Published online Jan 16, 2021. doi: 10.12998/wjcc.v9.i2.372
Peer-review started: June 6, 2020
First decision: August 8, 2020
Revised: August 22, 2020
Accepted: November 29, 2020
Article in press: November 29, 2020
Published online: January 16, 2021
Processing time: 215 Days and 17.9 Hours
Massive esophageal variceal bleeding can be catastrophic, leading to high morbidity and mortality. Patients experiencing massive esophageal variceal bleeding are at high risk of aspiration and hemorrhagic shock in acute episodes. Intubation and bleeding control are the two essential steps for resuscitation of these patients.
A 47-year-old male patient was admitted to our hospital with upper digestive tract bleeding. He was diagnosed with alcohol-induced liver cirrhosis and consequent esophagogastric varices. As he did not show a good response to somatostatin and Sengstaken-Blakemore tube placement, the patient was scheduled for endoscopic angiotherapy under anesthesia. Preoperative assessment showed an ASA physical status of III and Child-Pugh classification B. However, massive hemorrhage occurred just after induction of anesthesia. Intubation by video-guided laryngoscopy in the lateral decubitus position was attempted twice and was successful. After that, an experienced endoscopic ultrasound (EUS) specialist performed angiotherapy and occluded the culprit vessel. An ultra-thin gastroscope was then inserted into the endotracheal tube to extract the blood observed in the lobar bronchi. The patient suffered hemorrhagic shock with an estimated blood loss of 1500 mL in 20 min and remained in the intensive care unit for two days. The patient was discharged from our hospital eight days later without major complications.
Intubation in the lateral decubitus position and EUS-guided treatment can be life-saving procedures in patients with massive upper gastrointestinal hemorrhage.
Core Tip: Intubation in the lateral decubitus position, which can be easily achieved with the help of video-guided laryngoscopy, is an option in emergency situations to protect the airway. In addition, endoscopic ultrasound (EUS) is effective in stopping acute massive hemorrhage from esophageal varices due to the enhanced sonography of EUS from fluid. This case highlights the importance of both the intubation and EUS-guided therapy in the management of acute massive hemorrhage caused by esophageal varices.
- Citation: Wen TT, Liu ZL, Zeng M, Zhang Y, Cheng BL, Fang XM. Lateral position intubation followed by endoscopic ultrasound-guided angiotherapy in acute esophageal variceal rupture: A case report. World J Clin Cases 2021; 9(2): 372-378
- URL: https://www.wjgnet.com/2307-8960/full/v9/i2/372.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i2.372
Esophagogastric varices have a high perioperative bleeding risk. Variceal bleeding accounts for 15%-50% of mortality in acute episodes[1,2]. Airway protection is of great concern under such circumstances, as patients are at a great danger of aspiration and further suffocation. However, it is difficult to accomplish intubation in patients with active massive esophageal bleeding. Intubation in the lateral position in various emergency situations has been documented and can be a useful option to manage patients at high risk of aspiration and difficult airway[3-6].
To regain homeostasis, endoscopic procedures are the primary treatment recommended for hemorrhagic control[1,7]. Recently, endoscopic ultrasound (EUS), which enables direct visualization of the varices, has become a promising approach in bleeding control with a lower risk of complications[8-10]. However, EUS endoscope, which has a larger diameter (> 13 cm) than conventional digestive endoscope (< 10 cm), is difficult to tolerate in a conscious patient. Therefore, anesthesia or sedation is generally performed[11,12].
Here we report a case where intubation in the left lateral decubitus position followed by the use of EUS-guided angiotherapy successfully managed a patient with massive hemorrhage due to ruptured esophageal varices.
A 47-year old male patient was admitted to our hospital due to intermittent vomiting of blood for four days.
The patient was a heavy alcohol drinker for 15 years. He complained of no symptoms until hematemesis four days previously, which occurred for the first time.
The patient was free from other illnesses.
Before anesthesia, the patient showed vital signs in the normal range. He was pale, but cooperative. He showed no signs of jaundice or cyanosis.
A routine blood test showed moderate anemia (hemoglobin 70 g/L), hypoleuko-cytemia (leukocytes, 2.5 × 109/L), and thrombocytopenia (thrombocytes, 39 × 109/L). A routine blood biochemical examination showed normal liver enzyme levels, an albumin level of 34.6 g/L, a total bilirubin level of 42 mmol/L, a direct bilirubin level of 30.5 mmol/L, an indirect bilirubin level of 12.4 mmol/L, and a creatinine level of 164 mmol/L. Coagulation was slightly abnormal with an activated partial thromboplastin time of 28 s, a prothrombin time of 16.6 s and an international normalized ratio of 1.5.
Moderate ascites was observed from ultrasonography. Bilateral plural effusion, portal thrombosis, hepatomegaly and splenomegaly were detected by liver computed tomography angiography.
The patient was diagnosed with alcohol-induced chronic liver disease, hepatic cirrhosis, portal vein hypertension and consequent esophagogastric varices.
Somatostatin was administered to stop the bleeding, but the patient did not respond well. Intermittent bleeding continued, as shown by vomiting of blood twice, dark stool and a continuous decline in hemoglobin level even after RBC transfusion. A Sengstaken-Blakemore tube was placed to prevent further bleeding, which was ineffective. Thus, endoscopic therapy was scheduled and the patient was transferred to the endoscopic suite. A Sengstaken-Blakemore tube with deflated balloons was placed in the upper gastrointestinal tract and served as a drainage tube.
A preoperative assessment showed an ASA physical status of III and a Child-Pugh classification B. After the patient was transferred to the examination bed, he was positioned in the left lateral decubitus position as routinely performed at our endoscopic center. Oxygenation through a nasal catheter with 5 L of oxygen was provided. The Sengstaken-Blakemore tube was then extracted. Before anesthetic induction, the patient’s vital signs showed a non-invasive blood pressure (NIBP) of 110/65 mmHg, a peripheral oxygen saturation (SpO2) of 97%, and a heart rate of 70 bpm. Anesthesia was induced with 0.3 mg/kg of etomidate and 0.3 mcg/kg of remifentanil. Suddenly, massive blood came from the patient’s mouth before intubation. The oxygen supply through the nasal catheter was subsequently increased to the maximum. The first attempt at intubation using video laryngoscopy failed as the vocal cords could not be seen due to massive blood flow. To optimize the condition for intubation, a suction tube was placed upon the lower pyriform fossa with maximum suction force. The patient remained in the left lateral position with the head tilted upwards at 30 degrees. A second attempt at intubation with video laryngoscopy was then carried out which was successful. During this process, SpO2 dropped to 65% and recovered to 100% after intubation. Aspiration of blood into the trachea was inevitable and was observed under laryngoscopy due to massive bleeding.
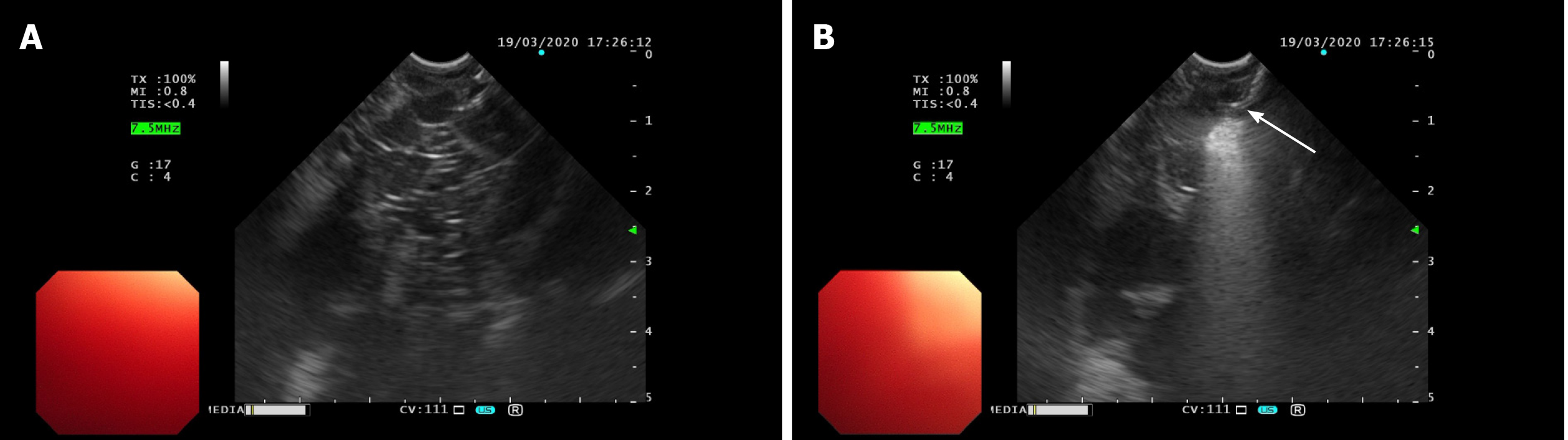
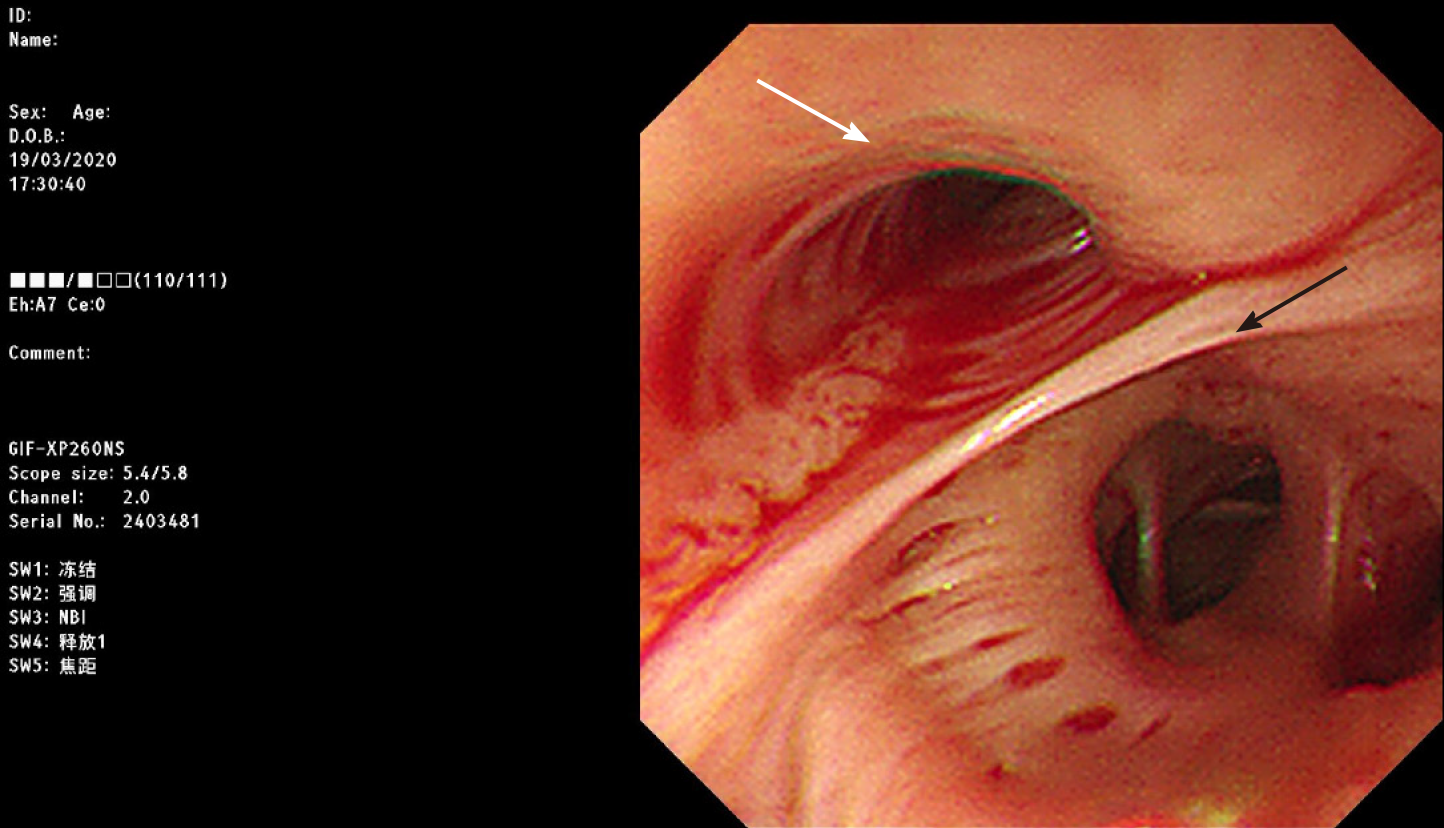
Immediately after intubation, an experienced endoscopist performed EUS endoscopy. The esophageal varices covered by blood were not visible through direct endoscopic view, but were detected during ultrasound scanning (Figure 1A). Sclerosing and adhesive agents were injected into the suspected varices in the lower part of the esophagus at two points (3 mL of polidocanol, 0.5 mL of cyanoacrylate and then 3 mL of polidocanol at each point) (Figure 1B). Bleeding stopped immediately. The whole endoscopic procedure took approximately five minutes. Next, an ultra-thin gastroscope with an outer diameter of 0.58 cm was inserted into the trachea through the endotracheal tube to drain the blood. Blood was observed coming from both the left and right lobar bronchi. Suction was performed until blood was no longer visible (Figure 2).
Hemorrhagic shock was noted with a NIPB of 60/40 mmHg. Fluid resuscitation, norepinephrine infusion and transfusion of red blood cell concentrate were immediately started to treat hemorrhagic shock. Afterwards, the patient was transported to the intensive care unit (ICU) for further treatment. Aspiration pneumonia was not observed after EUS-guided angiotherapy upon prophylactic intravenous piperacillin sodium and sulbactam sodium administration. C-reactive protein and procalcitonin level remained in the normal range after endoscopic treatment during his hospital stay.
The patient was extubated the next day and remained in ICU for two days without major complications. Eight days after endoscopic angiotherapy the patient was discharged from hospital.
Acute variceal bleeding is a life-threatening condition and is the most common reason for liver cirrhosis-related death. Massive acute hemorrhage is challenging to manage with high mortality rates. Airway protection and bleeding control are the two essential treatments used to resuscitate such patients in acute episodes. However, both treatments are difficult to accomplish. In the present case, the patient was successfully managed with lateral intubation and EUS-guided angiotherapy to obtain homeostasis.
Whether intubation is beneficial for patients with acute massive bleeding is still controversial. Anesthesia with or without intubation can be safely provided for stable patients with esophagogastric varices without massive bleeding. The role of anesthesia is to sedate patients and to make the endoscopic procedure easy and safe under continuous monitoring. However, two retrospective studies concluded that prophylactic intubation did not prevent cardiopulmonary complications in patients undergoing endoscopy for upper gastrointestinal hemorrhage[13,14]. In accordance with this, some clinicians suggested that intubation predicts worse outcomes after esophageal variceal bleeding. However, some clinicians suggest that it is extremely important to intubate patients to avoid aspiration in those with suspected variceal bleeding presenting with hematemesis[15]. In real crisis circumstances, the outcomes of the patients rely on their condition, the clinicians’ knowledge and experiences, the timing of intubation, hemorrhagic control, and teamwork of the anesthesiologists, surgeons/endoscopists and nurses.
The aspiration rate in the lateral decubitus position is presumed to be lower than that in the supine position. So far, the evidence to support this is sparse. One report from Takenaka and Aoyama showed in a manikin model that the aspiration rate is lower in the semi-lateral and lateral position[16]. In the real clinical setting, the aspiration rate is difficult to judge, as lateral position intubation is not adopted routinely in general due to the unfamiliarity of the anesthesiologist with this procedure. To draw such conclusions, a large number of subjects is needed. Furthermore, adverse effects, such as aspiration, which can range from mild to severe, are very likely to be missed in patient records. Retrospective studies are difficult to conduct for these two reasons. Thus, large-scale prospective trials are required in the future.
In our experience, intubation in the lateral position is safe and feasible[17,18]. Therefore, the lateral decubitus position is used routinely for patients who attend our endoscopic suite, both for intubational and non-intubational procedures. In our experience, the key to this depends on the following two steps. First, the anesthesiologist needs to expose the vocal cords with the help of video laryngoscopy. Video-guided laryngoscopy is more helpful for intubation than direct laryngoscopy, with the latter being more dependent on the position of the patient. Second, the anesthesiologist needs to turn the head and trunk to the same sagittal axis as the patient, which is similar to intubation in the supine position. This technique is easy to master and some authors have suggested that it should be included in trainees’ curricula[19]. Intubation in the lateral decubitus position can be a life-saving technique in patients experiencing difficult airway situations or in patients with restricted posture.
An ultra-thin gastroscope with an outer diameter of approximately 0.6 cm could be used in emergency situations as tracheal bronchoscope for guiding intubation and suction. Although a higher level of disinfection is required for bronchoscope than for digestive endoscope, the success of the intubation is considered a priority over avoiding infection in life-saving situations. When aspiration occurs, suction with digestive endoscope will not result in worse pneumonic infection as the airway is already contaminated. An endotracheal tube ≥ 7.0 cm in size is wide enough to let an ultra-thin gastroscope pass through. As in our case, ultra-thin gastroscopy is used for suction. In another difficult airway episode, we used ultra-thin gastroscopy-guided intubation where video laryngoscopy could not expose the vocal cords. Intubation with ultra-thin gastroscopy is an option when fiberoptic bronchoscopy is not available. To our knowledge, not every digestive endoscopic center is equipped with fiberoptic bronchoscope.
The reason for the acute massive bleeding in this patient was thought to be due to extraction of the Sengstaken-Blakemore tube. Even though it was deflated, long-time use of the balloon tamponade is associated with esophageal ulcers, which are vulnerable to any friction. This might have been the case in this patient[20,21]. There was a five-minute lag between tube extraction and induction of anesthesia. During this time, the esophagus served as a container for the blood. Once anesthetized, blood in large volume flowed out from the esophagus as the larynx muscle was relaxed. Aspiration could not be avoided as the protective laryngopharyngeal vagal reflex was also lost. Patients with long-time placement of a Sengstaken-Blakemore tube require special attention when they come to the endoscopic suite, which implies a high risk of re-bleeding perioperatively[22].
EUS is a promising procedure for hemorrhagic control[8-10]. Treatment of acute esophagogastric variceal bleeding includes fluid resuscitation, early use of vasoactive drugs, prophylactic use of antibiotics and endoscopic therapy. Endoscopic band ligation is the recommended first-line treatment during acute episodes of bleeding due to its safety and lower incidence of complications. Endoscopic injection of sclerosing or adhesive agents is also an option for variceal bleeding[23,24]. However, the success of these procedures largely relies on visualization of the varices and cooperation of the patient. In acute massive hemorrhage episodes, the view during direct endoscopy is largely compromised, as the upper digestive tract can be covered by a large amount of blood. In addition, the patient could be in a panic and not cooperate with endoscopic treatment when awake. This will further increase the difficulty for the endoscopist to perform the treatment. Ultrasound endoscopy, in which sonography is facilitated by fluid, allows injection of sclerosing and adhesive agent into varices under EUS guidance, resulting in less embolic complications[25].
In conclusion, intubation in the lateral decubitus position is feasible in patients with massive hemorrhage. Lateral decubitus position can be used both for intubational and non-intubational patients. In addition, EUS is effective in acute massive esophageal bleeding control when performed by an experienced endoscopist. Both the technique and effective teamwork of the anesthesiologist and endoscopist are key elements in patient management.
We would like to thank the EUS specialist, Dr. Hong-Tan Chen, from the Department of Gastroenterology, The First Affiliated Hospital, School of Medicine, Zhejiang University, China, for his valuable advice and discussion.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Altonbary AY, Casadesus D, Matowicka-Karna J S-Editor: Liu JH L-Editor: Webster JR P-Editor: Wang LL
| 1. | Jairath V, Rehal S, Logan R, Kahan B, Hearnshaw S, Stanworth S, Travis S, Murphy M, Palmer K, Burroughs A. Acute variceal haemorrhage in the United Kingdom: patient characteristics, management and outcomes in a nationwide audit. Dig Liver Dis. 2014;46:419-426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 69] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 2. | Reverter E, Tandon P, Augustin S, Turon F, Casu S, Bastiampillai R, Keough A, Llop E, González A, Seijo S, Berzigotti A, Ma M, Genescà J, Bosch J, García-Pagán JC, Abraldes JG. A MELD-based model to determine risk of mortality among patients with acute variceal bleeding. Gastroenterology 2014; 146: 412-19. e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 205] [Cited by in RCA: 264] [Article Influence: 24.0] [Reference Citation Analysis (0)] |
| 3. | Lim JA, Jeong MY, Kim JH. Airway management using laryngeal mask airway (LMA) in a patient in a lateral decubitus position: A case report. Medicine (Baltimore). 2019;98:e18287. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 4. | Singh N, Rao PB, Samal RL. TruView Video Laryngoscope for Lateral Position Intubation in a Patient With Giant Presacral Neurofibroma. J Emerg Med. 2019;57:380-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Kaur H, Singh G, Singh A, Kaur M, Sharda G. Video laryngoscope as an assist tool in lateral position laryngoscopy. Anesth Essays Res. 2016;10:373-375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Mahajan C, Rath GP, Bithal PK, Mahapatra AK. Perioperative Management of Children With Giant Encephalocele: A Clinical Report of 29 Cases. J Neurosurg Anesthesiol. 2017;29:322-329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 7. | Magaz M, Baiges A, Hernández-Gea V. Precision medicine in variceal bleeding: Are we there yet? J Hepatol. 2020;72:774-784. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 57] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 8. | Mohan BP, Chandan S, Khan SR, Kassab LL, Trakroo S, Ponnada S, Asokkumar R, Adler DG. Efficacy and safety of endoscopic ultrasound-guided therapy vs direct endoscopic glue injection therapy for gastric varices: systematic review and meta-analysis. Endoscopy. 2020;52:259-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 76] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 9. | ASGE Technology Committee, Trikudanathan G, Pannala R, Bhutani MS, Melson J, Navaneethan U, Parsi MA, Thosani N, Trindade AJ, Watson RR, Maple JT. EUS-guided portal vein interventions. Gastrointest Endosc. 2017;85:883-888. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 10. | Bick BL, Al-Haddad M, Liangpunsakul S, Ghabril MS, DeWitt JM. EUS-guided fine needle injection is superior to direct endoscopic injection of 2-octyl cyanoacrylate for the treatment of gastric variceal bleeding. Surg Endosc. 2019;33:1837-1845. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 52] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 11. | Campbell JA, Irvine AJ, Hopper AD. Endoscopic ultrasound sedation in the United Kingdom: Is life without propofol tolerable? World J Gastroenterol. 2017;23:560-562. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 6] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 12. | Cheriyan DG, Byrne MF. Propofol use in endoscopic retrograde cholangiopancreatography and endoscopic ultrasound. World J Gastroenterol. 2014;20:5171-5176. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 17] [Cited by in RCA: 27] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 13. | Rudolph SJ, Landsverk BK, Freeman ML. Endotracheal intubation for airway protection during endoscopy for severe upper GI hemorrhage. Gastrointest Endosc. 2003;57:58-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 67] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 14. | Rehman A, Iscimen R, Yilmaz M, Khan H, Belsher J, Gomez JF, Hanson AC, Afessa B, Baron TH Sr, Gajic O. Prophylactic endotracheal intubation in critically ill patients undergoing endoscopy for upper GI hemorrhage. Gastrointest Endosc. 2009;69:e55-e59. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 30] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 15. | Krystallis C, Masterton GS, Hayes PC, Plevris JN. Update of endoscopy in liver disease: more than just treating varices. World J Gastroenterol. 2012;18:401-411. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 16] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (1)] |
| 16. | Takenaka I, Aoyama K. Prevention of aspiration of gastric contents during attempt in tracheal intubation in the semi-lateral and lateral positions. World J Emerg Med. 2016;7:285-289. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 17. | Jin Y, Ying J, Zhang K, Fang X. Endotracheal intubation under video laryngoscopic guidance during upper gastrointestinal endoscopic surgery in the left lateral position: A randomized controlled trial. Medicine (Baltimore). 2017;96:e9461. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 18. | Li H, Wang W, Lu YP, Wang Y, Chen LH, Lei LP, Fang XM. Evaluation of Endotracheal Intubation with a Flexible Fiberoptic Bronchoscope in Lateral Patient Positioning: A Prospective Randomized Controlled Trial. Chin Med J (Engl). 2016;129:2045-2049. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 19. | Goh SY, Thong SY, Chen Y, Kong AS. Efficacy of intubation performed by trainees on patients in the lateral position. Singapore Med J. 2016;57:503-506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 20. | Nielsen TS, Charles AV. Lethal esophageal rupture following treatment with Sengstaken-Blakemore tube in management of variceal bleeding: a 10-year autopsy study. Forensic Sci Int. 2012;222:e19-e22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 21. | Lin CT, Huang TW, Lee SC, Kuo SM, Hsu KF, Hsu PS, Huang HK, Chang H. Sengstaken-Blakemore tube related esophageal rupture. Rev Esp Enferm Dig. 2010;102:395-396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 22. | Escorsell À, Pavel O, Cárdenas A, Morillas R, Llop E, Villanueva C, Garcia-Pagán JC, Bosch J; Variceal Bleeding Study Group. Esophageal balloon tamponade vs esophageal stent in controlling acute refractory variceal bleeding: A multicenter randomized, controlled trial. Hepatology. 2016;63:1957-1967. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 125] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 23. | Al-Khazraji A, Curry MP. The current knowledge about the therapeutic use of endoscopic sclerotherapy and endoscopic tissue adhesives in variceal bleeding. Expert Rev Gastroenterol Hepatol. 2019;13:893-897. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 24. | Villanueva C, Piqueras M, Aracil C, Gómez C, López-Balaguer JM, Gonzalez B, Gallego A, Torras X, Soriano G, Sáinz S, Benito S, Balanzó J. A randomized controlled trial comparing ligation and sclerotherapy as emergency endoscopic treatment added to somatostatin in acute variceal bleeding. J Hepatol. 2006;45:560-567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 137] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 25. | Alvarez-Sánchez MV, Jenssen C, Faiss S, Napoléon B. Interventional endoscopic ultrasonography: an overview of safety and complications. Surg Endosc. 2014;28:712-734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 54] [Article Influence: 4.5] [Reference Citation Analysis (0)] |