Published online Aug 26, 2021. doi: 10.12998/wjcc.v9.i24.7053
Peer-review started: April 22, 2021
First decision: May 24, 2021
Revised: May 29, 2021
Accepted: June 22, 2021
Article in press: June 22, 2021
Published online: August 26, 2021
Processing time: 123 Days and 13.5 Hours
Fracture risk assessment in children with benign bone lesions of long bones remains poorly investigated.
To investigate the risk factors for pathological fracture in children with benign bone lesions and to propose a modified scoring system for quantitative analysis of the pathologic fracture risk.
We retrospectively reviewed 96 pediatric patients with benign bone lesions. We compared radiographic and clinical features between 40 patients who had fractures through a benign bone lesion and 56 who had no fracture. Information including histological diagnosis, anatomical site, radiographic appearance, severity of pain, and lesion size was recorded for the patients. A modified scoring system was proposed to predict the risk of fracture.
The univariate comparisons showed a significant difference between the fracture and non-fracture groups in terms of lesion type, pain, lesion-to-bone width, and axial cortical involvement of the patients (P < 0.05). Lesion type, pain, lesion-to-bone width, and axial cortical involvement were independently correlated with an increased risk of fracture. The mean score of the fracture group was 7.89, whereas the mean score of the non-fracture group was 6.01. The optimum cut-off value of the score to predict pathological fracture was 7. The scoring system had a sensitivity of 70% and a specificity of 80% for detecting patients with fractures. The Youden index was 0.5, which was the maximum value. The area under the receiver operator characteristic was 0.814.
Lesion type, pain, lesion-to-bone width, and axial cortical involvement are risk factors for pathological fracture. The modified scoring system can provide evidence for clinical decision-making in children with benign bone lesions. A bone lesion with a total score > 7 indicates a high risk of a pathologic fracture and is an indication for prophylactic internal fixation.
Core Tip: The purpose of this study was to investigate the risk factors of pathological fracture in children with benign bone lesions and to propose a modified scoring system for quantitative analysis of the pathologic fracture risks. As a fracture predictive tool, the modified scoring system can be used to evaluate before treatment and provide reference for surgical decision-making.
- Citation: Li HB, Ye WS, Shu Q. Fracture risk assessment in children with benign bone lesions of long bones. World J Clin Cases 2021; 9(24): 7053-7061
- URL: https://www.wjgnet.com/2307-8960/full/v9/i24/7053.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i24.7053
Benign bone lesions refer to an inhomogeneous group of pathologic entities including benign and phymatoid lesions[1]. Most benign bone lesions occur in skeletally immature individuals and are generally located in the long bones. Benign bone lesions may be asymptomatic or incidentally discovered because of their insidious onset. After confirming that the lesion is benign, surgeons should undertake a fracture risk assessment and evaluate the treatment indications[2]. When an enlarging benign lesion occurs in the long bone of the extremities, pathologic fracture may occur frequently even with minimal trauma. Pathologic fracture will lead to fracture-related pain, deformity, and immobility[3]. Therefore, fracture prevention is a management priority[4].
Current management strategies for benign bone lesions include conservative treatment and surgical treatment. The option of treatment remains a subject of debate among surgeons. Conservative treatment involves close observations, avoiding weight-bearing, and immobilization with a brace. This is suitable for asymptomatic and small lesions[5]. Surgical treatment, including steroid injection, injection of bone graft or autologous bone marrow, open curettage, and bone grafting with or without stabilization of the lesion with internal fixation, is mainly used for moderate–large lesions[6-8]. The key critical point in clinical decision-making for the treatment of benign bone lesions hinges on whether the given lesion altering the strength of the bone will increase the risk of pathological fracture.
Previous studies have determined the risk factors of pathological fracture based on patient pain, site of lesion, lesion type, and size of lesion[9,10]. The populations of these studies were mainly adult patients with metastatic bone disease; however, rare research has investigated pediatric patients with benign bone lesions[11]. Therefore, we investigated the risk factors of pathological fracture in children with benign bone lesions. Our secondary aim was to propose a modified scoring system for quantitative analysis of the pathologic fracture risks.
After obtaining approval from our hospital’s ethics committee (2020-IRB-052), a retrospective study was performed on all pediatric patients with long bones affected by benign bone lesions in our hospital between January 2015 and December 2018. Informed consent form was signed by all parents of patients in the study. All methods were performed in accordance with the relevant guidelines and regulations. Patients who had a malignant tumor or had a history of previous treatment before admission to our hospital were excluded from the study. All patients underwent fine-needle or open biopsy for histological diagnosis. All patients who suffered spontaneous fractures or fractures that occurred as a consequence of minimal trauma were included in this study. Patients with pathologic fractures caused by adequate trauma or multiple pathologic fractures were excluded. This group of patients was defined as the fracture group. The non-fracture group consisted of patients without fractures. We reviewed all available patient information and extracted relevant details, including patients’ age, gender, histological diagnosis, location of lesion, lesion type, severity of pain, and lesion size.
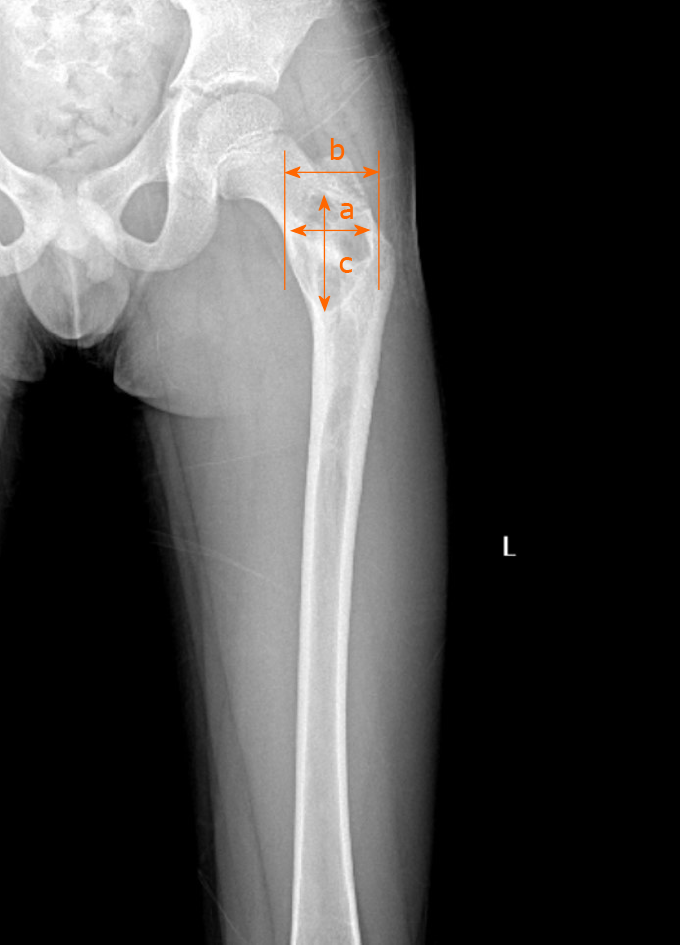
For both the fracture and non-fracture groups, the initial plain radiographs were reviewed to identify the location of the lesion (upper or lower limb), lesion type (osteoblastic, mixed, or osteolytic), and lesion size. The lesion size, including lesion-to-bone width and axial cortical involvement, were calculated based on anteroposterior or lateral radiographs (Figure 1). The lesion-to-bone width was calculated by the maximum ratio of lesion width to transverse width at the level of the lesion. Axial cortical involvement was measured by the largest longitudinal measurement of the entire lesion. The degree of pain was evaluated according to the Numerical Rating Scale. A score of 1-5 was defined as mild pain and 6-10 as severe pain.
A modified scoring system was proposed to predict the risk of fracture, using variables including lesion-to-bone width, axial cortical involvement, lesion type, and severity of pain (Table 1). We hypothesized that these variables were the risk factors for fracture. To validate the proposed scoring system, patients were scored by two blinded reviewers.
| Score | ||||
| Risk factor | 0 | 1 | 2 | 3 |
| Lesion-to-bone width | None | 1/3 | 1/3-2/3 | > 2/3 |
| Axial cortical involvement | None | < 20 mm | 20-30 mm | > 30 mm |
| Pain | None | Mild | severe | |
| Lesion type | Blastic | Mixed | Lytic |
Univariate analysis was conducted using Fisher’s exact test or chi-square test for categorical data (e.g., gender, histological diagnosis, anatomical site, etc.), or using Student’s t-test for continuous data (e.g., age) between the fracture and non-fracture groups. A P < 0.05 was considered statistically significant. Non-conditional logistic regression analysis was used to identify potential risk factors. Fracture-related variables at a P value of 0.05 or less on univariate analysis were placed in a non-conditional logistic regression equation. The interobserver reliability was determined by the interclass correlation coefficient. The diagnostic performances were detected at different cutoff values. The receiver operator characteristic (ROC) curve was drawn and applied to area calculation.
Ninety-six patients were included in this study. We included 55 boys and 41 girls with an average age of 8.3 years (range: 2.2-15.2 years). Twenty-five patients had a simple bone cyst, 18 aneurysmal bone cyst, 19 fibrous dysplasia, 11 non-ossifying fibroma, 15 Langerhans histiocytosis, 4 endochondroma, and 4 osteoblastoma. Thirty-three lesions were located in the upper limb and 63 in the lower limb. Univariate comparisons between the fracture and non-fracture groups showed a statistical difference in lesion type, pain, lesion-to-bone width, and axial cortical involvement (P < 0.05). No significant differences in age, sex, histological diagnosis, and lesion location were found between the two groups (Table 2). Clinical and radiographic features, including lesion type, pain, lesion-to-bone width, and axial cortical involvement, were assessed using non-conditional logistical regression analysis to determine whether any of these features were associated with fracture. Lesion type [P = 0.021, odds ratio (OR) = 3.247], pain (P = 0.007, OR = 2.847), lesion-to-bone width (P = 0.039, OR = 2.362), and axial cortical involvement (P = 0.047, OR = 1.885) were independent risk factors for pathologic fracture.
| Characteristic | Fracture group (n = 40) | Non-fracture group (n = 56) | P value |
| Mean (SD) | Mean (SD) | Univariate | |
| Age (yr) | 8.1 ± 3.6 | 8.3 ± 3.5 | 0.77 |
| Sex | |||
| Females | 24 | 31 | 0.65 |
| Males | 16 | 25 | |
| Histological diagnosis | 0.58 | ||
| Simple bone cyst | 10 | 15 | |
| Aneurysmal bone cyst | 7 | 11 | |
| Fibrous dysplasia | 8 | 11 | |
| Non-ossifying fibroma | 3 | 8 | |
| Langerhans histiocytosis | 6 | 9 | |
| Endochondroma | 3 | 1 | |
| Osteoblastoma | 3 | 1 | |
| Lesion location | 0.33 | ||
| Upper limp | 16 | 17 | |
| Lower limp | 24 | 39 | |
| Lesion type | 0.021 | ||
| Osteolytic | 28 | 29 | |
| Mixed | 12 | 19 | |
| Osteoblastic | 0 | 8 | |
| Pain | 0.004 | ||
| Severe | 12 | 4 | |
| Mild | 17 | 22 | |
| None | 11 | 30 | |
| Lesion-to-bone width | 0.006 | ||
| Size > 2/3 | 24 | 15 | |
| 1/3 < Size ≤ 2/3 | 14 | 30 | |
| Size ≤ 1/3 | 2 | 10 | |
| Axial cortical involvement | |||
| > 30 mm | 31 | 24 | 0.002 |
| 30 mm ≥ Size > 20 mm | 5 | 12 | |
| ≤ 20 mm | 4 | 20 |
The mean and median values of different observers are shown in Table 3. No significant differences were found between the two observers. The interclass correlation coefficient was 0.984. The mean score of the fracture group was 7.89, whereas the mean score of the non-fracture group was 6.01 (Table 4). Compared with the non-fracture group, the fracture group showed a significantly higher mean score (P = 0.00).
| Observer | Total population | Fracture group | Non- fracture group | ||||||
| No. patient | Mean | Median | No. patient | Mean | Median | No. patient | Mean | Median | |
| A | 96 | 6.88 | 7 | 40 | 7.98 | 8 | 56 | 6.01 | 6 |
| B | 96 | 6.91 | 7 | 40 | 8.00 | 8 | 56 | 6.12 | 6 |
| No. patient | Score | Mean (SD) | P value | |
| Fracture group | 40 | 5-10 | 7.98 (1.37) | 0.00 |
| Non-fracture group | 56 | 3-9 | 6.01 (1.55) |
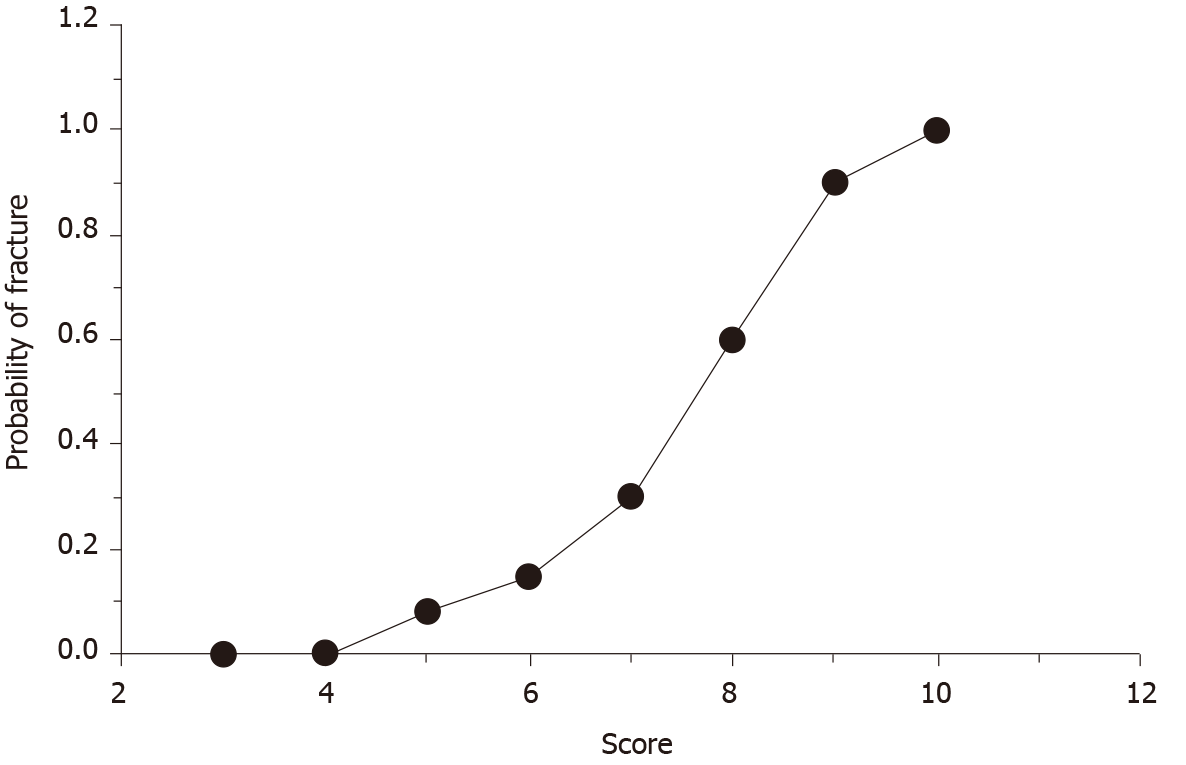
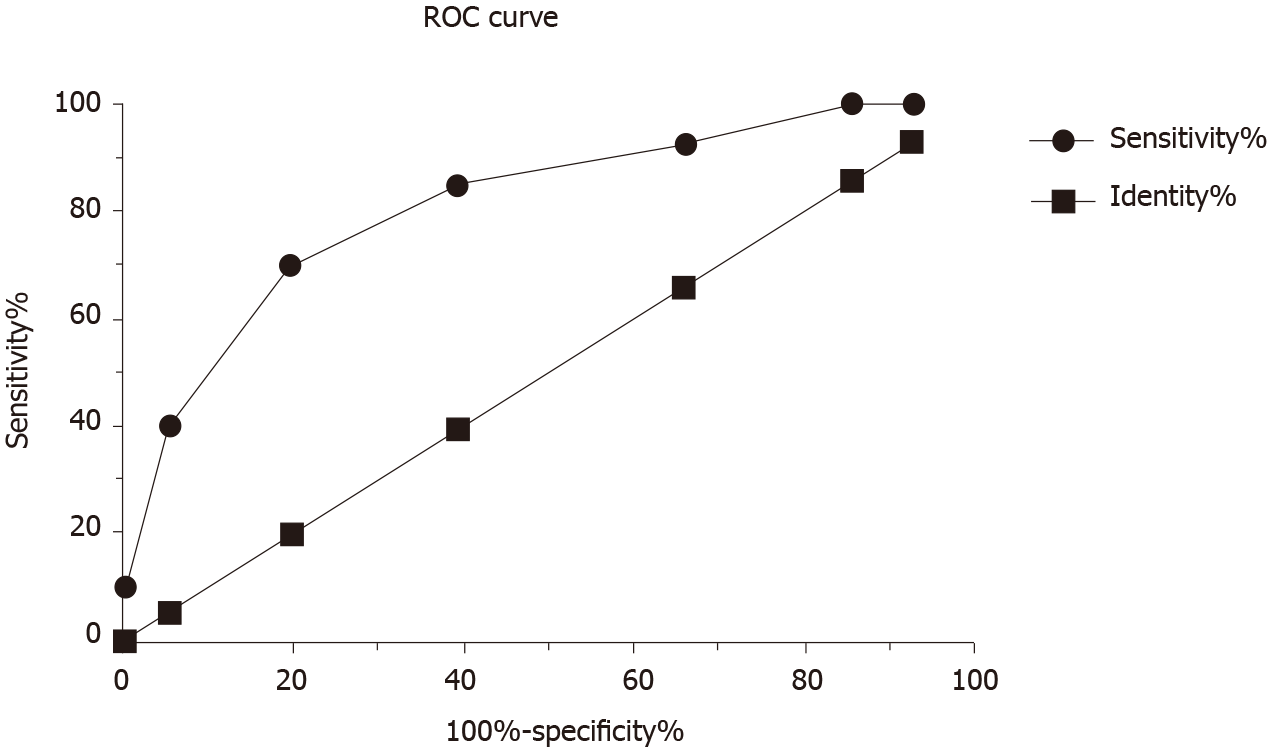
Diagnostic indices, including sensitive, specificity, positive predictive, negative predictive, accuracy, and Youden indexes calculated across varying cutoff levels, are shown in Table 5. When the cutoff value was 7, a sensitivity of 70% and a specificity of 80% can be reached for detecting patients with fractures. The Youden index was 0.5, which was the maximum value, indicating the highest diagnostic efficiency. The curve of fracture probability illustrated that fracture risk changed with increasing score (Figure 2). As shown in Figure 3, the area under the ROC curve was 0.814, which demonstrated that the scoring method gave an acceptable level of accuracy.
| Score | Fracture | Non-fracture | Sensitivity | Specificity | Positive predictive value | Negative predictive value | Accuracy | Fracture probability | Youden index |
| 3 | 0 | 4 | 100% | 7% | 43% | 100% | 46% | 0 | 0.07 |
| 4 | 0 | 4 | 100% | 14% | 45% | 100% | 50% | 0 | 0.14 |
| 5 | 3 | 11 | 92% | 34% | 50% | 86% | 58% | 0.08 | 0.31 |
| 6 | 3 | 15 | 85% | 64% | 60% | 85% | 71% | 0.15 | 0.41 |
| 7 | 6 | 11 | 70% | 80% | 72% | 79% | 76% | 0.3 | 0.5 |
| 8 | 12 | 8 | 40% | 95% | 84% | 69% | 72% | 0.6 | 0.35 |
| 9 | 12 | 3 | 10% | 100% | 100% | 61% | 63% | 0.9 | 0.1 |
| 10 | 4 | 0 | 0% | 100% | 0% | 58% | 58% | 1 | 0 |
Accurate assessment of pathological fracture risk for benign bone lesions is important in clinical decision making. However, studies on benign bone lesions in pediatric populations are limited because of a lack of understanding of the natural history of benign bone disorders[12]. Many surgeons treat these patients surgically in the light of personal experience, individual radiographic criteria, or some combination[3,13]. In our study, we present a modified scoring method predicting the risk of pathological fracture in pediatric patients based on four variables as scoring parameters. This predictive tool can be used to evaluate the fracture risk associated with by the lesion and provide a reference for surgical decision-making.
Kaelin and MacEwen[12] documented the natural history of simple bone cysts (SBC) in several patients. They used bone cyst index (BCI) to determine the risk of fracture. They suggested that a high risk of fracture was present when BCI in SBC was greater than 4 for the humerus and greater than 3.5 for the femur. However, Vasconcellos et al[14] demonstrated that BCI could not predict the risk of fracture accurately because of poor diagnostic performance and low reliability. Ahn and Park[15] reported that lesions with cortical involvement > 85% in children with SBC were associated with increased fracture risk. No specificity or sensitivity data were given in that study. Arata et al[16] reported transverse cortical involvement exceeded 50% and vertical length exceeded 33 mm in lower-extremity non-ossifying fibromas were predictors of pathologic fracture. Nevertheless, none of these studies could accurately predict the occurrence of pathologic fracture prospectively, and each of these approaches reported for the prediction of fracture is suitable for only a specific lesion or location.
Recently, additional studies, including computerized tomography (CT) or magnetic resonance imaging, have been applied for assessment of fracture risk[17]. Snyder et al[18] introduced CT-based structural rigidity analysis for prediction of pathological fracture in pediatric patients with benign skeletal neoplasms. Reduction equal to or greater than 33% in rigidity was at high risk for pathologic fracture. Leong et al[19] further validated this method in a prospective study. Although CT-based structural rigidity analysis was more accurate than findings obtained by plain radiography for fracture prediction, there were some limitations, including the requirement of normal contralateral bone for comparison and exposure to high doses of radiation. Pireau et al[20] reported that the cyst index calculated on T1-weighted magnetic resonance imaging was considered as the best predicting factor for fracture in SBC. However, this method does not apply to other types of benign bone lesions.
In 1989,a scoring system was proposed by Mirels, which is widely referenced in clinical practice[21]. The Mirels scoring system evaluates the fracture risk based on the location of the lesion, lesion size, radiographic appearance, and severity of pain. The score of each section ranges from 1 to 3 with a total score of 4 to12. Different management strategies are recommended according to different scoring statuses. When the Mirels score was 9 or higher, prophylactic fixation was considered as a treatment recommendation. However, this guideline is appropriately applied only to adults with metastatic bone disease. Referring to the method described by Mirels, we introduced a similar method to evaluate the risk of fracture for children with benign bone lesions. By comparing demographic features between fracture patients and non-fracture patients in our study, potentially important variables were identified and confirmed in non-conditional logistical regression analysis. Our results showed that the lesion site was not an independent risk factor of clinical fracture. Pain, lesion type, and size were identified as predictive variables. Therefore, the lesion site was not assigned to be a variable in our proposed modified scoring system. The size of the lesion was given more weight, namely, lesion-to-bone width and axial cortical involvement were endowed with an ascending score ranging from 1 to 3, respectively. Lesion type and pain were separately granted score from 0 to 2. Through retrospective analysis of 96 patients using the modified scoring system, we found a cutoff of 7 gave the optimum combination of specificity and sensitivity. The overall accuracy was 76%, and fracture probability was 30%. ROC curve analysis demonstrates that the modified scoring system had acceptable accuracy and had a similar area under the curve with the Mirels scoring system[10]. The ultimate goal of predicting pathological fractures is to inform rational treatment strategies for the prevention of pathological fractures. Therefore, we set a score of 7 as borderline. A lesion with a score > 7 is an indication for prophylactic stabilization because of high fracture risk, while a lesion with a score < 7 is evaluated as low fracture risk without the need for prophylactic stabilization.
An important advantage of our proposed scoring system is that it is a simple, rapid, and convenient method. However, this study has some limitations. First, the study was carried out at a single institution and in a retrospective fashion, so potential biases were present in case selection. Second, the number of patients in each type of bone lesion was relatively small and limited the generalizability of this scoring system. Finally, other factors that affect fracture risk should be taken into account. There is a need for a prospective, multicenter, large-scale trial to validate and expand this assessment method of fracture risk.
Increasing pain, osteolytic appearance, lesion-to-bone width (> 2/3), and axial cortical involvement (> 30 mm) are risk factors for pathological fracture. The modified scoring system is possibly a useful tool in clinical decision-making for clinicians. Lesions with a total score > 7 indicate a high risk of a pathologic fracture, when prophylactic internal fixation should be recommended. A total score < 7 is associated with a low risk of a pathologic fracture, and prophylactic internal fixation is not recommended.
A method regarding the appropriate assessment of fracture risk in long bone lesions affected by benign tumor is lacking.
We performed this study to determine an appropriate approach to assess the fracture risk in children with benign bone lesions of long bones.
The purpose of this study was to investigate the risk factors of pathological fracture and to propose a modified scoring system for quantitative analysis of the pathologic fracture risks.
We retrospectively analyzed the histological diagnosis, anatomical site, radiographic appearance, severity of pain, and lesion size of 40 patients who had fractures through a benign bone lesion and 56 who had no fracture at our institution.
Through retrospective analysis of 96 patients using our proposed scoring system, we found the cutoff was 7 in consideration of the optimum combination of specificity and sensitivity. The overall accuracy was 76% and fracture probability was 30%. The receiver operator characteristic curve analysis demonstrates that the modified scoring system is good regarding accuracy and has a similar area under the curve with the Mirels scoring system.
We set score of 7 as borderline. Lesion with a score > 7 is an indication for prophylactic stabilization because of high fracture risk, while lesion with a score < 7 is evaluated as low fracture risk without concern for prophylactic stabilization.
In follow-up work, a prospective, multicenter, large-scale study will be conducted to validate and improve our proposed scoring system for assessment of the fracture risk in children with benign bone lesions of long bones.
The authors acknowledge the assistance of Yang LL (The Children’s Hospital, Zhejiang University School of Medicine) for her help with language and grammar.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mayr J S-Editor: Fan JR L-Editor: Filipodia P-Editor: Liu JH
| 1. | Woertler K. Benign bone tumors and tumor-like lesions: value of cross-sectional imaging. Eur Radiol. 2003;13:1820-1835. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 76] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 2. | Tomaszewski R, Rutz E, Mayr J, Dajka J. Surgical treatment of benign lesions and pathologic fractures of the proximal femur in children. Arch Orthop Trauma Surg. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 14] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 3. | Erol B, Topkar MO, Aydemir AN, Okay E, Caliskan E, Sofulu O. A treatment strategy for proximal femoral benign bone lesions in children and recommended surgical procedures: retrospective analysis of 62 patients. Arch Orthop Trauma Surg. 2016;136:1051-1061. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 4. | Canavese F, Samba A, Rousset M. Pathological fractures in children: Diagnosis and treatment options. Orthop Traumatol Surg Res. 2016;102:S149-S159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 5. | Fritzsche H, Schaser KD, Hofbauer C. [Benign tumours and tumour-like lesions of the bone : General treatment principles]. Orthopade. 2017;46:484-497. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 6. | Noordin S, Allana S, Umer M, Jamil M, Hilal K, Uddin N. Unicameral bone cysts: Current concepts. Ann Med Surg (Lond). 2018;34:43-49. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 48] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 7. | Liu Q, He H, Zeng H, Yuan Y, Wang Z, Tong X, Luo W. Active unicameral bone cysts: control firstly, cure secondly. J Orthop Surg Res. 2019;14:275. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Jamshidi K, Mirkazemi M, Izanloo A, Mirzaei A. Locking plate and fibular strut-graft augmentation in the reconstruction of unicameral bone cyst of proximal femur in the paediatric population. Int Orthop. 2018;42:169-174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 9. | Lunkiewicz M, Anderson S, Havakeshian S, Würzburg A. Practical Input on Bone Tumor Imaging: Pathological Fracture, Risk Features, and When to Contact Orthopaedics. Semin Musculoskelet Radiol. 2019;23:19-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Howard EL, Cool P, Cribb GL. Prediction of pathological fracture in patients with metastatic disease of the lower limb. Sci Rep. 2019;9:14133. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 11. | Damron TA, Mann KA. Fracture risk assessment and clinical decision making for patients with metastatic bone disease. J Orthop Res. 2020;38:1175-1190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 62] [Article Influence: 12.4] [Reference Citation Analysis (1)] |
| 12. | Kaelin AJ, MacEwen GD. Unicameral bone cysts. Natural history and the risk of fracture. Int Orthop. 1989;13:275-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 64] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 13. | Lalam R, Bloem JL, Noebauer-Huhmann IM, Wörtler K, Tagliafico A, Vanhoenacker F, Nikodinovska VV, Sanal HT, Woude HV, Papakonstantinou O, Åström G, Davies M, Isaac A, Weber MA. ESSR Consensus Document for Detection, Characterization, and Referral Pathway for Tumors and Tumorlike Lesions of Bone. Semin Musculoskelet Radiol. 2017;21:630-647. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 27] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 14. | Vasconcellos DA, Yandow SM, Grace AM, Moritz BM, Marley LD, Fillman RR. Cyst index: a nonpredictor of simple bone cyst fracture. J Pediatr Orthop. 2007;27:307-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 15. | Ahn JI, Park JS. Pathological fractures secondary to unicameral bone cysts. Int Orthop. 1994;18:20-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 57] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 16. | Arata MA, Peterson HA, Dahlin DC. Pathological fractures through non-ossifying fibromas. Review of the Mayo Clinic experience. J Bone Joint Surg Am. 1981;63:980-988. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 17. | Damron TA, Nazarian A, Entezari V, Brown C, Grant W, Calderon N, Zurakowski D, Terek RM, Anderson ME, Cheng EY, Aboulafia AJ, Gebhardt MC, Snyder BD. CT-based Structural Rigidity Analysis Is More Accurate Than Mirels Scoring for Fracture Prediction in Metastatic Femoral Lesions. Clin Orthop Relat Res. 2016;474:643-651. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 85] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 18. | Snyder BD, Hauser-Kara DA, Hipp JA, Zurakowski D, Hecht AC, Gebhardt MC. Predicting fracture through benign skeletal lesions with quantitative computed tomography. J Bone Joint Surg Am. 2006;88:55-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 44] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 19. | Leong NL, Anderson ME, Gebhardt MC, Snyder BD. Computed tomography-based structural analysis for predicting fracture risk in children with benign skeletal neoplasms: comparison of specificity with that of plain radiographs. J Bone Joint Surg Am. 2010;92:1827-1833. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 27] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 20. | Pireau N, De Gheldere A, Mainard-Simard L, Lascombes P, Docquier PL. Fracture risk in unicameral bone cyst. Is magnetic resonance imaging a better predictor than plain radiography? Acta Orthop Belg. 2011;77:230-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 21. | Mirels H. Metastatic disease in long bones: A proposed scoring system for diagnosing impending pathologic fractures. 1989. Clin Orthop Relat Res. 2003;S4-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 87] [Article Influence: 4.0] [Reference Citation Analysis (0)] |