Published online Apr 26, 2020. doi: 10.12998/wjcc.v8.i8.1454
Peer-review started: February 18, 2020
First decision: March 5, 2020
Revised: March 12, 2020
Accepted: April 4, 2020
Article in press: April 4, 2020
Published online: April 26, 2020
Processing time: 65 Days and 1.5 Hours
Differential diagnosis between extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue and inflammatory bowel disease is mainly based on histopathologic evaluation of intestinal biopsies, although there is no single definitive diagnostic investigation and that circumstance can lead to misdiagnosis in particular cases. Herein we present a rare, ulcerative form of marginal zone lymphoma which mimics the Crohn’s disease (CD) of upper digestive tract.
A 50-year-old man was presented with recurrent episodes of malaise and melena also weight loss. Enteroscopy of the small bowel demonstrated an ulcer in the jejunum. Microscopically, biopsies showed lymphoplasmacytic infiltrate. Diagnosis of CD was made. Primary treatment consisted of prednisone and azathioprine and was followed by azathioprine 100 mg per day with good clinical response in the following 2 years until relapse. At this time the results of endoscopic biopsies derived from proximal wall of stomach revealed Helicobacter pylori-negative marginal zone lymphoma of the gastric fundus. Immunophenotyping confirmed atypical CD20-positive cell population. Based on these biopsies, marginal zone lymphoma of mucosa-associated lymphoid tissue was diagnosed. Unfortunately, the contact with the patient was lost until one year later he was hospitalized with nausea, vomiting and severe pain because of gastrointestinal perforation. Four months later after laparotomy, the patient was treated with a course of chemotherapy. Complete remission was observed following 6 cycles of treatment.
This case report highlights the clinical relevance of knowledge and awareness of marginal zone lymphoma simulating CD.
Core tip: Mucosa-associated lymphoid tissue (MALT) lymphoma and Crohn‘s disease require different treatments, but both diseases can cause similar gastrointestinal symptoms and have no definitive diagnostic tests. The goal of this case report is to promote the more attentive attitude of gastroenterologists to the rare cases of lymphomas. In the presented case of a 52-year-old patient with a previous diagnosis of the small intestine Crohn's disease and good response to the corresponding treatment, the MALT lymphoma had a rare presentation form–an ulcer, while most MALT lymphomas appear as a mass. This circumstance has made it very difficult to make a correct diagnosis.
- Citation: Stundiene I, Maksimaityte V, Liakina V, Valantinas J. Mucosa-associated lymphoid tissue lymphoma simulating Crohn’s disease: A case report. World J Clin Cases 2020; 8(8): 1454-1462
- URL: https://www.wjgnet.com/2307-8960/full/v8/i8/1454.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i8.1454
Isaacson and Wright[1] first identified extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue (MALT) lymphoma in 1983. It is a type of non-Hodgkin's lymphoma and it is defined as an extranodal lymphoma composed of morphologically heterogeneous small B-cells, including marginal (centrocyte-like) cells, a cell resembling monocytoid cells, small lymphocytes, scattered immunoblasts, and centroblast-like cells[1]. MALT lymphomas commonly follow dysregulation of the immune system triggered by sustained interference with chronic infections or autoimmune disorders.
Like every other gastrointestinal lymphoma, MALT lymphoma can be clinically confused with inflammatory bowel disease (IBD). Both of them can cause similar gastrointestinal symptoms such as abdominal pain, diarrhea, exhaustion, weight loss and malnutrition and lack of specificity in the clinical characteristics. On the other hand, they have other differences, including localization of the disease. Crohn’s disease (CD) can involve any segment of gastrointestinal tract from mouth to anus, especially the terminal ileum and ileocecal region[2]. Rarely, CD may affect the stomach or duodenum, sometimes-even esophagus[3]. Low-grade lymphomas can develop in every organ or cavity of the body that is lined by mucosa, although MALT is most often diagnosed in gastrointestinal organs of all non-Hodkin lymphomas, 5%-10%[4-6]. Even though, the primary gastric lymphoma still is a rare disease[7].
While endoscopy is the first choice for detecting lesions endoscopic findings are very important in differential diagnosis. Ulcers in CD patients tend to be longitudinal and stretched across several intestinal folds and ulcers in patients with lymphoma are usually characterized as irregular ulcers[8].
These two pathologies require specific treatment and provide different prognosis to the patient. The differentiation between these two pathologies sometimes is only based on histopathologic evaluation of intestinal biopsies.
The situation is further complicated because there is no single definitive diagnostic investigation or laboratory test to exist for the diagnosis of IBD[9]. All of the above leave the gastroenterologists at risk of making misdiagnosis of such patients.
While only a few cases of MALT lymphoma mimicking a CD have been reported, the goal of this case report is to promote the more attentive attitude of gastroenterologists to the rare cases of lymphomas. In connection with this, we want to encourage practitioners not to miss an unusual MALT lymphoma presentation like herein described case of 52-year-old patient with a previous diagnosis of small intestine CD who was later diagnosed for stomach and jejunum MALT lymphoma.
A 50-year-old Caucasian man was presented to our hospital with episode of malaise and melena.
He had reportedly lost 6 kg of weight during one year and had episodic abdominal cramping pain.
He had gastric ulcer disease diagnosed several years before.
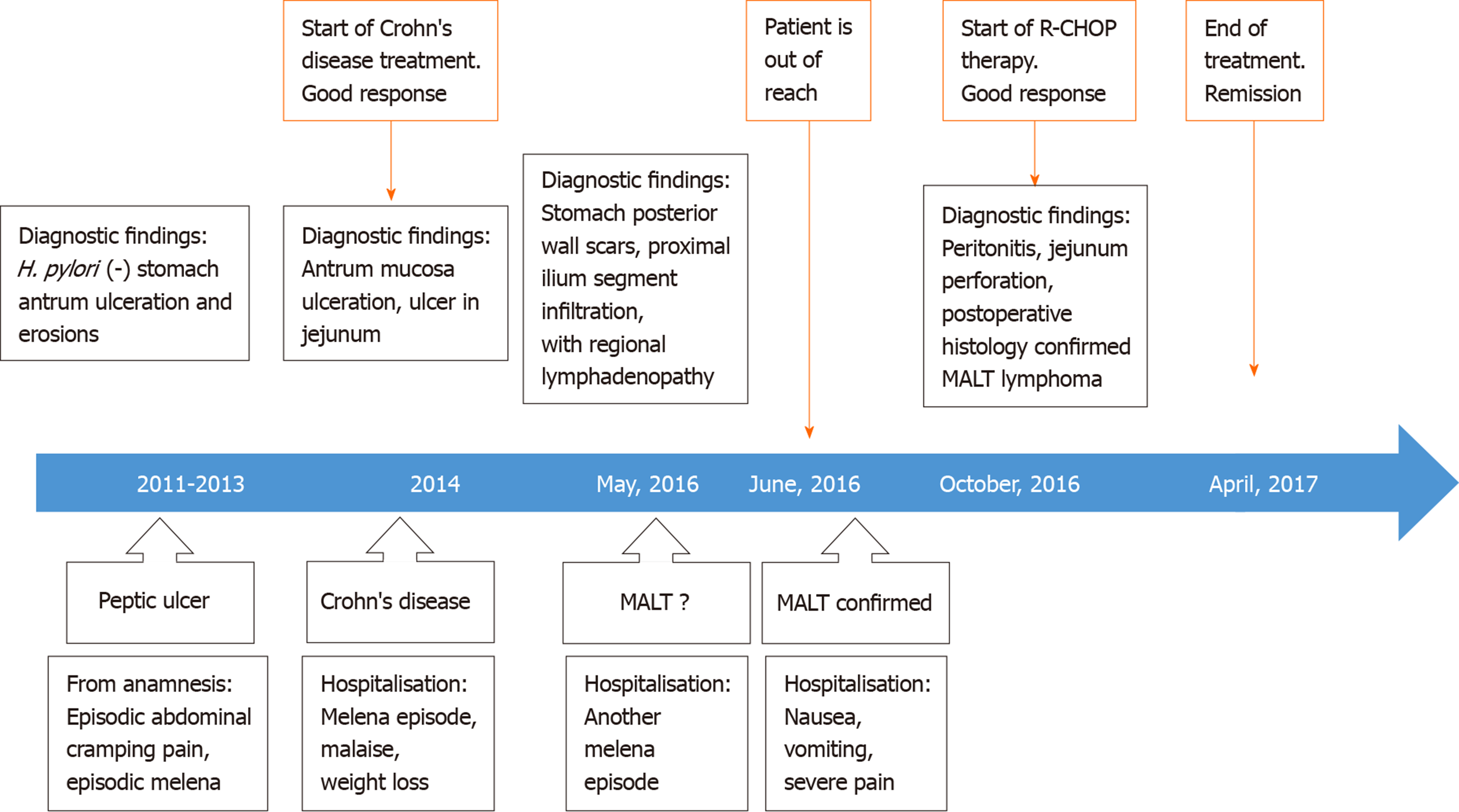
He had no other symptoms and no family history of gastrointestinal diseases or cancer (Figure 1).
Upon physical examination, no abnormal findings were found.
Complete blood count results were as follows: Red blood cells, 3.14 × 1012/L [(4–5.5) × 1012/L]; hemoglobin, 87 g/L [(120–160) g/L]; white blood cells, 6.56 × 109/L [(4–10) ×109/L]; platelets, 151 × 109/L [(100–300) × 109/L]. Biochemical examination revealed CRP 0.2 mg/L [(0-5) mg/L]. Serum albumin was not measured at this time.
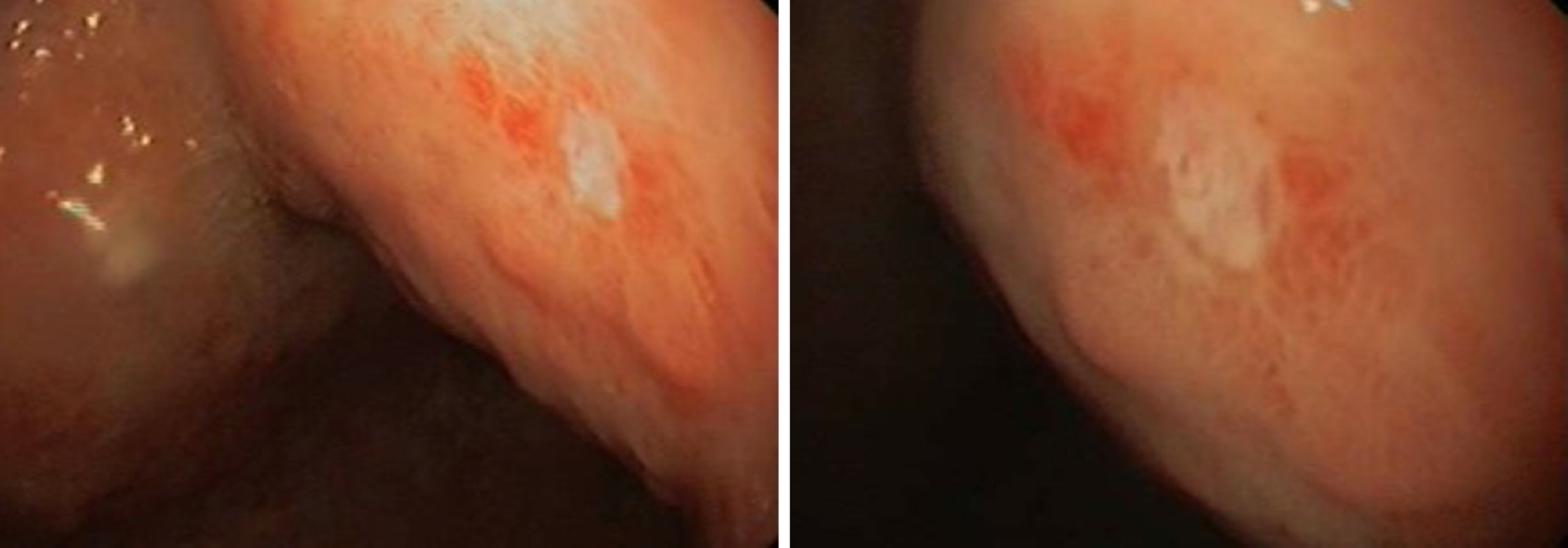
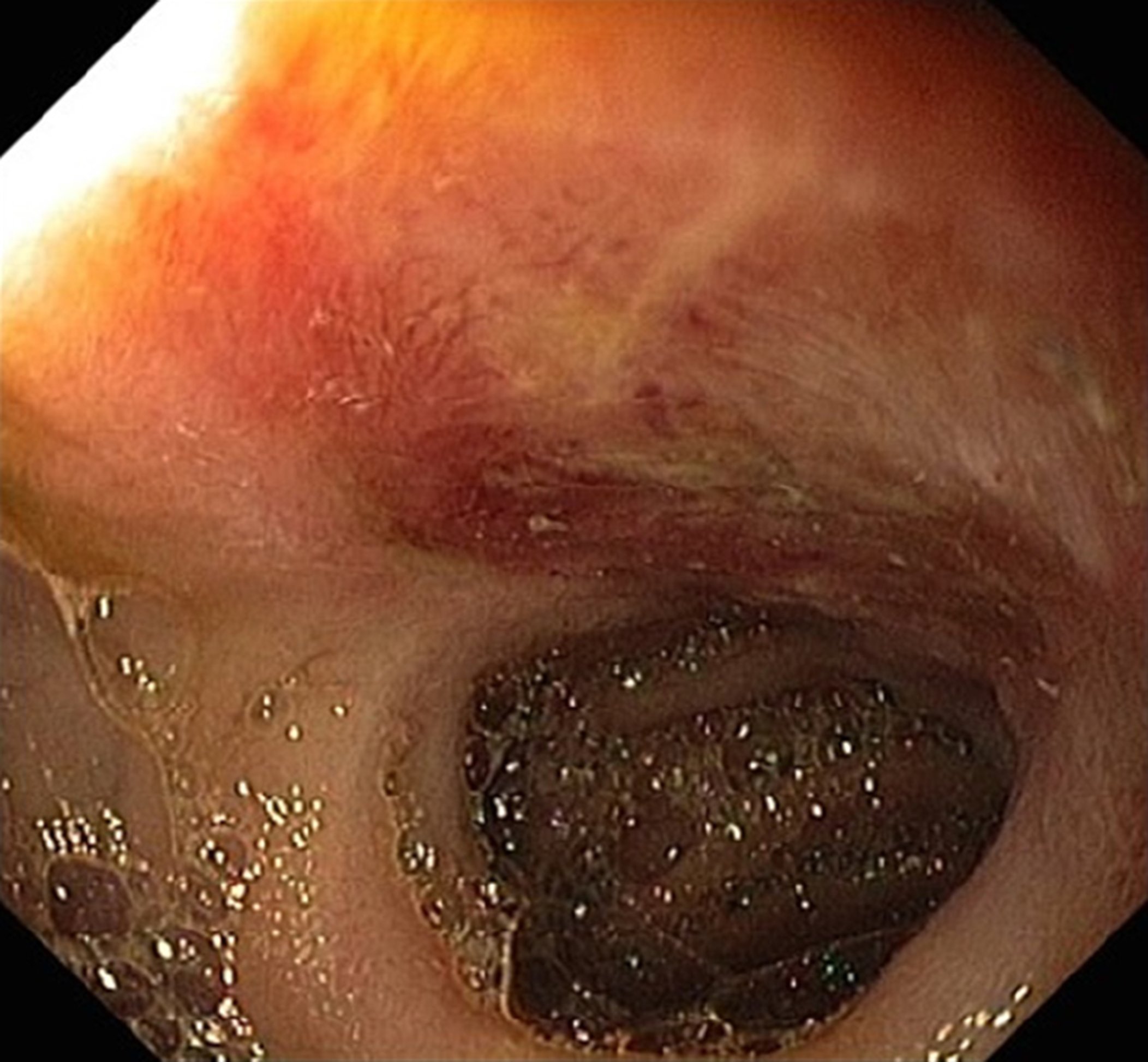
Upper gastrointestinal endoscopy revealed ulceration of mucosa in antrum. There were a few 5 mm superficial ulcers in the antrum (Figure 2). There were no specific findings in colonoscopy. Enteroscopy of the small bowel demonstrated a 1.5 cm ulcer in the jejunum (Figure 3).
Microscopically, stomach biopsies showed lymphoplasmacytic infiltrate with neutrophils and eosinophils, also a detritus with leukocytes and granulation tissue of one of the ulcers where biopsy was taken from. Biopsies were negative for Helicobacter pylori (H.pylori) infection.
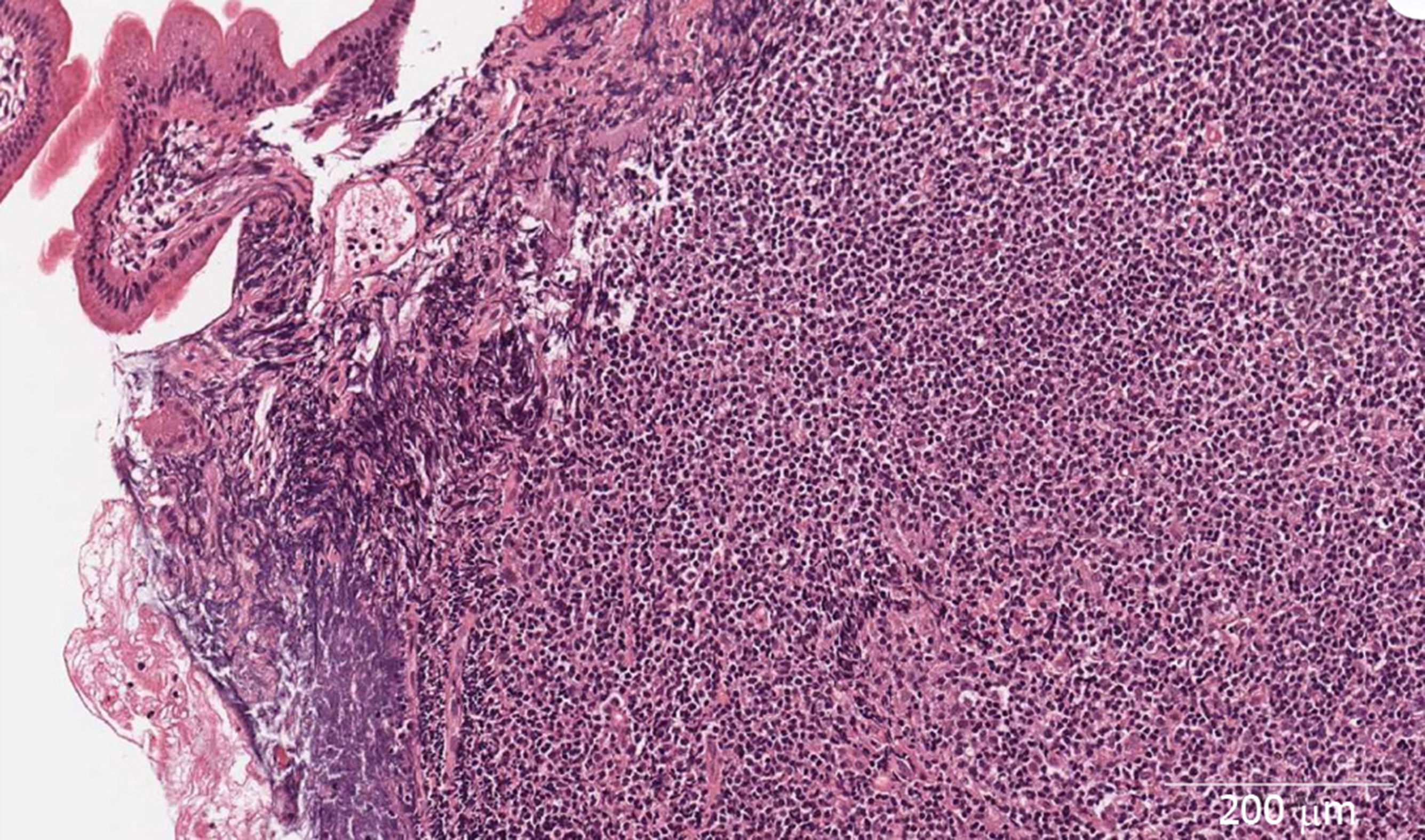
Microscopically, jejunum biopsies revealed lymphoplasmacytic infiltrate, a common finding in chronic CD, granulation tissue and crypt distortion suggesting chronic inflammation (Figure 4). Histopathology suggested the diagnosis of CD. Since there were no histological evidences of possible lymphoma, imunophenotyping was not performed at this time.
Diagnosis of CD was made. Primary treatment consisted of prednisone and azathioprine and was followed by azathioprine 100 mg per day.
Two years later, he had another melena episode and was hospitalized again. Laboratory testing indicated anemia - hemoglobin, 98 g/L (120–160 g/L). Lactate dehydrogenase, ferritin, electrolytes, glucose, renal function tests were all normal. CRP level was high 162.4 mg/L (0-5 mg/L). The patient was subjected to endoscopic esophageal gastroduodenoscopy. It revealed atrophic mucosal tissue interposed between normal appearing mucosa on the posterior wall of the stomach. Biopsy samples were acquired. The lumen along with mucosa of esophagus and duodenum were normal. Abdominal ultrasonography displayed a segmental ileum wall thickening. Enlarged lymph nodes (11 mm) were found in the lower part of the abdomen. No liver pathology was showed. Small bowel magnetic resonance imaging (MRI) enterography revealed local circumferential infiltration of the proximal part of the ileum. In addition, a mesenteric nodal mass was presented.
However, despite all the clinical details, the diagnosis of MALT lymphoma was hesitated. With the clinical picture and radiology findings, still not knowing results of the biopsy, it was decided to increase the dosage of azathioprine from 100 mg to 150 mg daily and discharge the patient from the hospital. CRP was 11.4 mg/L on the day patient was released from the hospital.
One week later, results of endoscopic biopsies derived from proximal wall of stomach revealed H. pylori negative MALT lymphoma of the gastric fundus. Immunophenotyping of biopsies confirmed a B-cell population with the surface proteins listed in Table 1[10]. Based on these biopsies, MALT lymphoma was diagnosed.
| Immunophenotype | Results | Typical MALT[10] |
| CD20 | + | + |
| CD23 | - | - |
| CD5 | - | - |
| CD21 | - | - |
| Bcl 6 | - | - |
| Cyclin D1 | - | - |
| CD 43 | - | +/- |
Unfortunately, the contact with the patient was lost and he failed to get any treatment due to MALT lymphoma diagnosis at this time.
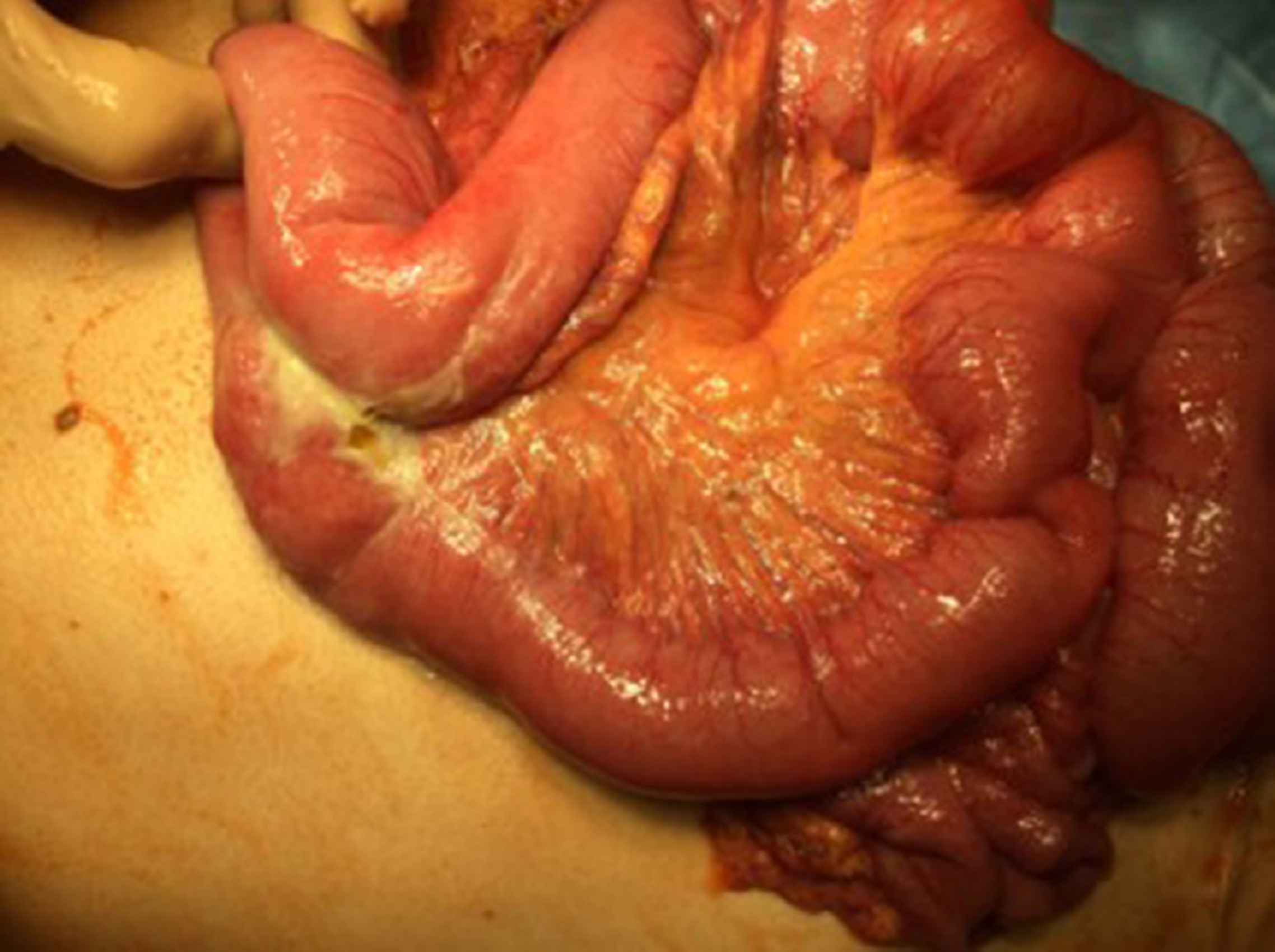
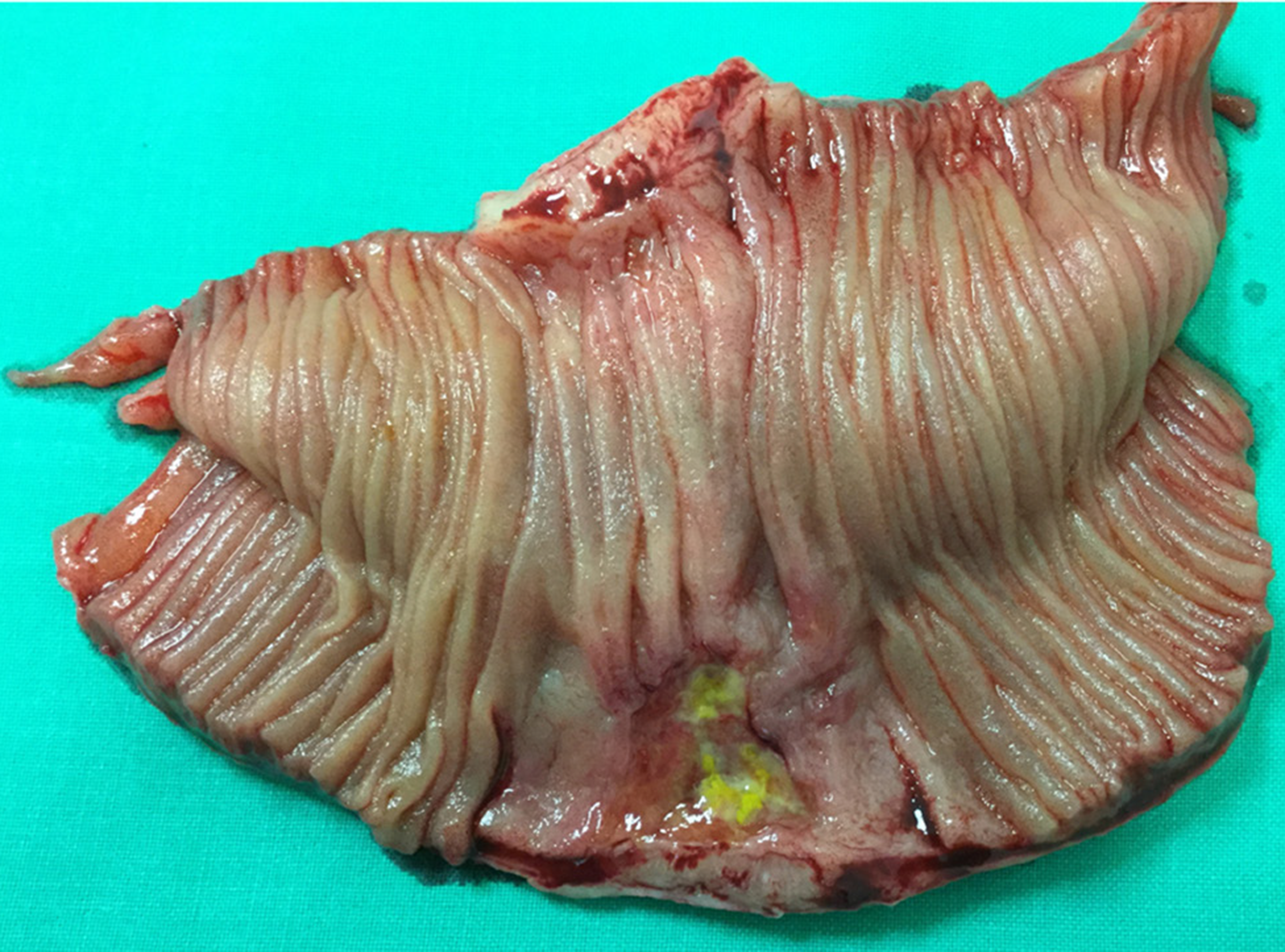
One year later he was hospitalized with nausea, vomiting and severe pain in the upper part of the abdomen. Physical examination revealed peritonitis. Computed tomography (CT) scan showed ileus of the small intestine and extraluminal air within the peritoneal cavity which led to gastrointestinal perforation diagnosis. The patient was scheduled for laparotomy. Intra-operatively, perforation was observed at mesenteric border of a jejunal segment 110 cm from the ligament of Treitz (Figure 5). During laparotomy, 10 centimeters of jejunum with mesentery was resected and abdominal drainage was established (Figure 6). A histopathology examination was performed of a resected brownish tissue fragment, measuring 1.8 cm × 0.7 cm × 0.6 cm.
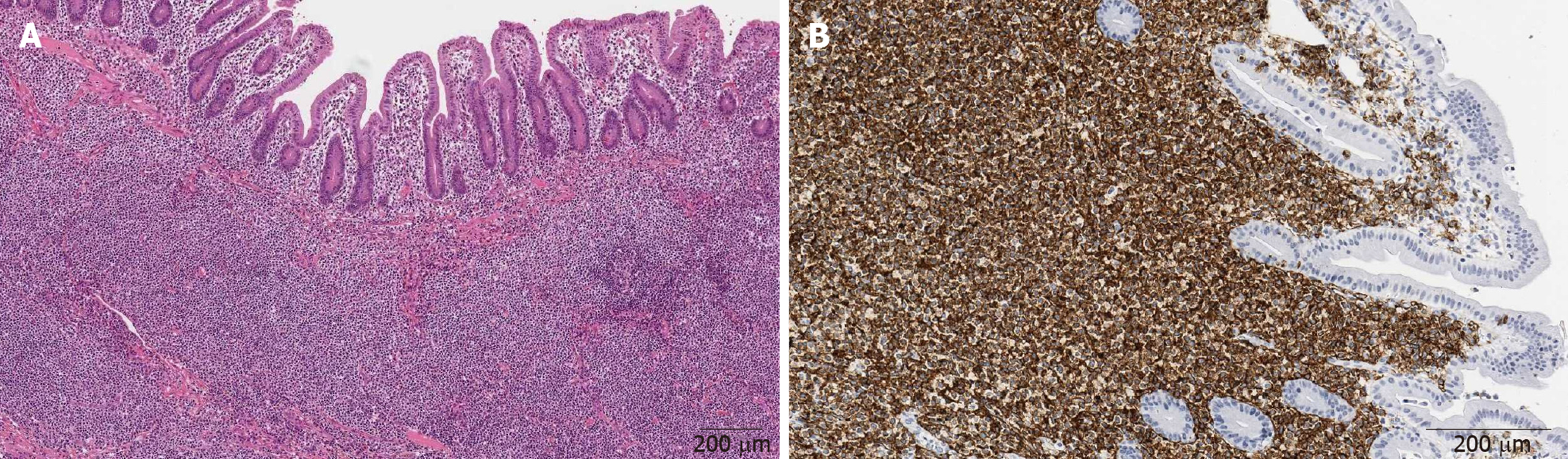
Histology of the postoperative jejunum disclosed jejunal MALT lymphoma, same immunophenotype as the gastric (Figure 7).
Four months later, according to the pathological findings, the patient was treated with a course of R-CHOP (rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone) chemotherapy.
Complete remission was observed following 6 cycles of treatment, as visualized by CT scan.
MALT lymphoma has the highest incidence between 50 and 60 years of age, but its prevalence has been shown to be significantly increased in patients over 40 years old. MALT lymphoma has no specific B-cells immunophenotype or antigenic profile and those circumstances complicate its diagnosis[7]. Gastric MALT lymphoma is most commonly found in the antrum but can also be present in any part of the organ[7].
CD is a chronic inflammatory disorder of the bowel and can occur from mouth to anus in any area of the gastrointestinal tract[11]. While there is no single definitive diagnostic test to confirm the diagnosis of CD, multiple examinations should be performed and should neither be based nor excluded on any one result or test. It is also very important to check a patient’s history of diarrhea, abdominal pain and weight loss. The most widely used diagnostic investigation these days is endoscopy with biopsies[12].
In the presented case, the patient was diagnosed with small bowel CD that occurs in 30% of all CD cases[13]. It is often hard to ensure the right diagnosis of small bowel due to the fact that it is beyond the reach of the gastroscope and colonoscope. Enteroscopy is the main diagnostic test that can provide biopsies and show pathology of the small intestine.
Our patient’s enteroscopy result revealed a 1.5 cm ulcer in the jejunum. Ulceration of small bowel is a symptomatic sign and suggest CD diagnosis but can also be congruent with other diseases, including carcinoma, Henoch-Schonlein purpura, lymphoma and a few others[14]. Primary gastrointestinal lymphomas endoscopically appear as a mass in 49% and only 4% appear as an ulcer. Most of the diffuse large B-cell lymphomas (86%) are mass-like and only 2% are ulcers[15]. MALT lymphoma ulcerative lesions are indistinguishable from CD lesions and this makes the differentiation between these two diseases even harder. The biopsy of our patient revealed lymphoplasmacytic infiltrate, which is a common finding in CD but also can be found in NH lymphomas.
Abdominal ultrasonography showed thickened mucosa and enlarged surrounding lymph nodes in a segment of the small intestine. Bowel wall thickening is also a common finding in both pathologies as well as enlarged lymph nodes. The MRI enterography revealed circumferential infiltration of the proximal part of the ileum. For CD, MRI has a sensitivity of 84% and a specificity of 100%[16] but in this particular report, findings were indistinguishable from lymphoma which made even harder to provide a diagnosis of MALT.
There are few cases of lymphoma mimicking CD in the literature. Koo et al[15] determined a small bowel diffuse large B-cell lymphoma mimicking CD. Capsule endoscopy in this case showed ulcers and lesions in the small bowel[15]. Erkan et al[17] reported the case of the terminal ileum Burkitt’s lymphoma simulating CD, where mesalasin was used to treat the patient. Lymphoma was only diagnosed by hystopathologic examination after patient’s death[17]. McCullough et al[18] described the case of mantle zone lymphoma presented as a diffuse ileocolitis imitating IBD.
It is still under debate if the CD itself increases lymphoma risk compared with the general population. While some studies show that IBD produces a predisposition for the development of lymphoma[19,20], the majority of confirmations support the fact that it does not increase the risk of lymphoma across-the-board[21]. A large study by Lewis et al[22] included nearly 7000 patients from United Kingdom with the diagnosis of CD. The results showed that the risk of lymphoma in these patients is not statistically elevated in a significant manner compared to the control population[22].
Since MALT lymphomas are inherent of inflammation and relying upon a recent understanding of the immune cells participation in the keeping of intestinal homeostasis one can conceive that constant pressure of undesirable representatives of microbiome which attack epithelia can cause a failure to accomplish its regeneration process. This assumption is confirmed by cases of successful H. pylori-associated MALT lymphoma treatment with antibiotics[23].
Taking into account persistent residence of activated immune cells endeavoring to stimulate regeneration of intestinal epithelium and misshapen epithelial-microbiota crosstalk in CD patients, a possibility is available for distortion of immune cell proliferation process in particular portion of such patients. A detailed study of peculiarities of immune cells functions in CD patients can provide clues for the elucidation of B-cell proliferation control deprivation and a better understanding of B-cell lymphoma pathology including MALT lymphomas.
It is necessary to mention the possibility of immunosuppression-related lymphomas in IBD. It is known that immunosuppressive therapy does increase the risk of non-Hodgkin lymphoma[24]. Our patient has been receiving a small dosage azathioprine therapy before being diagnosed with MALT lymphoma. As the analysis of more than 700000 Americans suffering from IBD revealed, treatment with thiopurines is associated with a 4-fold increase of lymphoma[25]. Moreover, the risk of lymphoma rises gradually for successive years of therapy while discontinuing thiopurine therapy reduces the risk in IBD patients. Khan et al[26] stated that the incidence rate of lymphoma during the first year, second year, third year, fourth year, and after 4 years of treatment with thiopurines was 0.9, 1.6, 5, and 8.9 cases per 1000 person-year, respectively[26]. A recent meta-analysis showed an overall standard incidence ratio for lymphoma of 4.92 in IBD patients receiving thiopurines either. It is also noted that risk level after 1 year of exposure became significant[27]. In the presented case, the patient was on azathioprine treatment for 2 years before being diagnosed with MALT lymphoma. Moreover, azathioprine dosage during time increased from 100 mg per day to 150 mg per day.
In our case, abdominal ultrasound, small bowel MRI and enteroscopy showed MALT lymphoma findings mimicking CD. However, the patient was misdiagnosed and received the wrong treatment. Although there are few cases of lymphoma mimicking CD in the literature it is still a very uncommon case. In addition, this case report highlights the clinical relevance of knowledge and awareness of MALT lymphoma simulating CD.
We express gratitude to our workmate gastroenterologist Tomas Jucaitis for the attentive endoscopic procedures performed and to the National Center of Pathology pathologist Dmitrij Seinin for comprehensive biopsy analysis.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: Lithuania
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): E
P-Reviewer: Cho YS, Maehata Y, Sha WH S-Editor: Zhang L L-Editor: A E-Editor: Liu JH
| 1. | Isaacson P, Wright DH. Malignant lymphoma of mucosa-associated lymphoid tissue. A distinctive type of B-cell lymphoma. Cancer. 1983;52:1410-1416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 2. | Sands BE. Crohn’s disease. In: Feldman M, Friedman LS, Sleisenger MH, editors. Sleisenger & Fordtran's Gastrointestinal and Liver Disease. 7th ed. Philadelphia: Saunders, 2002: 2005-2038. |
| 3. | Pimentel AM, Rocha R, Santana GO. Crohn's disease of esophagus, stomach and duodenum. World J Gastrointest Pharmacol Ther. 2019;10:35-49. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 34] [Cited by in RCA: 42] [Article Influence: 7.0] [Reference Citation Analysis (1)] |
| 4. | Terada T. Gastrointestinal malignant lymphoma: a pathologic study of 37 cases in a single Japanese institution. Am J Blood Res. 2012;2:194-200. [PubMed] |
| 5. | Zucca E, Roggero E, Bertoni F, Cavalli F. Primary extranodal non-Hodgkin's lymphomas. Part 1: Gastrointestinal, cutaneous and genitourinary lymphomas. Ann Oncol. 1997;8:727-737. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 240] [Cited by in RCA: 247] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 6. | Zullo A, Hassan C, Ridola L, Repici A, Manta R, Andriani A. Gastric MALT lymphoma: old and new insights. Ann Gastroenterol. 2014;27:27-33. [PubMed] |
| 7. | Violeta Filip P, Cuciureanu D, Sorina Diaconu L, Maria Vladareanu A, Silvia Pop C. MALT lymphoma: epidemiology, clinical diagnosis and treatment. J Med Life. 2018;11:187-193. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 77] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 8. | Zhang TY, Lin Y, Fan R, Hu SR, Cheng MM, Zhang MC, Hong LW, Zhou XL, Wang ZT, Zhong J. Potential model for differential diagnosis between Crohn's disease and primary intestinal lymphoma. World J Gastroenterol. 2016;22:9411-9418. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 15] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (1)] |
| 9. | Dignass A, Van Assche G, Lindsay JO, Lémann M, Söderholm J, Colombel JF, Danese S, D'Hoore A, Gassull M, Gomollón F, Hommes DW, Michetti P, O'Morain C, Oresland T, Windsor A, Stange EF, Travis SP; European Crohn's and Colitis Organisation (ECCO). The second European evidence-based Consensus on the diagnosis and management of Crohn's disease: Current management. J Crohns Colitis. 2010;4:28-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1118] [Cited by in RCA: 1031] [Article Influence: 68.7] [Reference Citation Analysis (1)] |
| 10. | Bautista-Quach MA, Ake CD, Chen M, Wang J. Gastrointestinal lymphomas: Morphology, immunophenotype and molecular features. J Gastrointest Oncol. 2012;3:209-225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 62] [Reference Citation Analysis (0)] |
| 11. | Thia KT, Sandborn WJ, Harmsen WS, Zinsmeister AR, Loftus EV. Risk factors associated with progression to intestinal complications of Crohn's disease in a population-based cohort. Gastroenterology. 2010;139:1147-1155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 481] [Cited by in RCA: 571] [Article Influence: 38.1] [Reference Citation Analysis (0)] |
| 12. | Ha F, Khalil H. Crohn's disease: a clinical update. Therap Adv Gastroenterol. 2015;8:352-359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 62] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 13. | Karnam US, Rosen CM, Raskin JB. Small Bowel Ulcers. Curr Treat Options Gastroenterol. 2001;4:15-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Stange EF, Travis SP, Vermeire S, Beglinger C, Kupcinkas L, Geboes K, Barakauskiene A, Villanacci V, Von Herbay A, Warren BF, Gasche C, Tilg H, Schreiber SW, Schölmerich J, Reinisch W; European Crohn's and Colitis Organisation. European evidence based consensus on the diagnosis and management of Crohn's disease: definitions and diagnosis. Gut. 2006;55 Suppl 1:i1-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 402] [Cited by in RCA: 381] [Article Influence: 20.1] [Reference Citation Analysis (0)] |
| 15. | Koo TH, Choi WJ, Han SH, Kim SY, Lee JH. [A Case of Small Bowel Diffuse Large B-cell Lymphoma Mimicking Crohn's Disease]. Korean J Gastroenterol. 2015;65:241-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | Laghi A, Borrelli O, Paolantonio P, Dito L, Buena de Mesquita M, Falconieri P, Passariello R, Cucchiara S. Contrast enhanced magnetic resonance imaging of the terminal ileum in children with Crohn's disease. Gut. 2003;52:393-397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 147] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 17. | Erkan G, Coban M, Calıskan A, Ataç GK, Gulpınar K, Degertekin B, Korkmaz A. A Burkitt's Lymphoma Case Mimicking Crohn's Disease: A Case Report. Case Rep Med. 2011;2011:685273. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 18. | McCullough JE, Kim CH, Banks PM. Mantle zone lymphoma of the colon simulating diffuse inflammatory bowel disease. Role of immunohistochemistry in establishing the diagnosis. Dig Dis Sci. 1992;37:934-938. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 19. | Hu Q, Zhang Y, Zhang X, Fu K. Gastric mucosa-associated lymphoid tissue lymphoma and Helicobacter pylori infection: a review of current diagnosis and management. Biomark Res. 2016;4:15. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 24] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 20. | Maclaurin BP, Cooke WT, Ling NR. Impaired lymphocyte reactivity against tumour cells in patients with Crohn's disease. Gut. 1972;13:614-620. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 21. | von Roon AC, Reese G, Teare J, Constantinides V, Darzi AW, Tekkis PP. The risk of cancer in patients with Crohn's disease. Dis Colon Rectum. 2007;50:839-855. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 214] [Cited by in RCA: 211] [Article Influence: 11.7] [Reference Citation Analysis (1)] |
| 22. | Lewis JD, Bilker WB, Brensinger C, Deren JJ, Vaughn DJ, Strom BL. Inflammatory bowel disease is not associated with an increased risk of lymphoma. Gastroenterology. 2001;121:1080-1087. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 226] [Cited by in RCA: 221] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 23. | Thieblemont C, Zucca E. Clinical aspects and therapy of gastrointestinal MALT lymphoma. Best Pract Res Clin Haematol. 2017;30:109-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 40] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 24. | Ujjani CS, Cohen P. An Association between Hodgkin's Lymphoma and Crohn's Disease: A Case Series. Blood. 2014;124:1611. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (2)] |
| 25. | Rawla P, Sunkara T, Raj JP. Role of biologics and biosimilars in inflammatory bowel disease: current trends and future perspectives. J Inflamm Res. 2018;11:215-226. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 81] [Cited by in RCA: 105] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 26. | Khan N, Abbas AM, Lichtenstein GR, Loftus EV, Bazzano LA. Risk of lymphoma in patients with ulcerative colitis treated with thiopurines: a nationwide retrospective cohort study. Gastroenterology. 2013;145:1007-1015.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 166] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 27. | Kotlyar DS, Lewis JD, Beaugerie L, Tierney A, Brensinger CM, Gisbert JP, Loftus EV, Peyrin-Biroulet L, Blonski WC, Van Domselaar M, Chaparro M, Sandilya S, Bewtra M, Beigel F, Biancone L, Lichtenstein GR. Risk of lymphoma in patients with inflammatory bowel disease treated with azathioprine and 6-mercaptopurine: a meta-analysis. Clin Gastroenterol Hepatol. 2015;13:847-858.e4; quiz e48-e50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 254] [Cited by in RCA: 278] [Article Influence: 27.8] [Reference Citation Analysis (0)] |