Published online Jan 16, 2021. doi: 10.12998/wjcc.v9.i2.489
Peer-review started: September 20, 2020
First decision: September 29, 2020
Revised: October 9, 2020
Accepted: November 29, 2020
Article in press: November 29, 2020
Published online: January 16, 2021
Processing time: 110 Days and 8.3 Hours
Sinusoidal obstructive syndrome (SOS) is a disease that damages hepatic sinusoidal endothelial cells, resulting in progressive occlusion and fibrosis of the lobular central vein and the occurrence of intrahepatic sinusoidal portal hypertension. However, SOS after liver transplantation (LT) is uncommon and potentially fatal. Here, we report a rare case of second-time recurrence of SOS after liver retransplantation (rLT).
A 22-year-old woman received a living donor LT due to SOS. Four years later, she developed abdominal distention and ascites with no apparent cause. She was diagnosed with recurrence of SOS and underwent rLT. But 2 mo post rLT, the patient suffered from aggravated jaundice and ascites again. She was diagnosed with second-time recurrence of SOS post-rLT according to computed tomography and liver pathology. After treatment with warfarin anticoagulation and immunosuppressant conversion, she gradually recovered with improvement of liver function and liver pathology. During the 17-mo follow-up period, she was in good condition with normal liver function and no ascites.
SOS can be a recurrent disease after LT, and autoimmune antibody and genetic sequencing should be screened before LT. For susceptible patients, anticoagulant drugs should be used for an extended period, and tacrolimus or other pathogenic agents should be avoided. Early diagnosis and treatment can improve the prognosis of patients and avoid graft failure or death.
Core Tip: Sinusoidal obstructive syndrome (SOS) is a complex entity with incompletely defined pathogenesis. It is also an uncommon complication after liver transplantation. We reported a rare case of SOS that recurred twice in liver allografts. We believed that this condition is uncommon and has rarely been reported in liver transplant recipients.
- Citation: Liu Y, Sun LY, Zhu ZJ, Wei L, Qu W, Zeng ZG. Is sinusoidal obstructive syndrome a recurrent disease after liver transplantation? A case report . World J Clin Cases 2021; 9(2): 489-495
- URL: https://www.wjgnet.com/2307-8960/full/v9/i2/489.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i2.489
Sinusoidal obstructive syndrome (SOS) is a rare disorder with a unique etiopathogenesis related to endothelial toxicity leading to fibrotic obliteration of the hepatic centrilobular veins with congestion and hemorrhage[1,2]. Liver transplantation (LT) is an effective treatment for SOS patients with severe liver failure. SOS after LT is very rare with an incidence of 1.9%-2.9%, but it includes a risk for graft failure. Some cytotoxic drugs and/or immunologic responses may be associated with this entity, but the causes and pathophysiological processes of SOS after LT are not well known[3]. Onset of SOS is characterized by ascites, hepatomegaly and jaundice. Here, we describe an unusual case of second-time recurrence of SOS after liver retransplantation (rLT).
A 27-year-old woman came to our center due to aggravated abdominal distension and ascites for 1 mo.
Two months ago, she received rLT from a donation after cardiac death in our center for recurrence of SOS after LT. She recovered well and was discharged on postoperative day 25 under treatment with methylprednisolone, tacrolimus, mycophenolate mofetil and warfarin. One month later, she developed progressive abdominal distension and mild elevation of transaminase with no apparent cause. Abdominal ultrasound showed massive ascites without vascular abnormality.
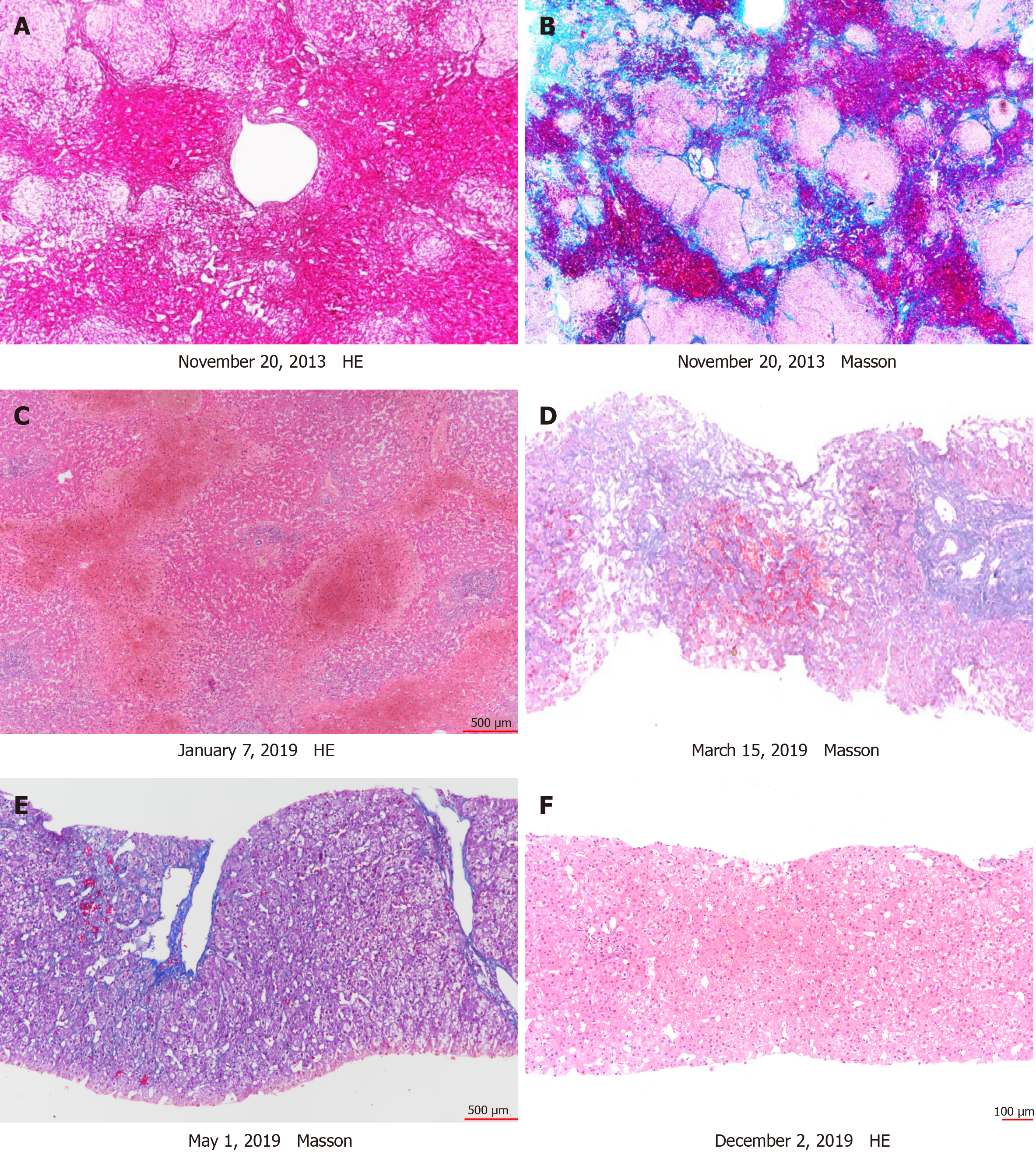
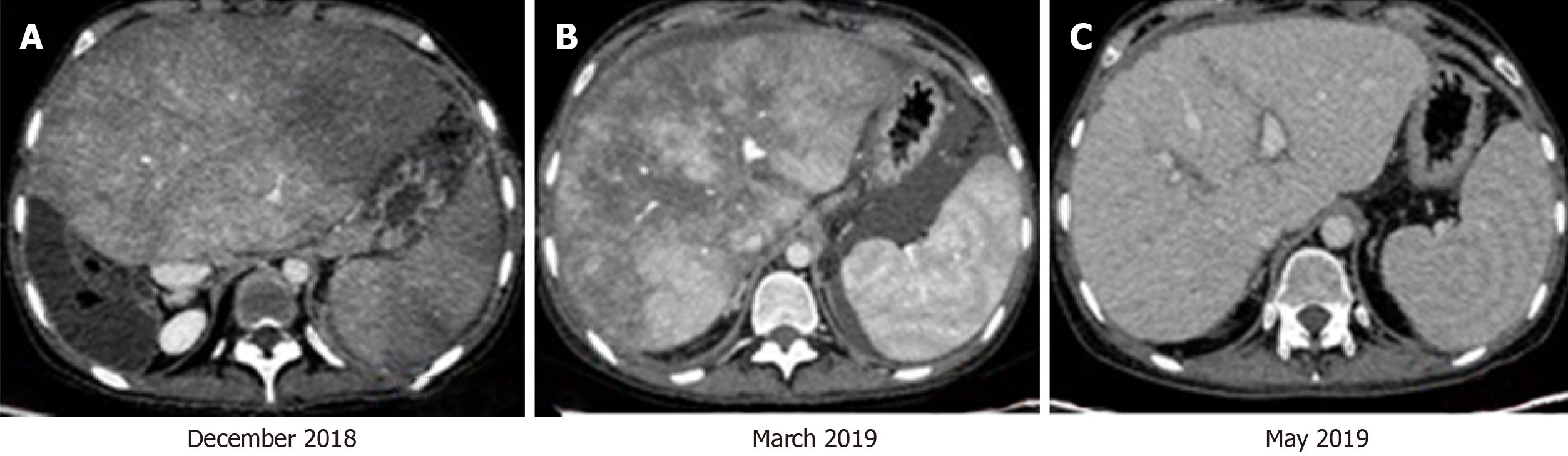
Five years ago, she underwent a living donor LT for SOS (Figure 1). Initially she recovered well with an immunosuppressive regimen of cyclosporine A and mycophenolate mofetil. One year ago, she developed abdominal distension and ascites. She was diagnosed with recurrence of SOS by computed tomography (CT) and histopathology (Figures 1 and 2). She was treated with diuretics and anticoagulants, but her ascites and abdominal distension were aggravated, along with jaundice. She had no abnormal personal and family history.
Her body temperature, blood pressure, heart rate and breathing rate were within normal limits. Main positive signs were cutaneous and sclera icterus with abdominal bulge and shifting dullness.
Laboratory results suggested that alanine aminotransferase was 61 IU/L, glutamic oxaloacetylase was 39.9 IU/L, alkaline phosphatase was 90 IU/L, glutamyl transpeptidase was 103 IU/L, total bilirubin was 40.85 μmol/L, direct bilirubin was 31.7 μmoL/L and creatinine was 130 mol/L. Tacrolimus trough level was 12.4 ng/mL. Testing for thrombophilia showed that she was positive for anticardiolipin antibody (ACL). Protein C, protein S and homocysteine were negative.
Abdominal ultrasound showed hepatomegaly with heterogenous echoes and seroperitoneum. CT revealed hepatomegaly with patchy enhancement and ascites (Figure 2). Then transjugular venography and liver biopsy were performed. Hepatic venography showed no stenosis of the hepatic vein or inferior vena cava, but hepatic venous pressure gradient was 21 mmHg. Liver pathology showed sinusoidal dilatation and congestion (Figure 1).
On the basis of these findings, she was diagnosed with second-time recurrence of SOS post-rLT.
Based on our past experience and literature review, tacrolimus was stopped and replaced with cyclosporine A, and warfarin was continued at 3 mg/d and was adjusted according to International Normalized Ratio (2-3).
After treatment, ascites gradually decreased with improvement of liver and renal function. Four months post-rLT, CT and histological examination were reviewed. The results showed that hepatomegaly, heterogeneous enhancement, sinusoidal dilatation and congestion were all relieved (Figures 1 and 2). During the 17 mo follow-up period, she was in good condition with normal liver function and no ascites.
SOS is a rare but fatal complication after LT, which can lead to graft failure and death. Although the pathogenesis of SOS after LT remains unknown, it is reported to be associated with azathioprine or tacrolimus[3], episodes of acute rejection[4], oxaliplatin-containing chemotherapy[5], irradiation[6] and intake of pyrrolizidine-alkaloid-containing plants[7]. In our case, the patient’s primary disease was SOS of unknown cause. After rLT, SOS recurred for the second time similar to the episode after the first LT. After withdrawal of tacrolimus, the patient experienced rapid clinical improvement, which was confirmed by imaging and histological examination. Tacrolimus may have potential cytotoxicity for endothelial cells and precipitate their dysregulation as reported[8].
In this case, it is strange that SOS occurred in the native liver and in the two subsequent liver allografts. We hypothesize that there may be something unusual in the patient initiating the thrombotic process. In our case, test for thrombotic disorder showed that ACL was positive. ACLs have been found in some patients with autoimmune disorder, acute infection or cardiovascular disease, and they have been associated with arterial and venous thrombosis[9,10]. Therefore, the patient likely had a form of thrombotic disorder leading to recurrence of SOS. Anticoagulation therapy with warfarin was administered at a dose of 3 mg/d. We performed a literature review and retrieved only two cases[11,12] in which SOS recurred sequentially in the two liver allografts (Table 1). In the case Fiel et al[12] reported, the patient also tested positive for high levels of ACL antibodies. Ansari et al[13] observed that whole exome sequencing can find high-risk patients with genetic susceptibility in pediatric patients with SOS after hematopoietic stem cell transplantation[13]. Some gene variants are associated with SOS in children receiving intravenous busulfan and cyclopho-sphamide before hematopoietic stem cell transplantation[14]. Therefore, repeated relapse of SOS is probably associated with antibody-mediated autoimmune response or genetic susceptibility. In these patients, SOS may be a recurrent disease after LT, and autoimmune antibody and genetic sequencing should be screened before LT. During the post-LT period, anticoagulant drugs should be used for a long time and tacrolimus or other potential pathogenic agents should be avoided.
| Ref. | Year of publication | Age in yr | Gender | Primary disease | Operation | IS | ACR post LT | Time of first SOS occurrence | ACR post rLT | Time of second recurrence | Pathologic findings | Complication post third LT |
| Martins et al[11] | 2007 | 20 | F | Type I autoimmune cirrhosis | LT | CsA/FK506 + Pre + Aza | Yes | 2 yr | Yes | 3 yr | Fibrous obliteration of centrilobular veins by connective tissue | Biliary stenosis; autoimmune hepatitis |
| Fiel et al[12] | 1999 | 37 | F | Primary sclerosing cholangitis | LT | FK506 + Pre + Aza | No | 2 mo | No | 20 mo | Obliteration of terminal hepatic venules by dense fibrosis | - |
We reported a rare case of SOS that recurred twice in liver allografts. Treatment of anticoagulation and immunosuppressant adjustment can be effective in reducing the symptoms. Although the patient has remained asymptomatic after drug adjustment, close monitoring is still needed in case of a third relapse. Though this is a single case, with the greater understanding of the disease, further studies will be of great help for the investigation of pathogenesis.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Rauchfuss F S-Editor: Fan JR L-Editor: Filipodia P-Editor: Li JH
| 1. | Poli E, Kounis I, Guettier C, Verstuyft C, Coilly A, Sobesky R, Feray C, Vibert E, Ciacio O, Samuel D, Bismuth H, Duclos-Vallée JC. Post-Liver Transplantation Sinusoidal Obstruction Syndrome With Refractory Ascites Induced by Mycophenolate Mofetil. Hepatology. 2020;71:1508-1510. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 2. | Piccin A, Sartori MT, Bisogno G, Van Schilfgaarde M, Saggiorato G, Pierro AMD, Corvetta D, Marcheselli L, Andrea M, Gastl G, Cesaro S. New insights into sinusoidal obstruction syndrome. Intern Med J. 2017;47:1173-1183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 3. | Shen T, Feng XW, Geng L, Zheng SS. Reversible sinusoidal obstruction syndrome associated with tacrolimus following liver transplantation. World J Gastroenterol. 2015;21:6422-6426. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 15] [Cited by in RCA: 19] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 4. | Kitajima K, Vaillant JC, Charlotte F, Eyraud D, Hannoun L. Intractable ascites without mechanical vascular obstruction after orthotopic liver transplantation: etiology and clinical outcome of sinusoidal obstruction syndrome. Clin Transplant. 2010;24:139-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Choi JH, Won YW, Kim HS, Oh YH, Lim S, Kim HJ. Oxaliplatin-induced sinusoidal obstruction syndrome mimicking metastatic colon cancer in the liver. Oncol Lett. 2016;11:2861-2864. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 6. | Fan CQ, Crawford JM. Sinusoidal obstruction syndrome (hepatic veno-occlusive disease). J Clin Exp Hepatol. 2014;4:332-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 202] [Cited by in RCA: 191] [Article Influence: 17.4] [Reference Citation Analysis (0)] |
| 7. | Yang XQ, Ye J, Li X, Li Q, Song YH. Pyrrolizidine alkaloids-induced hepatic sinusoidal obstruction syndrome: Pathogenesis, clinical manifestations, diagnosis, treatment, and outcomes. World J Gastroenterol. 2019;25:3753-3763. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 64] [Cited by in RCA: 52] [Article Influence: 8.7] [Reference Citation Analysis (3)] |
| 8. | Li L, Dong Y, Li RD, Tao YF, Shen CH, Wang ZX. Sinusoidal obstruction syndrome related to tacrolimus following liver transplantation. Hepatobiliary Pancreat Dis Int. 2020;19:299-302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Wang D, Lv W, Zhang S, Zhang J. Advances in the Research on Anticardiolipin Antibody. J Immunol Res. 2019;2019:8380214. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 10. | Tsuchimoto A, Matsukuma Y, Ueki K, Nishiki T, Doi A, Okabe Y, Nakamura M, Tsuruya K, Nakano T, Kitazono T, Masutani K. Thrombotic microangiopathy associated with anticardiolipin antibody in a kidney transplant recipient with polycythemia. CEN Case Rep. 2019;8:1-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Martins A, Monteiro E, Freire A, Carvalho A, Veloso J, Morbey A, Carrilho I, Martins A, Barroso E. Hepatic veno-occlusive disease after liver transplantation: an unusual case report. Transpl Int. 2007;20:1072-1073. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Fiel MI, Schiano TD, Klion FM, Emre S, Hytiroglou P, Ishak KG, Suriawinata A, Thung SN. Recurring fibro-obliterative venopathy in liver allografts. Am J Surg Pathol. 1999;23:734-737. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 13. | Ansari M, Petrykey K, Rezgui MA, Del Vecchio V, Cortyl J, Ralph RO, Nava T, Beaulieu P, St-Onge P, Jurkovic Mlakar S, Huezo-Diaz Curtis P, Uppugunduri CRS, Lesne L, Théoret Y, Chalandon Y, Bartelink IH, Boelens JJ, Bredius RGM, Dalle JH, Lewis V, Kangarloo BS, Peters C, Sinnett D, Bittencourt H, Krajinovic M; Pediatric Disease Working Party of the European Society for Blood and Marrow Transplantation. Genetic Susceptibility to Hepatic Sinusoidal Obstruction Syndrome in Pediatric Patients Undergoing Hematopoietic Stem Cell Transplantation. Biol Blood Marrow Transplant. 2020;26:920-927. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 14. | Huezo-Diaz Curtis P, Uppugunduri CRS, Muthukumaran J, Rezgui MA, Peters C, Bader P, Duval M, Bittencourt H, Krajinovic M, Ansari M. Association of CTH variant with sinusoidal obstruction syndrome in children receiving intravenous busulfan and cyclophosphamide before hematopoietic stem cell transplantation. Pharmacogenomics J. 2018;18:64-69. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |