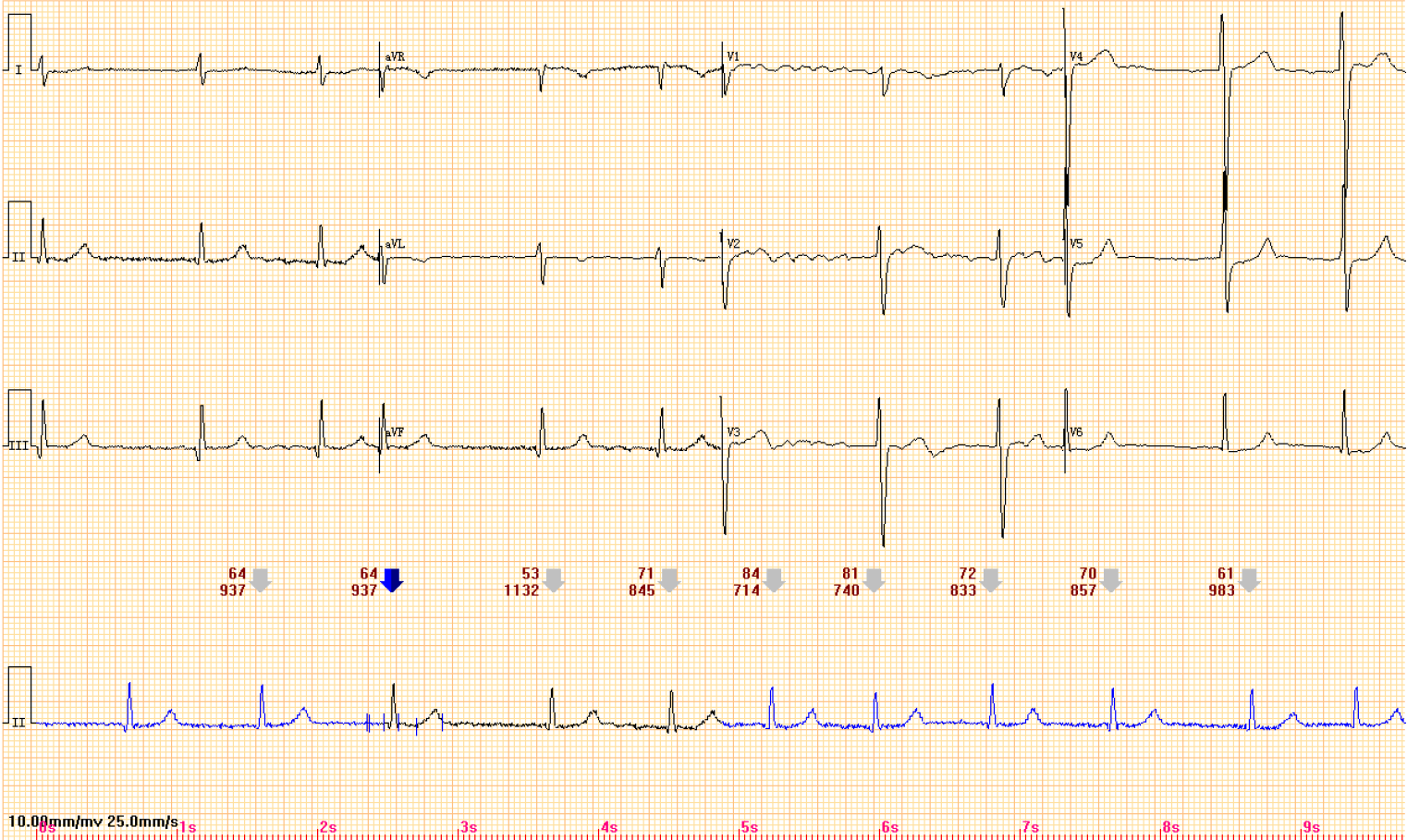
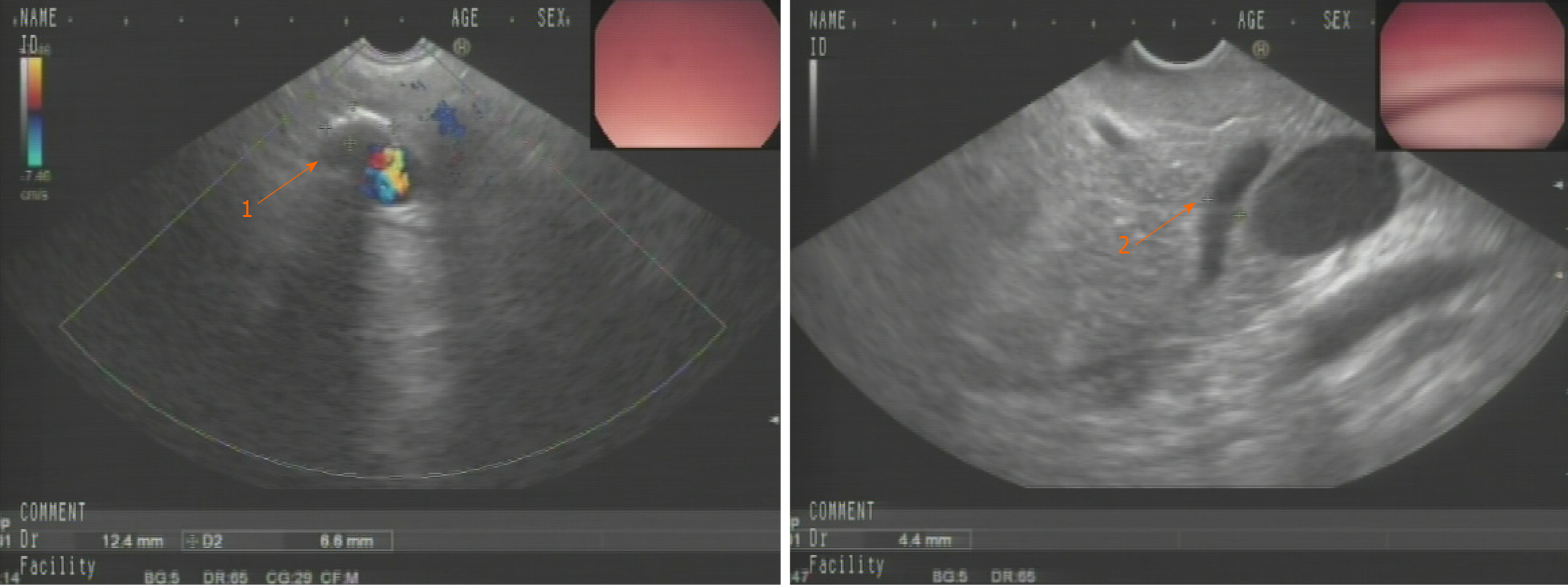
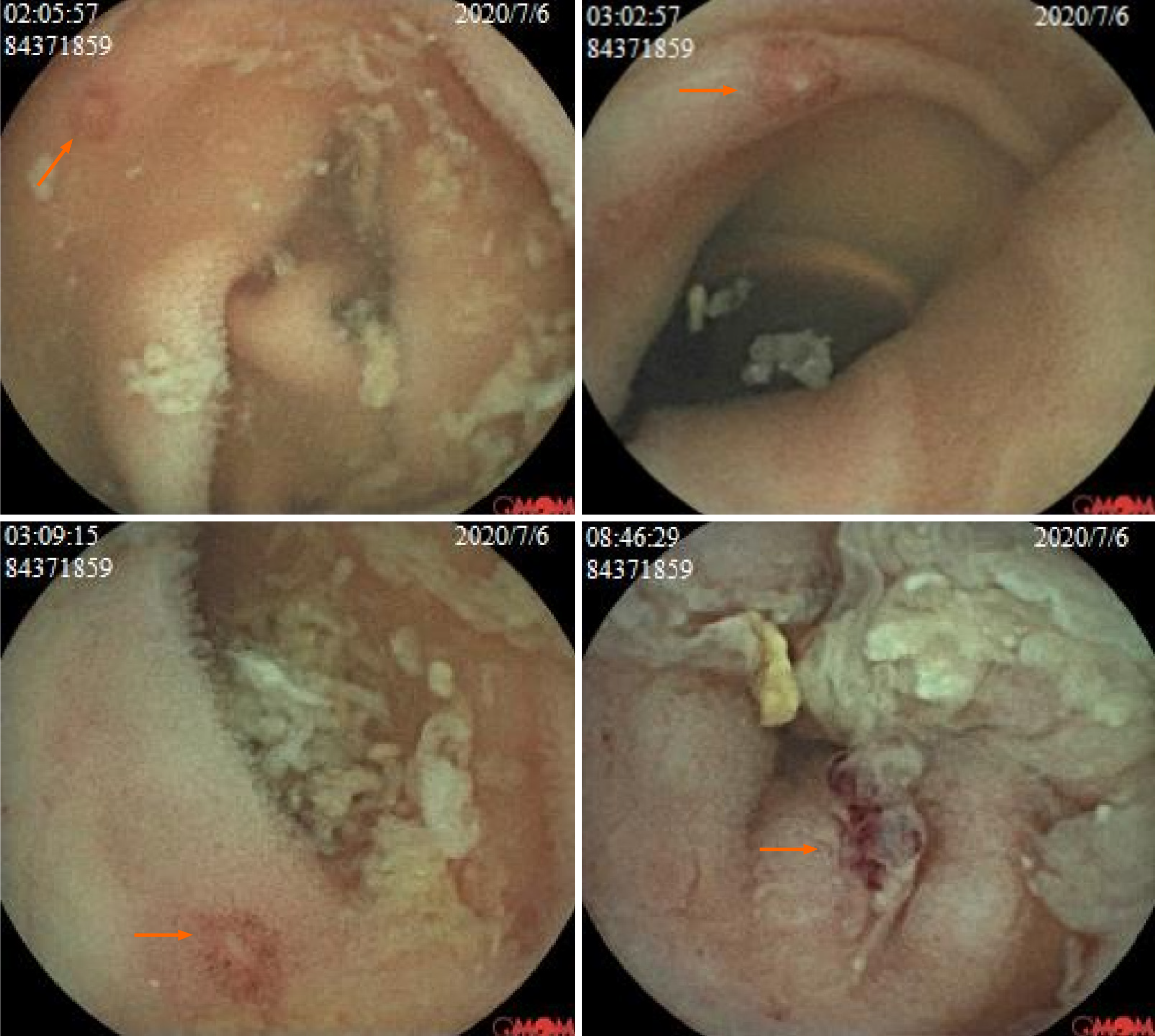
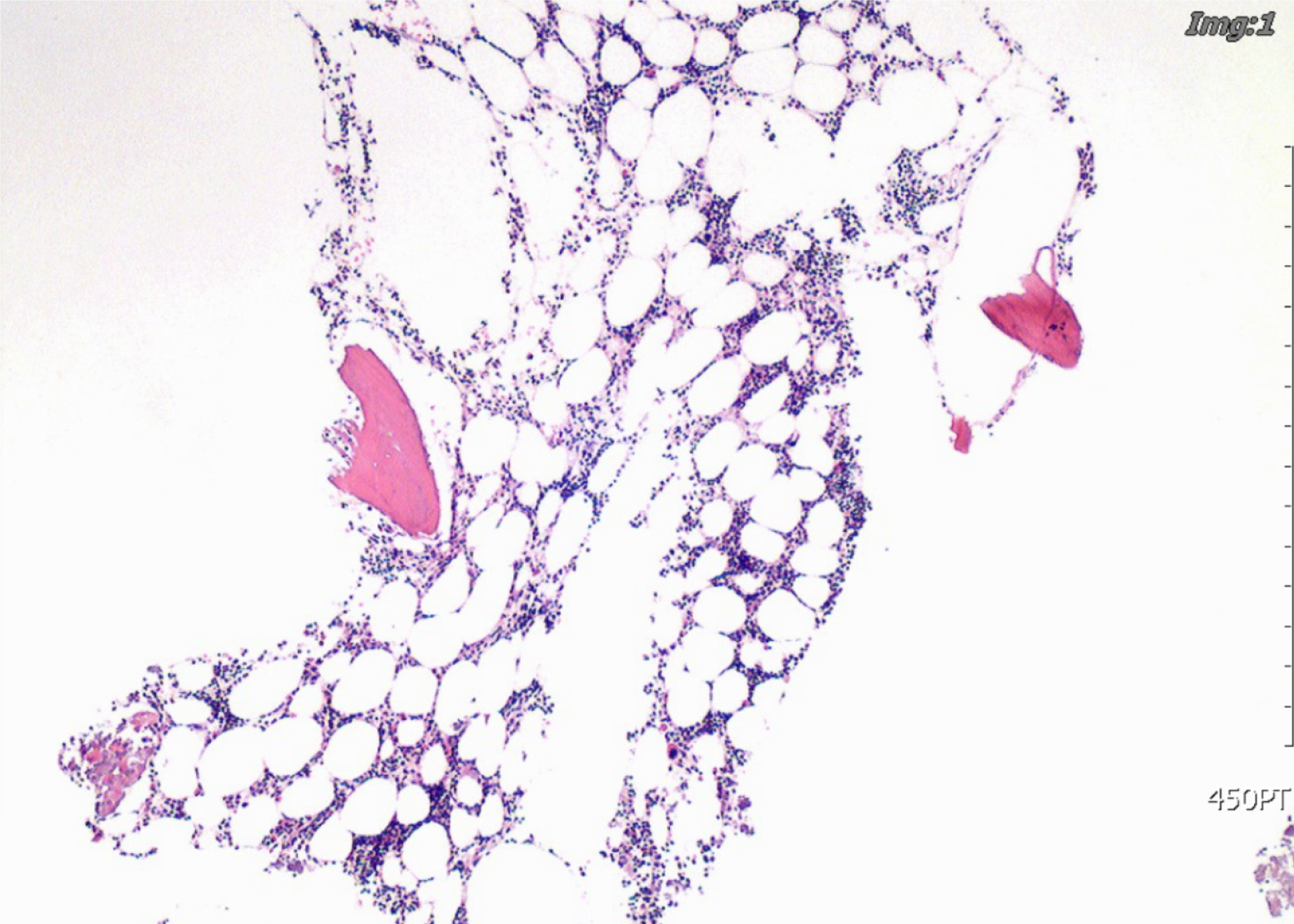
An electrocardiogram indicated atrial fibrillation (Figure 2). Colonoscopy found multiple small ridges in the terminal ileum, and the pathology showed chronic active inflammation and erosive mucosa. Additional gastroscopy showed atrophic gastritis, and pathology of the gastric antrum indicated inflammation, and the Helicobacter pylori test was negative. Ultrasound gastroscopy showed dilatation of pancreatic duct with pancreatic duct stones, which was considered as chronic pancreatitis (Figure 3). A capsule endoscopy was performed to further clarify the bleeding focus of the patient, and multiple intestinal erosions and ulcers were found (Figure 4). The bone marrow puncture smear of the iliac spine showed normal hematopoietic tissue hyperplasia, presence of three-line hematopoietic cells, expanded islands of erythroid cells, hyperplasia of erythroid cells, a reduced granulocytosis ratio, and a scattered distribution of megakaryocytes, which was considered as hyperplastic anemia (Figure 5).
The final diagnosis was minor intestinal bleeding caused by syphilis.
In hospital, the patient was started on benzathine penicillin (2.4 million units intramuscular injection) once weekly for 3 wk for the treatment of syphilis and thrombin (2000 units orally) 3 times daily for 3 consecutive days for the treatment of hemorrhage.
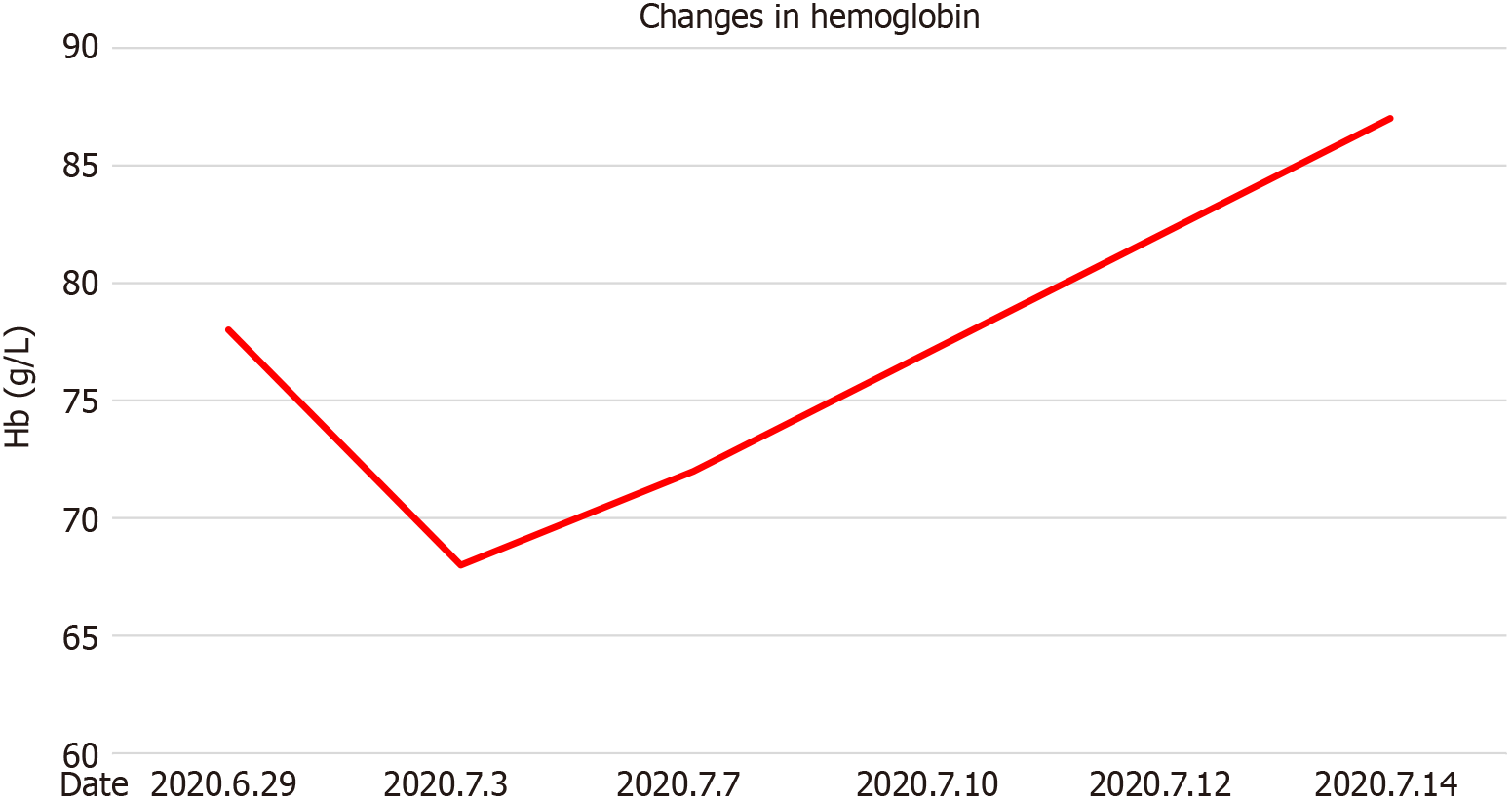
The patient’s hemoglobin gradually decreased from 78 g/L on June 29 to 68 g/L on July 3. After receiving oral thrombin and benzathine penicillin, the patient’s Hb gradually increased to 87 g/L on July 14 without blood transfusion (Figure 6 and Table 1). The patient also contacted her spouse for treatment of syphilis. After 6 mo of follow-up, the patient did not have gastrointestinal bleeding symptoms, such as hematemesis, melena and hematochezia, the Hb gradually recovered to about 120g/L by the second visit, and the syphilis titer was retested (-).
| Factor | ||||||
| Date | 2020.6.29 | 2020.7.3 | 2020.7.7 | 2020.7.10 | 2020.7.12 | 2020.7.14 |
| Hb (g/L) | 78 | 68 | 72 | 77 | 82 | 87 |
Gastrointestinal bleeding is a common digestive tract disease. The main clinical manifestations include hematemesis, melena, and bloody stools. The patient had recurrent melena and positive fecal occult blood accompanied by decreased hemoglobin. Repeated observation of the nasopharynx and oral cavity during hospitalization showed no obvious bleeding foci, which ruled out bleeding from those sites. Thus, the diagnosis of gastrointestinal bleeding was clear. After repeated gastroscopy, colonoscopy, CTA and MRA examinations, no bleeding foci were found, but capsule endoscopy suggested multiple intestinal ulcers. Hence, bleeding caused by multiple intestinal ulcers was considered.
The common causes of multiple intestinal ulcer disease include Bechet’s disease, Crohn’s disease, tuberculosis, cryptogenic multifocal ulcerative stenosis of the small intestine, lymphoma, and drug-induced lesions. There are also many rare diseases that can lead to intestinal ulceration[4-8]. No oral or perineal ulcers were found in this patient, but an ulcer of Bechet’s disease was isolated. It was round, deep, and large, with a clear boundary. The patient also had no history of tuberculosis, cough, or sputum. No obvious abnormalities were found in the PPD, tuberculosis antibody, and tuberculosis T-cell tests. The endoscopic manifestations of Crohn’s disease are longitudinal fissure-like ulcers, paving stone changes, discontinuous lesions, and the mucosa between lesions may be completely normal. This was seen in cryptic multifocal ulcerative stenosis of the small intestine. No lymphoma was detected by endoscopic pathological examination of the terminal ileum and full-abdominal CT, and no lymphoma was detected by capsule endoscopy. The patient had no history of long-term use of drugs that could cause multiple intestinal ulcers. In addition, bone marrow puncture indicated hyperplastic anemia that was consistent with the manifestations of gastrointestinal bleeding, which could then be identified as bleeding without a hematologic causing bleeding. Therefore, the gastrointestinal bleeding of this patient was considered to be caused by other diseases.
Syphilis is a sexually transmitted disease. Early syphilis is usually cured in 4-6 wk. Late syphilis leads to systemic organ damage, such as aortitis, meningitis and uveitis[1]. There are also many reports of patients with cardiovascular syphilis needing mitral valve and tricuspid valve surgery[9-11]. In recent years, some rare cases of syphilis infection with formation of colorectal inflammatory masses that caused gastro
This case report found that syphilis can mimic systemic disease and cause intestinal bleeding. In addition, the treatment of the disease requires both sexual partners to be treated. Finally, although syphilis is easy to treat, it is more important to consider whether bleeding might be caused by syphilis.
Manuscript source: Unsolicited manuscript
Corresponding Author's Membership in Professional Societies: Chinese Society of Digestive Endoscopy; Fujian Provincial Society of Digestive Endoscopy.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Plagens-Rotman K S-Editor: Ma YJ L-Editor: Filipodia P-Editor: Wang LYT
| 1. | Plagens-Rotman K, Przybylska R, Gerke K, Piskorz-Szymendera M, Tomaszewska M, Sadowska-Przytocka A, Adamski Z, Czarnecka-Operacz M. Syphilis and a pregnant woman: a real danger for the woman and the child. Postepy Dermatol Alergol. 2019;36:119-124. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Serigado J, Lewis E, Kim G. Rectal bleeding caused by a syphilitic inflammatory mass. BMJ Case Rep. 2019;12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Gerson LB, Fidler JL, Cave DR, Leighton JA. ACG Clinical Guideline: Diagnosis and Management of Small Bowel Bleeding. Am J Gastroenterol. 2015;110:1265-87; quiz 1288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 368] [Cited by in RCA: 447] [Article Influence: 44.7] [Reference Citation Analysis (1)] |
| 4. | Lichtenstein GR, Loftus EV, Isaacs KL, Regueiro MD, Gerson LB, Sands BE. ACG Clinical Guideline: Management of Crohn's Disease in Adults. Am J Gastroenterol. 2018;113:481-517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 612] [Cited by in RCA: 927] [Article Influence: 132.4] [Reference Citation Analysis (0)] |
| 5. | Hatemi G, Christensen R, Bang D, Bodaghi B, Celik AF, Fortune F, Gaudric J, Gul A, Kötter I, Leccese P, Mahr A, Moots R, Ozguler Y, Richter J, Saadoun D, Salvarani C, Scuderi F, Sfikakis PP, Siva A, Stanford M, Tugal-Tutkun I, West R, Yurdakul S, Olivieri I, Yazici H. 2018 update of the EULAR recommendations for the management of Behçet's syndrome. Ann Rheum Dis. 2018;77:808-818. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 243] [Cited by in RCA: 286] [Article Influence: 40.9] [Reference Citation Analysis (0)] |
| 6. | Thanassi W, Behrman AJ, Reves R, Russi M, Swift M, Warkentin J, Miyakawa R, Wegener D, Budnick L, Murray E, Scarpita A, Hurst BJ, Foster-Chang S, Mathew T, Gruden M, Higashi J, Hudson TW 3rd. Tuberculosis Screening, Testing, and Treatment of US Health Care Personnel: ACOEM and NTCA Joint Task Force on Implementation of the 2019 MMWR Recommendations. J Occup Environ Med. 2020;62:e355-e369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Zelenetz AD, Gordon LI, Abramson JS, Advani RH, Bartlett NL, Caimi PF, Chang JE, Chavez JC, Christian B, Fayad LE, Glenn MJ, Habermann TM, Lee Harris N, Hernandez-Ilizaliturri F, Kaminski MS, Kelsey CR, Khan N, Krivacic S, LaCasce AS, Mehta A, Nademanee A, Rabinovitch R, Reddy N, Reid E, Roberts KB, Smith SD, Snyder ED, Swinnen LJ, Vose JM, Dwyer MA, Sundar H. NCCN Guidelines Insights: B-Cell Lymphomas, Version 3.2019. J Natl Compr Canc Netw. 2019;17:650-661. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 116] [Article Influence: 23.2] [Reference Citation Analysis (0)] |
| 8. | Hoppe RT, Advani RH, Ai WZ, Ambinder RF, Armand P, Bello CM, Benitez CM, Bierman PJ, Boughan KM, Dabaja B, Gordon LI, Hernandez-Ilizaliturri FJ, Herrera AF, Hochberg EP, Huang J, Johnston PB, Kaminski MS, Kenkre VP, Khan N, Lynch RC, Maddocks K, McConathy J, McKinney M, Metzger M, Morgan D, Mulroney C, Rabinovitch R, Rosenspire KC, Seropian S, Tao R, Winter JN, Yahalom J, Burns JL, Ogba N. Hodgkin Lymphoma, Version 2.2020, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2020;18:755-781. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 88] [Article Influence: 17.6] [Reference Citation Analysis (0)] |
| 9. | Nomura R, Yamazaki F, Egawa Y. Syphilitic aortitis: chronic left coronary ostial occlusion and aortic regurgitation with aortitis. Gen Thorac Cardiovasc Surg. 2021;69:736-739. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | De Martino A, Bortolotti U, Pucci A. The comeback of syphilitic aortitis. Cardiovasc Pathol. 2020;49:107229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Yuan SM. Syphilitic aortic aneurysm. Z Rheumatol. 2018;77:741-748. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 12. | Xu L, Han F. Neurosyphilis complicated with pial arteriovenous fistula: A rare case report. Medicine (Baltimore). 2019;98:e17770. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 13. | Wallace HE, Harrison LC, Monteiro EF, Jones RL. The Great Pretender: early syphilis mimicking acute sclerosing cholangitis. Frontline Gastroenterol. 2015;6:178-181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Quesada D, Stapleton M, Heer J, Aguìñiga-Navarrete P, Kim L. An Unusual Case of Unilateral Papilledema. Clin Pract Cases Emerg Med. 2019;3:444-445. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 15. | Kern C, Elmoursi A, Blake C, Hoellein A. Syphilis Hepatitis Presenting as a Mimic of Primary Biliary Cholangitis. ACG Case Rep J. 2020;7:e00497. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 16. | Imoto W, Arima H, Yamada K, Kanzaki T, Nakagawa C, Kuwabara G, Yamairi K, Shibata W, Oshima K, Watanabe T, Asai K, Kaneko Y, Kawaguchi T, Goto T, Kakeya H. Incidental finding of neurosyphilis with intracranial hemorrhage and cerebral infarction: A case report. J Infect Chemother. 2021;27:521-525. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 17. | da Silva BA, Soi TS, Cameron D, Karikkineth AC, Williams RB. Syphilis, Hepatitis, and Pancreatitis: Is the Uncommon Becoming Common in the HIV(+) Patient? Case Rep Infect Dis. 2013;2013:293823. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |