Published online Jun 6, 2021. doi: 10.12998/wjcc.v9.i16.3848
Peer-review started: December 9, 2020
First decision: February 12, 2021
Revised: March 17, 2021
Accepted: March 29, 2021
Article in press: March 29, 2021
Published online: June 6, 2021
Processing time: 155 Days and 22.4 Hours
Conventional recanalization techniques may fail in patients with completely occluded superior vena cava (SVC).
To analyze the effectiveness and complications of sharp recanalization for completely occluded SVC.
This was a retrospective study of patients that underwent puncture and recanalization of the SVC between January 2016 and December 2017 at our hospital. Sharp recanalization was performed using the RUPS-100 system. The patients were followed for 12 mo. The main outcomes were the patency rate of SVC and arteriovenous fistula flow during dialysis.
The procedure was successful in all 14 patients (100%). Blood pressure in the distal SVC decreased in all 14 cases (100%) from 26.4 ± 2.7 cmH2O to 14.7 ± 1.3 cmH2O (P < 0.05). The first patency rates of the SVC at 24 h and at 3, 6, 9 and 12 mo after sharp recanalization were 100%, 92.9%, 85.7%, 78.6% and 71.4%, respectively. There were two (14.3%) severe, one (7.1%) moderate and one (7.1%) minor complication. The severe complications included one case of pericardial tamponade and one case of hemothorax.
The results suggest that sharp recanalization can be an additional tool to extend or renew the use of an occluded upper extremity access for hemodialysis. This could be of use in patients with long-term maintenance hemodialysis in whom the maintenance of central venous access is often a challenge.
Core Tip: Conventional recanalization techniques may fail in patients with completely occluded superior vena cava. This study aimed to analyze the effectiveness and complications of sharp recanalization for completely occluded superior vena cava. The results suggest that sharp recanalization can be an additional tool to extend or renew the use of an occluded upper extremity access for hemodialysis. This could be of use in patients with long-term maintenance hemodialysis in whom the maintenance of central venous access is often a challenge.
- Citation: Wu XW, Zhao XY, Li X, Li JX, Liu ZY, Huang Z, Zhang L, Sima CY, Huang Y, Chen L, Zhou S. Effectiveness of sharp recanalization of superior vena cava-right atrium junction occlusion. World J Clin Cases 2021; 9(16): 3848-3857
- URL: https://www.wjgnet.com/2307-8960/full/v9/i16/3848.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i16.3848
Central vein stenosis (CVS) is a common complication of ipsilateral limb arteriovenous fistula (AVF) dialysis, which leads to obstructed AVF or arteriovenous graft (AVG) and reduced patency or swollen limbs in severe cases[1]. Although most CVS can be treated with a relatively good effect using conventional intravascular blunt recanalization using guidewires and catheters, the remaining options are limited in cases of failure of traditional recanalization. Therefore, a sharp recanalization technique using a puncture needle to directly puncture the occluded vascular segment was proposed for revascularization. Sharp recanalization was first described in two case series by Gupta et al[2] and Murphy et al[3]. Since then, several case series demonstrated the practicality and relative security of this technique. Goo et al[4] used the Rosch-Uchida needle to perform puncture, recanalization, balloon dilation and stenting of obstructed segments of the subclavian and brachiocephalic veins in 33 patients. The complications of this approach included pneumothorax, hemothorax and arterial and nerve damage. Therefore, the aim of the present study was to assess the effectiveness and complications of sharp recanalization for the management of CVS by using the RUPS-100 system. The results could provide a novel method to rescue central venous access for dialysis.
This was a case series of patients that underwent puncture and recanalization of the SVC between January 2016 and December 2017 at the Interventional Department of our hospital. The study was approved by the ethics committee of our hospital. The need for individual consent was waived by the committee.
The inclusion criteria were: (1) > 18 years of age; (2) Was undergoing autologous AVF/AVG dialysis for > 3 mo with regular dialysis three times a week and 4 h each time; (3) At least one symptom of SVC stenosis or occlusion[5-7]: (a) Facial and neck swelling; (b) Swelling and pain of the upper limb at the side of the internal AVF or bilateral upper limbs, skin pigmentation, ulceration and dysfunction; (c) Establishment of collateral circulation around the shoulders and chest wall; (d) Internal AVF murmur or change of pulse; and (e) Increased venous pressure during hemodialysis, venous blood flow ≥ 400 mL/min and difficulty of compression hemostasis at the puncture point of the internal fistula after dialysis; (4) Color Doppler ultrasound showed that the diameter of the internal fistula vessel was normal, and enhanced computed tomo
The exclusion criteria were: (1) Severe heart, liver or brain diseases; (2) Malignant SVC obstruction syndrome; (3) Combined with severe infection; (4) Loss to follow-up after surgery; or (5) Patients could not cooperate due to mental health problems.
Under local anesthesia, angiography was performed to evaluate the conditions of fistula inflow and outflow tract and central venous conditions by anterograde puncture of the outflow tract vein use a 21-G puncture needle. Then conventional catheter and guidewire technique was used to attempt recanalization. If failed, sharp recanalization was performed. Under the guidance of anteroposterior and lateral digital subtraction angiography and DynaCT (Siemens, Erlangen, Germany), a 21-G needle (Cook Medical, Bloomington, IN, United States) was used to puncture the brachiocephalic vein before a 0.035-inch Safe-TJ guidewire (Terumo, Tokyo, Japan) and a 6Fr or 7Fr vascular sheath (Terumo, Tokyo, Japan) were placed in the brachiocephalic vein. After that, a pigtail catheter (Terumo, Tokyo, Japan) was introduced to measure venous pressure at the distal end of the obstructed segment before the RUPS-100 system (Cook Medical, Bloomington, IN, United States) was placed in the brachiocephalic vein to perform puncture. The vertebral artery catheter was guided through the femoral vein access to the proximal end of the obstruction as the puncture guiding point. After identifying successful puncture, 0.035-inch guidewire and puncture needle catheter were introduced into the right atrium. Afterwards 8-12 mm balloon (Bard Peripheral Vascular, Inc., Tempe, AZ, United States) and 8-13.5 mm covered stent (Bard Peripheral Vascular, Inc., Tempe, AZ, United States) were introduced into the obstructed segment to reconstruct the inferior vena cava blood flow. The pressure at the distal end of the obstruction was measured again. If there were no abnormalities and no hemorrhagic complications, then low molecular weight heparin sodium and clopidogrel tablets were used for anticoagulation. To prevent the occurrence of pericardial tamponade, mediastinal hematoma and other serious complications caused by intraoperative hemorrhea, no routine anticoagulation treatment was used during the operation.
Technical success was defined as the diameter of the stenosis segment of the obstructed segment after percutaneous transluminal stenting (PTS) was not less than 50% of the diameter of the adjacent normal vessel[8]. Clinical success was defined as the successful use of internal AVF to complete more than once hemodialysis after surgery[9]. Early failure rate was defined as the guidewire or dilated balloon during the first PTS could not pass the affected segment of the blood vessels or ≥ 30% of vessels showed restenosis within 30 d after PTS[8]. The first patency time was defined as the time after percutaneous transluminal angioplasty and PTS to a second intervention[10].
Follow-up was censored on December 31, 2018. The patients were followed at 24 h and at 3, 6, 9 and 12 mo after percutaneous transluminal angioplasty/PTS. The patency rate of the SVC and monitoring of the AVF flow during dialysis were evaluated. The long-term outcomes were: (1) AVF flow < 200 mL/min; (2) AVG < 180 mL/min; (3) Patient died; or (4) Patient underwent balloon dilatation of SVC for a second time.
SPSS 22.0 (IBM, Armonk, NY, United States) was used for data analysis. Continuous data were presented as mean ± SD. The paired t test was used to analyze the continuous variables before/after surgery. The Kaplan-Meier method was used to analyze the patency time of the SVC after percutaneous transluminal angioplasty.
Fourteen patients were included. There were five males and nine females. They were 59.6 ± 18.9 years. The causes leading to chronic renal failure were primary ne
| Variables | n = 14 |
| Age in yr | 59.6 ± 18.9 |
| Male/female | 5/9 |
| Body mass index in kg/m2 | 23.8 ± 1.9 |
| Blood pressure in mmHg | |
| Systolic | 143.2 ± 30.7 |
| Diastolic | 82.1 ± 9.9 |
| Primary nephropathy, n (%) | 9 (64.3) |
| Diabetic nephropathy, n (%) | 3 (21.4) |
| Hypertensive nephropathy, n (%) | 2 (14.3) |
| Time of hemodialysis, n (%) | 6.5 (5-10) |
| Previous vascular access, n (%) | |
| 1 | 1 (7.1) |
| ≥ 2 | 13 (92.9) |
| Patient | Sex | Age | CVC implantation | AVF/AVG application time in mo | Symptoms | Number of collateral branches | Width of azygos vein in mm | Type of central venous stenosis | Length of obstructed segment | Diameter of balloon in mm | Diameter of stent in mm | Postoperative anticoagulation | SIR grade of complications | Remission of clinical symptoms | Venous pressure gradient before and after recanalization in cmH2O |
| 1 | F | 25 | Yes | 30 | Yes | 4 | 10.7 | IV | 10.3 | 12.0 | 12.0 | No | D | Yes | 11.7 |
| 2 | F | 43 | Yes | 12 | Yes | 2 | 9.5 | IV | 7.3 | 10.0 | 10.0 | Yes | - | Yes | 12.5 |
| 3 | F | 65 | Yes | 37 | Yes | 2 | 10.5 | IV | 8.0 | 8.0 | 8.0 | Yes | - | Yes | 10.6 |
| 4 | F | 50 | Yes | 15 | Yes | 3 | 11.7 | IV | 7.0 | 10.0 | 10.0 | No | B | Yes | 13.4 |
| 5 | F | 67 | Yes | 24 | Yes | 1 | 9.8 | IV | 8.0 | 10.0 | 8.0 | Yes | - | Yes | 12.3 |
| 6 | M | 63 | Yes | 36 | Yes | 1 | 10.4 | IV | 10.5 | 12.0 | 10.0 | No | B | Yes | 10.8 |
| 7 | F | 27 | Yes | 36 | Yes | 0 | 8.6 | IV | 8.0 | 8.0 | 8.0 | Yes | - | Yes | 13.9 |
| 8 | F | 48 | No | 84 | Yes | 0 | 9.3 | IV | 8.5 | 12.0 | 12.0 | Yes | - | Yes | 11.4 |
| 9 | F | 83 | Yes | 10 | Yes | 4 | 11.8 | IV | 6.7 | 12.0 | 12.0 | No | D | Yes | 10.7 |
| 10 | F | 60 | Yes | 4 | Yes | 0 | 9.2 | IV | 7.5 | 8.0 | 8.0 | Yes | - | Yes | 9.6 |
| 11 | M | 78 | Yes | 12 | Yes | 1 | 10.6 | IV | 8.5 | 12.0 | 12.0 | Yes | - | Yes | 13.2 |
| 12 | M | 72 | Yes | 5 | Yes | 0 | 9.5 | IV | 7.0 | 8.0 | 8.0 | Yes | - | Yes | 12.1 |
| 13 | M | 67 | Yes | 84 | Yes | 3 | 10.5 | IV | 6.8 | 8.0 | 8.0 | Yes | - | Yes | 11.9 |
| 14 | M | 86 | Yes | 96 | Yes | 0 | 10.3 | IV | 9.0 | 10.0 | 10.0 | Yes | - | Yes | 10.2 |
In this study, 13/14 (92.9%) patients with SVC occlusion had a history of central venous dialysis catheterization, including seven cases of right jugular vein, one of right subclavian vein and five of left jugular vein. All patients developed facial and neck edema, limb swelling and upper extremity and chest wall varicose veins. Five patients showed chest tightness and shortness of breath. Intraoperative angiography showed that the diameters of the azygous veins in the 14 patients were increased (diameter: 10.0 ± 0.9 mm). In 14 patients, the AVF could not meet the dialysis needs because the increased venous pressure reduced the dialysis flow: 11 patients had AVF flow of 200 mL/min and 3 had AVG flow of 180 mL/min. Chest CT-enhanced venography was performed before surgery. SVC angiography was performed through the internal AVF access and confirmed that the occlusion lesion was located at the AVC-right atrium junction; all the SVC occlusions were type IV[11]. The average length of the occlusion segments was 8.1 ± 1.2 mm.
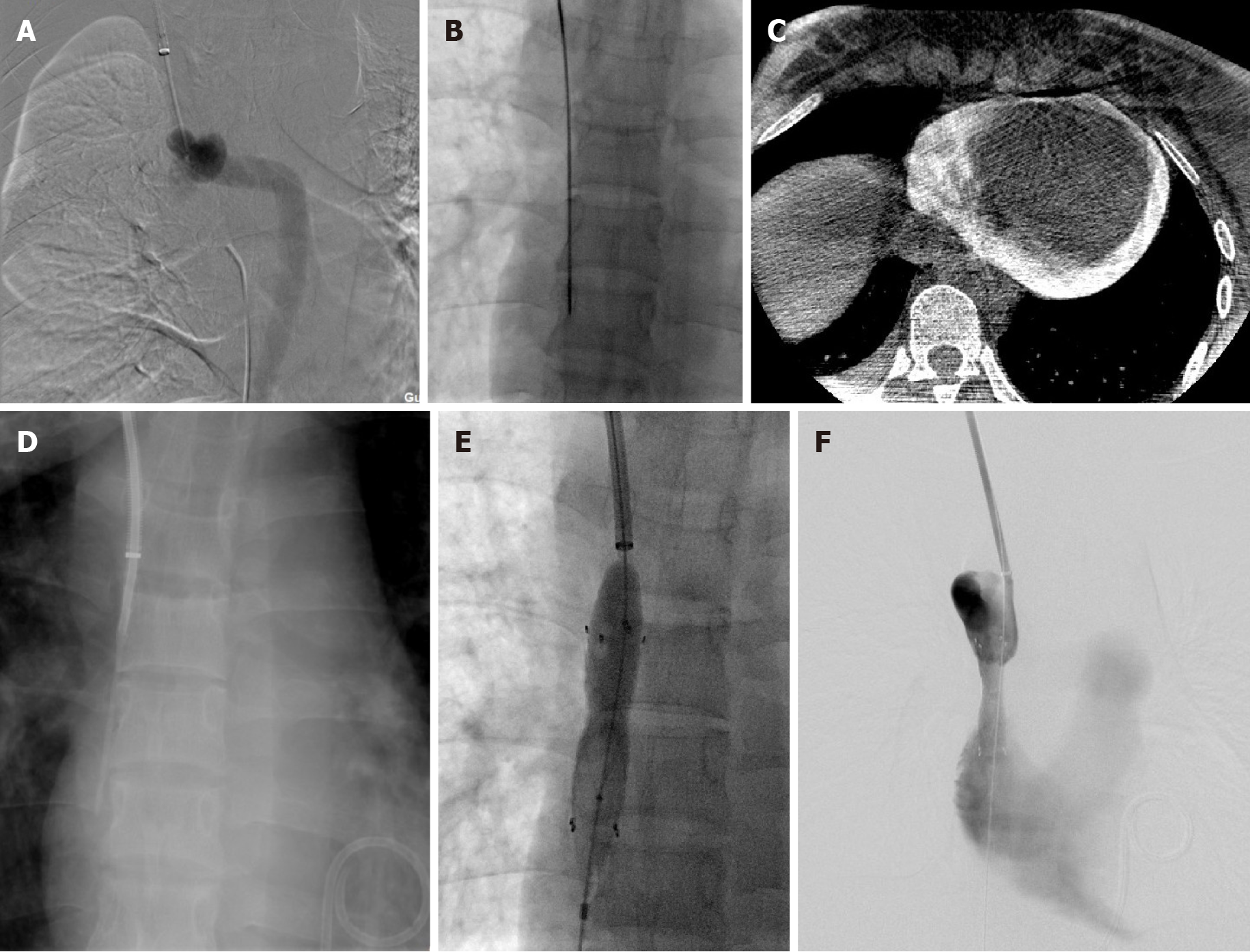
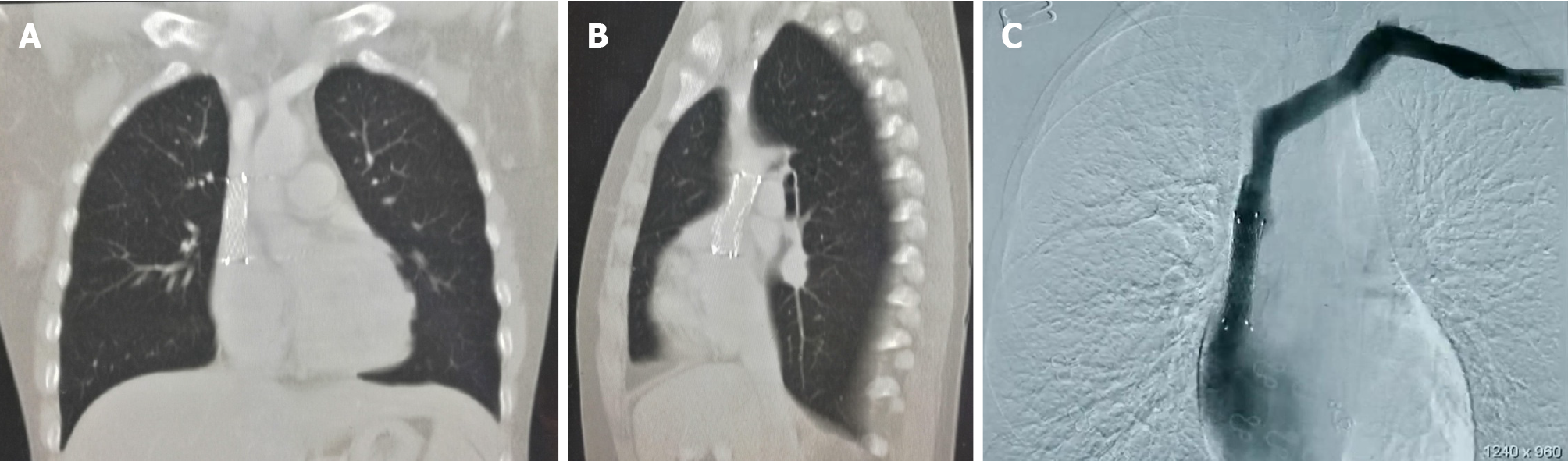
For occlusions at the SVC-right atrium junction, the technical success rate of puncture and recanalization using the RUPS-100 was 100%, and the technical success rate one-time patency was 85.7% (12/14). Surgery was stopped in one case due to intraoperative pericardial tamponade. After emergency treatment, the condition was stable and sharp recanalization was performed again after 2 wk with success (Figure 1). In another case, the surgery was stopped due to hemothorax and was also successful later. After recanalization, intraoperative angiography showed that the blood flow of the SVC was smooth, and the collateral circulation was not significantly developed compared with baseline. All symptoms of the 14 patients were relieved within 24-72 h after surgery. In the 14 patients (14/14, 100%), the pressure of the SVC was measured after recanalization, and the pressure was decreased. Figure 2 showed a typical case of recanalization after surgery. The pressure at the distal end of the obstruction was 26.4 ± 2.7 cmH2O before recanalization and was 14.7 ± 1.3 cmH2O after recanalization; the average SVC pressure gradient before and after surgery was 11.7 cmH2O (P < 0.05). Hemodialysis was performed after surgery. AVF flow was 250 mL/min, and AVG flow was 220 mL/min, which could meet the requirements for normal hemodialysis.
Complications occurred in four cases (28.6%), including two of Society of Interventional Radiology (SIR) grade D[12] (pericardial tamponade and hemothorax) and two of SIR grade B[12] (mediastinal hematoma and errhysis at supraclavicular puncture site). No perioperative deaths occurred. One patient (1/14, 7.1%) had chest pain, chest tightness and palpitation during surgery. Blood pressure dropped to 54/36 mmHg, heart rate was 120 bpm, and SaO2 was 89%. The lips showed cyanosis. Auscultation showed distant heart sounds, and then sudden cardiac arrest occurred. External chest compression was performed, and heart rate was recovered. Emergency bedside ultrasound and DynaCT identified acute pericardial tamponade. Immediate pericardial catheterization drainage was performed, and 450 mL of hemorrhagic fluid was drained. After 4 d, ultrasound showed no pericardial effusion, and the pericardial drainage tube was withdrawn after successful recanalization after the second surgery 2 wk later. One patient (1/14, 7.1%) had severe pain during surgery. The Numerical Rating Scale score was 10 points, and the vital signs were stable. DynaCT scan showed large exudation in the lung and new pleural effusion. The thoracic catheter drainage showed hemorrhagic fluid, and the diagnosis was hemothorax. The patient was treated with analgesics and internal medicine was used to stop bleeding. One week later, chest CT showed that the bleeding was self-absorbed. One patient (7.1%) had postoperative errhysis at the right supraclavicular puncture site. Sterile gauze was used for compression for 5-10 min, and the site was correct after gauze fixation. No surgical treatment was needed. One patient (1/14, 7.1%) had chest pain after surgery. Re-examination of the chest CT showed mediastinal hematoma (diameter of 1 cm). It was relieved after analgesic treatment. One week later, chest CT showed that the mediastinal hematoma had resolved by itself.
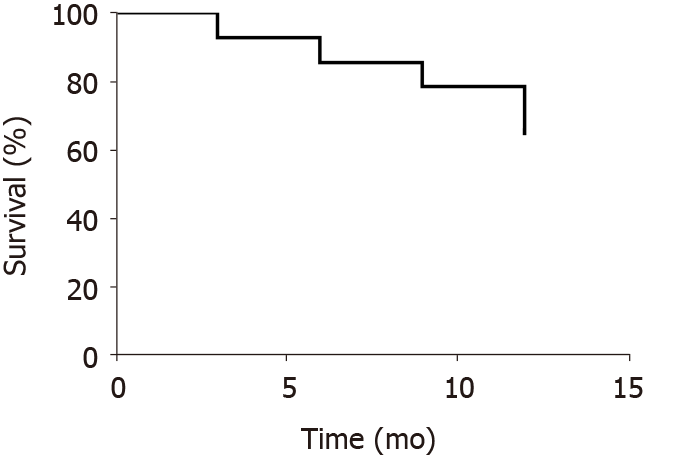
Fourteen patients were successfully treated with RUPS-100 recanalization of the SVC. All 14 patients (14/14, 100%) were able to use the AVF/AVG for hemodialysis after surgery. The first patency rate of the SVC was 100% in 14 patients at 24 h after surgery. The first patency rate was 92.9%, 85.7%, 78.6% and 71.4% at 3, 6, 9 and 12 mo postoperatively, respectively (Figure 3).
After autologous AVF/AVG surgery, complete SVC occlusion occurred.
For the patient with the operation failure of the conventional recanalization, a sharp puncture was performed at the junction of the SVC and the right atrium by using RUPS-100 puncture system. Then the sacculi dilation and stent with tectorial membrane implantation were performed to recanalization.
In a total of 14 patients, all 14 cases (14/14, 100%) were successfully recanalized. All patients were able to be treated with AVF/AVG hemodialysis after surgery. From 3, 6, 9, 12 mo after surgery, the patency was 92.9%, 85.7%, 78.6 % and 71.4%, respectively.
This case series suggested that sharp recanalization can be an additional tool to extend or renew the use of an occluded upper extremity access for hemodialysis. This could be of use in patients with long-term maintenance hemodialysis in whom the maintenance of the central venous access is often a challenge.
In the present study, all patients developed facial and neck edema, limb swelling and upper extremity and chest wall varicose veins. Five patients showed chest tightness and shortness of breath. Intraoperative angiography showed that the diameters of the azygous veins in all 14 patients were increased. In a study by Levit et al[13], 9% (8/86) of venography showed complete occlusion of the central vein, but no symptoms such as upper limbs, chest wall or facial swelling occurred. It strongly suggests that the establishment of collateral circulation can significantly reduce the abnormal blood pressure caused by the AVF. Symptomatic CVS that cannot be compensated by collateral circulation needs to be treated. Due to the small number of patients, we failed to validate this view and further analyzed the relationship between the establishment of the collateral circulation and the severity of AVC occlusion. In the 14 patients, the AVF could not meet the dialysis requirement because of low flow. Chest CT-enhanced venography was performed before surgery, and SVC angiography was performed through the internal AVF access to confirm that the occlusion was located at the SVC-right atrium junction. All SVC occlusions were type IV[11].
Advances in endovascular treatment technology have provided a safe and viable first-line therapy for clinicians to treat CVS. However, when the central vein is completely occluded, it is often impossible to achieve vascular recanalization using conventional recanalization techniques. Gupta et al[2] first reported the sharp recanalization technique using an 18-G needle to puncture the right subclavian vein, but different tools can be used. Compared to Gupta et al[2], Anil et al[14] and Brountzos et al[15] reported sharp recanalization technique using the Outback LTD catheter (OutBack LTD reentry catheter, Cordis Medical, Fremont, CA, United States) with better guidance quality.
We selected the RUPS-100 puncture system because it has a similar guidance quality to the Outback LTD catheter for sharp puncture. Consistent with our study, Goo et al[4] used the Rosch-Uchida needle for sharp recanalization, balloon dilation and stenting of the obstructed segment of subclavian vein and brachial vein in 33 patients. In their study, a Rosch-Uchida needle was introduced through the internal AVF to puncture and recanalize the occluded vascular segment to treat the subclavian vein occlusion after failure with conventional guidewire catheter. In addition, the catheter was placed in the proximal end of the occlusion through the femoral vein, which was used as the diagnostic catheter to mark the end point of the puncture.
For the occluded segment of the brachiocephalic vein with failed recanalization, a Rosch-Uchida sheath was inserted through the internal jugular vein and the diagnostic catheter was placed in the SVC. In contrast to the internal jugular vein, we selected the right brachiocephalic vein to place the Rosch-Uchida sheath, where it can be easier to adjust the puncture direction of the trocar during the puncture process. In addition, in the study of Zhai et al[16], for patients with bilateral innominate vein occlusion, a percutaneous cholecystectomy needle was used to directly puncture the SVC through the subclavian vein to achieve central venous catheterization. In contrast to Zhai et al[16], we used the Chiba needle to puncture the right brachiocephalic vein directly through the right supraclavicular site to avoid the interference of the clavicle and rib on the puncture.
The risks of SVC surgery include pneumothorax, hemothorax, arterial or nerve injury, pericardial tamponade and mediastinal hematoma. In our study, one case of hemothorax occurred, which was thought to be caused by damage to the lung tissue or pleura by the needle. It was improved after thoracic drainage and drug treatment with no sequelae, and the SIR grade was D. In this study, there was also one case of pericardial tamponade (SIR D). Because the occluded segment was close to the right atrium, it was caused by the puncture-induced injury of the pericardium during puncture and recanalization. It was improved after emergency treatment with no sequelae.
In this study, the success rate of sharp recanalization in treating SVC-right atrial junction occlusion was 100%, and the success rate of one-time recanalization was 85.7%. The pressure difference from before to after recanalization was statistically significant. In our study, after recanalization, blood flow was seen in the SVC, and collateral circulation was not significantly developed compared with that before surgery. The symptoms of SVC obstruction were all relieved within 72 h after surgery. In addition, all patients were able to undergo conventional hemodialysis with adequate AVF flow rate. The first patency rate of the SVC was 100% at 24 h postoperatively. The first patency rates at 3, 6, 9, and 12 mo were 92.9%, 85.7%, 78.6% and 71.4%, respectively. In the study by Goo et al[4], the technical success rate was 93.9% (31/33), and the primary patency rates at 3, 6, and 12 mo after surgery were 43.6%, 24% and 8%, respectively, and the secondary patency rates at 3, 6 and 12 mo were 77.4%, 68.8% and 55.9%, respectively. The technical success rate of the surgery and the first patency rate were relatively high, which is associated with the small number of samples, the maturity of the technique and the placement of covered stent in the present study.
The present study has limitations. It was a retrospective study with all the inherent limitations, and there was no control group. The sample size was small, and some results may be biased. In addition, because of the complications associated with surgery, anticoagulation therapy was not routinely used after surgery. Although the study by Haddad et al[17] showed that the clinical and therapeutic results of benign SVC syndrome after stenting were not significantly different between patients with and without postoperative anticoagulation, this point still needs further research for confirmation.
This study retrospectively analyzed the cases of the SVC-right atrial junction occlusion that underwent sharp recanalization. The results strongly suggested that sharp recanalization has a relatively high surgical success rate and low complication rate. This could be an effective method for vascular recanalization when the routine endovascular treatment fails. It provides the possibility for extending and rebuilding the upper limb access for hemodialysis.
Conventional recanalization techniques may fail in patients with completely occluded superior vena cava (SVC).
Although most central vein stenosis can be treated with a relatively good effect using conventional intravascular blunt recanalization using guidewires and catheters, the remaining options are limited in cases of failure of traditional recanalization.
This study aimed to analyze the effectiveness and complications of sharp recanalization for completely occluded SVC.
This was a retrospective study of patients that underwent puncture and recanalization of the SVC between January 2016 and December 2017 at our hospital. Sharp recanalization was performed using the RUPS-100 system. The patients were followed for 12 mo. The main outcomes were the patency rate of SVC and AVF flow during dialysis.
The procedure was successful in all 14 patients (100%). Blood pressure in the distal SVC decreased in all 14 cases (100%) from 26.4 ± 2.7 cmH2O to 14.7 ± 1.3 cmH2O (P < 0.05). The first patency rates of the SVC at 24 h and at 3, 6, 9 and 12 mo after sharp recanalization were 100%, 92.9%, 85.7%, 78.6% and 71.4%, respectively. There were two (14.3%) severe, one (7.1%) moderate and one (7.1%) minor complication. The severe complications included one case of pericardial tamponade and one case of hemothorax.
The results suggest that sharp recanalization can be an additional tool to extend or renew the use of an occluded upper extremity access for hemodialysis. This could be of use in patients with long-term maintenance hemodialysis in whom the maintenance of central venous access is often a challenge.
The clinical and therapeutic results of benign SVC syndrome after stenting were not significantly different between patients with and without postoperative anticoagulation. This point still needs further research for confirmation.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Jamil AK, Lee SS S-Editor: Gao CC L-Editor: Filipodia P-Editor: Yuan YY
| 1. | Cuthbert GA, Lo ZJ, Kwan J, Chandrasekar S, Tan GWL. Outcomes of Central Venoplasty in Haemodialysis Patients. Ann Vasc Dis. 2018;11:292-297. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 2. | Gupta H, Murphy TP, Soares GM. Use of a puncture needle for recanalization of an occluded right subclavian vein. Cardiovasc Intervent Radiol. 1998;21:508-511. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 46] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 3. | Murphy TP, Webb MS. Percutaneous venous bypass for refractory dialysis-related subclavian vein occlusion. J Vasc Interv Radiol. 1998;9:935-939. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Goo DE, Kim YJ, Choi DL, Park SI, Yang SB, Moon C, Song D. Use of a rosch-uchida needle for recanalization of refractory dialysis-related central vein occlusion. AJR Am J Roentgenol. 2010;194:1352-1356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 5. | Kundu S. Central venous disease in hemodialysis patients: prevalence, etiology and treatment. J Vasc Access. 2010;11:1-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 53] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 6. | Aj A, Razak Uk A, R P, Pai U, M S. Percutaneous intervention for symptomatic central vein stenosis in patients with upper limb arteriovenous dialysis access. Indian Heart J. 2018;70:690-698. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Horikawa M, Quencer KB. Central Venous Interventions. Tech Vasc Interv Radiol. 2017;20:48-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 24] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 8. | Karnabatidis D, Kitrou P. Drug eluting balloons for resistant arteriovenous dialysis access stenosis. J Vasc Access. 2017;18:88-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 9. | Chandler NM, Mistry BM, Garvin PJ. Surgical bypass for subclavian vein occlusion in hemodialysis patients. J Am Coll Surg. 2002;194:416-421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 34] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 10. | Dember LM, Holmberg EF, Kaufman JS. Randomized controlled trial of prophylactic repair of hemodialysis arteriovenous graft stenosis. Kidney Int. 2004;66:390-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 99] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 11. | Stanford W, Doty DB. The role of venography and surgery in the management of patients with superior vena cava obstruction. Ann Thorac Surg. 1986;41:158-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 53] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 12. | Cohen EI, Beck C, Garcia J, Muller R, Bang HJ, Horton KM, Hakki F. Success Rate and Complications of Sharp Recanalization for Treatment of Central Venous Occlusions. Cardiovasc Intervent Radiol. 2018;41:73-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 52] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 13. | Levit RD, Cohen RM, Kwak A, Shlansky-Goldberg RD, Clark TW, Patel AA, Stavropoulos SW, Mondschein JI, Solomon JA, Tuite CM, Trerotola SO. Asymptomatic central venous stenosis in hemodialysis patients. Radiology. 2006;238:1051-1056. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 84] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 14. | Anil G, Taneja M. Revascularization of an occluded brachiocephalic vein using Outback-LTD re-entry catheter. J Vasc Surg. 2010;52:1038-1040. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 15. | Brountzos EN, Preza O, Kelekis A, Panagiotou I, Kelekis N. Recanalization of dialysis catheter-related subclavian vein occlusion using a re-entry device: report of two patients. Cardiovasc Intervent Radiol. 2011;34:207-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Zhai S, Zhao Q, Feng Y, Yu Y, Zhou L, Cui T, Fu P. Placement of tunneled cuffed vascular catheter through superior vena cava puncture. J Vasc Surg Venous Lymphat Disord. 2017;5:547-552. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 17. | Haddad MM, Thompson SM, McPhail IR, Bendel EC, Kalra M, Stockland AH, Neidert NB, Andrews JC, Misra S, Bjarnason H, Neisen MJ. Is Long-Term Anticoagulation Required after Stent Placement for Benign Superior Vena Cava Syndrome? J Vasc Interv Radiol. 2018;29:1741-1747. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 21] [Article Influence: 3.0] [Reference Citation Analysis (0)] |