Published online Jul 26, 2021. doi: 10.12998/wjcc.v9.i21.5921
Peer-review started: February 15, 2021
First decision: April 25, 2021
Revised: May 5, 2021
Accepted: June 1, 2021
Article in press: June 1, 2021
Published online: July 26, 2021
Processing time: 155 Days and 20.3 Hours
Neonatal pain has been underdiagnosed due to several false beliefs.
To determine the status of neonatal pain in newborns who are admitted to intensive care units.
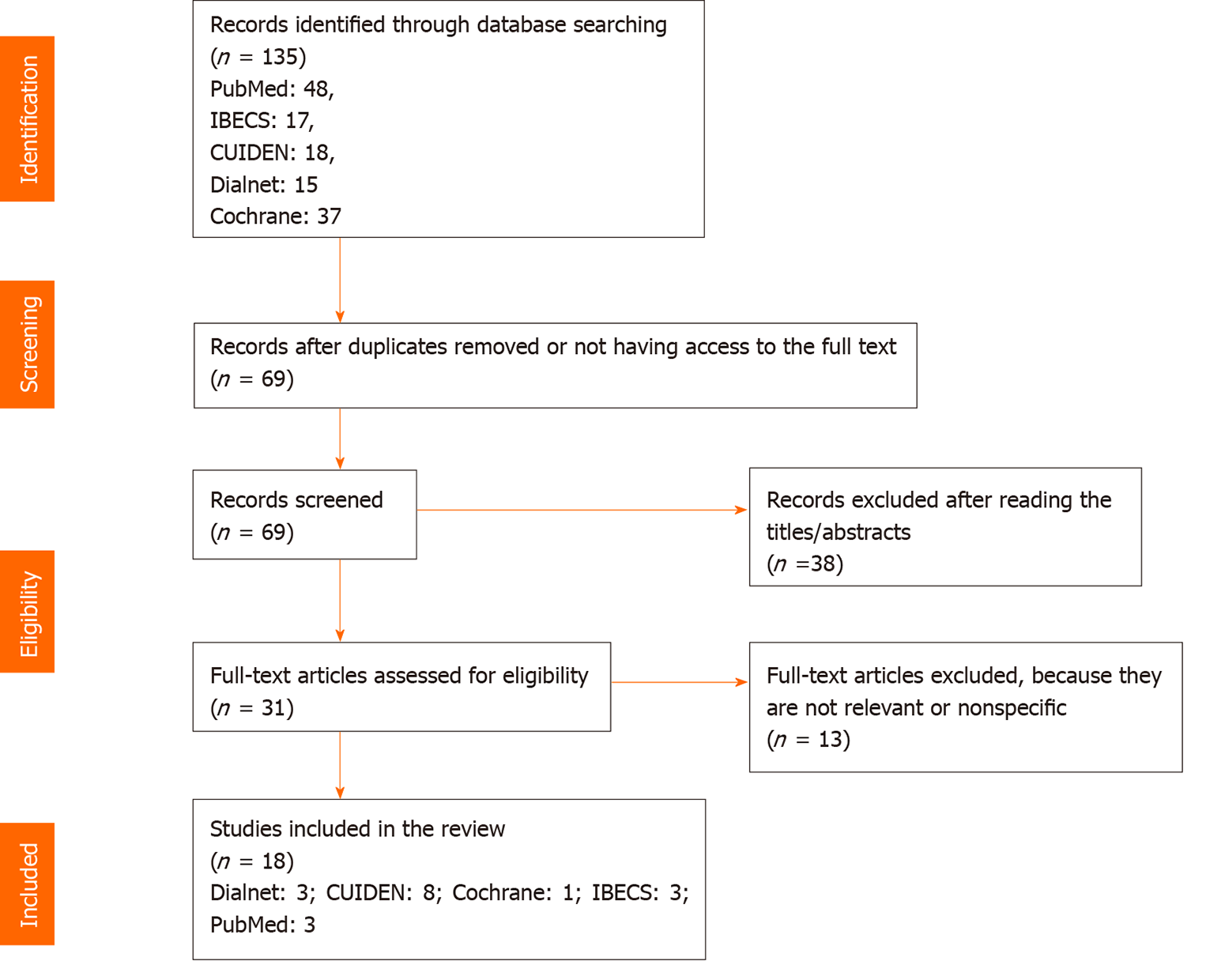
Different databases were searched. Literature reviews and research reports conducted in newborns that were written in English, Spanish, or Portuguese, published between 2010 and 2020, and having free access to the full text were selected. A total of 135 articles were found, and 18 articles were finally reviewed.
Newborns are exposed to numerous painful procedures. In order to assess their pain levels, several scales have been used, although they are sometimes not correctly interpreted. In terms of pain management, the nursing team plays a very important role based mainly on both pharmacological and non-pharmacological approaches.
Nursing staff members must be well trained in order to identify pain and to interpret the scales correctly. Besides, they have an important role in performing non-pharmacological procedures for pain management.
Core Tip: The painful experiences in newborns can cause side effects both in the short and long term. Nowadays, most newborns admitted to intensive care units do not receive adequate pain assessment using validated clinic scales. Training healthcare professionals is important, so that they can correctly assess and manage pain in newborns, based on evidence and not only on clinical practice or personal experience. There is a lack of protocols about neonatal pain management in intensive care units as well as little presence of pain management teams and/or leaders to tackle it correctly.
- Citation: Garcia-Rodriguez MT, Bujan-Bravo S, Seijo-Bestilleiro R, Gonzalez-Martin C. Pain assessment and management in the newborn: A systematized review. World J Clin Cases 2021; 9(21): 5921-5931
- URL: https://www.wjgnet.com/2307-8960/full/v9/i21/5921.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i21.5921
The latest definition of pain, according to the International Association for the Study of Pain (2016), is: An unpleasant sensory and emotional experience associated with, or resembling, actual or potential tissue damage[1]. However, neonatal pain was not taken into account for a long time, since it was believed that newborns barely felt pain and, therefore, tolerated it well. Neonatal pain was completely underestimated and insufficiently treated[2]. Currently, we know that babies are able to feel painful stimuli already in the uterus. Researchers have proposed that some newborns may retain some memories of these painful experiences and may develop greater sensitivity to pain and less tolerance for pain as they grow older[3]. Newborns experience painful stimuli from the moment they are born, often related to procedures carried out in the hospital[4]. These painful experiences can cause both short-term and long-term side effects[3] , and, in many cases, adequate measures are not taken to relieve or prevent pain[5]. Nowadays, most newborns admitted to intensive care units (ICUs) do not receive adequate pain assessment using validated clinic scales. Avila-Alvarez et al[5] indicate in their study carried out in different Spanish neonatal intensive care units (NICUs) that, despite the existence of recent studies on this topic, there are very few papers that prospectively assess newborns’ pain to understand its impact, assessment, and treatment. These authors show that pain was only assessed with a clinical scale in 16.7% (n = 78) of the newborns included in the study (n = 468). Even so, 42.3% of the patients received a sedative or analgesic treatment, and 33.1% needed stronger analgesics. Out of the 30 units that participated in the study, 20 units did not assess pain using clinical scales. Sixty-six point 6 percent of the units used local guidelines for pain management, whilst 43.3% had guidelines for pain assessment. Only 13 units had a pain management team.
Therefore, the objective of this review is to define and assess the status of neonatal pain and pain management in newborns admitted to ICUs. In addition, given that the nursing team is responsible for carrying out a correct ongoing assessment of the patient’s situation, this paper addresses the knowledge of these healthcare professionals regarding neonatal pain.
This review was written following the Preferred Reporting Items for Systematic Reviews and Meta Analyses protocol for systematic reviews[6,7]. The research questions were “How is pain in newborns admitted to the NICU assessed and managed” and “what is the nursing staff’s knowledge of neonatal pain?”.
Our literature search was guide by the PICOT framework, and the components include: (P) population of interest, (I) issue of interest, (C) comparison of interest, (O) outcome of interest, and (T) timeframe[8]. The search was focused on newborn patients admitted to ICU (P) and on the pain assessment and management (I). Comparison of interest (C) was not relevant, because the review purpose was to know the pain assessment and management in newborns and the nursing staff knowledge about the newborn pain. The outcomes (O) were categorized as “Neonatal pain assessment and management” and “Nursing staff knowledge about neonatal pain”. We set a timeframe (T) of research published from 2010 to 2020. The inclusion criteria were: (1) Literature reviews; (2) Research reports conducted in newborns; (3) Written in English, Spanish or Portuguese; (4) Published between 2010 and 2020; (5) Articles with free access to full text; and (6) Considered of interest for the systematized review. Two nurse researchers identified the Mesh terms and used the keywords to develop a rigorous search strategy in different databases (PubMed, Dialnet Plus, Cochrane Library Plus, Cuiden, and IBECS). The key words used separately and in combination were: ”pain”, “acute pain”, ”pain management”, ”infant, newborn”, “intensive care units, neonatal”, and “nursing care”. And the used limits were: ‘humans’, ‘English’, ’Spanish’, ‘Portuguese’, and articles with free access to full text considered relevant for the work (Table 1). The search of literature was from January 2010 to April 2020.
| Search | Terms | Results |
| #1 | “Pain” [Mesh] | 390.237 |
| #2 | “Acute Pain” [Mesh] | 2.063 |
| #3 | “Pain Management” [Mesh] | 33.044 |
| #4 | #1 OR #2 OR #3 | 402.906 |
| #5 | “Infant, Newborn” [Mesh] | 600.745 |
| #6 | "Intensive Care Units, Neonatal" [Mesh] | 14.373 |
| #7 | “Nursing Care” [Mesh] | 134.280 |
| #8 | #4 AND #5 AND #6 AND #7 | 48 |
| #9 | #8 Filters: Full text; published in the last 10 yr | 19 |
The articles initial selection was carried out according to the exclusion and inclusion criteria, followed by reading the title and/or abstract. If the title responded to the subject of the review, the abstract was retrieved for reading, and if it was considered relevant, the full text was accessed. Three researchers independently screened the titles and abstracts of the studies found to identify those that met the inclusion criteria. Then, the articles that were not discarded were read in full text and assessed for their election. Disagreement over eligibility of studies was solved through discussion and by a fourth reviewer. To assess the quality of the articles, the scientific level of evidence designed by United States Agency for Healthcare Research and Quality[9] was used due to its simplicity and clarity. According to United States Agency for Healthcare Research and Quality, there are five levels of scientific evidence depending on the type of study, establishing that the levels with a highest degree of scientific evidence are those that are in the highest part of the scale (such as meta analyses and systematic reviews), and the lower levels are those that have less evidence and therefore less reliability.
A data extraction sheet was developed, and the data were extracted by the authors. Differences were face to face discussed and when there was consensus the data were included. The variables were taken into account were: Title and author, journal, country, year of publication, level of evidence, research design, pain assessment, pain management, painful procedures, and aim of the study. Data were synthesized and analyzed by the review authors, and the discrepancies were solved by consensus. The results were written as a descriptive narrative synthesis, and tables were made to collect the variables taken into account.
After the bibliographic search, 135 articles were found. Sixty-six were removed for being duplicates or not having access to the full text. The remaining 69 articles were assessed by the authors in a primary review based on the reading of the titles and abstracts, discarding those articles (n = 38) in which certain criteria were not fulfilled: The title did not respond to the subject of the review and/or the inclusion criteria were not met. Thirty-one articles were read full text by authors, and 13 were excluded because they did not focus on the objective of the work because it was nonspecific or minimally relevant. A total of 18 articles were included in the scoping review for this study (Figure 1).
Most of the selected articles were of South American origin (61.0%)[10-20], and the rest of them were of European (27.8%)[3,5,21-23] and north American[24,25] origin. The main publication country was Brazil (n = 8)[12-20], followed by Spain (n = 4)[3,5,21,22]. The types of studies included in the review were: Bibliographic reviews (n = 5)[3,13,19,22,24], qualitative studies (n = 4)[12,15,18,20], and quantitative studies (n = 9). The level of evidence of the articles, according to the United States Agency for Healthcare Research and Quality, was Ia for five articles[3,13,19,22,24] and III for the rest of them. Regarding the assess
The main outcomes were categorized in two parts: (1) Neonatal pain assessment and management; and (2) Nursing staff knowledge about neonatal pain (Table 2).
| Ref. | Level of Evidence | Research Design | Pain Assessment | Pain Management | Painful Procedures | Aim |
| Gonzalez et al[3] | Ia | Systematic review | Scales: NIPS, PIPP, CRIES, NFCS, COMFORT | NPI: Environmental, behavioral and nutritional intervention: sucrose, dummy (non-nutritive suction), kangaroo method or skin to skin.PI: Paracetamol, morphine, ketamine, metamizole, thiopental, chloral hydrate… | Venipuncture, lumbar/heel puncture, peripheral/central venous catheter insertion, umbilical catheterization, injections, aspiration, orogastric catheterization | To know the neonatal pain impact and its treatment in painful procedures. Purpose: To sensitize health professionals about pain management in NBs |
| Avila-Alvarez et al[21] | III | Multicenter, observational, longitudinal and prospective study | NA | NPI: Sweet oral solution: Sucrose (most common) and glucose. PI: Fentanyl (most used), midazolam, morphine, paracetamol | Invasive and non-invasive mechanical ventilation | To determine the clinical practice in relation to sedation and analgesia in Spanish ICUs and to identify factors associated with the use of drugs |
| Guzmán et al[10] | III | Prospective-descriptive pilot study | Observational: Signs of pain (crying), contraction of facial muscles, heart rate and respiratory rate | Sentire method: Psychotherapeutic pain management through music and touch | Clinical procedures, separation from mother, ambient noise > 45 dB | Analyze the effectiveness of the Sentire method |
| San Martín et al[11] | III | Descriptive correlational cross-sectional study | Susan Givens-Bell Scale | NA | Venous and arterial puncture, orogastric catheterization, aspiration of secretions | Assess the pain intensity in NB against nursing procedures |
| Aguilar et al[22] | Ia | Systematic review | Most employed: PIPP and NIPS | NPI: Oral administration of sweet solutions, breastfeeding and kangaroo care | Heel puncture, injections and vaccines, venous lines cannulation | To analyze studies that assess the effectiveness of NPIs during painful procedures |
| Avila-Alvarez et al[5] | III | Observational longitudinal prospective study | Most used scales: NIPS, CRIES and Susan-Givens. Others: PIPP, NPASS, COMFORT | PI: Sedative or analgesic medication | Invasive mechanical ventilation | To determine the clinical practice in relation to the assessment of neonatal pain in Spain and the factors associated with the use of scales |
| Veronez et al[12] | III | Qualitative descriptive study | Observation: Crying, facial expression, irritability and agitation. Physiological alterations: Heart rate, blood pressure, respiratory parameters, etc | NPI(mild pain): Oral glucose administration, non-nutritive suction, group procedures, environmental measuresPI (severe pain): Non-opioid and opioid analgesics | Venous puncture, capillary glycemia, adhesive removal, tracheal aspiration, dressings… | Describe the perception of neonatal pain by ICU nursing professionals |
| Do Prado et al[13] | Ia | Systematic review | Physiological and behavioral alterations. Scales: NIPS, NFCS, PIPP, CRIES, N-PAS | NPI: Oral glucose and non-nutritive suction (most used), environmental and postural care, breastfeeding… PI: NSAIDs, opioids, sedatives, local anesthetics | Venipuncture, blood collection, gastric catheterization, intubation… | To analyze the Brazilian scientific production on the evaluation and therapeutic approach of pain in newborns admitted to NICU |
| Thomé et al[14] | III | Cross-sectional study | NIPS scale | NA | Orotracheal tube and airway aspiration, venipuncture, intubation and insertion of PICC | Assess pain in NBs admitted to the NICU during invasive procedures |
| Do Nascimento et al[15] | III | Descriptive exploratory study with a qualitative approach | Physiological and behavioral responses. Scales: NFCS, NIPS and PIPP | NPI: Non-nutritive suction, positioning and containment. PI: Opioids, topical analgesics and sedatives | Diagnostic, surgical and therapeutic procedures: Venipuncture, capillary blood glucose, improper management, orotracheal aspiration… | Identify how the nursing staff assesses and manages NB pain in the NICU |
| Costa et al[16] | III | Descriptive cross-sectional study | Scales: NIPS, CRIES. Physiological and behavioral alterations | NPI: Oral glucose, non-nutritive sucking and laying. PI: Paracetamol, fentanyl and morphine | Venous punctures, tracheal aspirations, surgeries | Verify the nurses knowledge and practices about NBs pain management admitted to the NICU |
| Bonolo et al[17] | III | Descriptive exploratory study | Physiological and behavioral indicators: Heart rate, facial expression, cryingScales: CRIES, PIPP, NIPS, NFCS, N-PASS | NPI: Positioning, non-nutritive suction, environmental measures. PI: Opioids, NSAIDs, local anesthetics | Venipuncture, overhandling, heel stick, blood draw, aspiration | To characterize the nursing staff and identify how it assesses and manages pain for preterm newborns |
| Alves et al[18] | III | Convergent care study | Escala: PASVital signs daily assessment | NPI: Reducing environmental stimulus, grouping procedures and promoting sleep, kangaroo mother care, containment during procedures, administration of oral glucose, non-nutritive sucking | Environmental stimulus and invasive procedures: Venous/arterial puncture, oro/nasogastric catheterization, endotracheal aspiration, lumbar puncture | Develop a nursing care plan based on non-pharmacological methods for neonatal pain treatment in ICUs. |
| Assunçao et al[19] | Ia | Exploratory qualitative bibliographic review | Physiological indicators (heart rate, respiratory rate, oxygen saturation) and behavioral (crying, facial expression and motor activity). Scales: NFCS, NIPS, PIPP | NPI: Non-nutritive suction, oral glucose/sucrose, positioning, skin-to-skin contact, environmental measures… PI: Opioids (morphine, fentanyl) non-opioids (acetaminophen, dipyrone) and sedatives (propofol, midazolam, diazepam) | Mechanical ventilation, postoperative period, insertion of central catheter and thoracic drains | Analyze the evaluation and intervention methods of neonatal pain and reflect on the nurse competence in the control and management of pain |
| Stevens et al[24] | Ia | Literature review of randomized control trials | Scales: PIPP, DAN, NIPS, NFCS, NAPI, N-PASS, BPSN. Physiological and behavioral indicators | NPI: Sucrose administration (most effective in combination with other interventions, such as non-nutritive sucking) | Heel puncture, venous/arterial puncture, injections, bladder and nasogastric catheterization, circumcision, retinopathy of prematurity eye exam | To determine the efficacy, dose and method of sucrose administration for pain relief during procedures in the NB |
| Desai et al[25] | III | Scales: N-PASS and NIPS | NA | Laboratory tests, venous/arterial puncture, intubation, aspirations… | To improve newborns acute and chronic pain measurements in a NICU by implementing the N-PASS scale | |
| Santos et al[20] | III | Qualitative descriptive study | Physiological and behavioral indicators (heart rate, breath rate, crying, facial expression..) | NPI: Containment, environmental measures (light and noise), touch, skin-to-skin contact, non-nutritive suction and glucose | Venous punctures, orogastric and bladder catheterization, capillary blood glucose, dressings, airway aspiration, orotracheal intubation | Analyze the parameters used by the nursing team to assess pain and intervention in the premature newborn |
| Dionysakopoulo et al[23] | III | Cross-sectional study | Most used scales: NIPS, PIPP Others: CRIES, NFCS, OPS, PAT, N-PASS | NA | Venipuncture, airway aspiration, tube placement and removal… | Evaluation and validation of scales (NIPS-PIPP) in hospitalized newborns in two Greek ICUs |
Neonatal pain assessment and management: Twelve papers about neonatal pain assessment and management were found[3,5,10,11,13,14,19,21-25](Table 2). Among the most painful and stressful procedures for ICU newborns were punctures (venepuncture, heel lance, capillary blood glucose, etc.)[3,11,13,14,19,22-25], followed by insertion of nasogastric or orogastric tubes and aspirations[11,13,14,23-25]. Other procedures that have been shown to be painful are mechanical ventilations[5,19,21], circumcisions[24], intubations[13,14,25], and eye examinations[24]. Out of the 12 studies, only one used the observational/physical alteration technique (crying, heart rate, etc.)[10] as a method assessment. Three papers used both scales and observation of physical and behavioral disturbances[13,19,24]. Thus, in the review carried out by Do Prado et al[13], they observed that the most widely used scale for pain assessment was the Neonatal Infant Pain Scale (NIPS), finding that crying was not considered by all studies as an adequate parameter for pain assessment, as it could also indicate hunger or discomfort. Whereas, for Assunçao et al[19], the most appropriate scales were those that take into account both behavioral and physiological responses, with the Neonatal Facial Coding System, NIPS, and Premature Infant Pain Profile (PIPP) being the most representative. Regarding the assessment of pain due to behavioral changes, they say that the clinical condition, sedation, and immaturity of the newborn must be taken into account, since they may hinder the response to the painful stimulus and, therefore, not be well assessed by the professional. According to this author, another factor that should be taken into account in the assessment of pain in the newborn is the professional's interpretation of behavioral changes, since it is sometimes difficult to differentiate between pain and unpleasant stimuli that are not painful. In the review carried out by Stevens et al[24], they assess sugar as analgesia in different painful procedures in newborns admitted to the ICU. The authors report that physiological indicators (heart rate, respiratory rate, etc.), behavioral indicators (duration of crying, proportion of time spent crying, etc.), and pain rating scales were used to assess pain. Of the articles reviewed, heel lance and venepuncture were the most common painful procedures. Guzmán et al[10] propose in their study the psychotherapeutic manage
The remaining studies used different pain assessment scales. Among the most commonly used scales are NIPS[3,5,13,14,19,22-25], PIPP[3,5,13,19,22-24], Neonatal Facial Coding System[3,13,19,23,24], and N-PASS[5,13,23-25]. The CRIES, Susan Givens, or COMFORT scales have also been used[3,5,11,13,23]. Regarding pain man
According to Do Prado et al[13] non-pharmacological pain relief measures should be used for procedures causing mild pain, with non-nutritive suctioning and oral glucose being the most commonly used. While for procedures causing moderate or severe pain, pharmacological measures such as analgesics should be used. In contrast, Assunçao et al[19] believed that the aim of pharmacological measures is pain relief, while non-pharmacological measures are to reduce environmental stimuli and stress and to prevent physiological and behavioral alterations. In the study by Avila-Alvarez et al[21] they observed that among the pharmacological measures used, fentanyl was the most commonly used drug and receiving sedation or analgesia was associated with having invasive ventilation and scores > 3 on the Clinical Risk Index for Babies scale, the existence of pain assessment guidelines and a pain leader. As for the use of non-pharmacological measures, only 38.4% of patients received some type of oral sweet solution. This low percentage was related to the fact that no exhaustive records were kept of their administration, as is the case with pharmaceuticals, and to the reluctance of professionals to use them due to a lack of knowledge about their mechanism of action. Finally, the review carried out by Gonzalez et al[3] recommends that, if the procedure to be performed is very aggressive, non-pharmacological measures should be accompanied by drugs to be chosen according to the World Health Organization analgesic scale.
Nursing staff knowledge about neonatal pain: Six papers regarding nursing staff knowledge about neonatal pain were found[12,15-18,20](Table 2). Healthcare professionals consider both punctures and aspirations to be the most common painful procedures for newborns[12,15-18,20]. Other painful procedures are catheterizations[18,20] or dressings[12,20]. Regarding pain assessment, only two articles do not use any scale, with physical and behavioral responses being the way to assess newborn pain[12,20]. In the remaining studies, healthcare professionals combined some type of scale with physical/behavioral responses in order to assess pain. The most commonly used scale was the NIPS[15-17]. Non-pharmacological measures were used to control pain in only two studies[18,20]. The remaining studies used both pharmacological and non-pharmacological techniques[12,15-17]. Among the most commonly used non-pharmacological measures were non-nutritive suckling[12,15-18,20] and glucose intake[12,16,18,20]. The most commonly used pharmacological measures were non-opioid[12,15,17] and topical analgesics[15,17].
In general, the authors of these studies concluded that the professionals lacked training on this subject, and therefore, on occasions, the assessment of pain and its management in the newborn was not carried out adequately, as indicated by Veronez et al[12] in the study carried out on 25 professionals in a neonatal ICU. Santos et al[20] pointed out that the identification of pain was carried out in a fragmented and non-systematized way, not using scales for a more exhaustive assessment. However, they consider that the professionals were aware of and knew how to use adequately non-pharmacological measures to alleviate the newborn’s pain. In the study by Bonolo et al[17], they noted that some of the scales used to assess pain in newborns were not suitable for this age group. In addition, they considered that both work experience and professional qualifications influenced pain assessment and management. Do Nascimento et al[15] indicated that pain assessment should be carried out with multidimensional measures, taking into account the environmental context and subjective and objective variables. Furthermore, in the study they conducted, there were respondents who were not aware of the pain scales in use. Costa et al[16] concluded that strategies to transfer knowledge to professionals were needed to improve pain assessment and management. They found that, although nursing staff considered the systematic use of pain assessment scales important, they did not always use them, and considered that pain management should be carried out by a multidisciplinary team. Finally, the study by Alves et al[18] was based on the develop
After review was carried out, it is clear that newborns are exposed to several diagnostic, therapeutic, and surgical procedures that cause pain. In the research conducted by San Martín et al[11], 65.4 % of the newborns studied had moderate to severe pain. Neonates with a gestational age between 33-37 wk showed more pain. These results are consistent with other studies such as that of Thomé et al[14] where the level of pain suffered by patients was moderate to severe, with men experiencing more pain. Avila-Alvarez et al[21] also showed that the age range receiving the most analgesics was that of newborns between 37-42 wk. The most common causes of pain are invasive procedures, such as venepunctures, aspiration of secretions, heel lances, etc.[11,13,15,16,18,20,22-25]. Among punctures, several papers agree that venipunc
Regarding neonatal pain management and treatment, the nursing team has a very important role, based mainly on a pharmacological and non-pharmacological approach. Out of the 18 papers reviewed, 12 of them mentioned non-pharmacological measures used by the nursing staff to relieve neonatal pain[3,12,13,15-22,24], whilst 8 of them mention pharmacological measures[3,5,12,13,15,16,19,21]. The most common non-pharmacological measure was the oral administration of glucose/sucrose[3,12,13,16,18-20,22,24]. In accordance with the paper published by Stevens et al[24], the use of oral sucrose is effective in reducing pain caused by invasive procedures such as venepunctures, heel lancets, or intramuscular injections in both premature and full-term newborns. No side effects were observed. However, an optimal dose could not be identified. In this work, we have also taken into account a less frequent and innovative non-pharmacological method of pain management: The Sentire Method[10]. This method is based on pain control through music and touch. The authors observed that both heart and respiratory rate decreased with this method. Therefore, they concluded that music and touch helped relaxation, decreasing pain. Pain management by pharmacological interventions is normally used in moderate to severe cases. The most commonly used drugs for neonatal pain relief are opioids, non-opioids, and sedatives. According to Avila-Alvarez et al[21], in Spanish ICUs the most common pharmacological procedures were fentanyl infusions and the combination of fentanyl and midazolam.
With regard to the studies that mention nursing staff’s knowledge[12,15-18,20], in most cases we observed that nurses show some working experience in ICUs[12,15,16,20], although none of the papers mention specific training on pain management in newborns. The study carried out by Veronez et al[12] showed an average of 4.39 years of nursing team experience, while the study by Costa et al[16] showed a higher mean of 6.02 years. Regarding the perception of pain in newborns, healthcare professionals are aware that they feel pain and know its consequences in patients[12,15,17], although some of them consider that pain in newborns and adults is similar. This consideration is wrong, since newborns have a better perception of pain due to their limited ability to inhibit it[12]. In order to assess pain, in the study carried out by Costa et al[16], healthcare professionals were asked if they knew of any guidelines, protocols, or routines, and most of them (66.7%) did not know of any or did not know what to answer. In general, nurses use structured scales in order to assess newborns’ pain[15-17], although sometimes these scales are not suitable for neonates[17]. In other cases, due to lack of knowledge or training, nurses only identify pain through the patient's physical or behavioral alterations[12,15,20].
Despite the methodology used, the review may have some limitations regarding the following biases: Language bias, papers written in languages other than Spanish, English, or Portuguese have been excluded. This is a limitation, since there may be papers in other languages with relevant information on the topic. Selection bias: Determined by the criteria used to include and exclude papers in the review. In order to avoid this bias, we tried to define clearly these criteria and to be as objective as possible. Accessibility bias: Papers that we could not access with available resources were not included in this review. This could have caused lower quality results. Despite these biases, we consider that the subject of this review should be taken into account given the negative consequences of pain in newborns.
This article reviewed the literature on the assessment and management of pain in newborn admitted to the NICU. It has become evident that the neonates admitted to the NICUs are undergoing several painful procedures. The first step in addressing pain in newborns is a correct pain assessment, and nurses have a key role in this. Although several pain assessment scales have been validated, in clinical practice, most nurses do not use them or do not use them properly, therefore, the staff should be trained to make good use of them. Pain management is the second step in the approach to pain and, in this sense; the nursing team has an important role in carrying out non-pharmacological procedures.
There is a lack of protocols about management of neonatal pain in the ICUs as well as a scarce presence of pain management teams and/or leaders to address it correctly. If nursing wants to offer a more humane treatment to these patients, they must develop protocols and be part of the pain management teams. This way, there will be a standard procedure for pain assessment and management in NICUs.
Painful experiences in newborns can cause both short- and long-term side effects. Newborns admitted to the Neonatal Intensive Care Unit (NICU) are frequently subjected to procedures that will cause pain, which must be assessed and treated appropriately for its relief and well-being of the newborn.
To contribute to the knowledge of newborn pain and its assessment and management.
To define and assess the status of neonatal pain and pain management in newborns admitted to the NICU and to determine the knowledge of healthcare professionals about neonatal pain.
A search was carried out in different databases such as PubMed, Dialnet Plus, Cochrane Library Plus, Cuiden, and IBECS.
A total of 135 articles were found, and 18 articles were finally reviewed. Among the most painful and stressful procedures for NICU newborns were punctures. The methods used to assess pain were the observation of physical and behavioral alterations and validated scales, the most widely used being the Neonatal Infant Pain Scale. With regard to the knowledge of professionals, it has been observed that there is a lack of training on this subject, which is the making and carrying out of the correct assessment and management of pain.
Neonates admitted to the NICU undergo a number of painful procedures. It is essential that professionals have the appropriate knowledge to perform correct assessment and management of pain. This would require the development of protocols and multidisciplinary pain teams.
This document not only establishes the need for training of healthcare professionals to assess correctly and manage pain in newborns, based on evidence and not only on clinical practice or personal experience, but also the need for pain guidelines and pain teams to carry out quality care.
Manuscript source: Invited manuscript
Specialty type: Nursing
Country/Territory of origin: Spain
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Trkulja V S-Editor: Ma YJ L-Editor: Filipodia P-Editor: Ma YJ
| 1. | López SJ, Rivera LS. Historia del concepto de dolor total y reflexiones sobre la humanización de la atención a pacientes terminales. Revista Ciencias de la Salud. 2018;16:340-356. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Perez LE, Genovés CA, Muñoz IM. Valoración y manejo del dolor en neonatos. Enfermeria Integral: Revista cientifica del Colegio Oficial de Enfermeria de Valencia. 2011;9-12. |
| 3. | Gonzalez FC, Fernández MI. Revisión bibliográfica en el manejo del dolor neonatal. ENE Revista de Enfermería. 2012;6. |
| 4. | Perez VR, Villalobos AE, Aguayo GK, Guerrero FM. Valoración y estrategias no farmacológicas en el tratamiento del dolor neonatal. Rev Cubana Pediatr. 2006;78. |
| 5. | Avila-Alvarez A, Carbajal R, Courtois E, Pertega-Diaz S, Anand KJ, Muñiz-Garcia J; Grupo español del proyecto Europain. [Clinical assessment of pain in Spanish Neonatal Intensive Care Units]. An Pediatr (Barc). 2016;85:181-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 2.0] [Reference Citation Analysis (1)] |
| 6. | Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62:e1-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6253] [Cited by in RCA: 7637] [Article Influence: 477.3] [Reference Citation Analysis (1)] |
| 7. | Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, Moher D, Peters MDJ, Horsley T, Weeks L, Hempel S, Akl EA, Chang C, McGowan J, Stewart L, Hartling L, Aldcroft A, Wilson MG, Garritty C, Lewin S, Godfrey CM, Macdonald MT, Langlois EV, Soares-Weiser K, Moriarty J, Clifford T, Tunçalp Ö, Straus SE. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169:467-473. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22118] [Cited by in RCA: 18483] [Article Influence: 2640.4] [Reference Citation Analysis (1)] |
| 8. | Riva JJ, Malik KM, Burnie SJ, Endicott AR, Busse JW. What is your research question? J Can Chiropr Assoc. 2012;56:167-171. [PubMed] |
| 9. | Martinez NA, Gijón NG. La evidencia científica: método de la evaluación de resultados clínicos, el camino para la podología. Revista Española de Podología. 2017;28:58-60. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 10. | Guzmán SV, Nicolini PD, Domínguez TB, Guzmán MJ. Manejo psicoterapéutico del dolor a través de la música y el tacto: el Método Sentire. Estudios sobre las culturas contemporaneas. 2018;24:9-40. |
| 11. | San Martín GD, Valenzuela SS, Huaiquian SJ, Luengo ML. Dolor del recién nacido expuesto a procedimientos de enfermería en la unidad de neonatología de un hospital clínico chileno. Enfermeria Global. 2017;16:1-23. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 12. | Veronez M, Martins CD. A dor e o recém-nascido de risco: percepçao dos profissionais de enfermagem. Cogitare Enfermagem. 2010;15:263-270. [RCA] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Do Prado FA, Da Silva SA, Morato SM, Ramos Lima L. Abordagem terapêutica da dor em neonatos sob cuidados intensivos: uma breve revisão. Revista de Enfermagem do Centro Oeste Mineiro. 2012;2:108-123. [DOI] [Full Text] |
| 14. | Thomé CC, Sonego GJ, Kirchenr R, Fernandes E. Evaluation of pain of neonates during invasive procedures in intensive care. Rev dor. 2016;17:197-200. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 15. | Do Nascimento R, Rangel SL, Domingues Bernardes SM, Moreira CM. Avaliaçao da dor do recém-nascido na unidade terapia intensva neonatal sob o olhar dos profissionais de enfermagem de um hospital universitário. Revista de Pesquisa Cuidado é Fundamental Online. 2010;2:1410-1417. |
| 16. | Costa T, Rossato LM, Bueno M, Secco IL, Sposito NP, Harrison D, Freitas JS. Nurses' knowledge and practices regarding pain management in newborns. Rev Esc Enferm USP. 2017;51:e03210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 17. | Bonolo AJ, Alves RT, Contim D, Barichello E. Equipe de enfermagem diante da dor do recém-nascido pré-termo. Esc Anna Nery. 2014;18:241-246. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 18. | Alves CR, Costa R. Métodos nao farmacológicos para alivio do desconforto e da dor no recém-nascido:uma construçao coletiva da enfermagem. Texto contexto - enferm. 2014;23:185-192. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 19. | Assunçao SA, Vargas DI, Ribeiro SL. O enfermeiro no manejo da dor neonatal. Revista Baiana de Enfermagem. 2011;25:301-309. |
| 20. | Santos LM, Ribeiro IS, Santana RC. [Identification and treatment of pain in the premature newborn in the intensive care unit]. Rev Bras Enferm. 2012;65:269-275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 21. | Avila-Alvarez A, Carbajal R, Courtois E, Pertega-Diaz S, Muñiz-Garcia J, Anand KJ; Grupo Español del proyecto Europain. [Sedation and analgesia practices among Spanish neonatal intensive care units]. An Pediatr (Barc). 2015;83:75-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 22. | Aguilar Cordero MJ, Baena García L, Sánchez López AM, Mur Villar N, Fernández Castillo R, García García I. [Non pharmacological methods to reduce pain in newborns; systematic review]. Nutr Hosp. 2015;32:2496-2507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 23. | Dionysakopoulou C, Giannakopoulou M, Lianou L, Bozas E, Zannikos K, Matziou V. Validation of Greek Versions of the Neonatal Infant Pain Scale and Premature Infant Pain Profile in Neonatal Intensive Care Unit. Pain Manag Nurs. 2018;19:313-319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 24. | Stevens B, Yamada J, Ohlsson A, Haliburton S, Shorkey A. Sucrose for analgesia in newborn infants undergoing painful procedures. Cochrane Database Syst Rev. 2016;7:CD001069. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 132] [Cited by in RCA: 146] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 25. | Desai A, Aucott S, Frank K, Silbert-Flagg J. Comparing N-PASS and NIPS: Improving Pain Measurement in the Neonate. Adv Neonatal Care. 2018;18:260-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 21] [Article Influence: 3.0] [Reference Citation Analysis (0)] |