Published online Apr 6, 2020. doi: 10.12998/wjcc.v8.i7.1295
Peer-review started: December 10, 2019
First decision: October 25, 2019
Revised: March 6, 2020
Accepted: March 27, 2020
Article in press: March 27, 2020
Published online: April 6, 2020
Processing time: 117 Days and 18.8 Hours
Pulmonary cryptococcosis is an opportunistic infection that mainly occurs among immunocompromised patients although it can sometimes occur in immunocompetent individuals. However, the imaging findings of pulmonary cryptococcosis in immunocompetent hosts differ from those in immunosuppressed patients. In addition, the most common imaging findings of isolated pulmonary cryptococcosis are single or multiple nodules. Cavities and the halo sign are, however, prevalent in immunosuppressed patients. In immunocompetent patients, lung consolidation, pleural effusion or cavities are scarce.
A 29-year-old Asian male was admitted to our hospital with complaints of cough and fever that had persisted for a month. As a chest computed tomography scan showed consolidation in his left lower lobe, he was initially diagnosed with pneumonia and received antibiotic treatment. A second review of the chest computed tomography image revealed multiple cavities and pleural effusion. Flexible fiberoptic bronchoscopy was subsequently performed, bronchoalveolar lavage fluid and serum cryptococcal antigen tests were positive. Cryptococcus capsules were observed in bronchoalveolar lavage fluid ink stain. Histopathological examination of a percutaneous lung biopsy from the left lower lobe further revealed granulomatous inflammation, and periodic acid-Schiff staining showed red-colored yeast walls, signifying pulmonary cryptococcosis. The patient was then treated with a daily dose of fluconazole (0.4 g), but the cough and fever still persisted. We therefore changed treatment to voriconazole (0.2 g, twice a day), and the patient’s clinical outcome was satisfactory.
Although rare, clinicians should not disregard the possibility of cavities and pleural effusion occurring in immunocompetent hosts without underlying diseases.
Core tip: The most common imaging findings of isolated pulmonary cryptococcosis are single or multiple nodules located in the peripheral lung field. Cavities and pleural effusion are scarce in immunocompetent patients. In this study, we report a case of isolated cryptococcal pneumonia in an immunocompetent patient without underlying diseases, but exhibiting rare radiologic findings of pleural effusion and cavities. Although rare, clinicians should not disregard the possibility of cavities and pleural effusion occurring in immunocompetent hosts without underlying diseases.
- Citation: Wu HH, Chen YX, Fang SY. Pleural effusion in an immunocompetent host with cryptococcal pneumonia: A case report. World J Clin Cases 2020; 8(7): 1295-1300
- URL: https://www.wjgnet.com/2307-8960/full/v8/i7/1295.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i7.1295
Cryptococcosis mainly occurs as a result of inhalation of fungal spores in the environment. It has been reported that approximately 35% of patients with pulmonary cryptococcosis are immunocompetent[1]. The imaging manifestations of pulmonary cryptococcosis vary considerably, depending on the immune status of the host. Most radiologic findings of pulmonary cryptococcosis in immunocompetent patients exhibit single or multiple peripheral nodule or masses, and localized pneumonia-like lesions[2,3]. Nodular and masses with burrs and lobes can easily be misdiagnosed as lung cancer. Most of these lesions are located in the peripheral lung field, usually subpleural within the inferior lobes, often in the right lower lobe. However, immunocompromised patients have more extensive and varied imaging findings. Besides nodular and mass lesions, diffuse, disseminated pneumonia-like infiltration and consolidation are common, leading to the formation of cavities and the halo sign[4]. Other changes on imaging include grid infiltration, hilar and mediastinal lymphadenopathy, pleural effusion, diffuse miliary shadows, and ground-glass opacity. In such cases, the diagnosis of pulmonary cryptococcosis becomes very challenging; therefore, invasive examination is occasionally conducted to confirm the diagnosis.
A 29-year-old Asian male was admitted to our emergency department after complaining of cough and fever that had persisted for a month.
The patient’s symptoms started a month ago with cough and fever. At a local hospital, he underwent a chest computed tomography (CT) scan and oral antibiotics (unknown); however, his cough and fever were not relieved.
His history of past illness was negative.
Physical examination revealed crackle in the left lower lobe. Neurological examination was normal. On admission, he had a pulse of 106 beats/min, blood pressure of 130/70 mmHg, and a body temperature of 38.2ºC. According to the patient’s chest CT scan result, it was thought that he might have bacterial pneumonia and was prescribed cefoperazone as empirical treatment.
Laboratory data, including white blood cell count, platelet count, renal and liver function, C-reactive protein, procalcitonin, and tumor markers, were all considered normal. Moreover, his human immunodeficiency virus (HIV) serology was negative and CD4 count was normal.
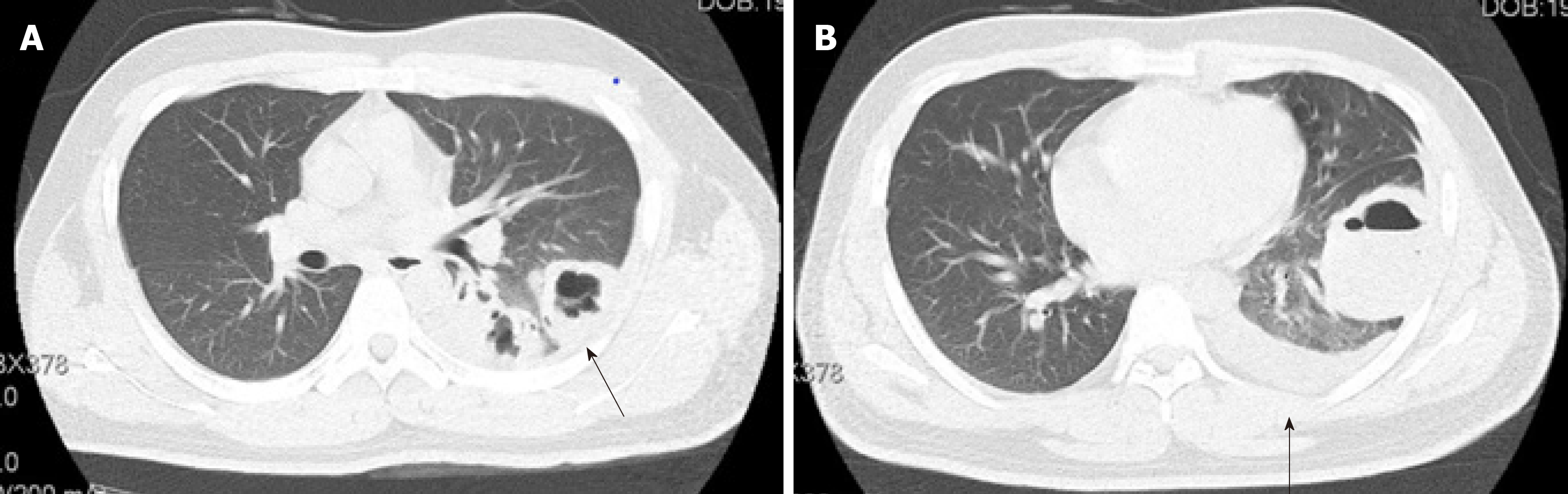
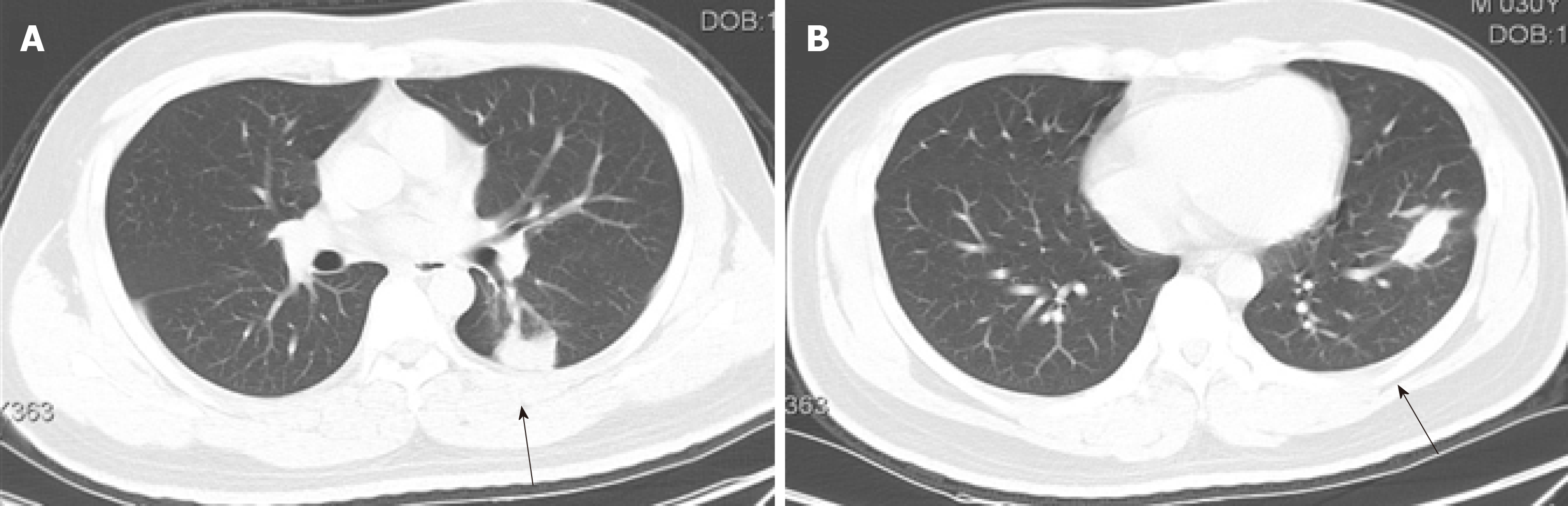
After a week of antibiotic therapy, his cough and fever still persisted, with additional chest pain. Therefore, he underwent another CT scan to evaluate the therapeutic effects. We observed that the lesions revealed in the previous CT scan had not resolved, and multiple cavities and pleural effusion were also visible (Figure 1), prompting another diagnosis.
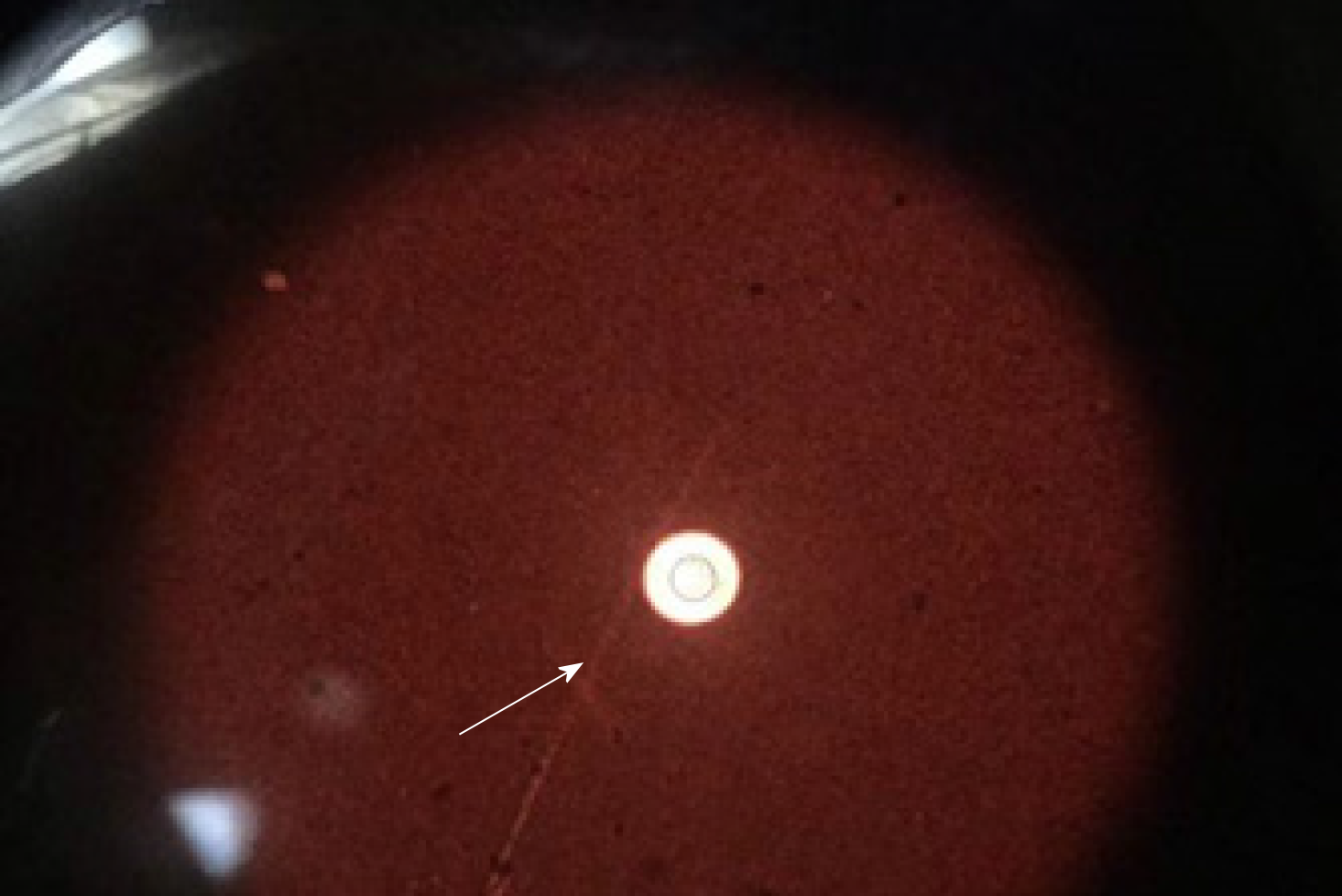
A tuberculosis infection T-cell spot test (T-SPOT.TB; Oxford Immunotec, Marlborough, MA, United States) was then performed, but yielded negative results. Flexible fiberoptic bronchoscopy was subsequently performed. Bronchoalveolar lavage fluid (BAL) and serum cryptococcal antigen (CrAg) testing were positive for cryptococcosis. Cryptococcus capsules were observed on BAL ink stain (Figure 2). Furthermore, histopathological examination of a percutaneous lung biopsy from the left lower lobe revealed granulomatous inflammation, and periodic acid-Schiff staining showed red-colored yeast walls.
According to the pathology and BAL ink stain, the diagnosis of pulmonary cryptococcosis was confirmed.
The patient was then treated with a daily dose of fluconazole (0.4 g), but exhibited unsatisfactory clinical outcome as cough and mild fever persisted, a week later. Therefore, the anti-fungal treatment was changed from fluconazole to voriconazole (0.2 g, twice a day)[5,6].
After 8 months of antifungal therapy, his cough and fever improved. A repeated chest CT scan showed significant absorption of the lesion. In addition, no recurrence was observed after follow-up (Figure 3).
As mentioned above, approximately 35% of patients with pulmonary cryptococcosis are immunocompetent, and there are also reports to show that more than 50% of patients with pulmonary cryptococcosis are immunocompetent[2,7]. In addition, approximately 60% of patients with HIV-negative pulmonary cryptococcosis do not have underlying disease[4]. The imaging findings of pulmonary cryptococcosis are often related to the patient's immune status. Liu et al[4] summarized the imaging findings of 88 patients with pulmonary cryptococcosis, and found that poorly-defined nodules, cavity, and the halo-sign were more frequent in immunosuppressed patients than in immunocompetent patients. Solitary and well-defined nodules were more common in patients with normal immune function. Zhang et al[2] summarized the imaging findings of 76 patients with pulmonary cryptococcosis, and found that pneumonia-like manifestations were more common in immunocompetent patients than in immunocompromised patients. Regardless of whether the patient’s immune function was impaired, the most prevalent imaging findings in both immuno-competent and immunocompromised patients are nodules or masses located mainly in the peripheral lung field (outer third of the lung), and close to the pleura[8]. In this study, we observed that missed diagnosis or misdiagnosis of pulmonary cryptococcosis was highly likely as its CT images mimicked lung cancer, tuberculosis, and bacterial infection.
Testing for CrAg in serum and cerebrospinal fluid is an important diagnostic procedure for the detection of cryptococcosis. Although this non-invasive procedure has been reported to be sensitive, contrary reports have emerged showing that its sensitivity is insufficient in the diagnosis of isolated pulmonary cryptococcosis. A study reported that only 56% of patients with non-HIV related isolated pulmonary cryptococcosis tested positive for serum CrAg[9]. Another recent study of 23 non-HIV related pulmonary cryptococcosis patients showed that the positive rate of CrAg testing in BAL was 82.6%, which was higher than the serum positive rate[10]. In this study, we also found BAL CrAg testing to be more sensitive. Therefore, BAL CrAg detection can be used as an adjunctive diagnostic tool for patients with pulmonary cryptococcosis.
Fluconazole is the preferred drug for treating cryptococcosis that has not spread to the central nervous system. This antifungal therapy prevents or diminishes the risk of disease progression. However, increasing fluconazole resistance in Cryptococcus is a major drawback to this mode of treatment. For example, a recent study revealed fluconazole resistance of 10.6% in 4995 Cryptococcus isolates from HIV-positive patients[11], with the resistance rate set to increase over time. In cases where fluconazole is not available or contraindicated, oral voriconazole (200 mg twice a day) has been proposed as a suitable substitute[12]. Unlike after fluconazole therapy, we observed a significant improvement in the patient's lung lesions after voriconazole treatment.
Pulmonary cryptococcosis also affects immunocompetent patients, and its clinical outcome is always satisfactory if the disease is diagnosed and treated early. Therefore, if a patient has a relatively slow progression of lesions, as well as a poor response to antibiotics, without the signs of inflammation caused by tuberculosis and lung cancer, then the possibility of pulmonary cryptococcosis should be considered. Clinicians should not disregard the possibility of cavities and pleural effusion occurring in immunocompetent hosts without underlying diseases.
Manuscript source: Unsolicited Manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Boots RJ, Surani SR S-Editor: Ma YJ L-Editor: Webster JR E-Editor: Xing YX
| 1. | Aberg JA, Mundy LM, Powderly WG. Pulmonary cryptococcosis in patients without HIV infection. Chest. 1999;115:734-740. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 121] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 2. | Zhang Y, Li N, Zhang Y, Li H, Chen X, Wang S, Zhang X, Zhang R, Xu J, Shi J, Yung RC. Clinical analysis of 76 patients pathologically diagnosed with pulmonary cryptococcosis. Eur Respir J. 2012;40:1191-1200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 81] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 3. | Kohno S, Kakeya H, Izumikawa K, Miyazaki T, Yamamoto Y, Yanagihara K, Mitsutake K, Miyazaki Y, Maesaki S, Yasuoka A, Tashiro T, Mine M, Uetani M, Ashizawa K. Clinical features of pulmonary cryptococcosis in non-HIV patients in Japan. J Infect Chemother. 2015;21:23-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 56] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 4. | Liu K, Ding H, Xu B, You R, Xing Z, Chen J, Lin Q, Qu J. Clinical analysis of non-AIDS patients pathologically diagnosed with pulmonary cryptococcosis. J Thorac Dis. 2016;8:2813-2821. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 53] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 5. | Perfect JR, Dismukes WE, Dromer F, Goldman DL, Graybill JR, Hamill RJ, Harrison TS, Larsen RA, Lortholary O, Nguyen MH, Pappas PG, Powderly WG, Singh N, Sobel JD, Sorrell TC. Clinical practice guidelines for the management of cryptococcal disease: 2010 update by the infectious diseases society of america. Clin Infect Dis. 2010;50:291-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1988] [Cited by in RCA: 1797] [Article Influence: 119.8] [Reference Citation Analysis (0)] |
| 6. | Editorial Board of Chinese Journal of Mycology. Chinese expert consensus statement on management of cryptococcal infection. Zhonguo Zhenjun Xue Zazhi. 2010;5: 65-68. [DOI] [Full Text] |
| 7. | Ye F, Xie JX, Zeng QS, Chen GQ, Zhong SQ, Zhong NS. Retrospective analysis of 76 immunocompetent patients with primary pulmonary cryptococcosis. Lung. 2012;190:339-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 44] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 8. | Fisher JF, Valencia-Rey PA, Davis WB. Pulmonary Cryptococcosis in the Immunocompetent Patient-Many Questions, Some Answers. Open Forum Infect Dis. 2016;3:ofw167. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 40] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 9. | Pappas PG, Perfect JR, Cloud GA, Larsen RA, Pankey GA, Lancaster DJ, Henderson H, Kauffman CA, Haas DW, Saccente M, Hamill RJ, Holloway MS, Warren RM, Dismukes WE. Cryptococcosis in human immunodeficiency virus-negative patients in the era of effective azole therapy. Clin Infect Dis. 2001;33:690-699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 446] [Cited by in RCA: 434] [Article Influence: 18.1] [Reference Citation Analysis (0)] |
| 10. | Oshima K, Takazono T, Saijo T, Tashiro M, Kurihara S, Yamamoto K, Imamura Y, Miyazaki T, Tsukamoto M, Yanagihara K, Mukae H, Kohno S, Izumikawa K. Examination of cryptococcal glucuronoxylomannan antigen in bronchoalveolar lavage fluid for diagnosing pulmonary cryptococcosis in HIV-negative patients. Med Mycol. 2018;56:88-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 11. | Bongomin F, Oladele RO, Gago S, Moore CB, Richardson MD. A systematic review of fluconazole resistance in clinical isolates of Cryptococcus species. Mycoses. 2018;61:290-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 115] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 12. | Limper AH, Knox KS, Sarosi GA, Ampel NM, Bennett JE, Catanzaro A, Davies SF, Dismukes WE, Hage CA, Marr KA, Mody CH, Perfect JR, Stevens DA; American Thoracic Society Fungal Working Group. An official American Thoracic Society statement: Treatment of fungal infections in adult pulmonary and critical care patients. Am J Respir Crit Care Med. 2011;183:96-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 363] [Cited by in RCA: 392] [Article Influence: 28.0] [Reference Citation Analysis (0)] |