Published online Jun 6, 2021. doi: 10.12998/wjcc.v9.i16.4024
Peer-review started: January 12, 2021
First decision: February 11, 2021
Revised: February 19, 2021
Accepted: March 13, 2021
Article in press: March 13, 2021
Published online: June 6, 2021
Processing time: 122 Days and 2.4 Hours
Endoscopic thyroidectomy has obvious advantages over conventional surgical techniques in terms of postoperative cosmetic outcome. Although the incidence of carbon dioxide embolism (CDE) during endoscopic thyroidectomy is very low, it is potentially fatal. The clinical manifestations of CDE vary, and more attention should be paid to this disorder.
A 27-year-old man was scheduled for thyroidectomy by the transoral vestibular approach. The patient had no other diseases or surgical history. During the operation, he developed a CDE following inadvertent injury of the anterior jugular vein. The clinical manifestation in this patient was a transient sharp rise in end-tidal carbon dioxide, and his remaining vital signs were stable. In addition, loud coarse systolic and diastolic murmurs were heard over the precordium. The patient was discharged on day 4 after surgery without complications.
A transient sharp rise in end-tidal carbon dioxide is considered a helpful early sign of CDE during endoscopic thyroidectomy.
Core Tip: Carbon dioxide embolism can occur during endoscopic thyroidectomy and is potentially fatal. The clinical manifestations of carbon dioxide embolism vary. Thus, anesthesiologists should pay more attention when diagnosing and managing such patients.
- Citation: Tang JX, Wang L, Nian WQ, Tang WY, Xiao JY, Tang XX, Liu HL. Asymptomatic carbon dioxide embolism during transoral vestibular thyroidectomy: A case report. World J Clin Cases 2021; 9(16): 4024-4031
- URL: https://www.wjgnet.com/2307-8960/full/v9/i16/4024.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i16.4024
Endoscopic thyroid surgery, also called remote-access thyroidectomy, has obvious advantages over conventional surgical techniques in terms of postoperative cosmetic outcome[1]. Endoscopic thyroidectomy was first reported in 1997. It has gradually become popular worldwide and consists of the transoral, postauricular, anterior chest, breast and transaxillary approaches[2]. Thyroidectomy by the transoral approach results in no surgical incision scars, less surgical trauma, a broader surgical view of the thyroid gland and a shorter learning curve for surgeons; thus, it is considered to be the ultimate surgical procedure for endoscopic thyroidectomy[3,4].
Endoscopic thyroidectomy can be divided into gasless endoscopic thyroidectomy and carbon dioxide (CO2) inflatable endoscopic thyroidectomy[5]. CO2 insufflation improves surgical field exposure but has the potential risk of subcutaneous emphysema, hypercapnia, cerebral edema and carbon dioxide embolism (CDE)[6,7]. We recently encountered a case of CDE during transoral vestibular thyroidectomy. To our knowledge, this is the first report of CDE that manifested as a sudden and dramatic increase in end-tidal carbon dioxide (ETCO2) during endoscopic thyroidectomy.
A 27-year-old man was admitted to our hospital with a thyroid tumor of the middle and lower poles of the right thyroid, which was found 1 wk previously.
The patient was admitted to the hospital for routine physical examination 1 wk ago. Through thyroid color Doppler ultrasound, a thyroid tumor in the middle and lower poles of the right thyroid was found. The patient denied any symptoms such as dyspnea, fear of heat and lethargy.
The patient had no other diseases or surgical history.
The patient did not smoke or drink and denied a family history of genetic disease.
The patient’s trachea was in the center, breath sounds in both lungs were clear and symmetrical, and there was no murmur on heart auscultation.
The results of preoperative blood examinations, blood biochemistry tests, coagulation function tests, thyroid function tests, urinalysis and stool analysis were normal.
Preoperative color Doppler ultrasound of the thyroid revealed a 1.9 cm × 2.6 cm nodule in the middle and lower poles of the right thyroid. The results of preoperative chest roentgenogram, electrocardiography and echocardiography were normal.
On admission to the operating room, the patient’s heart rate, blood pressure, oxygen saturation and electrocardiography were monitored. Propofol, vecuronium and sufentanil were administered intravenously for induction of general anesthesia and sevoflurane, propofol and remifentanil for maintenance anesthesia. ETCO2 and body temperature were continuously monitored throughout general anesthesia.
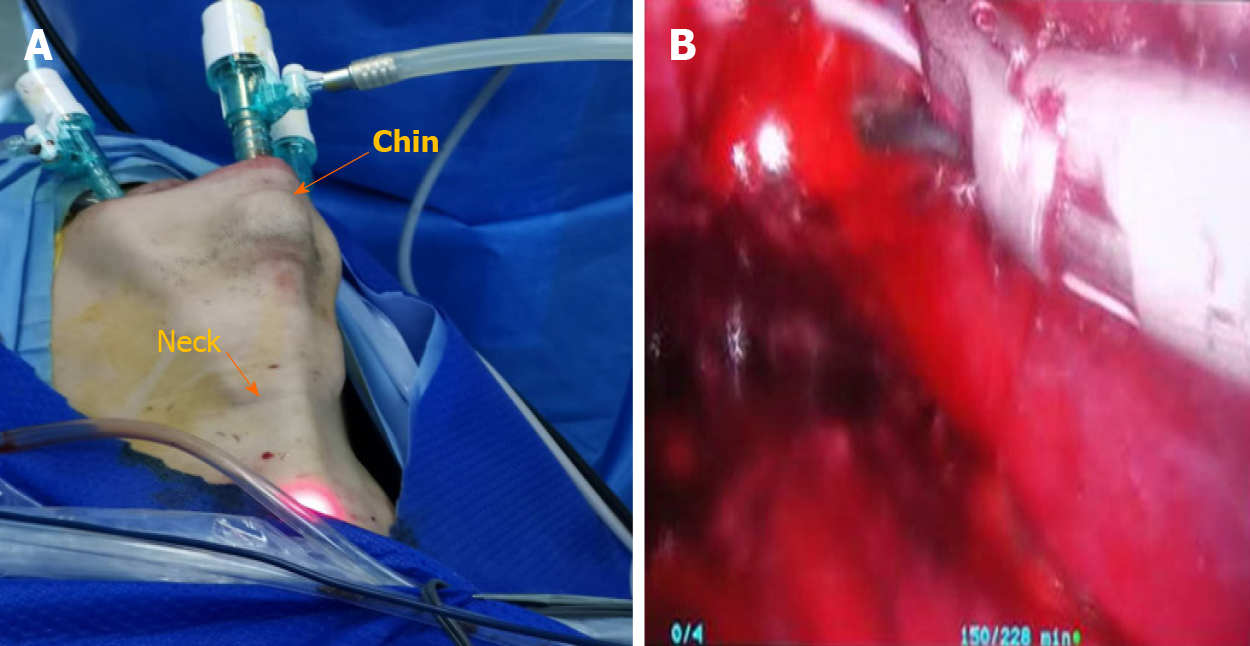
The patient was placed in the supine position, and the neck was extended with a shoulder pillow. In brief, after sterilization and draping, one 1.2-cm horizontal incision was made from 5 mm anterior the lower oral frenulum, and another two 5-mm horizontal incisions were made on either side of the first incision. Then 20 mL of 0.9% saline solution, containing 0.375% ropivacaine and epinephrine (1:40000), was injected subcutaneously into the submental and anterior neck area. A blunt-tipped 12 mm trocar was inserted into the space for insertion of a 10 mm 30-degree rigid endoscope (KARL STORZ-ENDOSKOPE, STORZ, Indonesia). The pressure of CO2 insufflation was 6 mmHg, and then two 5 mm trocars were inserted into the oral vestibule on both sides of the endoscope. Under endoscopy, grasping forceps and an ultrasonic knife were used to dissect the skin flap in the plane of the subplatysmal layer. The flap ranged from the level of the sternal notch and the anterior border of the sternocleido
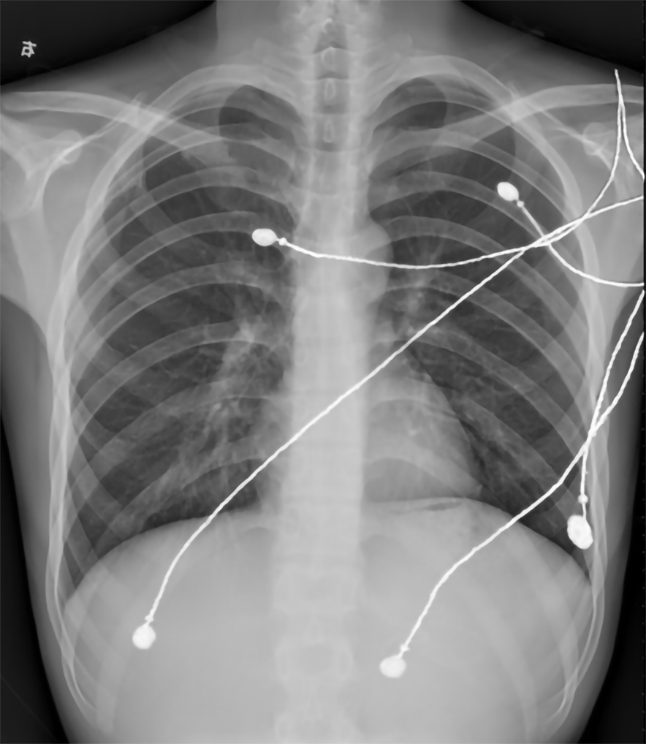
During dissection of the anterior cervical area, the anterior jugular vein was inadvertently injured, and obvious bleeding in the surgical area was observed. The ultrasonic scalpel was used to staunch the bleeding (Figure 1). At this time, the patient’s ETCO2 had increased from 46 mmHg to 68 mmHg and continued to reach a maximum of 84 mmHg 1 min later (Table 1). His heart rate, blood pressure, oxygen saturation, heart rhythm and airway pressure were similar throughout the procedure. A CDE was initially considered, and CO2 insufflation was immediately ceased, the sevoflurane vaporizer was turned off, and the patient was placed in the Steep-head down, left-lateral decubitus (Durant’s) position. Loud coarse systolic and diastolic murmurs were heard over the precordium using a stethoscope, and breath sounds were normal on both sides. The patient’s ETCO2 began to drop to 82 mmHg at the third min, then gradually decreased to the preoperative baseline level of 40 mmHg within approximately 10 min. Surgery was continued using a gasless facelift approach. After the operation, the patient was transferred to the post anesthesia care unit. Bedside chest roentgenogram was immediately performed in the post anesthesia care unit and showed no abnormalities (Figure 2).
| Parameter | 12:51 | 12:52 | 12:53 | 12:54 | 12:55 | 12:56 | 12:57 | 12:58 | 12:59 | 13:00 | 13:01 |
| End-tidal CO2 in mmHg | 46 | 68 | 84 | 82 | 78 | 73 | 65 | 60 | 55 | 50 | 47 |
| Noninvasive systolic blood pressure in mmHg | (-) | 99 | (-) | (-) | 101 | (-) | (-) | 103 | (-) | (-) | 101 |
| Noninvasive diastolic blood pressure in mmHg | (-) | 57 | (-) | (-) | 53 | (-) | (-) | 51 | (-) | (-) | 57 |
| Heart rate in bpm | 68 | 67 | 66 | 66 | 64 | 63 | 64 | 65 | 64 | 64 | 65 |
| Blood oxygen saturation, % | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 |
To further examine the characteristics of CDE, such as the clinical manifestations, diagnosis, treatment and prognosis, in endoscopic thyroidectomy, we identified similar cases reported in the past decade. We first performed an electronic search of several databases including PubMed, Cochrane Library, EMBASE and Web of Science from January 2010 to November 2020. The search words included “embolism,” “hypercapnia,” “end-tidal carbon dioxide” and “thyroidectomy” and were adopted for all search strings according to the unique characteristics of each database. After the electronic search, we confirmed the included studies using the following entry criteria: the types of the published articles were case reports, prospective studies or retrospective studies, and the papers that reported hypercapnia or CDE occurring after CO2 insufflation during endoscopic thyroidectomy were included. Meta-analyses and non-English language studies were excluded.
Finally, 5 cases in four articles were obtained[7-10]. Data on age, weight, tumor size, surgical approach, insufflation pressure, intraoperative anesthesia, embolization time, possible causes, clinical manifestations, diagnostic tools, treatment and prognosis were extracted and are shown in Table 2. Surgical approaches included the bilateral axilla and nipple areola approach, transoral robotic approach, axillo-bilateral-breast approach and the transoral approach. Insufflation pressure was set to 20 mmHg in one study, 8 mmHg in one study and 6 mmHg in two studies. Gas embolism developed in 2 cases when CO2 was insufflated, and the other cases developed CDE during the process of tissue dissection. Only one report suggested a possible anterior jugular vein tear, and the other three reports did not specify the cause.
| Characteristic | Rajan et al[8], 2016 | Kim et al[7], 2018 | Kim et al[9], 2010 | Fu et al[10], 20181 |
| Age in yr | 48 | 59 | 59 | UN |
| Weight in kg | 68 | 57 | 54 | UN |
| Size of thyroid nodules in cm | 4.0 × 5.0 | 1.1 × 0.8 × 1.0 | UN | UN |
| Surgical approach | Bilateral axilla and nipple areola | Transoral robotic | Axillo-bilateral-breast approach | Transoral |
| Insufflation pressure in mmHg | 20 | 6 | 6 | 8 |
| Maintenance of anesthesia | UN | O2–air-sevoflurane | O2–air-sevoflurane | UN |
| Time of event | 3 h after operation | During skin flap elevation | Beginning of CO2 insufflation | Beginning of CO2 insufflation |
| Possible causes | UN | Anterior jugular vein was lacerated | UN | UN |
| Clinical manifestations | ETCO2↓, SPO2↓, hypotension, bradycardia | ETCO2↓, SPO2↓, hypotension, bradycardia, premature atrial complexes, asystole | ETCO2↓, SPO2↓, hypotension, tall peaked T-wave | SPO2↓, hypotension, tachycardia, asystole |
| Diagnosis tools | ETCO2 | ETCO2 | ETCO2, TEE | Precardial Doppler sonography |
| Treatment | Reduced insufflation pressure, Trendelenburg position, glycopyrrolate 0.2 mg, ephedrine 6 mg, 100% O2 hyperventilation, aggressive intravenous volume expansion, 6 cmH2O PEEP | Stopped CO2 gas insufflation, Durant’s position, ephedrine 10 mg, atropine 0.5 mg, 100% O2 hyperventilation, chest compression, epinephrine 1 mg | Stopped CO2 gas insufflation, Durant’s position, 100% O2 hyperventilation, ephedrine 5 mg | Stopped CO2 gas insufflation, Left lateral decubitus, dexamethasone, aminophylline, dopamine, high flow O2, chest compression |
| Prognosis | Good | Good | Good | Good |
The clinical manifestations after embolism mainly included a sudden and severe drop in ETCO2, a drop in oxygen saturation, hypotension, sinus bradycardia, sinus tachycardia, atrial premature contraction and paradoxical embolism. Three cases developed cardiac arrest. Three reports mentioned ETCO2, one of which used transesophageal echocardiography (TEE) combined with ETCO2, and another reported the use of transthoracic Doppler ultrasound for diagnosis. The treatment methods for CDE included discontinuation of insufflation, adjustment of the patient’s position to Durant’s position, 100% oxygen hyperventilation, the administration of vasopressors and inotropic agents, aggressive volume expansion, positive end-expiratory pressure for ventilation and cardiopulmonary resuscitation for cardiac arrest.
From the prospective study of a small sample of 81 patients by Fu et al[10], 2 patients were identified as having CDE[10]. We calculated that the incidence of CDE in transoral endoscopic thyroidectomy was approximately 2.4%. The prognosis of these 5 patients was good. However, we believe that a long term, high-volume, prospective study is required to accurately quantify the incidence of CDE in endoscopic thyroidectomy (using reference standard monitoring) and its consequences.
We found that CDE during endoscopic thyroidectomy is rare, and it can develop at any time during surgery. Although CDE may occur under various insufflation pressures, low pressures below 6 mmHg are generally recommended[11]. If necessary, gasless endoscopic thyroidectomy can be considered as an alternative, which can significantly reduce or even avoid the occurrence of CDE[12-14].
Carbon dioxide embolism
We immediately ceased CO2 insufflation, turned off the sevoflurane vaporizer and placed the patient in the Durant’s position.
The patient was extubated 30 min after surgery and discharged on day 4 after surgery without complications related to CDE.
Endoscopic surgical techniques, including those that involve insufflation of the tissues with carbon dioxide, are gaining wider acceptance and use worldwide. These advances have introduced the possibility of carbon dioxide embolus (including life-threatening embolus). Such factors introduce challenges in preventing, diagnosing and treating carbon dioxide embolus and determining how the risk of embolus affects the risk-to-benefit profile of any new surgical procedure. These issues have recently been reviewed by Lanier et al[15], as related to colorectal surgery[15]. We will discuss some of these same issues as they apply to endoscopic thyroid surgery.
CDE can occur during various laparoscopic surgeries. CO2 can directly enter veins through the pneumoperitoneum needle, which can be placed into veins or solid organs in error[16]. CO2 may also enter the right heart system through an opening in damaged vessels during surgery[7]. Due to the lack of a preexisting cavity in the neck, during endoscopic thyroid surgery a tunnel under the skin is necessary to establish a working space for the operation. During this process, blood vessels may be injured. This may be one of the causes of CDE in endoscopic thyroid surgery. The clinical manifestations of CDE range from asymptomatic to neurological impairment, cardiovascular system collapse and even death, depending on the capacity and absorption rate of CO2[17]. The volume and rate of gas entering the vein are positively related to the size of the damaged vascular cavity and the gas-blood pressure gradient[18].
At present, the most sensitive and specific method for diagnosing CDE is TEE, which can detect CO2 at 0.1 mL/kg[19]; however, TEE is limited due to its high cost, high invasiveness and complicated technique. ETCO2 is a sensitive and noninvasive method for diagnosing CDE, and sudden or dramatic changes in ETCO2 values, including rapid rise or fall in ETCO2, can help diagnose CDE[20-22]. Animal experiments have shown that a decline in ETCO2 was only seen in air embolism and a large CDE, and in continuous low-dose CDE, ETCO2 did not change significantly[23]. A possible mechanism for this is that a large amount of CO2 blocks the right ventricular outflow tract and pulmonary artery, which increases the ventilation dead space and leads to a decrease in ETCO2[17]. Deformable emboli smaller than 14-22 μm will be filtered in pulmonary capillaries with a diameter of 3-15 μm[24]. Therefore, if the total volume of the CO2 emboli is not too large and the speed of entering the right atrium is not too fast, most of the emboli will be filtered by the lungs without the “gas-lock” effect. In addition, the high solubility of CO2 in the blood and high dispersibility to the lungs increase the excretion of CO2 through the lungs, thus leading to the increase of ETCO2[17].
The diagnostic sensitivity of CDE by auscultation of “mill-wheel” murmurs through a precardiac or transesophageal stethoscope is low[17]. However, auscultation is simple, noninvasive, inexpensive and may identify abnormalities earlier than other indicators[25]. Even in the absence of clinical signs, typical murmurs of air embolism can also occur, which is a good method for the diagnosis of CDE[22]. In our patient, there were no obvious reasons for simultaneous appearance of a cardiac murmur and transient elevation of ETCO2, other than CDE. Our patient was in good health. The preoperative cardiac examination and thyroid function examination were normal. In addition to the heart murmur and transient and severe ETCO2 rise during the operation, the vital signs including body temperature were normal, the breath sounds of both lungs were normal on auscultation, and the airway pressure was normal during the operation. We did not touch the subcutaneous emphysema. The chest roentgenogram immediately after the operation also showed no abnormalities. (Figure 2). Therefore, we strongly considered the diagnosis of CDE in our patient.
For the treatment of carbon dioxide embolism, we emphasize early diagnosis and timely and correct treatment. Routine monitoring of ETCO2 and auscultation of abnormal heart sounds in the precordial area can detect an early diagnosis of CDE. If necessary, TEE can be used to obtain direct evidence of CDE. Once CDE is suspected, CO2 insufflation should be discontinued immediately. Hyperventilation with 100% oxygen is important to wash out CO2 and improve hypoxemia[17]. To facilitate gas bubbles to rise to the top of the right atrium and reduce the "gas-lock" effect, the patient should adopt the Durant’s position[26]. If the patient has a central venous catheter, the gas can be aspirated from the central venous catheter[26].
The most important cause of life-threatening CDE is that CO2 emboli block the right ventricular outflow channel, causing pulmonary hypertension and eventually right heart failure followed by left ventricular failure due to insufficient left ventricular filling. The application of vasopressor drugs and inotropic drugs to maintain heart rate and cardiac output is very important for maintaining hemodynamic stability and maintaining the oxygenation of vital organs[17]. Chest compression itself is thought to force air out of the pulmonary outflow tract. To improve forward blood flow, cardiopulmonary resuscitation should be initiated if the patient suffers a cardiac arrest[18]. If a patient remains unstable, cardiopulmonary bypass or internal cardiac massage can be considered[27,28].
CDE during endoscopic thyroidectomy is rare, and it can develop at any time and under various insufflation pressures during surgery. The clinical manifestations of CDE vary, and more attention should be paid to this disorder. Based on current evidence, we recommend low insufflation pressures below 6 mmHg should be used. If necessary, then gasless endoscopic thyroidectomy can be considered as an alternative. The comprehensive use of multiple diagnostic tools, such as ETCO2, precordial auscultation and TEE, etc. should be performed to diagnose CDE to conduct timely intervention and treatment.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: William LL S-Editor: Zhang L L-Editor: Filipodia P-Editor: Ma YJ
| 1. | Lee DW, Ko SH, Song CM, Ji YB, Kim JK, Tae K. Comparison of postoperative cosmesis in transaxillary, postauricular facelift, and conventional transcervical thyroidectomy. Surg Endosc. 2020;34:3388-3397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 31] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 2. | Tae K, Ji YB, Song CM, Ryu J. Robotic and Endoscopic Thyroid Surgery: Evolution and Advances. Clin Exp Otorhinolaryngol. 2019;12:1-11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 74] [Cited by in RCA: 144] [Article Influence: 20.6] [Reference Citation Analysis (0)] |
| 3. | Tae K. Transoral Thyroidectomy: Is It a Real Game Changer? Clin Exp Otorhinolaryngol. 2020;13:93-94. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 4. | Razavi CR, Vasiliou E, Tufano RP, Russell JO. Learning Curve for Transoral Endoscopic Thyroid Lobectomy. Otolaryngol Head Neck Surg. 2018;159:625-629. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 83] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 5. | Muenscher A, Dalchow C, Kutta H, Knecht R. The endoscopic approach to the neck: a review of the literature, and overview of the various techniques. Surg Endosc. 2011;25:1358-1363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 44] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 6. | Kwek JWM, Pang MJ, Heah HHW. Pneumoperitoneum after transoral endoscopic thyroidectomy vestibular approach. Laryngoscope Investig Otolaryngol. 2020;5:580-583. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 7. | Kim KN, Lee DW, Kim JY, Han KH, Tae K. Carbon dioxide embolism during transoral robotic thyroidectomy: A case report. Head Neck. 2018;40:E25-E28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 51] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 8. | Rajan S, Paul J, Kumar L. Carbon dioxide embolism during endoscopic thyroidectomy. Indian J Anaesth. 2016;60:65-66. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Kim SH, Park KS, Shin HY, Yi JH, Kim DK. Paradoxical carbon dioxide embolism during endoscopic thyroidectomy confirmed by transesophageal echocardiography. J Anesth. 2010;24:774-777. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Fu J, Luo Y, Chen Q, Lin F, Hong X, Kuang P, Yan W, Wu G, Zhang Y. Transoral Endoscopic Thyroidectomy: Review of 81 Cases in a Single Institute. J Laparoendosc Adv Surg Tech A. 2018;28:286-291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 48] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 11. | Tae K, Ji YB, Song CM, Park JS, Park JH, Kim DS. Safety and efficacy of transoral robotic and endoscopic thyroidectomy: The first 100 cases. Head Neck. 2020;42:321-329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 49] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 12. | Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359-E386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20108] [Cited by in RCA: 20516] [Article Influence: 2051.6] [Reference Citation Analysis (20)] |
| 13. | Kim EY, Lee KH, Park YL, Park CH, Lee CR, Jeong JJ, Nam KH, Chung WY, Yun JS. Single-Incision, Gasless, Endoscopic Trans-Axillary Total Thyroidectomy: A Feasible and Oncologic Safe Surgery in Patients with Papillary Thyroid Carcinoma. J Laparoendosc Adv Surg Tech A. 2017;27:1158-1164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 34] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 14. | Song CM, Cho YH, Ji YB, Jeong JH, Kim DS, Tae K. Comparison of a gasless unilateral axillo-breast and axillary approach in robotic thyroidectomy. Surg Endosc. 2013;27:3769-3775. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 31] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 15. | Lanier WL, Warner MA. Assessing Acceptable Risk in New Surgical Procedures, With Special Reference to Gas Emboli in Transanal Total Mesorectal Surgery. Dis Colon Rectum. 2019;62:777-780. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 16. | Smith HJ. Carbon dioxide embolism during pneumoperitoneum for laparoscopic surgery: a case report. AANA J. 2011;79:371-373. [PubMed] |
| 17. | Park EY, Kwon JY, Kim KJ. Carbon dioxide embolism during laparoscopic surgery. Yonsei Med J. 2012;53:459-466. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 86] [Cited by in RCA: 85] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 18. | Mirski MA, Lele AV, Fitzsimmons L, Toung TJ. Diagnosis and treatment of vascular air embolism. Anesthesiology. 2007;106:164-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 400] [Cited by in RCA: 376] [Article Influence: 20.9] [Reference Citation Analysis (0)] |
| 19. | Couture P, Boudreault D, Derouin M, Allard M, Lepage Y, Girard D, Blaise G. Venous carbon dioxide embolism in pigs: an evaluation of end-tidal carbon dioxide, transesophageal echocardiography, pulmonary artery pressure, and precordial auscultation as monitoring modalities. Anesth Analg. 1994;79:867-873. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 48] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 20. | Abraham MA, Jose R, Paul MJ. Seesawing end-tidal carbon dioxide: portent of critical carbon dioxide embolism in retroperitoneoscopy. BMJ Case Rep. 2018;2018. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 21. | Hou W, Zhong J, Pan B, Huang J, Wang B, Sun Z, Miao C. Paradoxical carbon dioxide embolism during laparoscopic surgery without intracardiac right-to-left shunt: two case reports and a brief review of the literature. J Int Med Res. 2020;48:300060520933816. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 22. | Shulman D, Aronson HB. Capnography in the early diagnosis of carbon dioxide embolism during laparoscopy. Can Anaesth Soc J. 1984;31:455-459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 71] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 23. | Richter S, Matthes C, Ploenes T, Aksakal D, Wowra T, Hückstädt T, Schier F, Kampmann C. Air in the insufflation tube may cause fatal embolizations in laparoscopic surgery: an animal study. Surg Endosc. 2013;27:1791-1797. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 24. | Butler BD, Hills BA. Transpulmonary passage of venous air emboli. J Appl Physiol (1985). 1985;59:543-547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 164] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 25. | de Plater RM, Jones IS. Non-fatal carbon dioxide embolism during laparoscopy. Anaesth Intensive Care. 1989;17:359-361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 14] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 26. | Brull SJ, Prielipp RC. Vascular air embolism: A silent hazard to patient safety. J Crit Care. 2017;42:255-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 67] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 27. | Diakun TA. Carbon dioxide embolism: successful resuscitation with cardiopulmonary bypass. Anesthesiology. 1991;74:1151-1153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 45] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 28. | Cobb WS, Fleishman HA, Kercher KW, Matthews BD, Heniford BT. Gas embolism during laparoscopic cholecystectomy. J Laparoendosc Adv Surg Tech A. 2005;15:387-390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 24] [Article Influence: 1.3] [Reference Citation Analysis (0)] |