Published online Jul 26, 2021. doi: 10.12998/wjcc.v9.i21.6026
Peer-review started: March 18, 2021
First decision: April 23, 2021
Revised: May 1, 2021
Accepted: May 20, 2021
Article in press: May 20, 2021
Published online: July 26, 2021
Processing time: 124 Days and 15 Hours
Follicular lymphoma (FL) is more common in lymph nodes, while primary extranodal lymphomas are rare. Urinary tract lymphoid neoplasms are extremely rare, accounting for less than 5% of all extranodal lymphomas. Only one case of FL from the renal pelvis has previously been reported.
A 70-year-old male patient with a history of esophageal cancer visited our hospital for follow-up examination. Abdominal computed tomography revealed a malignant mass in the right renal pelvis. The whole-body positron emission tomography/computed tomography showed a significant increase in fluo
Extranodal FL is more common in the skin and gastrointestinal tract but rarely occurs in the urinary tract. This is the second report of primary renal FL. Localized extranodal FL is expected to have a favorable prognosis and can be cured by local resection.
Core Tip: Follicular lymphoma (FL) is more common in lymph nodes, while primary extranodal lymphomas are rare. Urinary tract lymphoid neoplasms are extremely rare, accounting for less than 5% of all extranodal lymphomas. We reported a rare case of primary FL of the renal pelvis in a 70-year-old man with a history of esophageal cancer, which was treated with surgery. Localized extranodal FL is expected to have a favorable prognosis and can be cured by local resection.
- Citation: Shen XZ, Lin C, Liu F. Primary follicular lymphoma in the renal pelvis: A rare case report. World J Clin Cases 2021; 9(21): 6026-6031
- URL: https://www.wjgnet.com/2307-8960/full/v9/i21/6026.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i21.6026
Follicular lymphoma (FL) accounts for 22% of all non-Hodgkin's lymphoma cases worldwide. FL is the most common form of indolent lymphoma, especially in the elderly. FL has an excellent prognosis among lymphomas, with a median survival of 8-10 years. FL is more common in lymph nodes, while primary extranodal lymphomas are rare. Urinary tract lymphoid neoplasms are extremely rare, accounting for less than 5% of all extranodal lymphomas. Herein, we report a rare case of primary FL of the renal pelvis in a 70-year-old man with a history of esophageal cancer, which was treated with surgery.
A 70-year-old male patient who had been previously diagnosed with esophageal cancer revisited our hospital for follow-up. The patient had been diagnosed with esophageal squamous cell carcinoma by esophagoscopic biopsy 5 years ago, followed by radical radiotherapy and four cycles of combination chemotherapy. Two years ago, he visited our hospital for follow-up, and no tumor recurrence or metastasis was found. This time, the patient complained of slight swallowing discomfort and had no other symptoms.
The patient's current renal pelvic tumor was incidentally discovered on computed tomography (CT) examination after hospitalization and had no clinical manifestations.
The patient had been diagnosed with esophageal squamous cell carcinoma by esophagoscopic biopsy 5 years ago, followed by radical radiotherapy and four cycles of combination chemotherapy. Two years ago, he visited our hospital for follow-up, and no tumor recurrence or metastasis was found.
He has a history of radiotherapy for esophageal cancer.
Physical examination showed no positive signs.
In the male tumor markers combination (14 items), CA724 serum level increased to 23.45 IU/mL (normal range, 0-6 IU/mL), and all other markers were within the normal range.
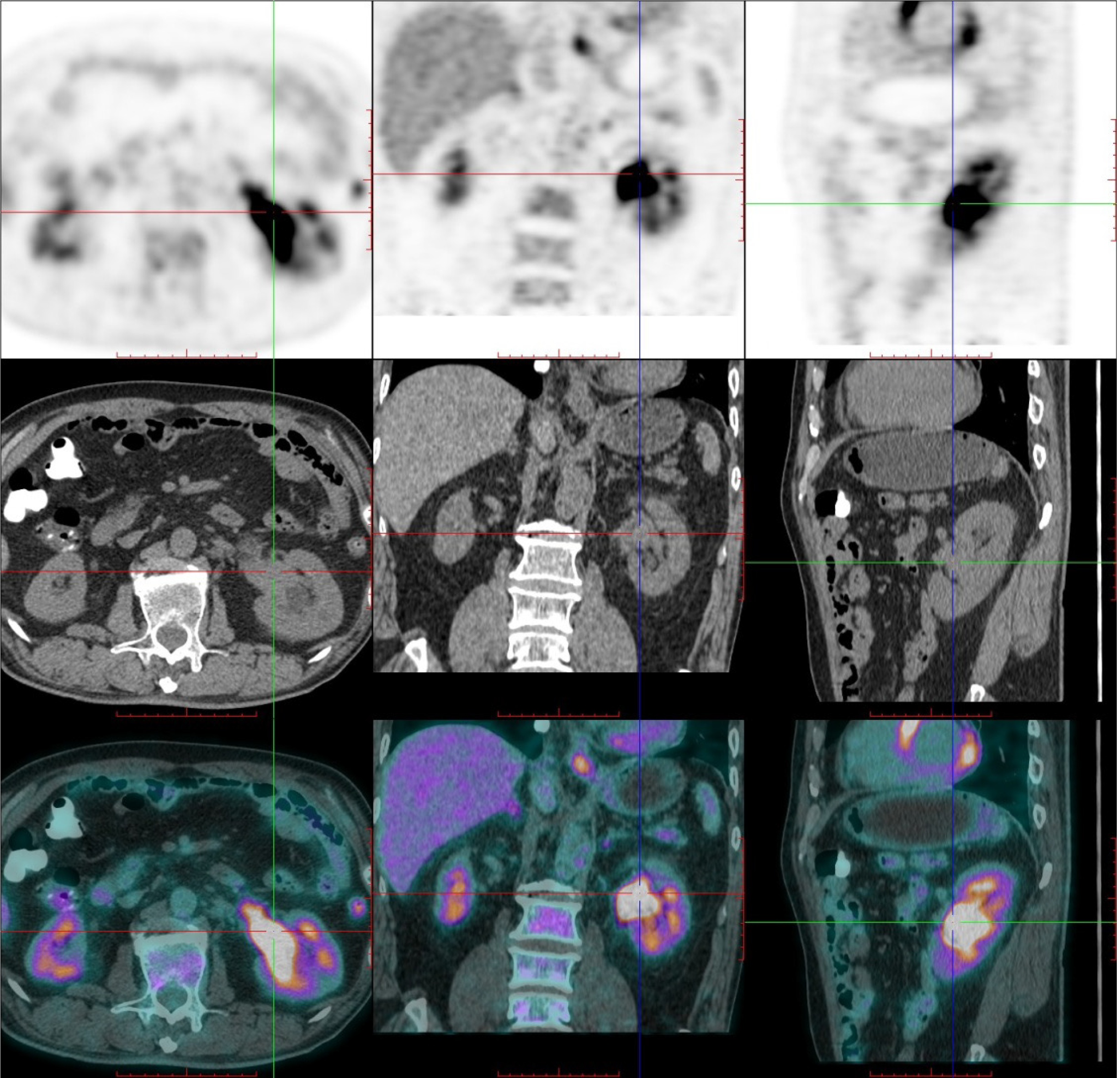
The upper alimentary tract double-contrast barium examination showed that the wall of the upper esophagus was slightly rigid, which was considered to be a change after chemoradiotherapy. Esophagoscopy showed esophageal scarring. Abdominal enhanced CT scan showed soft tissue masses in the left renal pelvis and the beginning of the left ureter, with uniform density and moderate enhancement (Figure 1). The whole-body positron emission tomography (PET)/CT showed a significant increase in fluorodeoxyglucose (FDG) uptake of this approximately 67 mm × 27 mm soft tissue mass (Figure 2), and the maximum standardized uptake value of routine and delayed imaging after 1.5 h was about 11.7 and 16.5, respectively. The PET/CT examination showed no abnormal FDG uptake in the esophageal wall.
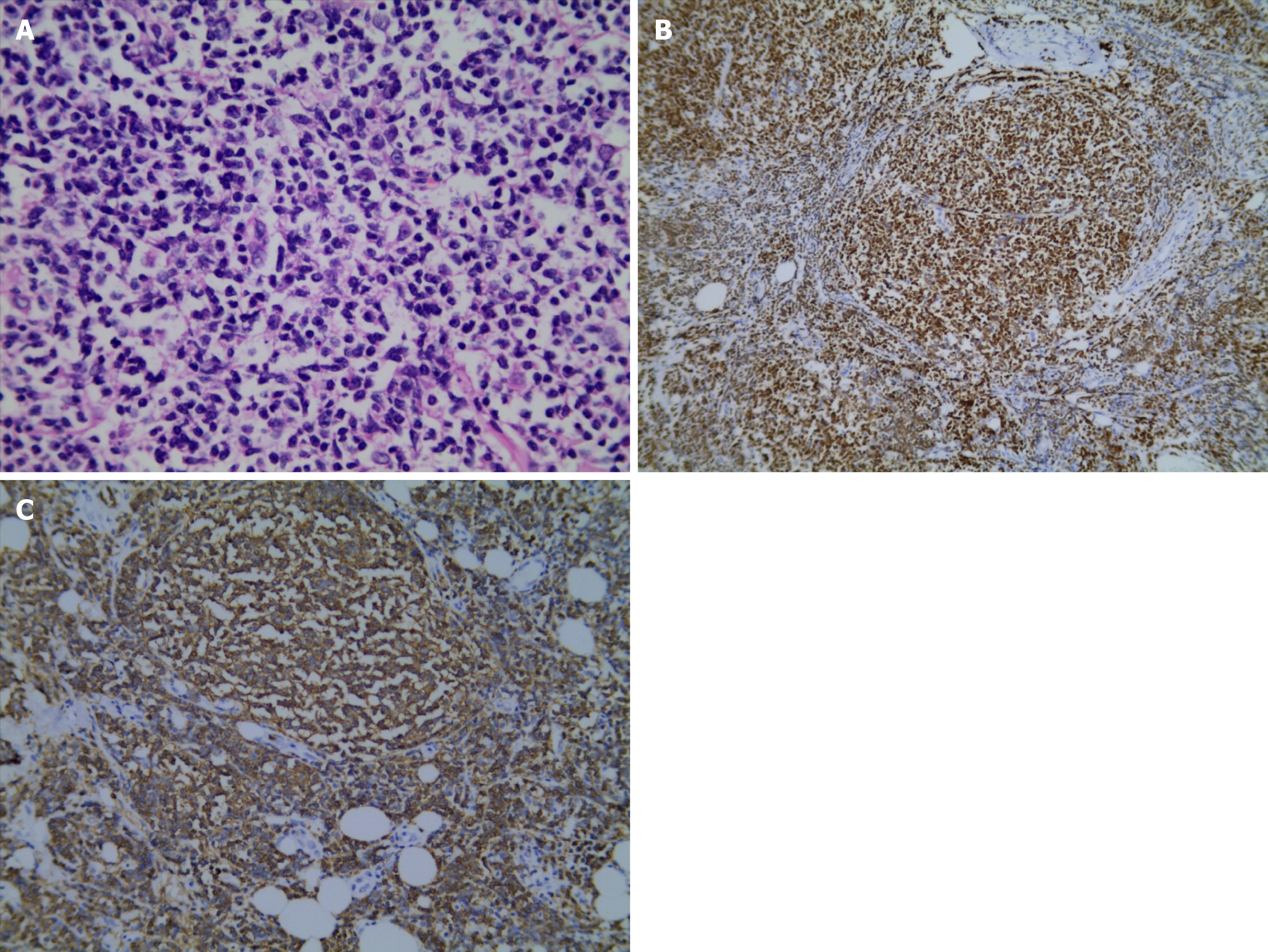
Microscopically, the tumor surgical specimen was mainly composed of large central cells, with no obvious nucleoli, scattered centroblasts, missing follicular structure, and lack of sheath (Figure 3A). The immunophenotyping study revealed positive staining for Bcl-2 (Figure 3B), Bcl-6, CD10, CD20 (Figure 3C), CD23, CD3, CD31, CD35, and Pax-5 but negative staining for CD56, cyclin D1, Mum-1, and terminal deoxynucleotidyl transferase. The postoperative pathological diagnosis was B-cell lymphoma, which was considered as FL.
The patient subsequently underwent radical resection of the malignant tumor of the left kidney. The left kidney, ureter, and partial bladder were removed.
The patient received no radiation or chemotherapy after surgery, and no recurrence of lymphoma or other malignant tumors was found at the 1-year follow-up.
Renal pelvis tumors are rare, accounting for only 0.1% of all cancers. Primary renal pelvis and ureteral lymphomas are extremely rare, and only a few cases have been reported in the literature[1-6].
Since lymphoid tissue is scarce throughout the urinary tract, primary renal lymphomas are rare, while primary lymphoma of the renal pelvis is extremely rare[2,3].
Among the primary lymphomas in the renal pelvis and ureter, mucosa-associated lymphoid tissue lymphomas are relatively common, and a total of 9 cases have been reported in the retrievable English literature[4,5]. Maeda et al[6] reported a middle-aged man who received a kidney transplant from his healthy daughter due to chronic kidney failure, but 2 years later, the transplanted renal pelvis developed malignant lymphoma, which was B-cell immunoblastic lymphoma. Primary pelvis and ureteral lymphoma must be differentiated from metastatic tumor in diagnosis. Metastatic tumors usually have the presence or history of the primary malignancy, and metastatic tumors are often multiple. Solitary metastasis may occasionally occur in renal parenchyma but rarely only in the pelvis and ureter[7].
FL is a malignant proliferative disease of germinal center B cell origin. It is the most common pathological type of infirm lymphoma and the second histological type in non-Hodgkin's lymphoma. FL patients are typically over 60 years of age, and the incidence is positively correlated with age. The median overall survival is about 8-10 years. The most common manifestation of FL is painless lymphadenectasis, typically manifested as multiple lymphoid tissue invasion. Histologically, FL presents as a follicular or nodular growth. FL has a characteristic immunophenotype. Typical immunohistochemical markers such as CD20+, CD23+/-, CDl0+, CD43-, Bcl2+, Bcl-6+, and CD5- were found in most cases[8]. The majority of FL patients have widespread disease that can affect the extranodal sites, but the incidence of primary extranodal FL is very low. Extranodal FL is more common in the skin and gastrointestinal tract but rarely occurs in the urinary tract[2]. Bozas et al[2] reported the first case of primary renal pelvic FL in a 70-year-old man with chronic lower back pain in 2006. To the best of our knowledge, this is the second reported primary renal FL, also in a 70-year-old male.
Our patient recovered well after surgery. No radiotherapy or chemotherapy was performed for 1 year. No tumor recurrence was observed during follow-up. Hence, localized extranodal FL is expected to have a favorable prognosis and can be cured by local resection.
On CT, renal FL presents as a well-defined, homogeneous soft tissue mass, with moderate enhancement on contrast-enhanced scan. On FDG PET/CT, the mass may present with low or high uptake of FDG, depending on the grade of the tumor. However, renal FL has no specific imaging, clinical, or laboratory findings. Hence, it is difficult to differentiate from other renal malignancies, and its incidence is extremely low, so its diagnosis must rely on pathology.
Manuscript source: Unsolicited Manuscript
Specialty type: Oncology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Huang AHC S-Editor: Ma YJ L-Editor: Filipodia P-Editor: Li JH
| 1. | Naik N, Lin M, Lin P. Genitourinary involvement of lymphomas on FDG-PET. Br J Radiol. 2018;91:20170273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 2. | Bozas G, Tassidou A, Moulopoulos LA, Constandinidis C, Bamias A, Dimopoulos MA. Non-Hodgkin's lymphoma of the renal pelvis. Clin Lymphoma Myeloma. 2006;6:404-406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 3. | Boscolo-Berto R, Raduazzo DI, Vezzaro R, Marino D, Aversa SM, Gardiman M. Aggressive non-Hodgkin's lymphoma mimicking unilateral transitional cell carcinoma of renal pelvis. The risk of making a diagnostic mistake. Arch Ital Urol Androl. 2011;83:163-165. [PubMed] |
| 4. | Mita K, Ohnishi Y, Edahiro T, Fujii T, Yamasaki A, Shimamoto F. Primary mucosa-associated lymphoid tissue lymphoma in the renal pelvis. Urol Int. 2002;69:241-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Otsuki H, Ito K, Sato K, Kosaka T, Shimazaki H, Kaji T, Asano T. Malignant lymphoma of mucosa-associated lymphoid tissue involving the renal pelvis and the entire ureter: A case report. Oncol Lett. 2013;5:1625-1628. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Maeda K, Hawkins ET, Oh HK, Kini SR, Van Dyke DL. Malignant lymphoma in transplanted renal pelvis. Arch Pathol Lab Med. 1986;110:626-629. [PubMed] |
| 7. | Haddad FS. Metastases to the ureter. Review of the world literature, and three new case reports. J Med Liban. 1999;47:265-271. [PubMed] |
| 8. | Chinese Society of Hematology, Chinese Medical Association; Chinese Society of Lymphoma, Chinese Anti-cancer Association. Chinese Society of Lymphoma, Chinese Anti-cancer Association. [Chinese guidelines for diagnosis and treatment of follicular lymphoma(2013)]. Zhonghua Xue Ye Xue Za Zhi. 2013;34:820-824. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |