Published online Jun 6, 2021. doi: 10.12998/wjcc.v9.i16.4046
Peer-review started: January 14, 2021
First decision: February 11, 2021
Revised: February 24, 2021
Accepted: March 24, 2021
Article in press: March 24, 2021
Published online: June 6, 2021
Processing time: 120 Days and 5.4 Hours
Previous studies reported that most of the intracranial dermoid cyst ruptures were spontaneous, and only a few were traumatic, with asymptomatic much rarer than the symptomatic ruptures. Hence, how to deal with the asymptomatic traumatic rupture of intracranial dermoid cyst remains a challenge in the clinic.
A 59-year-old man was accidentally diagnosed with intracranial dermoid cyst through a cranial computed tomography (CT) scan due to a car accident. A mixed-density lesion with fat and a calcified margin was observed in the midline of the posterior fossa, accompanied with lipid droplet drifts in brain sulci, fissures, cisterns, and ventricles. After 1 wk of conservative observation, no change was observed on the updated cranial CT scan. After 2 wk of conservative observation, magnetic resonance imaging examination confirmed that the lesion was a traumatic rupture of a posterior fossa dermoid cyst with lipid droplet drifts. As the patient exhibited no adverse symptoms throughout the 2 wk, a 6-mo follow-up visit was arranged for him instead of aggressive treatment. Nonethe
Asymptomatic traumatic rupture of intracranial dermoid cyst could be just followed or treated conservatively rather than treated aggressively.
Core Tip: A case of traumatic intracranial dermoid cyst rupture in a 59-year-old man was analyzed retrospectively. Imaging findings, clinical manifestations, treatment, and follow-up results for 6 mo were collected. Combined with the relevant literature, the cause and treatment of asymptomatic cyst rupture were analyzed. For a traumatic intracranial dermoid cyst rupture, if the lesion is small, affects the adjacent structures only slightly, and has few lipid droplet drifts, conservative treatment or only follow-up visits could be adopted according to the patient’s neurological examination results.
- Citation: Zhang MH, Feng Q, Zhu HL, Lu H, Ding ZX, Feng B. Asymptomatic traumatic rupture of an intracranial dermoid cyst: A case report. World J Clin Cases 2021; 9(16): 4046-4051
- URL: https://www.wjgnet.com/2307-8960/full/v9/i16/4046.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i16.4046
Intracranial dermoid cyst is a rare embryonal benign cystic mass and accounts for 0.04%-0.6% of intracranial tumors[1,2]. Previous studies reported that most of the intracranial dermoid cyst ruptures were spontaneous[2-5], and only a few were traumatic[1,6], with asymptomatic much rarer than the symptomatic ruptures. The current study aimed to comprehensively analyze the imaging characteristics of traumatic dermoid cyst rupture based on the existing case and literature, thereafter the intervention was determined based on the imaging characteristics and clinical symptoms.
A 59-year-old man was admitted to the hospital due to a car accident.
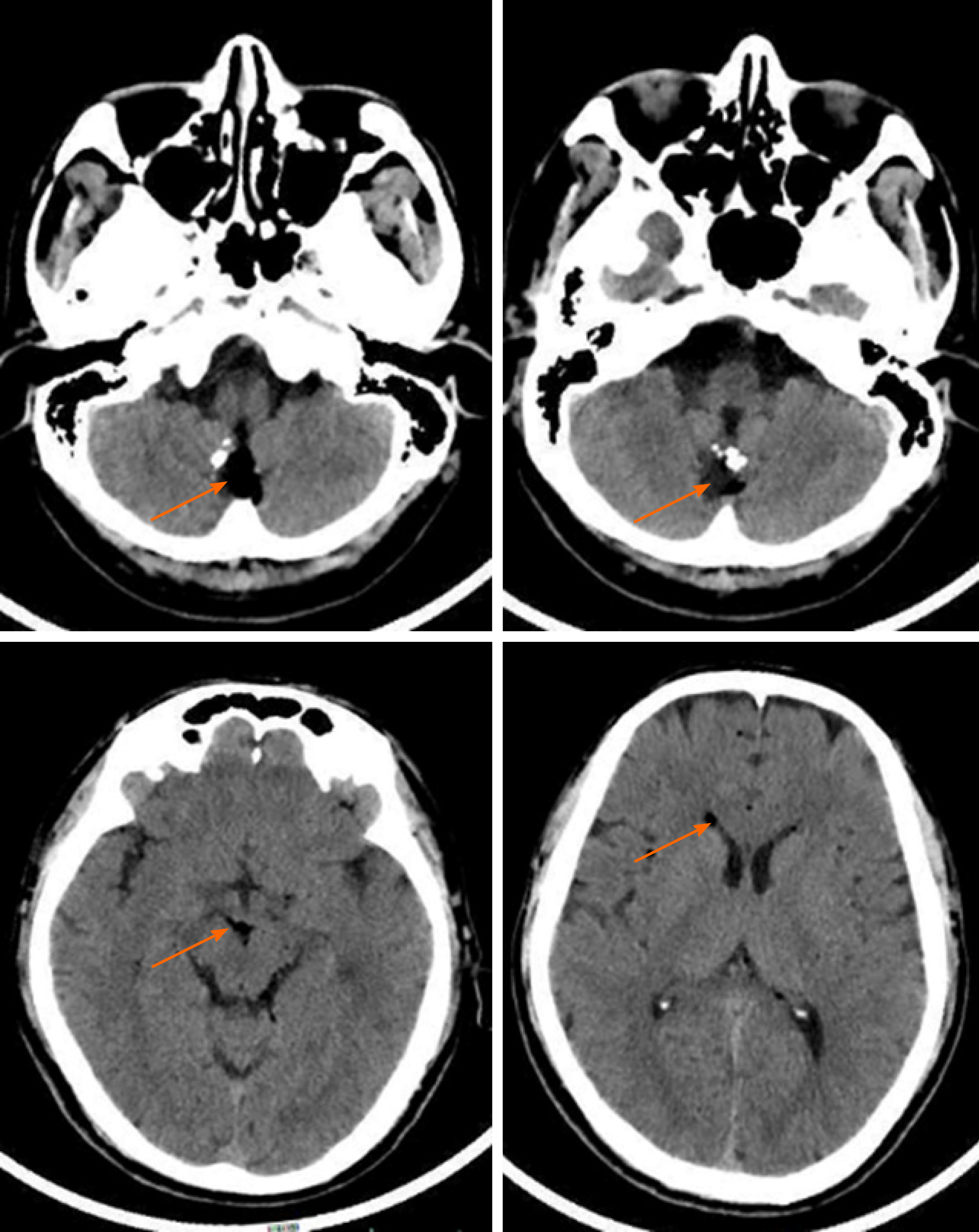
A cranial computed tomography (CT) scan revealed a mixed-density lesion near the midline of the posterior fossa (anterior and superior to the occipital protuberance), accompanied by a calcified margin.
No other traumatic lesions, such as intracranial hemorrhage and skull fracture, were observed (Figure 1). As the patient had no obvious neurological symptoms, he was discharged and sent home for recuperation.
The CT value in the low-density lesion area was about 14 Hounsfield Units (HU) and that in the fat-density area was -60 to -40 HU; the size of the lesion was 14.6 mm × 21.1 mm without a space-occupying effect. In addition, low-density spotted shadows were observed in the ambient cistern, interpeduncular cistern, longitudinal fissure cistern, juxta-right cavernous sinus, lateral ventricles, and sulus; the CT value was about -60 to -40 HU, and the maximum length of the lipid droplets was 5 mm.
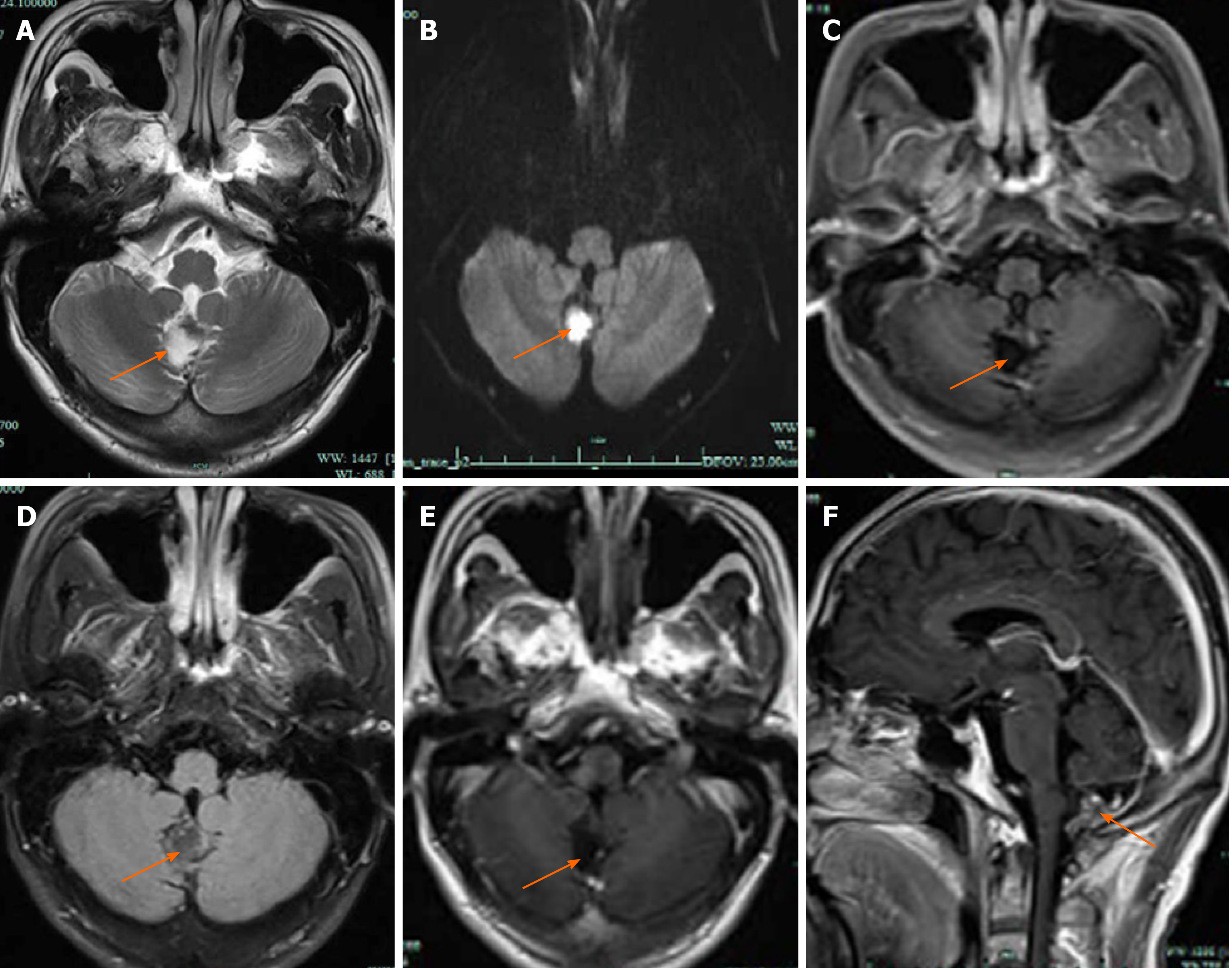
On the updated cranial CT scan after 1 wk, no changes were detected in the lesion or the distribution or the size of the lipid droplets as compared to that at the first admission. After 2 wk of conservative observation, the patient underwent cranial magnetic resonance imaging (MRI) examination, in which the lesion was located below the cerebellar vermis, with the anterior part extending into the fourth ventricle. As a result, hyperintensity was detected on T2 weighted image, hypointensity on T1-fluid attenuated inversion recovery (FLAIR), iso-hypointensity on T2-FLAIR, and hyperintensity on diffusion weighted image (b = 1000 s/mm2). A T1-FLAIR contrast-enhanced scan did not show any abnormal enhancement in the cystic lesion area or other brain tissues or meninges, and that the fat area presented a slightly hyperintensity and was connected to the subarachnoid space (Figure 2). Interestingly, no abnormal signal was observed in other brain tissue sequences.
According to the CT and MRI findings, the patient was finally diagnosed with traumatic rupture of a posterior fossa dermoid cyst with lipid droplet drifts.
As the patient had no obvious neurological symptoms, he was discharged and sent home for recuperation. As no positive imaging findings or abnormal neurological symptoms were found after 2 wk of conservative observation, a 6-month follow-up visit was arranged for the patient instead of aggressive treatment.
After 1 mo, the patient underwent a neurological examination, which showed no positive findings, no nausea, vomiting, headache, or epilepsy, no abnormal changes in mental state, and normal vital signs and laboratory test results. The patient was proclaimed well in the follow-up visits for up to 6 mo.
Dermoid cysts are epithelial cells remaining in the neural crest ectoderm during 3-5 wk of embryonic development that are wrapped with the closure of neural tubes. Eventually, the cysts are formed that are primarily located in the sellar region, juxtasellar region, juxta-cavernous sinus, lateral fissures, brainstem, posterior cranial fossa, juxta-fourth ventricle, anterior cranial fossa bottom, and spinal canal[7-9], and larger cysts grow across the cranial fossa[10]. With the advancing age, hormonal changes lead to increased secretion of glans, resulting in the rapid growth of tumors and spontaneous ruptures. When a patient is in his/her adulthood, the hormone level stabilizes. The dermoid cyst is less affected by the hormone and stops growing. In this case, the patient was 59 years old, and had no neurological symptoms before head trauma, suggesting that the lesion was stable. The reason for the dermoid cyst rupture after trauma might be damaged cyst wall and lipid spill caused by the mechanical stress of the internal occipital protuberance on the lesion due to external force to the posterior fossa.
There are two main reasons for the clinical symptoms caused by dermoid cyst rupture. One is the effect of the lesion on the surrounding structure, and the other is aseptic meningitis, vasospasm, and nerve injury caused by the stimulation of the split contents on local meninges, blood vessels, and nerves[10,11]. In this case, no obvious neurological symptoms were observed in the patient before and at the time of injury and during the 6 mo of follow-up visits, which might be related to the location of the lesion below the cerebellar vermis, with no adjacent major nerve or blood vessel. Also, the lesion was small and hence did not exert any obvious compression on the surrounding structure and produced a few split contents after rupture.
In this case, the dermoid cyst extended into the fourth ventricle in the front and connected to the subarachnoid space in the lower part, such that the rupture resulted in extensive drifts of lipid droplets. Although widely distributed, the lipid droplets were small in size, with a maximum length of 5 mm, affecting the local structure slightly and not causing any obvious symptoms. The lipid droplets are difficult to move once they enter the subarachnoid space. However, their extension showed neither absorption of such drifted lipid droplets nor further spread or displacement. The patient did not develop any new neurological symptoms or other adverse clinical consequences[12]. Thus, no special treatment was required for these small lipid droplets according to the study results of the case and literature.
Intracranial dermoid cyst rupture has typical imaging characteristics. In this case, a mixed-density shadow was detected below the cerebellar vermis on CT scan. Furthermore, MRI confirmed the nature and characteristics of the lesion, such as the lipid signal, absence of enhancement area, and limited dispersion, which further affirmed our diagnosis. MRI is superior to CT in determining the correlation between a tumor and the adjacent neurovascular structures, as it excludes the possibility of cerebral infarction, cerebral contusion, and aseptic meningitis, providing a direction for further treatment. Some traumatic or spontaneous dermoid cyst ruptures were treated conservatively with glucocorticoid drugs, which were sufficiently effica
Traumatic intracranial dermoid cyst rupture without neurological symptoms is rare and can be accurately assessed by detailed imaging examinations. For a traumatic intracranial dermoid cyst rupture, if the lesion is small, affects the adjacent structures only slightly, and has few lipid droplet drifts, conservative observation or follow-up visits could be adopted according to the patient’s neurological examination results.
Manuscript source: Unsolicited manuscript
Specialty type: Radiology, nuclear medicine and medical imaging
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ak R, Oura S, Park SB S-Editor: Gong ZM L-Editor: Wang TQ P-Editor: Li JH
| 1. | Esquenazi Y, Kerr K, Bhattacharjee MB, Tandon N. Traumatic rupture of an intracranial dermoid cyst: Case report and literature review. Surg Neurol Int. 2013;4:80. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 2. | Balasundaram P, Garg A, Prabhakar A, Joseph Devarajan LS, Gaikwad SB, Khanna G. Evolution of epidermoid cyst into dermoid cyst: Embryological explanation and radiological-pathological correlation. Neuroradiol J. 2019;32:92-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 33] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 3. | Asil K, Gunduz Y, Ayhan LT, Aksoy YE, Yildiz C. Spontaneous rupture of intracranial dermoid tumor in a patient with vertigo. Computed tomography and magnetic resonance imaging findings. Pol J Radiol. 2013;78:79-82. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Ak R, Doğanay F, Doğan M. Rare cause of seizures: ruptured intracranial dermoid cyst. Clin Exp Emerg Med. 2019;6:89-90. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Yamagami K, Kakuta N, Seki K, Nakamura R, Hanioka Y, Nakamura T, Goto H. Acute Urinary Retention Induced by Chemical Meningitis Which Occurred Due to a Ruptured Dermoid Cyst. Intern Med. 2018;57:729-731. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Ramlakhan R, Candy S. Traumatic rupture of an intracranial dermoid cyst. Radiol Case Rep. 2015;10:1053. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Jamesh R, Indiran V, Maduraimuthu P. Ruptured Intracranial Dermoid Cyst in Temporal Fossa. Acta Neurol Taiwan. 2016;25:70-72. [PubMed] |
| 8. | Muçaj S, Ugurel MS, Dedushi K, Ramadani N, Jerliu N. Role of MRI in Diagnosis of Ruptured Intracranial Dermoid Cyst. Acta Inform Med. 2017;25:141-144. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 9. | Prasad GL, Sinha S, Krishna G. Rupture of spinal dermoid cyst with intracranial dissemination: Report of a case and review of the literature. Neurol India. 2018;66:1195-1199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Paik SC, Kim CH, Cheong JH, Kim JM. A Ruptured Dermoid Cyst of the Cavernous Sinus Extending into the Posterior Fossa. J Korean Neurosurg Soc. 2015;57:364-366. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Wani AA, Raswan US, Malik NK, Ramzan AU. Posterior fossa ruptured dermoid cyst presenting with hydrocephalus. Neurosciences (Riyadh). 2016;21:358-360. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 12. | Liu JK, Gottfried ON, Salzman KL, Schmidt RH, Couldwell WT. Ruptured intracranial dermoid cysts: clinical, radiographic, and surgical features. Neurosurgery. 2008;62:377-384; discussion 384. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 82] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 13. | Kosuge Y, Onodera H, Sase T, Uchida M, Takasuna H, Ito H, Oshio K, Tanaka Y. Ruptured dermoid cyst of the lateral cavernous sinus wall with temporary symptoms: a case report. J Med Case Rep. 2016;10:224. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |