Published online Jun 6, 2021. doi: 10.12998/wjcc.v9.i16.4001
Peer-review started: January 11, 2021
First decision: January 24, 2021
Revised: January 26, 2021
Accepted: February 26, 2021
Article in press: February 26, 2021
Published online: June 6, 2021
Processing time: 121 Days and 6.4 Hours
Pericardial rupture caused by blunt chest trauma is rare in clinical practice. Because of its atypical clinical symptoms, and because surgeons are often unfamiliar with the clinical and radiological manifestations of the injury, preoperative diagnosis is difficult; it is easily misdiagnosed and causes serious consequences.
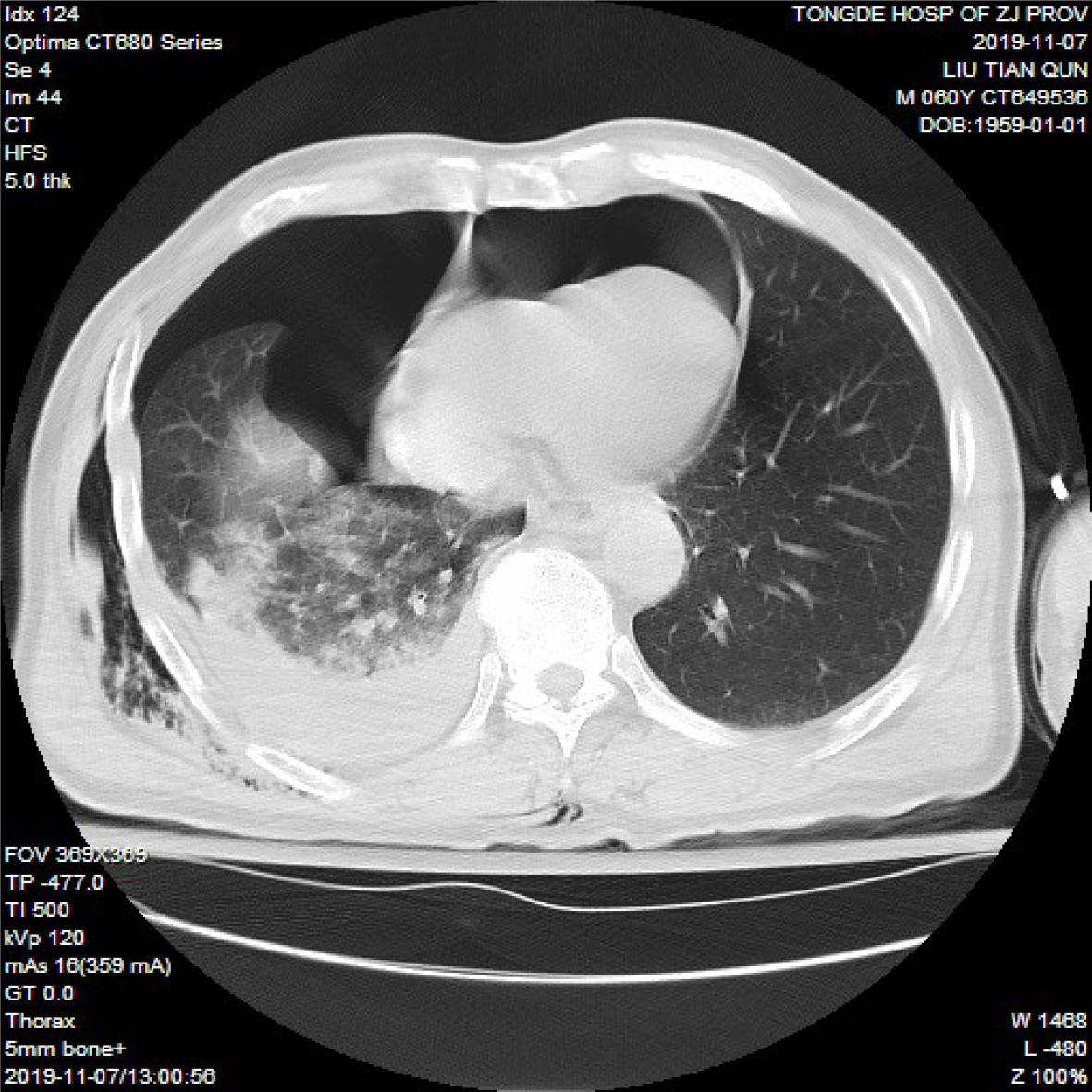
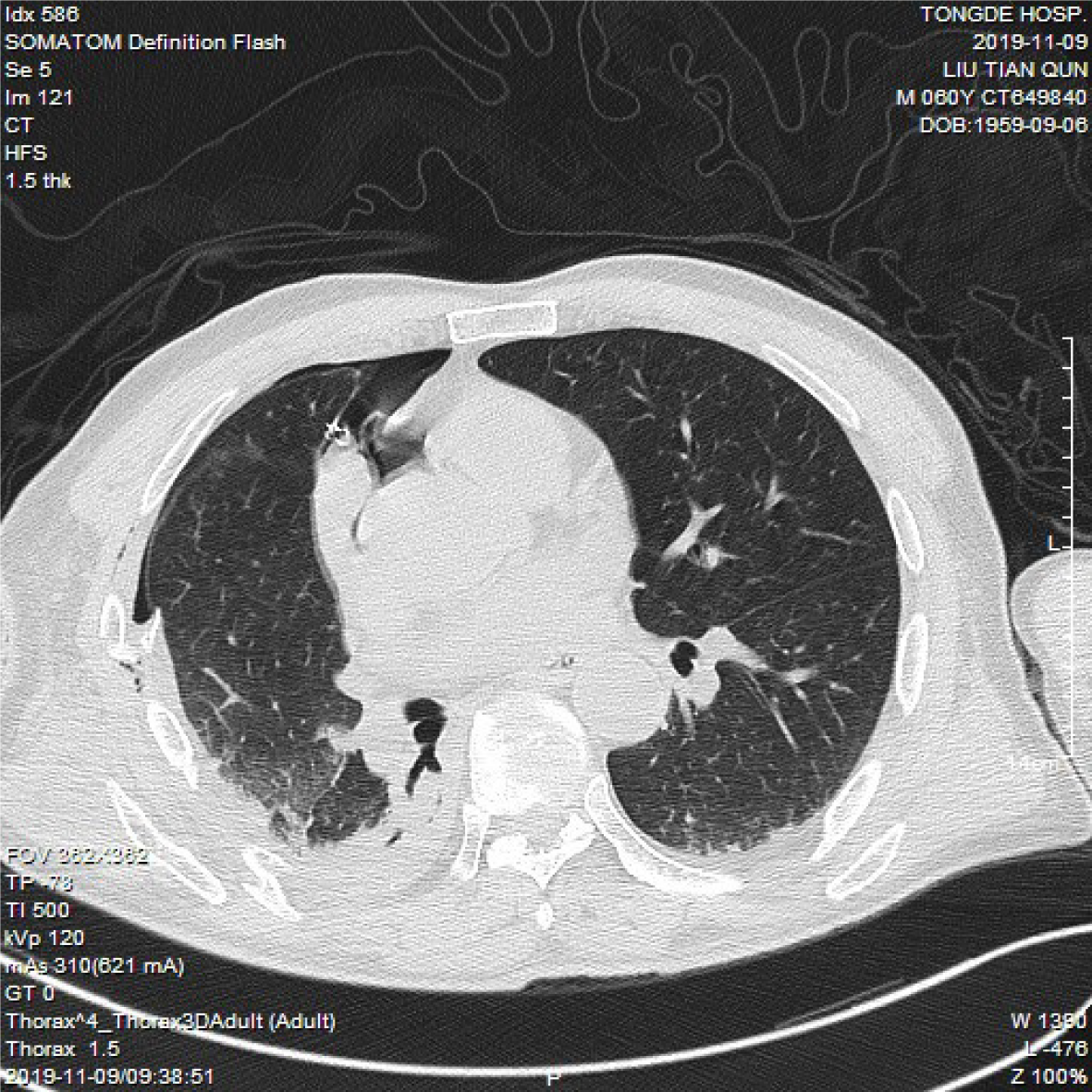
A 60-year-old man, previously healthy, was transported to the emergency room after falling from a great height. Upon arrival, his vital signs were stable. Electrocardiography and echocardiography were performed, and there was no sign of cardiac injury or ischemia. Chest and abdomen computerized tomography revealed pneumopericardium, hemopneumothorax, lung contusion, multiple rib fractures on the right side (Figure 1), and right scapula and clavicle fractures. He was admitted to the inpatient department for further observation after tube thoracostomy. The next day, the patient suddenly experienced rapid arrhythmia (the ventricular rate reached 150-180 beats/min) when turning onto his right side, accompanied by a blood pressure drop to 70/45 mm Hg and a chief complaint of palpitation. Thoracoscopy was performed urgently, and a large vertical tear (8 cm × 6 cm) was found in the pericardium. The defect was successfully repaired using a heart Dacron patch. His postoperative condition was uneventful without any fluctuations in vital signs, and he was transferred to the orthopedics department for further surgery on postoperative day 8.
Although the possibility of pericardial rupture combined with cardiac hernia is extremely low, it is one of the causes of cardiogenic shock following blunt trauma. Therefore, clinicians need to be more familiar with its characteristic manifestations and maintain a high degree of vigilance against such injuries to avoid disastrous consequences.
Core Tip: This case report describes a patient with multiple trauma following a fall from a height, who developed pericardial rupture combined with cardiac hernia. The diagnosis was not made accurately and timely before operation despite suggestive clinical and radiological findings. Therefore, clinicians need to be aware of the presentation of this potentially fatal injury so that the diagnosis can be made and thoracoscopic or thoracotomy exploration should be instituted at an earlier stage.
- Citation: Wu YY, He ZL, Lu ZY. Thoracoscopic diagnosis of traumatic pericardial rupture with cardiac hernia: A case report. World J Clin Cases 2021; 9(16): 4001-4006
- URL: https://www.wjgnet.com/2307-8960/full/v9/i16/4001.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i16.4001
Blunt traumatic rupture of the pericardium is uncommon, with an estimated incidence of 0.4%-2% among blunt trauma cases. Cardiac herniation, with a mortality rate of 67%-75%, is the most serious complication related to pericardium rupture[1]. High-velocity deceleration injuries, particularly motor vehicle accidents or falls from a height, are characteristic. However, it is usually not an isolated injury and is difficult to diagnose in the setting of acute multiple traumas.
A 60-year-old man was admitted to the emergency department after falling from a height of 3 m with complaints of whole body aches and dyspnea.
The patient was transported to the emergency room with symptoms of whole body aches and dyspnea after falling from a great height 3 h previously. Chest and abdomen computed tomography (CT) revealed pneumopericardium, hemopneumothorax, lung contusion, multiple rib fractures on the right side, and right scapula and clavicle fractures. He was admitted to the inpatient department for further observation and treatment after tube thoracostomy.
The patient had no notable previous medical history.
The patient denied any family history and had no notable past history.
The patient was conscious, and his answers were smooth and accurate. His vital signs were as follows: Body temperature, 37.2 °C; pulse, 106/min; respiration rate, 25/min; blood pressure, 110/72 mm Hg; and oxygen saturation, 98%. The heart sounds were regular, and there were no murmurs, rubs, or gallops. The breath sound on the right hemithorax was markedly decreased. Abdominal findings were unremarkable. The pelvic separation and compression tests were positive.
Laboratory data were unremarkable except for a decreased hemoglobin level at 10.3 g/dL. Electrocardiography and echocardiography were performed, and there was no sign of cardiac injury or ischemia.
Chest and abdomen CT revealed multiple rib fractures on the right side, hemopneumo
Pericardium rupture; heart hernia; hemopneumothorax; multiple rib fractures; right scapula fracture; and pelvic fracture.
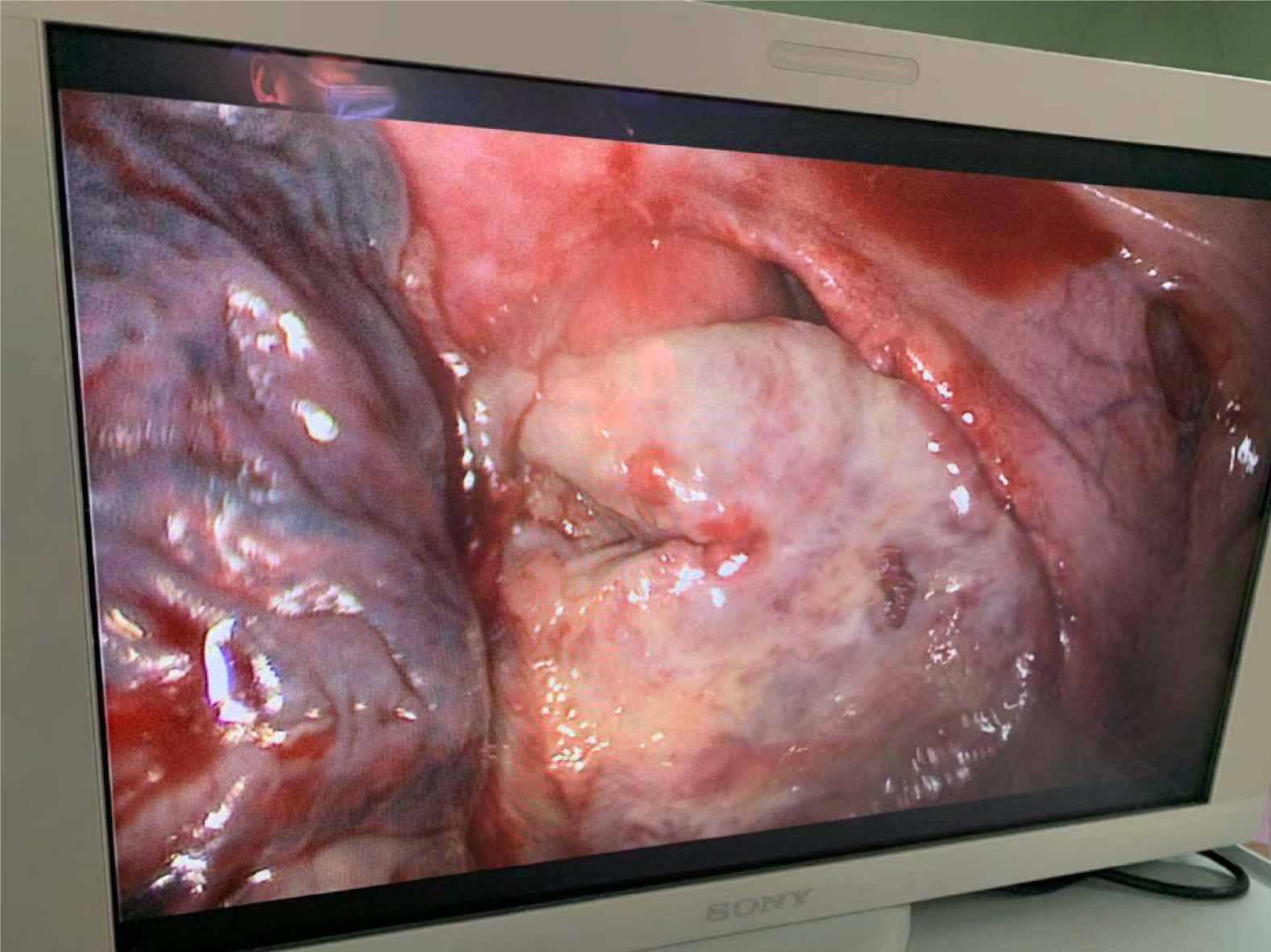
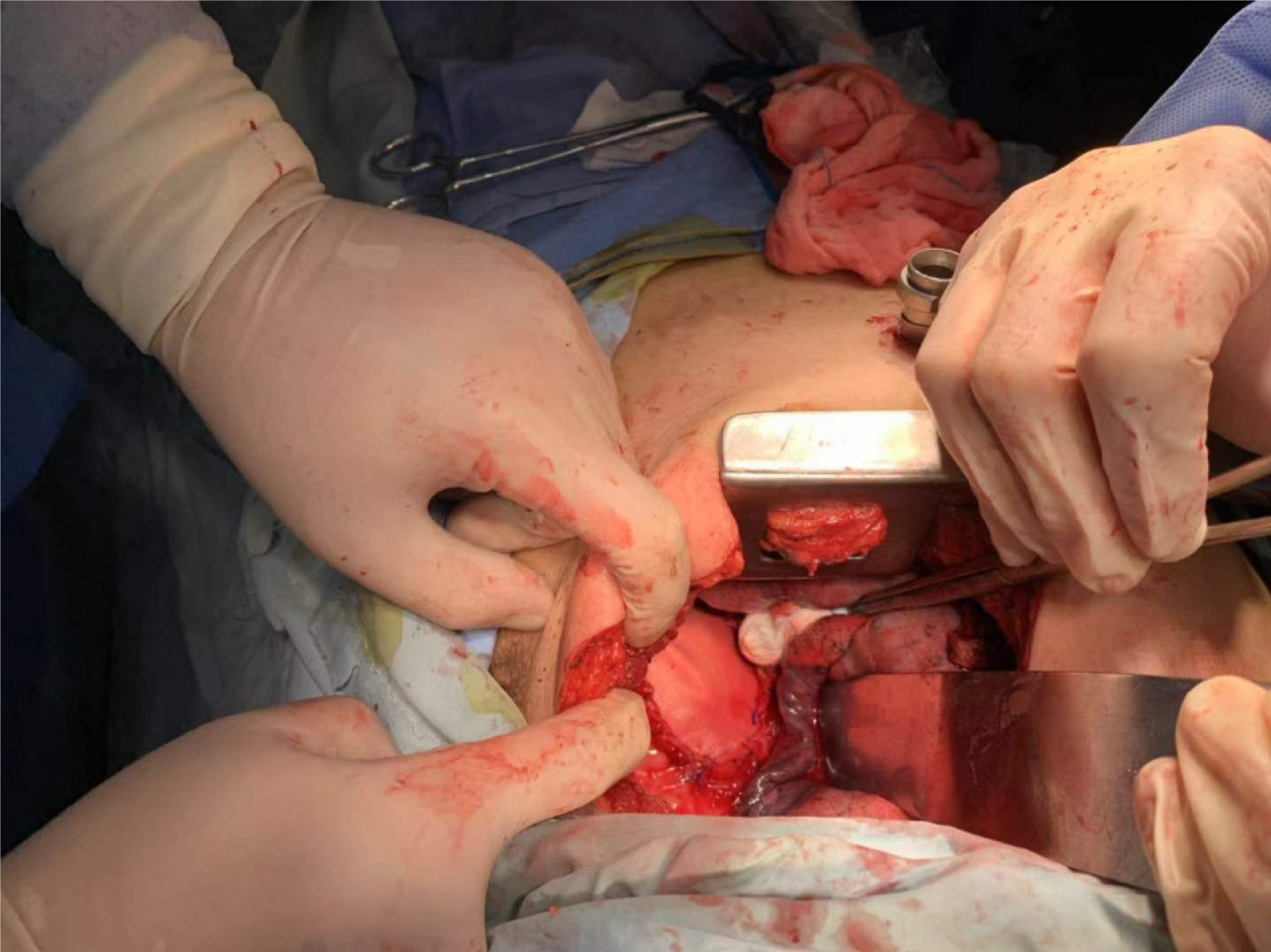
Thoracoscopy was performed on November 19, 2019. The patient was intubated with a double-lumen endotracheal tube and was positioned in the left lateral decubitus position. During the operation, there was a large vertical tear (8 cm × 6 cm) in the pericardium, and the right atrial appendage, right atrium, and superior vena cava were visualized. There was no evidence of apparent injury to the heart (Figure 3), and the right phrenic nerve was intact. The tissue edge appeared friable because of the acute inflammation and edema, and the phrenic nerve was running along the right edge. Taking the findings into consideration, we thought that a heart Dacron patch would provide a safer protection than direct suturing. Then, posterolateral thoracotomy was performed from the fifth intercostal space, and the pericardium defect was repaired using a heart Dacron patch (Figure 4). After placing the pericardial and mediastinal drainage tubes, the surgical incision was closed. His postoperative condition was uneventful without any fluctuations in vital signs, and he was transferred to the orthopedics department for further surgery on postoperative day 8.
The patient was discharged 5 wk post-injury. A follow-up CT scan 3 mo later showed no pneumothorax or pneumopericardium.
Pericardial rupture is often secondary to severe traffic accident trauma or falling from a height; because these patients have multiorgan traumatic injury, and the symptoms of pericardial rupture are sometimes atypical, it is easy to misdiagnose, which can result in serious consequences. Cook et al[3] reported that only 18% of patients had a correct diagnosis preoperatively, with most of the cases diagnosed intraoperatively. Cardiac hernia secondary to pericardial rupture is the most serious complication; if not diagnosed in time, the mortality rate can be very high[2].
Pericardial rupture can occur in two different locations: The diaphragmatic pericardium and pleural pericardium. If the diaphragmatic pericardium is damaged, the contents of the abdomen may herniate into the pericardial space, causing cardiac compression and cardiogenic shock. If the pleural pericardium ruptures, the heart may herniate into one of the pleural cavities, causing contraction, strangulation, or torsion of large blood vessels. The most common is left pleural pericardium tears, followed by diaphragm and right pleural pericardium tears[4,5]. The early diagnosis of pericardial rupture mainly relies on imaging examinations, including chest CT and transthoracic or esophageal echocardiography. If there are imaging manifestations suspicious for pericardial defects, cardiac displacement, and pneumopericardium, clinicians should be highly alert. When pericardial rupture occurs, surgical exploration should be performed immediately[6].
Cardiac hernia and pericardial rupture do not necessarily coexist at the same time; if the pericardial defect is 8-12 cm, changing the patient’s position may cause the heart to herniate through the pericardial defect and partially or completely protrude and twist, forming a heart hernia[7]. The patient may have signs consistent with cardiac tampon
In this case, clinicians did not pay enough attention to the pneumopericardium in the imaging examination. The patient repeatedly experienced pericardial tamponade symptoms such as rapid arrhythmia accompanied by a blood pressure drop during the process of turning over in the lying position. After the relevant physician departments ruled out other causes of vital sign fluctuations, it was considered that there may be pericardial rupture with cardiac hernia, and a thoracoscopic exploration was performed to confirm the preoperative suspicion and prevent disastrous complica
Traumatic rupture of the pericardium is a difficult diagnosis because pericardial defects, even with cardiac herniation, are not always associated with clinical symptoms. A high index of suspicion, prompt diagnostic protocols, and appropriate surgical management are essential to a better outcome.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Beshay M, Kermenli T S-Editor: Zhang L L-Editor: Wang TQ P-Editor: Li JH
| 1. | Guenther T, Rinderknecht T, Phan H, Wozniak C, Rodriquez V. Pericardial rupture leading to cardiac herniation after blunt trauma. Trauma Case Rep. 2020;27:100309. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 2. | Nan YY, Lu MS, Liu KS, Huang YK, Tsai FC, Chu JJ, Lin PJ. Blunt traumatic cardiac rupture: therapeutic options and outcomes. Injury. 2009;40:938-945. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 58] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 3. | Cook F, Mounier R, Martin M, Dhonneur G. Late diagnosis of post-traumatic ruptured pericardium with cardiac herniation. Can J Anaesth. 2017;64:94-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 4. | Kamiyoshihara M, Igai H, Kawatani N, Ibe T. Right or Left Traumatic Pericardial Rupture: Report of a Thought-Provoking Case. Ann Thorac Cardiovasc Surg. 2016;22:49-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Lindenmann J, Matzi V, Neuboeck N, Porubsky C, Ratzenhofer B, Maier A, Smolle-Juettner FM. Traumatic pericardial rupture with cardiac herniation. Ann Thorac Surg. 2010;89:2028-2030. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Fiedler AG, Banka P, Zaleski K, Fahey MC, Breitbart RE, Fynn-Thompson F. Delayed Presentation of Traumatic Pericardial Rupture: Diagnostic and Surgical Considerations for Treatment. Heart Surg Forum. 2018;21:E254-E256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Poletti PA, Platon A, Shanmuganathan K, Didier D, Kalangos A, Terrier F. Asymptomatic traumatic pericardial rupture with partial right atrial herniation: case report. J Trauma. 2005;58:1068-1072. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Dakak M, Gürkök S, Gözübüyük A, Genc O. Surgical repair of congenital sternal cleft in an adult to prevent traumatic pericardial rupture. Thorac Cardiovasc Surg. 2006;54:551-553. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Lee JW, Hwang JJ, Kim KD, Choi JH. Blunt cardiac and pericardial rupture without cardiac herniation: a diagnostic challenge. ANZ J Surg. 2011;81:489-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Nakamura T, Maloney JD, Osaki S. Traumatic pericardial rupture without cardiac injury. Gen Thorac Cardiovasc Surg. 2008;56:602-605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |