Published online Jul 16, 2021. doi: 10.12998/wjcc.v9.i20.5611
Peer-review started: February 8, 2021
First decision: March 27, 2021
Revised: April 7, 2021
Accepted: May 20, 2021
Article in press: May 20, 2021
Published online: July 16, 2021
Processing time: 148 Days and 16.6 Hours
Treatment-resistant schizophrenia is a severe form of schizophrenia characterized by poor response to at least two antipsychotic drugs and is typically treated with clozapine. However, clozapine lowers the epileptic threshold, leading to seizures, which are severe side effects of antipsychotics that result in multiple complications. Clozapine-related seizures are generally considered to be dose-dependent and especially rare in the low-dose (150-300 mg/d) clozapine treated population. Due to clinical rarity, little is known about its clinical characteristics and treatment.
A 62-year-old Chinese man with a 40-year history of treatment-resistant schizophrenia presented to the Emergency Department with symptoms of myoclonus, consciousness disturbance and vomiting after taking 125 mg clozapine. Upon admission, the patient had a suddenly generalized tonic-clonic seizure lasting for about half a minute with persistent disturbance of consciousness, fever, cough and bloody sputum, which was considered to be low-dose clozapine-related seizure. After antiepileptic and multiple anti-infection treatments, the patient was discharged without epileptic or psychotic symptoms.
Our aim is to highlight the early prevention and optimal treatment of clozapine-related seizure through case analysis and literature review.
Core Tip: Clozapine-related seizure is a serious adverse reactions of clozapine, which should be given more attention to its early prevention and optimal treatment. Clinical features, treatment options and factors that may contribute to the development of clozapine-related seizures were summarized through case analysis and literature review, and relevant cases published in the last 20 years were summarized and listed.
- Citation: Le DS, Su H, Liao ZL, Yu EY. Low-dose clozapine-related seizure: A case report and literature review . World J Clin Cases 2021; 9(20): 5611-5620
- URL: https://www.wjgnet.com/2307-8960/full/v9/i20/5611.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i20.5611
Clozapine, the first officially marketed atypical antipsychotic, has a unique therapeutic effect on treatment-resistant schizophrenia (TRS)[1] that significantly improves patients' quality of life, reduces violent and impulsive behavior[2] and reduces suicide and mortality rates[2-4]. Notably, the incidence of clozapine-related seizure is up to 4%-6%[5,6], which is higher than that of other typical or atypical antipsychotics[7] and will lead to further complications and ultimately increased mortality.
Clozapine-related seizures are generally considered to be dose-dependent and are rare in people treated with conventional doses of clozapine (300-450 mg/d), and especially rare in the low-dose (150-300 mg/d) clozapine treated population. Due to clinical rarity, little is known about its clinical characteristics and treatment. Thus, we herein report a 62-year-old Chinese male who had schizophrenia with low-dose clozapine-related seizure followed by aspiration pneumonia. Previous clinical cases of clozapine-related seizure were identified in a database and carefully reviewed to identify the clinical features, treatment options and factors that may contribute to the development of this rare disease entity.
A 62-year-old Chinese male presented to the Emergency Department of our hospital with complaints of myoclonus, consciousness disturbance and vomiting for 1 h.
In the absence of a caregiver, the patient was found lying unconscious with myoclonic movements, surrounded by vomit. The number of remaining tablets suggested 125 mg clozapine had been taken.
According to medical history, the patient has had TRS for 40 years, presenting with hallucinations, delusions, splitting of thought and a weak response to olanzapine, risperidone and perphenazine. The patient has been regularly taking clozapine 62.5 mg/d and quetiapine 300 mg/d for the last 10 years, and the mental symptoms were well controlled.
The patient has been regularly taking clozapine 62.5 mg/d and quetiapine 300 mg/d for the last 10 years, and the mental symptoms were well controlled. No family history of mental illness was reported.
Upon admission, the patient had a generalized tonic-clonic seizure (GTCS) lasting for about half a minute with persistent consciousness disturbance, fever, cough and bloody sputum.
Emergency laboratory tests revealed a white cell count of 10.11 × 109/L, 89.3% of which were neutrophils, and a high-sensitivity C-reactive protein content of 4.8 mg/L; the sputum culture indicated the presence of gram-negative bacilli. The blood concentration of clozapine was higher than 1500 ng/mL (reference: 350-600 ng/mL) at the 24th h and the 48th h after last administration. No other obvious abnormalities were found upon cerebrospinal fluid examination.
On the 10th day of hospitalization, the blood concentration of clozapine was 153 ng/mL (reference = 350-600 ng/mL).
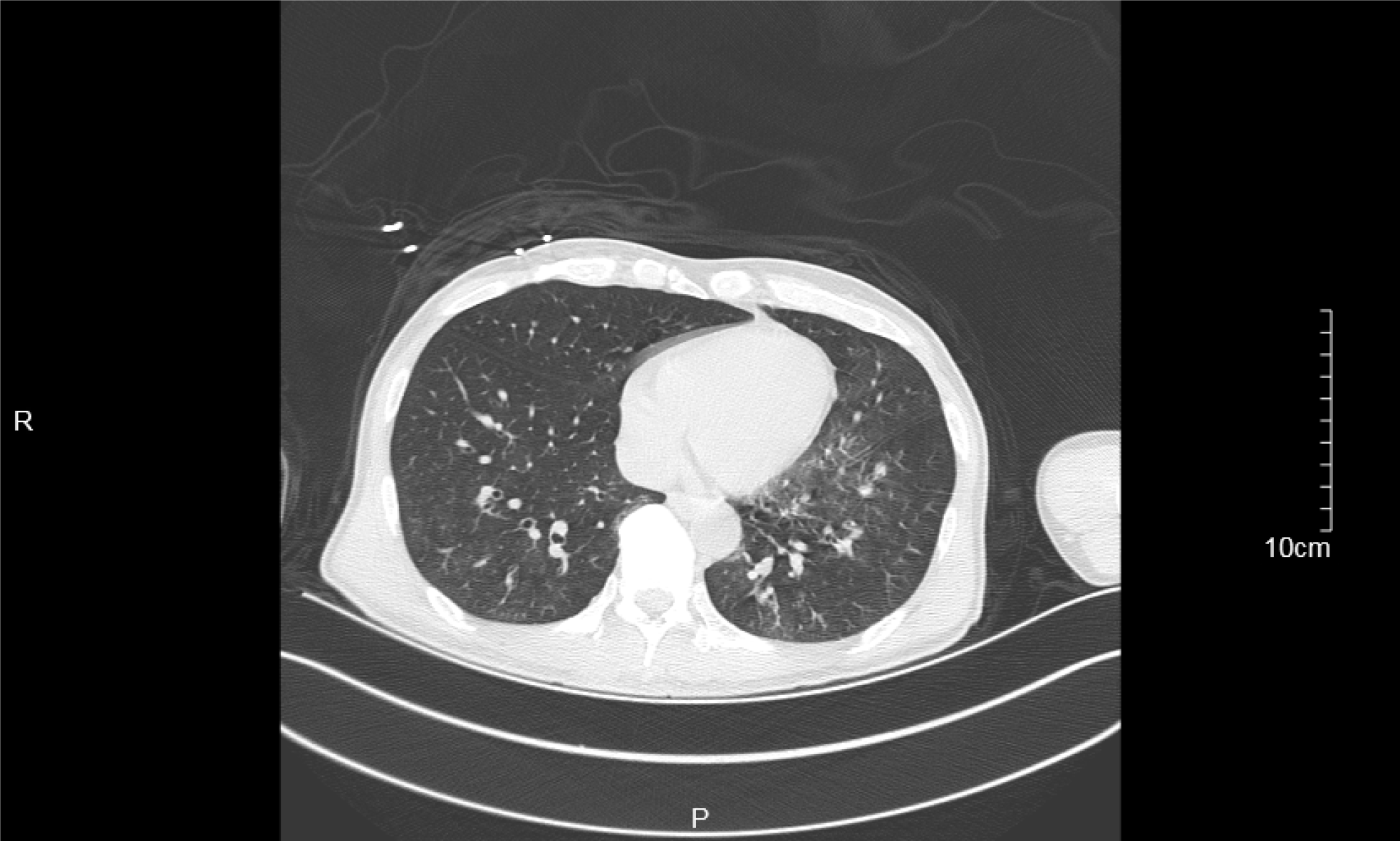
Emergency chest computed tomography indicated bilateral pneumonia with bilateral pleural effusion (Figure 1), and no other obvious abnormalities were found upon cranial computed tomography.
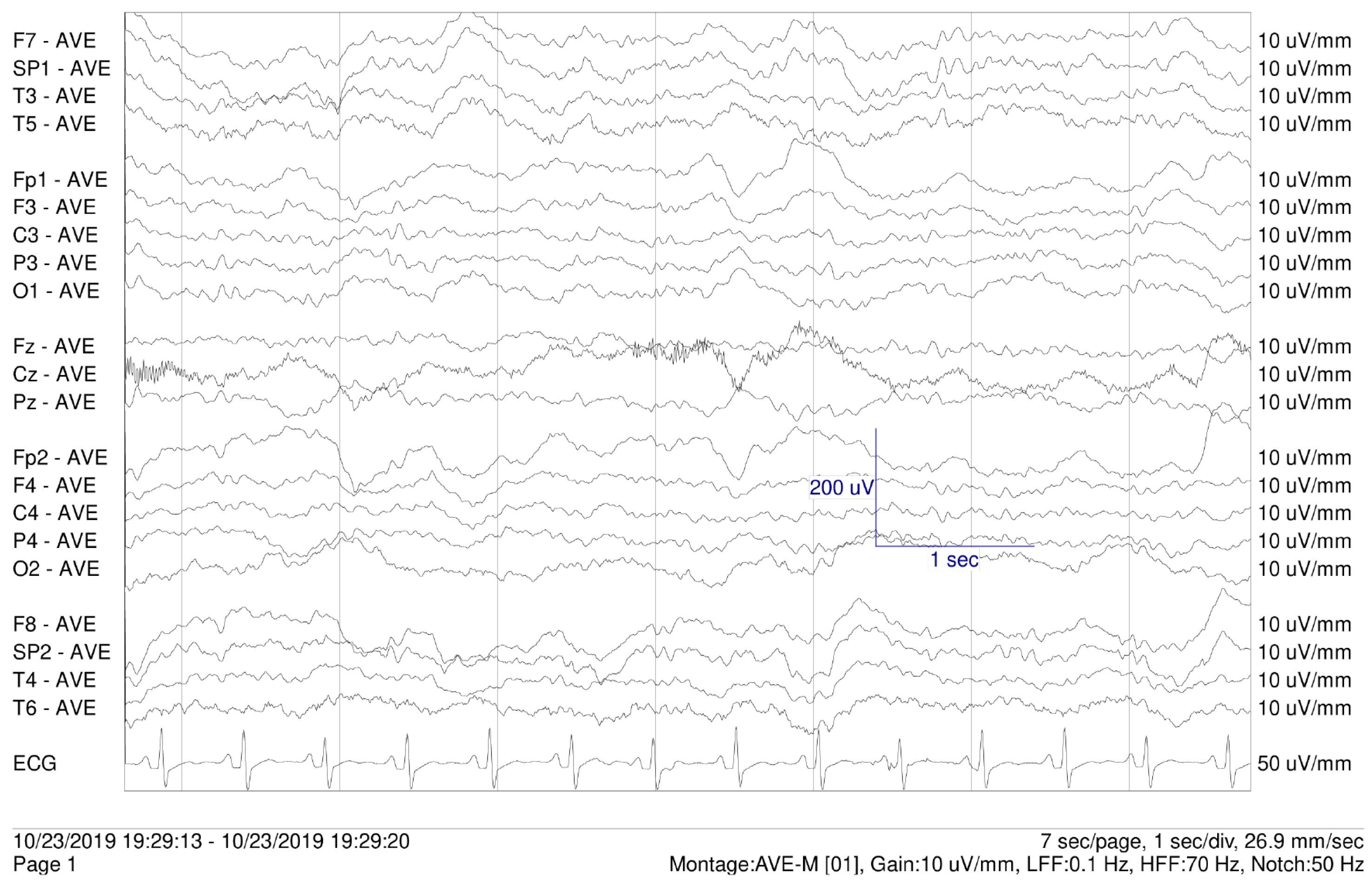
On the 3rd day of hospitalization, electroencephalogram (EEG) showed slow-wave and no epileptiform discharges (Figure 2).
Schizophrenia with low-dose clozapine-related seizure followed by aspiration pneumonia.
Treatment mainly included antiepileptic therapy, multiple anti-infection therapies, and psychotolytic therapy under the premise of the patency of airway.
After admission, clozapine was discontinued immediately, and sodium valproate 1000 mg/d, diazepam 2.5 mg/d, quetiapine 300 mg/d, acyclovir 500 mg/d and cefoperazone 2000 mg/d were administrated.
On the 5th day of hospitalization, the patient developed dyspnea with an oxygen saturation of 60%-70% and no significant improvement after sputum aspiration, which was considered as respiratory failure. Thus, immediate tracheal intubation and mechanical ventilatory support were performed, and the treatment regimens were adjusted as meropenem 2000 mg/d, capophenine 50 mg/d and levetiracetam 1000 mg/d in addition to atomization, phlegm reduction and enteral nutrition.
On the 11th day of hospitalization, psychotic symptoms were observed after extubation, hallucinations, and splitting of thought. Therefore, clozapine 25 mg/d (slowly increased to 62.5 mg over 2 wk) and quetiapine 300 mg/d were administered.
Eventually, the patient was discharged with no obvious seizures or psychotic symptoms and was satisfied with his treatment. After discharge, the patient took clozapine 62.5 mg/d and quetiapine 300 mg/d regularly under the supervision of a caregiver. During 3 mo of follow-up, the patient recovered well, and no exacerbations were detected.
Schizophrenia is a debilitating and heterogeneous mental disorder characterized by discordance between mental activity and the environment and manifests as a complex blend of positive and negative symptoms and cognitive impairment[8,9]. The lifetime suicide risk of patients with schizophrenia is 2 to 3 times higher than that in the general population[10], estimated to be about 5%[11], and life expectancy is about 20% less than that of the general population[12]. TRS, which is characterized by poor response to at least two antipsychotic drugs, is a severe form of schizophrenia that accounts for approximately one-third of all schizophrenia cases[13].
Clozapine not only has better effects on positive and negative symptoms and cognitive impairment than typical antipsychotics but also is associated with fewer adverse reactions[1,2]. Moreover, clozapine has unique therapeutic effects against TRS[1] that can significantly improve patients’ quality of life, reduce violence and impulsive behaviors[2] and decrease the suicide rate and mortality[2-4]. However, the incidence of clozapine-related seizure is 4%-6%[5,6], which is higher than that of seizures related to typical antipsychotics[7]. Moreover, the uncertainty and unpredictability of epileptic seizures are closely related to negative emotions[14], which may result in the generation, maintenance or exacerbation of mental disorders[15].
In this case, EEG examinations were not performed in a timely manner, and no significant abnormalities were found in subsequent EEG reports. No psychometric scale results were reported, and the evaluation of therapeutic efficacy for schizophrenia was based primarily on clinical presentation. This case does not prove a link between low-dose clozapine, seizure and pneumonia nor does it reflect the wider population. Therefore, a review of the previous literature and a summary of the published case reports is necessary.
The mechanism of clozapine-related seizure may be caused by the combined action of multiple receptors. Dopamine has been shown to reduce the excitability of the primary sensorimotor cortex in adult rats[16]. Clozapine may increase cortical excitability by reducing dopamine neurotransmission[16]. Serotonin receptors are expressed in almost all neural networks associated with seizure. Consumption of serotonin in the brain can enhance the excitability of neurons, reduce the seizure threshold and increase seizure frequency[17]. The antiepileptic effects of selective serotonin reuptake inhibitors have been demonstrated in controlled trials[18].
Clozapine-related seizure is widely considered as dose-dependent[6]. Standard titration of clozapine refers to starting at a dosage of 12.5-25 mg/d and increasing the dosage by 25-50 mg/d to reach a maintenance dosage of 300-400 mg/d after 2 wk[19]. This slow titration method can reduce the risk of seizure, but it may extend the treatment time or require the combination of clozapine with other drugs to control mental symptoms over time[19,20]. In contrast, the rapid increase regimen can quickly control psychiatric symptoms and reduce medical costs[19,21] but may lead to unnecessarily high drug doses that cause adverse drug reactions such as seizure. However, in some clinical trials, the rapid titration of clozapine was reported to be safe and effective and to be beneficial for aggressive or suicidal patients[19,22].
The dosage regimen of clozapine directly affects blood concentration. A study showed that the risk of seizure is 3% when the dose of clozapine does not exceed 300 mg/d, that the risk increases to 8% when the dose is 325 to 500 mg/d and that the risk is as high as 38% when the dose exceeds 500 mg/d[6]. The lower limit of the therapeutic range for clozapine serum levels is between 250 and 420 ng/mL, and the risk of seizure increases when the serum level is > 750 ng/mL[23] and increases significantly when the serum level exceeds 1300 ng/mL[24]. Moreover, for every 100 mg/d increase in daily dose of clozapine, the abnormal rate of EEG increases by 8%, and for every 100 mg/L increase in plasma level of clozapine, the rate increases by 12%[25]. However, the serum level is affected by age[23], gender[26], smoking status[23], caffeine use[27] and other factors, hence, neither the serum level nor the dose of clozapine could accurately predict the occurrence of seizure. In clinical practice, most practitioners take 600 mg/d as the safety threshold[5], but cases of clozapine-related seizure have also been reported in the low-dose (150-300 mg/d)[28] treatment group[29,30]. Literature was systematically retrieved from electronic databases (PubMed and Web of Science) to review cases of clozapine-related seizure published between 2000 and 2019. A total of 18 studies were included (Table 1)[6,29-35], eight of which reported 14 cases of low-dose clozapine-related seizure.
| Ref. | Year | Gender | Age | Clozapine dose (mg/d) | Type of seizure |
| Haberfellner[31] | 2002 | Female | 29 | 150 | Myoclonus and GTCS |
| Praharaj et al[32] | 2010 | Male | 38 | 250 | Myoclonus |
| Horga et al[33] | 2010 | Male | 15 | 300 | GTCS |
| Park et al[34] | 2014 | Female | 26 | 300 | GTCS |
| Kikuchi et al[35] | 2014 | Female | 24 | 300 | Myoclonus |
| Grover et al[6] | 2015 | Male | 54 | 200 | GTCS |
| Bolu et al[29] | 2017 | Male | 29 | 200 | GTCS |
| Borah et al[30] | 2019 | Female | 42 | 300 | Jerky movement of limbs |
| Male | 63 | 275 | GTCS | ||
| Male | 25 | 250 | GTCS | ||
| Female | 34 | 225 | GTCS | ||
| Female | 34 | 150 | GTCS | ||
| Female | 22 | 300 | Myoclonus | ||
| Female | 25 | 275 | Myoclonus |
Antiepileptic drugs (AEDs) are widely used in the treatment of clozapine-related seizures. Some authors believe that the dose of clozapine should be reduced by 40%-50% when a seizure occurs for the first time and that AEDs should not be started until the second seizure is observed[36]. In clinical cases, dose reduction may lead to recurrence of psychiatric symptoms[37]. There are also studies suggesting that the continued use of clozapine is beneficial for patients and that AEDs starting at a dosage of 500 mg/d should be used[5]. However, the use of AEDs such as lamotrigine[38], levetiracetam[38] and topiramate[39] may increase the risk of mental illness through increasing central dopamine activity[40], and drug interactions may lead to other adverse reactions[24]. Thus, AEDs are not recommended as the main preventive agents before the occurrence of clozapine-related seizure[24].
Valproate, a broad-spectrum AED, is currently widely regarded as the first choice for the treatment of clozapine-related seizure and has a significant therapeutic effect on GTCS[5] and myoclonus[33,41]. Valproate is especially suitable for patients with affective disorders because of its emotional stabilization and antimania effects[42]. Interestingly, valproic acid can reduce clozapine plasma concentrations[5,25,41], allowing patients to continue to use it safely. It also allows clozapine-treated patients to remain seizure-free.
Electroconvulsive therapy involves stimulation of the brain through electric currents and has been reported to increase the levels of dopamine and its metabolites[43]. Electroconvulsive therapy has been regarded as an effective treatment[44] for mental illness since the 1930s, and it can effectively reduce the frequency of seizures in patients that show insufficient responses to AEDs[45]. In addition, intracranial electroencephalographic monitoring has been found to have important clinical value in human experimental reports, and it may be used in the monitoring of drug-related seizures in the future[46]. Monitoring still has some potential safety risks that need to be further studied and reduced[46].
This case demonstrates the clinical presentation of and effective treatments for low-dose clozapine-related seizure followed by aspiration pneumonia. We reviewed the associated literature to identify the influencing factors and summarized the research progress of clozapine-related seizure to potential provide ideas for early clinical prevention and treatment (Table 2)[6,29-35,41,47-55]. Given the limited nature of case reports and the urgent clinical need, this field should be taken seriously and further studied.
| Ref. | Year | Age | Gender | Dose of clozapine | Blood concentration of clozapine | Blood concentration of norclozapine | Type of seizure | EEG | Antiepileptic drugs | Further use of clozapine | Other psychiatric drugs |
| Usiskin et al[47] | 2000 | 15 | M | 400 mg/d | - | - | Myoclonus and GTCS | Bihemispheric epileptiform activity | Gabapentin 2100 mg/dClonazepam 2 mg/d | 300 mg/d | Olanzapine 25 mg/d |
| Navarro et al[48] | 2001 | 23 | F | 200 mg/d | - | - | GTCS | Bihemispheric epileptiform activity | Topiramate 200 mg/d | 200 mg/d | - |
| Haberfellner[31] | 2002 | 29 | F | 150 mg/d | - | - | Myoclonus and GTCS | Paroxysmal generalized spikes | - | 100 mg/d | Haloperidol 10 mg/d |
| Duggal et al[49] | 2002 | 28 | M | 300 mg/d | - | - | Stuttering | - | - | - | - |
| 425 mg/d | - | - | GTCS | Generalized nonparoxysmal slowing and a photic convulsive response | Valproate 800 mg/d | 300 mg/d | - | ||||
| Foster et al[50] | 2005 | 32 | F | 125 mg/d | - | - | TCS | - | - | - | - |
| 237.5 mg/d | - | - | TCS | - | Valproate 500 mg/d | 450 mg/d | Citalopram 20 mg/d | ||||
| Begum et al[51] | 2005 | - | - | 300 mg/d | - | - | Myoclonus and stuttering | - | Valproate 400 mg/d | 300 mg/d | - |
| Muzyk et al[52] | 2010 | 20 | M | 600 mg/d | - | - | Myoclonus and GTCS | - | Lamotrigine 200 mg/d | 550 mg/d | Lithium 900 mg/d |
| Praharaj et al[32] | 2010 | 38 | M | 250 mg/d | - | - | Myoclonus | Bilateral frontal theta waves and sharp–slow wave | Clonazepam 1000 mg/d | 250 mg/d | - |
| Horga et al[33] | 2010 | 15 | M | 350 mg/d | - | - | Speech dysfluency and myoclonus | - | - | 300 mg/d | Clomipramine 225 mg/d |
| 300 mg/d | - | - | GTCS | Generalized andMultifocal paroxysmal epileptiform discharges | Sodium valproate 500 mg/d | 300 mg/d | Clomipramine 225 mg/d | ||||
| Leung et al[53] | 2014 | 52 | F | 450 mg/d | 1400 ng/mL (36 h after the last dose) | 606 ng/mL (36 h after the last dose) | Myoclonus | - | - | 225.5 mg/d | - |
| Park et al[34] | 2014 | 26 | F | 450 mg/d | - | - | GTCS | - | - | 300 mg/d | - |
| 300 mg/d | - | - | GTCS | No epileptiform discharge | Valproate 250 mg | Drug withdrawal | ECT, risperidone 6 mg/d, escitalopram 15 mg/d | ||||
| Kikuchi et al[35] | 2014 | 19-48 | F (n = 12) | 275-600 mg/d | - | - | TCS and myoclonic (n =1) TCS (n = 1) Myoclonic (n = 4) | Spike and slow wave | Lamotrigine 150-300 mg/d (n = 2) Valproate 400-800 mg/d (n = 3) | 200-550 mg/d | - |
| Grover et al[6] | 2015 | 24-63 | F (n = 3) M (n = 9) | 150-600 mg/d | - | - | GTCS (n = 12) | - | Lamotrigine (n = 1) Valproate 1000 mg/d (n = 3) | 150-600 mg/d | Haloperidol (n = 1) Sertraline 75 mg/d (n = 1) |
| Osborne et al[41] | 2015 | 20 | M | 400 mg/d | 140 ng/mL | 130 ng/mL | Myoclonus | - | - | - | - |
| 400 mg/d | 180 ng/mL | 150 ng/mL | GTCS | - | Valproate 1000 mg/d | 475 mg/d | - | ||||
| Bolu et al[29] | 2017 | 29 | M | 200 mg/d | - | - | TCS | Bilateral diffuse epileptic activity | Valproate 1000 mg/d | 100 mg/d | - |
| Rachamallu et al[54] | 2017 | 16 | M | 350 mg/d | - | - | Orofacial dyskinesia with perioral twitching | - | - | - | - |
| 400 mg/d | - | - | Stuttering | Several episodes of generalized spike | Valproate 1000 mg/d | 450 mg/d | - | ||||
| Borah et al[30] | 2019 | 42 | F | 300 mg/d | - | - | Twitching and urinary incontinence | - | - | 250 mg/d | Haloperidol 10 mg/d |
| Chochol et al[55] | 2019 | 57 | M | 600 mg/d | 866 ng/mL | 301 ng/mL | Myoclonus and stuttering | Bilateral sharp waves and slow wave complexes | - | 300 mg/d | Risperidone 1.5 mg/d, Risperidone 37.5 mg every 2 wk |
Manuscript source: Unsolicited Manuscript
Specialty type: Psychiatry
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kai K S-Editor: Ma YJ L-Editor: Filipodia P-Editor: Li JH
| 1. | Schrader JM, Irving CM, Octeau JC, Christian JA, Aballo TJ, Kareemo DJ, Conti J, Camberg JL, Lane JR, Javitch JA, Kovoor A. The differential actions of clozapine and other antipsychotic drugs on the translocation of dopamine D2 receptors to the cell surface. J Biol Chem. 2019;294:5604-5615. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 2. | Nucifora FC Jr, Mihaljevic M, Lee BJ, Sawa A. Clozapine as a Model for Antipsychotic Development. Neurotherapeutics. 2017;14:750-761. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 111] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 3. | Taipale H, Tanskanen A, Mehtälä J, Vattulainen P, Correll CU, Tiihonen J. 20-year follow-up study of physical morbidity and mortality in relationship to antipsychotic treatment in a nationwide cohort of 62,250 patients with schizophrenia (FIN20). World Psychiatry. 2020;19:61-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 263] [Article Influence: 52.6] [Reference Citation Analysis (0)] |
| 4. | Vermeulen JM, van Rooijen G, van de Kerkhof MPJ, Sutterland AL, Correll CU, de Haan L. Clozapine and Long-Term Mortality Risk in Patients With Schizophrenia: A Systematic Review and Meta-analysis of Studies Lasting 1.1-12.5 Years. Schizophr Bull. 2019;45:315-329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 162] [Article Influence: 27.0] [Reference Citation Analysis (0)] |
| 5. | Williams AM, Park SH. Seizure associated with clozapine: incidence, etiology, and management. CNS Drugs. 2015;29:101-111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 80] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 6. | Grover S, Hazari N, Chakrabarti S, Avasthi A. Association of Clozapine with Seizures: A Brief Report Involving 222 Patients Prescribed Clozapine. East Asian Arch Psychiatry. 2015;25:73-78. [PubMed] |
| 7. | Lertxundi U, Hernandez R, Medrano J, Domingo-Echaburu S, García M, Aguirre C. Antipsychotics and seizures: higher risk with atypicals? Seizure. 2013;22:141-143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 57] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 8. | Owen MJ, Sawa A, Mortensen PB. Schizophrenia. Lancet. 2016;388:86-97. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1067] [Cited by in RCA: 1289] [Article Influence: 143.2] [Reference Citation Analysis (1)] |
| 9. | Schulz SC, Murray A. Assessing cognitive impairment in patients with schizophrenia. J Clin Psychiatry. 2016;77 Suppl 2:3-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 10. | Brown S, Kim M, Mitchell C, Inskip H. Twenty-five year mortality of a community cohort with schizophrenia. Br J Psychiatry. 2010;196:116-121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 411] [Cited by in RCA: 443] [Article Influence: 29.5] [Reference Citation Analysis (0)] |
| 11. | Hor K, Taylor M. Suicide and schizophrenia: a systematic review of rates and risk factors. J Psychopharmacol. 2010;24:81-90. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 648] [Cited by in RCA: 555] [Article Influence: 37.0] [Reference Citation Analysis (0)] |
| 12. | Crump C, Winkleby MA, Sundquist K, Sundquist J. Comorbidities and mortality in persons with schizophrenia: a Swedish national cohort study. Am J Psychiatry. 2013;170:324-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 398] [Cited by in RCA: 440] [Article Influence: 36.7] [Reference Citation Analysis (0)] |
| 13. | Siskind D, Siskind V, Kisely S. Clozapine Response Rates among People with Treatment-Resistant Schizophrenia: Data from a Systematic Review and Meta-Analysis. Can J Psychiatry. 2017;62:772-777. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 267] [Article Influence: 33.4] [Reference Citation Analysis (0)] |
| 14. | Błaszczyk B, Czuczwar SJ. Epilepsy coexisting with depression. Pharmacol Rep. 2016;68:1084-1092. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 76] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 15. | Kovac S, Walker MC. Recent advances in epilepsy. J Neurol. 2014;261:837-841. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 16. | Hosp JA, Hertler B, Atiemo CO, Luft AR. Dopaminergic modulation of receptive fields in rat sensorimotor cortex. Neuroimage. 2011;54:154-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 17. | Pottoo FH, Javed MN, Barkat MA, Alam MS, Nowshehri JA, Alshayban DM, Ansari MA. Estrogen and Serotonin: Complexity of Interactions and Implications for Epileptic Seizures and Epileptogenesis. Curr Neuropharmacol. 2019;17:214-231. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 36] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 18. | Alper K, Schwartz KA, Kolts RL, Khan A. Seizure incidence in psychopharmacological clinical trials: an analysis of Food and Drug Administration (FDA) summary basis of approval reports. Biol Psychiatry. 2007;62:345-354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 344] [Cited by in RCA: 301] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 19. | Ifteni P, Teodorescu A, Dima L, Burtea V. Rapid Titration of Clozapine in Schizophrenia and Bipolar Disorder. Am J Ther. 2021;28:e224-e227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 20. | Lochhead JD, Nelson MA, Schneider AL. Risks and Benefits of Rapid Clozapine Titration. Ment Illn. 2016;8:6457. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 21. | Poyraz CA, Özdemir A, Sağlam NG, Turan Ş, Poyraz BÇ, Tomruk N, Duran A. Rapid Clozapine Titration in Patients with Treatment Refractory Schizophrenia. Psychiatr Q. 2016;87:315-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 22. | Ifteni P, Correll CU, Nielsen J, Burtea V, Kane JM, Manu P. Rapid clozapine titration in treatment-refractory bipolar disorder. J Affect Disord. 2014;166:168-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 38] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 23. | Ulrich S, Baumann B, Wolf R, Lehmann D, Peters B, Bogerts B, Meyer FP. Therapeutic drug monitoring of clozapine and relapse--a retrospective study of routine clinical data. Int J Clin Pharmacol Ther. 2003;41:3-13. [PubMed] |
| 24. | Caetano D. Use of anticonvulsants as prophylaxis for seizures in patients on clozapine. Australas Psychiatry. 2014;22:78-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 25. | Varma S, Bishara D, Besag FM, Taylor D. Clozapine-related EEG changes and seizures: dose and plasma-level relationships. Ther Adv Psychopharmacol. 2011;1:47-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 108] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 26. | Tang YL, Mao P, Li FM, Li W, Chen Q, Jiang F, Cai ZJ, Mitchell PB. Gender, age, smoking behaviour and plasma clozapine concentrations in 193 Chinese inpatients with schizophrenia. Br J Clin Pharmacol. 2007;64:49-56. [PubMed] |
| 27. | Rajkumar AP, Poonkuzhali B, Kuruvilla A, Jacob M, Jacob KS. Clinical predictors of serum clozapine levels in patients with treatment-resistant schizophrenia. Int Clin Psychopharmacol. 2013;28:50-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 71] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 28. | Subramanian S, Völlm BA, Huband N. Clozapine dose for schizophrenia. Cochrane Database Syst Rev. 2017;6:CD009555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 29] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 29. | Bolu A, Akarsu S, Pan E, Aydemir E, Oznur T. Low-dose Clozapine-induced Seizure: A Case Report. Clin Psychopharmacol Neurosci. 2017;15:190-193. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 30. | Borah AJ, Kalita A, Dutta SK. Clozapine-induced seizure. Indian J Pharmacol. 2019;51:410-412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 31. | Haberfellner EM. Myoclonic and generalized tonic clonic seizures during combined treatment with low doses of clozapine and haloperidol. Eur Psychiatry. 2002;17:55-56. [PubMed] |
| 32. | Praharaj SK, Venkatesh BG, Sarkhel S, Zia-ul-Haq M, Sinha VK. Clozapine-induced myoclonus: a case study and brief review. Prog Neuropsychopharmacol Biol Psychiatry. 2010;34:242-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 33. | Horga G, Horga A, Baeza I, Castro-Fornieles J, Lázaro L, Pons A. Drug-induced speech dysfluency and myoclonus preceding generalized tonic-clonic seizures in an adolescent male with schizophrenia. J Child Adolesc Psychopharmacol. 2010;20:233-234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 34. | Park S, Lee MK. Successful electroconvulsive therapy and improvement of negative symptoms in refractory schizophrenia with clozapine-induced seizures: a case report. Psychiatr Danub. 2014;26:360-362. [PubMed] |
| 35. | Kikuchi YS, Sato W, Ataka K, Yagisawa K, Omori Y, Kanbayashi T, Shimizu T. Clozapine-induced seizures, electroencephalography abnormalities, and clinical responses in Japanese patients with schizophrenia. Neuropsychiatr Dis Treat. 2014;10:1973-1978. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 30] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 36. | Wong J, Delva N. Clozapine-induced seizures: recognition and treatment. Can J Psychiatry. 2007;52:457-463. [PubMed] |
| 37. | Murphy R, Gallagher A, Sharma K, Ali T, Lewis E, Murray I, Hallahan B. Clozapine-induced stuttering: an estimate of prevalence in the west of Ireland. Ther Adv Psychopharmacol. 2015;5:232-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 38. | Anzellotti F, Franciotti R, Zhuzhuni H, D'Amico A, Thomas A, Onofrj M. Nonepileptic seizures under levetiracetam therapy: a case report of forced normalization process. Neuropsychiatr Dis Treat. 2014;10:959-964. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 39. | Mula M, Trimble MR. The importance of being seizure free: topiramate and psychopathology in epilepsy. Epilepsy Behav. 2003;4:430-434. [PubMed] |
| 40. | Kawakami Y, Itoh Y. Forced Normalization: Antagonism Between Epilepsy and Psychosis. Pediatr Neurol. 2017;70:16-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 41. | Osborne IJ, McIvor RJ. Clozapine-induced myoclonus: a case report and review of the literature. Ther Adv Psychopharmacol. 2015;5:351-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 42. | Brodtkorb E, Mula M. Optimizing therapy of seizures in adult patients with psychiatric comorbidity. Neurology. 2006;67:S39-S44. [PubMed] |
| 43. | Nikisch G, Mathé AA. CSF monoamine metabolites and neuropeptides in depressed patients before and after electroconvulsive therapy. Eur Psychiatry. 2008;23:356-359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 57] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 44. | Stefanou MI, Vittore D, Wolz I, Klingberg S, Wildgruber D. Recurrent Episodes of Paraphilic Behavior Possibly Associated With Olanzapine and Aripiprazole Treatment in a Patient With Schizophrenia. Front Psychiatry. 2020;11:318. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 45. | Chi SH, Jeong HG, Lee S, Oh SY, Kim SH. Effects of Psychotropic Drugs on Seizure Threshold during Electroconvulsive Therapy. Psychiatry Investig. 2017;14:647-655. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (1)] |
| 46. | Cook MJ, O'Brien TJ, Berkovic SF, Murphy M, Morokoff A, Fabinyi G, D'Souza W, Yerra R, Archer J, Litewka L, Hosking S, Lightfoot P, Ruedebusch V, Sheffield WD, Snyder D, Leyde K, Himes D. Prediction of seizure likelihood with a long-term, implanted seizure advisory system in patients with drug-resistant epilepsy: a first-in-man study. Lancet Neurol. 2013;12:563-571. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 533] [Cited by in RCA: 547] [Article Influence: 45.6] [Reference Citation Analysis (0)] |
| 47. | Usiskin SI, Nicolson R, Lenane M, Rapoport JL. Gabapentin prophylaxis of clozapine-induced seizures. Am J Psychiatry. 2000;157:482-483. [PubMed] |
| 48. | Navarro V, Pons A, Romero A, Bernardo M. Topiramate for clozapine-induced seizures. Am J Psychiatry. 2001;158:968-969. [PubMed] |
| 49. | Duggal HS, Jagadheesan K, Nizamie SH. Clozapine-induced stuttering and seizures. Am J Psychiatry. 2002;159:315. [PubMed] |
| 50. | Foster R, Olajide D. A case of clozapine-induced tonic-clonic seizures managed with valproate: implications for clinical care. J Psychopharmacol. 2005;19:93-96. [PubMed] |
| 51. | Begum M. Clozapine-induced stuttering, facial tics and myoclonic seizures: a case report. Aust N Z J Psychiatry. 2005;39:202. [PubMed] |
| 52. | Muzyk A, Gala G, Kahn DA. Use of lamotrigine in a patient with a clozapine-related seizure. J Psychiatr Pract. 2010;16:125-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 53. | Leung JG, Nelson S, Takala CR, Gören JL. Infection and inflammation leading to clozapine toxicity and intensive care: a case series. Ann Pharmacother. 2014;48:801-805. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 38] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 54. | Rachamallu V, Haq A, Song MM, Aligeti M. Clozapine-Induced Microseizures, Orofacial Dyskinesia, and Speech Dysfluency in an Adolescent with Treatment Resistant Early Onset Schizophrenia on Concurrent Lithium Therapy. Case Rep Psychiatry. 2017;2017:7359095. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (1)] |
| 55. | Chochol MD, Kataria L, OʼRourke MC, Lamotte G. Clozapine-Associated Myoclonus and Stuttering Secondary to Smoking Cessation and Drug Interaction: A Case Report. J Clin Psychopharmacol. 2019;39:275-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |