Published online Mar 6, 2020. doi: 10.12998/wjcc.v8.i5.939
Peer-review started: October 9, 2019
First decision: January 7, 2020
Revised: February 3, 2020
Accepted: February 12, 2020
Article in press: February 12, 2020
Published online: March 6, 2020
Processing time: 148 Days and 17.7 Hours
Dedifferentiated liposarcoma in the mediastinum is an extremely rare malignant neoplasm. A few previous case reports indicate that surgical resection is the major treatment, but frequent recurrence occurs locally. Due to its rarity, its clinical characteristics, optimal treatment and clinical outcomes remain unclear. Here, we report a case of multifocal recurrent dedifferentiated liposarcoma in the posterior mediastinum treated by combining surgery with 125I brachytherapy, and summarize its clinical features, treatment and prognosis.
A 75-year-old man was admitted to our hospital with a history of gradual dysphagia for one year and aggravated dysphagia for 3 mo. Contrast-enhanced computed tomography (CT) revealed several large cystic-solid masses with lipomatous density, and calcification in the posterior-inferior mediastinum. The patient received a wide excision by video-assisted thoracoscopic surgery. Pathological analysis confirmed the tumors were dedifferentiated liposarcomas. The tumor locally relapsed 24 mo later, and another operation was performed by video-assisted thoracoscopic surgery. Fifteen months after the second surgery, the tumor recurred again, and the patient received CT-guided radioactive seeds 125I implantation. After 8 mo, follow-up chest CT showed an enlarged tumor. Finally, his condition exacerbated with severe dysphagia and dyspnea, and he died of respiratory failure in July 2018.
We reviewed the literature, and suggest that surgical resection provides beneficial effects for dedifferentiated liposarcoma in the mediastinum, even in cases with local recurrence. 125I brachytherapy may be beneficial for recurrent unresectable patients.
Core tip: Dedifferentiated liposarcoma in the mediastinum is an extremely rare malignant neoplasm. Only a few cases have been reported, and its clinical characteristics, optimal treatment and clinical outcomes remain unclear. Here, we report a male patient with recurrent mediastinal dedifferentiated liposarcoma that was successfully treated by surgery combined with 125I brachytherapy. A review of the literature is also provided to improve the overall awareness of this disease. To our knowledge, this literature review covers the largest number of cases as any prior, and is the first report on dedifferentiated liposarcomas treated by 125I brachytherapy.
- Citation: Chen HG, Zhang K, Wu WB, Wu YH, Zhang J, Gu LJ, Li XJ. Combining surgery with 125I brachytherapy for recurrent mediastinal dedifferentiated liposarcoma: A case report and review of literature. World J Clin Cases 2020; 8(5): 939-945
- URL: https://www.wjgnet.com/2307-8960/full/v8/i5/939.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i5.939
Liposarcoma is a malignant adipocytic neoplasm with varying degrees of atypia. According to the 2019 NCCN classification, liposarcoma has been classified into four types: Well-differentiated, myxoid, pleomorphic, and dedifferentiated. Dedifferentiated liposarcoma is a common form of liposarcoma, accounting for the most pleomorphic sarcoma in the retroperitoneum[1], but rarely occurs in the mediastium, and the exact frequency is unknown[2]. Thus far, limited cases of mediastinal dedifferentiated liposarcoma have been reported, and its clinical characteristics, optimal treatment and clinical outcomes remain unclear.
The present study reports a case of primary multifocal recurrent dedifferentiated liposarcomas in the posterior mediastinum treated by combining surgery with 125I brachytherapy following recurrence. In addition, 38 cases of primary mediastinal dedifferentiated liposarcoma from the English literature are reviewed to illustrate the clinical characteristics, treatment and outcomes of the disease. To our knowledge, our literature review covers the largest number of cases compared to any prior reviews, and is the first report of dedifferentiated liposarcomas treated by 125I brachytherapy.
Progressive dysphagia for one year.
A 75-year-old male was admitted in December 2013 due to gradually progressive dysphagia, and the symptoms became more aggravated 3 mo before admission. He had no chest pain, acid reflux or weight loss.
Atrial fibrillation had been diagnosed eight years prior, but had been left untreated. There was no history of trauma, thoracic disease, thoracic surgery or abdominal disease.
No remarkable abnormality was found upon physical examination, with the exception of atrial fibrillation with a heart rate of approximately 80 beats per minute.
Tumor markers were in the normal range, including α-fetoprotein, carcinoembryonic antigen, β-human chorionic gonadotropin, cytokeratin 19-fragments (CYFRA21-1), neuron specific enolase, cancer antigens 19-9 and squamous cell carcinoma antigen.
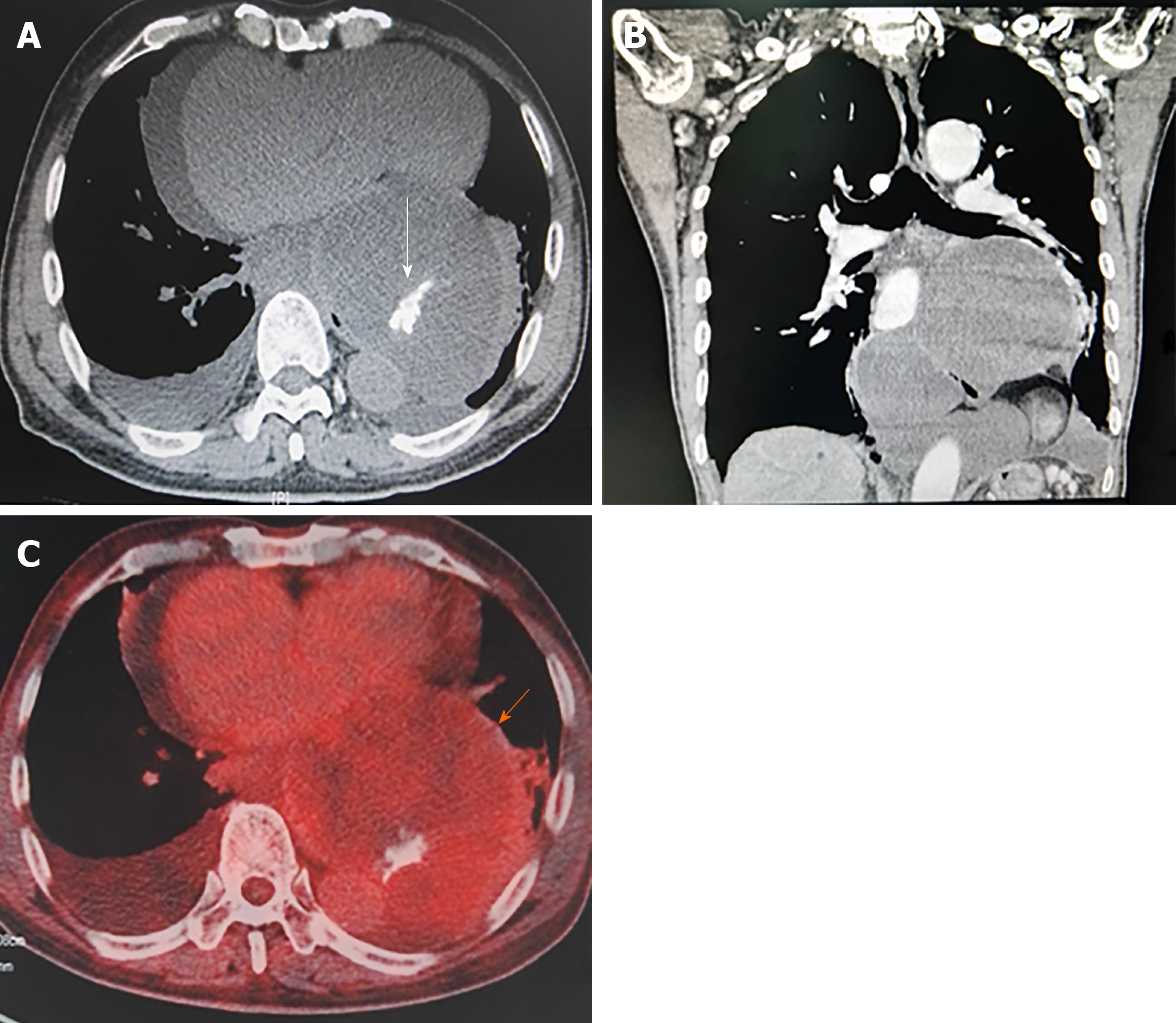
Chest contrast-enhance computed tomography (CT) revealed several large cystic-solid masses that compressed the left atrium, left ventricular and esophagus in the posterior-inferior mediastinum. The largest mass was about 10.5 cm × 9 cm in size and had three attenuation components, namely a lipomatous element, a soft tissue density component and a high attenuation calcified area (Figure 1A and B). The other masses had only two attenuation components without calcification. All of the masses had a relatively distinct margin, and the CT value was 19 HU. A small amount of pericardial effusion and bilateral pleural effusion were present. No obvious enhancement was found in any of the stages after enhancement, and no obviously enlarged lymph nodes were found. The 18F-fluorodeoxyglucose positron emission tomography (PET) showed an maximum standardized uptake value (SUVmax) of 1.8 (Figure 1C) and no metastasis. Esophageal dynamic radiography and fibergastroscopy showed that the lower esophagus was significantly compressed. No obvious changes were observed on the mucosal surface of the esophagus, and no tumorous lesion was seen.
Teratoma in the posterior mediastinum.
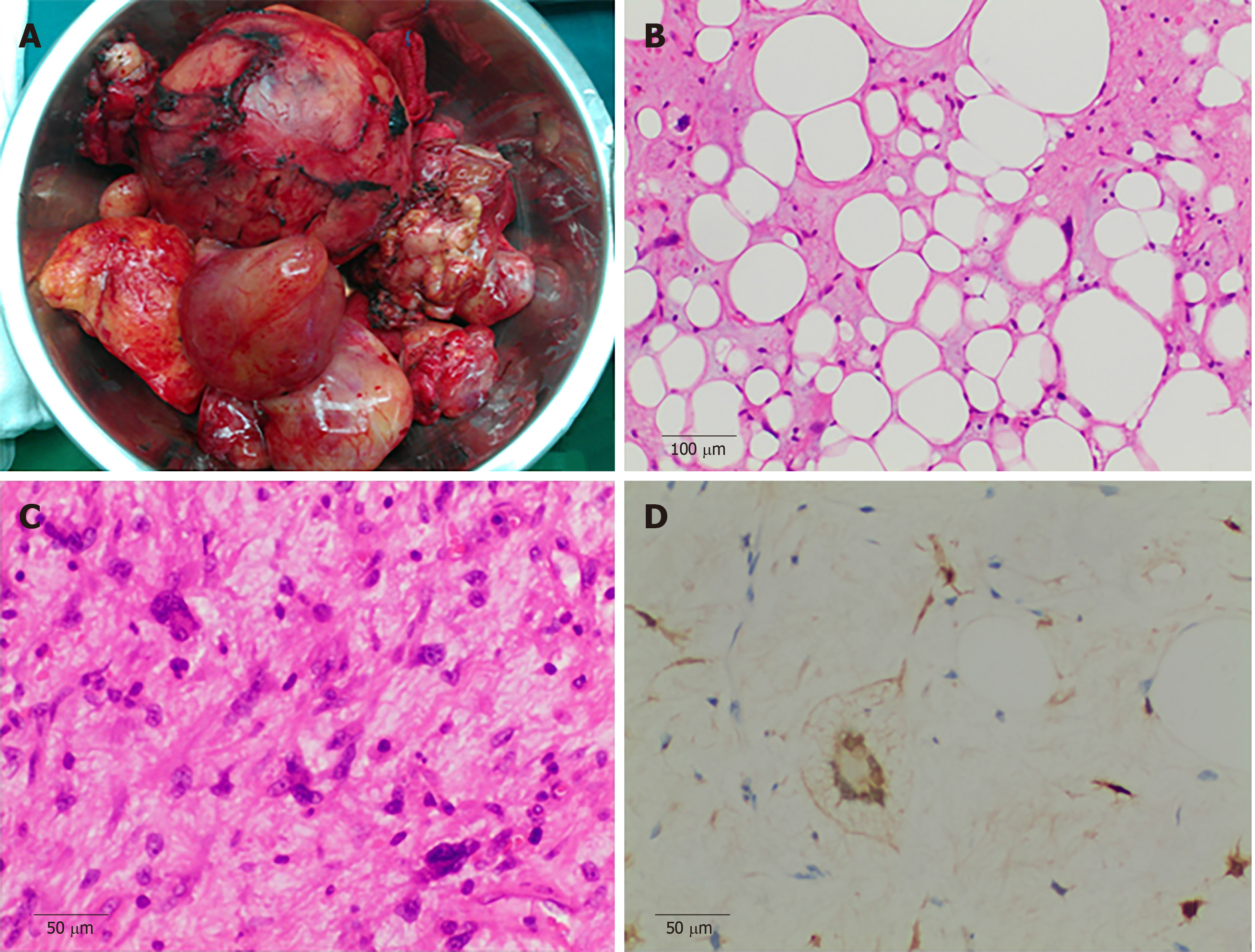
Grossly, all tumors had an integrated capsule, and there was some adipose tissues between adjacent tumors (Figure 2A). Within the tumor, the cut interface presented as variegated tan-yellow to brown, and had a partial myxoid appearance. Haematoxylin and eosin staining showed proliferating fat cells and well-differentiated liposarcoma, as well as spindle cell sarcoma with spindle nuclei and nuclear fission (Figure 2B and C). Immunohistochemical analysis showed that the tumor was positive for vimentin, S100 (Figure 2D), CD34, CD68 (diffused), and Desmin (partial), but negative for SMA, and the ki-67 index was 5%. Finally, a diagnosis of dedifferentiated liposarcoma was made.
The patient immediately underwent wide excision by video-assisted thoracoscopic surgery, with a small incision (8 cm) made in the right thoracic cavity. The tumors presented as encapsulated and smooth, and occupied a large part of the left pleural cavity. There were mild adhesions, with fat tissue between tumors and lung, esophagus, descending aorta, left atrium, and left ventricular, but no direct invasion. Finally, a total of eight tumors were resected completely. The largest tumor was about 10.5 cm × 9 cm × 8.9 cm in size, and the smallest one was about 2 cm in diameter (Figure 2A).
The postoperative course was uneventful. The patient rejected adjuvant therapy, and chest CT was performed at a 6-mo interval for follow-up. The patient suffered from slight dysphagia again for 24 mo after the operation. Contrast-enhanced CT showed a mass (about 5 cm in diameter) in the posterior-inferior mediastinum-compressed esophagus, and the patient underwent re-operation by video-assisted thoracoscopic surgery. A total of five tumors were resected. Pathological analysis confirmed the diagnosis of dedifferentiated liposarcoma. The patient still rejected postoperative adjuvant chemotherapy or radiotherapy. Unfortunately, the chest CT showed tumor recurrence 15 mo after the re-operation. The condition of the disease was explained to the patient and his family, and the patient rejected repeat surgery and received CT-guided radioactive seeds 125I implantation in another hospital. After 8 mo, follow-up chest CT showed an enlarged tumor. Finally, the patient rejected any treatment, and died from severe dysphagia and respiratory failure in July 2018.
Dedifferentiated liposarcoma is one type of liposarcoma that was first described by Evans in 1979[3]. According to the World Health Organization, dedifferentiated liposarcoma is a malignant adipocytic neoplasm showing a transition from atypical lipomatous tumor/well-differentiated liposarcoma to non-lipogenic sarcoma of variable histological grade[1]. Dedifferentiated liposarcoma most commonly occurs in the retroperitoneum, followed by extremities, and scrotum/spermatic cord, but its origin in the mediastinum is extremely rare[4].
The present study reviewed the English literature in PubMed between 1950 and 2018 using the keywords: Dedifferentiated/de-differentiated, liposarcoma, mediastinum or mediastinal, and identified 39 cases of primary mediastinal dedifferentiated liposarcoma, including this case[2,5-24]. In these cases, the tumors all occurred in adults, and the mean patient age was 62.9 years, with an age range of 34 years to 83 years, and a predilection for males (26 males and 13 females). Of the 39 cases, 24 were reported in American and European populations, and 15 cases in Asian populations. There were 24 cases describing symptom details: Sixteen with some symptoms and eight without symptoms. The common complaints included dyspnea (nine cases), cough (five cases), and dysphagia (five cases). The other symptoms included weight loss, hoarseness, chest pain and arm weakness. The tumor most frequently occurred in the anterior and posterior mediastinum (15 cases respectively), followed by the middle (three cases), and the anterior-middle mediastinum (one case). The tumor size varied from 6 cm to 61 cm. The mean size of the tumor was 18.5 cm, and only five cases exhibited a tumor of < 10 cm, meanwhile ten cases were > 20 cm in diameter. The mean SUVmax of the tumor was 3.7 in seven cases (range 1.8 to 9.2), and four cases exhibited < 2.5. Only four cases had reported tumor invasion of the surrounding structures, including pleura, pericardium and the phrenic nerve. Distant metastasis only occurred in four cases, and common metastasis occurred in the lung and pleura.
In terms of initial management, 30 patients underwent complete surgical resection, three patients received incomplete surgical resection, two patients received chemotherapy, one patient received neoadjuvant chemotherapy and three patients were unknown. Of the 34 surgical cases, three patients received adjuvant therapy after surgery (two for chemotherapy and one for radiotherapy). Unfortunately, the tumor recurred in 13 cases (13/34, 38.2%), and nine cases were further treated by repeat surgery, while the other patients received chemotherapy (one case), chemoradiotherapy (one case), and radiotherapy (one case). Six cases of repeat surgical patients were reported with the second relapse (6/9, 66.7%). The mean time of recurrence-free survival (RFS) was 24.5 mo for the first relapse (range 5 mo to 50 mo) and was 35.8 mo for the second relapse (range 8 mo to 96 mo). Median RFS was 24 mo for the first relapse and 14.5 mo for the second relapse. Of the 39 total patients, 21 cases were alive with no evidence of disease, five cases were alive with the disease, seven cases were dead (five cases dead of disease and two cases dead of other disease) and six cases were lost to follow-up. The longest survival time was 114 mo.
Since the first case reported by Evans et al[22] in 1994, surgical resection was usually utilized in the management of mediastial dedifferentiated liposarcoma. Based on previous reports, complete resection is the optimal method to eradicate the tumor[2,5-9,11-21,23,24]. Hahn et al[21] reported six cases of mediastinal dedifferentiated liposarcoma treated by complete resection, and three cases of them had a disease-free survival (DFS) of more than 50 mo. Recently, Miura et al[2] reported five cases of mediastinal dedifferentiated liposarcoma, and reviewed 14 cases in the literature. They performed complete surgical resection in four patients, and claimed that complete surgical resection is the best treatment for mediastinal dedifferentiated liposarcoma. In our report, the patient underwent complete surgical resection and had an RFS of 24 mo. Although mediastinal dedifferentiated liposarcoma usually grows to be very large, the growth pattern tends to be of the expansive type rather than infiltrative type, and metastasis rarely occurs. Of the 39 cases, only one case showed metastasis and four cases had invaded surrounding structures at the time of the first visit. These conditions are conducive to complete surgical resection. However, 13 of 32 patients with complete resection developed local recurrence in the mediastinum, and it appeared that the tumor tended to recur after surgery. Although there was loose connective tissue between the tumor and surrounding structure, and the tumor did not invade surrounding organs, it is difficult to completely resect all of the fat tissue in the mediastinum. In addition, atypical cells were found in the peripheral fat tissue[2]. These may explain the predisposition for recurrence. Fortunately, according to the literature review, repeat surgery is still valid for patients with recurrence, with a median RFS of 14.5 mo in seven cases of secondary relapse. Thus, despite a high risk of recurrence, we conclude that a complete resection is the best method to cure the tumor, even in patients with local recurrence.
As discussed above, repeat surgery is still valid for patients with recurrent mediastial dedifferentiated liposarcoma, but some patients refused repeat surgery or were unsuitable for repeat surgery. External radiotherapy is an optional strategy used to treat these patients. Miura et al[2] reported a patient with recurrent mediastial dedifferentiated liposarcoma who was treated by radiotherapy, and the disease was well-controlled. Coulibaly et al[19] reported a case of recurrent dedifferentiated liposarcoma of the mediastinum treated by repeat surgery combined with adjuvant radiotherapy (60 Gy), and the patient had an RFS of 8 years. However, an adequate therapeutic dose of radiotherapy to the mediastinal tumor may damage the important adjacent organs, including lung, esophagus and heart, which are often radiosensitive and have a low radiation tolerance. 125I brachytherapy can deliver a large total radiotherapy dose to the target tumor and overcome these problems. Radioactive seeds 125I implantation was widely used in advanced hepatic carcinoma and soft tissue sarcoma with good outcomes[25,26]. Yang et al[25] reported CT-guided 125I seed implantation for inoperable retroperitoneal, including eight cases of liposacoma, and good local control was achieved. We consider 125I brachytherapy to be effective because its application to locally recurrent tumors was effective in this case, with a PFS of 8 mo, although its efficacy has not been confirmed in dedifferentiated liposarcoma. To our knowledge, this is the first attempt to treat mediastinal dedifferentiated liposarcoma by CT-guided 125I seed implantation. This approach needs to be further explored by large sample studies.
Due to its rarity, with only a few case reports, the long-term prognosis of mediastinal dedifferentiated liposarcoma is not clear. Coulibaly et al[19] reported a patient with mediasinal dedifferentiated liposarcoma, who underwent complete surgery with a DFS of 15 mo. The patient received repeat surgery and adjuvant radiotherapy with a DFS of 96 mo, and died 3 mo later. The survival time of the patient was 114 mo. This is the longest survival time in the literature. Hahn et al[21] studied 24 cases of mediastinal liposarcoma, including eight cases of dedifferentiated liposarcoma. In the last follow-up, four patients were alive with no evidence of disease with a median DFS of 51.5 mo, and one patient died of unrelated disease with a survival time of 5 mo. In this study, of the 39 cases, there were 21 cases alive with no evidence of disease with a mean DFS of 29.8 mo, and five patients died of the disease with a mean survival time of 42.3 mo. However, as mentioned above, local recurrence was common, with 13 (13/39, 33.3%) cases developing recurrent tumors after a mean interval of 24.5 mo. The mean tumor size of ten patients with recurrence was 24.5 ± 17.3 cm, and that of 16 patients without recurrence was 17.1 ± 9.6 cm. The difference was statistically significant between the two groups. According to our literature review, we speculated tumor size to be one of the risk factors for tumor recurrence, whereas gender, tumor location and symptoms are not. Therefore, we speculate that complete surgical resection and tumor size are associated with recurrence and prognosis, and complete resection should be attempted if possible.
PET/CT and SUVmax were widely used to evaluate the tumor characteristics. In this case, the SUVmax results of the tumor was 1.8 and relatively low. Miura et al[2] reported two cases of mediastinal dedifferentiated liposarcoma with a low SUVmax result, and three cases with a high SUVmax result. Therefore, it seems that PET/CT cannot reliably identify mediastinal dedifferentiated liposarcoma. Meanwhile, we found the ki-67 index to be 5%, which was relatively low and consistent with the low SUVmax result. Thus, we speculate that SUVmax and Ki-67 may be used as prognostic indicators in mediastinal dedifferentiated liposarcoma.
In summary, we described a case of primary multifocal and recurrent mediastinal dedifferentiated liposarcoma treated by combining surgery with 125I brachytherapy, as well as a review of the literature. We suggest that surgical resection provides beneficial effects for dedifferentiated liposarcoma in mediastinum, even in cases with local recurrence. 125I brachytherapy may be beneficial for recurrent unresectable patients.
Manuscript source: Unsolicited Manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: da Costa AC, Vermeersch P S-Editor: Tang JZ L-Editor: Filipodia E-Editor: Xing YX
| 1. | Dei Tos AP, Pedeutour F, Marino-Enriquez A, Rossi S. Dedifferentiated liposarcoma in World Health Organization classification of tumours pathology and genetics of tumours of soft tissue and bone. Fletcher CDM, Bridge JA, Hogendoorn PCW, Mertens F, editor. Lyon: IARC Press 2013; 39. |
| 2. | Miura K, Hamanaka K, Matsuoka S, Takeda T, Agatsuma H, Hyogotani A, Ito KI, Nishimaki F, Koizumi T, Uehara T. Primary mediastinal dedifferentiated liposarcoma: Five case reports and a review. Thorac Cancer. 2018;9:1733-1740. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 3. | Evans HL. Liposarcoma: a study of 55 cases with a reassessment of its classification. Am J Surg Pathol. 1979;3:507-523. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 402] [Cited by in RCA: 376] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 4. | Thway K, Jones RL, Noujaim J, Zaidi S, Miah AB, Fisher C. Dedifferentiated Liposarcoma: Updates on Morphology, Genetics, and Therapeutic Strategies. Adv Anat Pathol. 2016;23:30-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 103] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 5. | Weaver HL, Preston SD, Wong HH, Jani P, Coonar AS. Surgical resection of a massive primary mediastinal liposarcoma with cervical extension. Ann R Coll Surg Engl. 2018;100:e22-e27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Soeroso NN, Pradana A, Djaka M, Ayudika M, Ngadimin S, Soeroso L. An unusual case of recurrent huge primary mediastinal dedifferentiated liposarcoma. Int J Surg Case Rep. 2018;50:140-143. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Kim SY, Froelich JJ, Dawson H, Peters AA, Tappero C, Heverhagen JT. Inflammatory calcified de-differentiated liposarcoma of the anterior mediastinum. ANZ J Surg. 2019;89:1326-1327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Sbrana F, Ugolini C, Taddei C, Alì G, Pasanisi EM. Mediastinal dedifferentiated liposarcoma. Acta Cardiol. 2017;72:499-500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Muthukumar S, Rajendiran S, Damodharan J. Primary dedifferentiated massive mediastinal liposarcoma weighing 5.3 kg. Asian Cardiovasc Thorac Ann. 2017;25:472-473. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Mansuet-Lupo A, Lococo F, Larousserie F, Alifano M, Saliceti R. Dedifferentiated primary mediastinal liposarcoma mimicking a thymic tumor. Pathologica. 2017;109:401-404. [PubMed] |
| 11. | Narasimman S, Jasjit SN, Navarasi SR, Premnath N. A dedifferentiated large posterior mediastinal liposarcoma - An incidental finding successfully resected. Med J Malaysia. 2016;71:201-202. [PubMed] |
| 12. | Harth S, Litzlbauer HD, Behrens CB, Roller FC, Gamerdinger U, Burchert D, Krombach GA. Dedifferentiated Liposarcoma of the Anterior Mediastinum: A Rare Case. Rofo. 2016;188:95-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Hamanaka K, Ohashi M, Nakamura T. Primary mediastinal dedifferentiated liposarcoma resected by lateral thoracotomy with video-assisted thoracoscopic surgery. J Surg Case Rep. 2016;2016. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Fujimoto R, Sato M, Miyata R, Minakata K, Omasa M, Kubo T, Date H. Successful resection of recurrent mediastinal liposarcoma using preoperative evaluation of organ invasion by four-dimensional computed tomography. Gen Thorac Cardiovasc Surg. 2016;64:488-491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Ortega P, Suster D, Falconieri G, Zambrano E, Moran CA, Morrison C, Suster S. Liposarcomas of the posterior mediastinum: clinicopathologic study of 18 cases. Mod Pathol. 2015;28:721-731. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 29] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 16. | Chen M, Yang J, Zhu L, Zhou C, Zhao H. Primary intrathoracic liposarcoma: a clinicopathologic study and prognostic analysis of 23 cases. J Cardiothorac Surg. 2014;9:119. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 40] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 17. | Boland JM, Colby TV, Folpe AL. Liposarcomas of the mediastinum and thorax: a clinicopathologic and molecular cytogenetic study of 24 cases, emphasizing unusual and diverse histologic features. Am J Surg Pathol. 2012;36:1395-1403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 68] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 18. | Fukai R, Fukumura Y, Suzuki K. A dedifferentiated liposarcoma of the anterior mediastinum. Int J Clin Oncol. 2009;14:174-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 19. | Coulibaly B, Bouvier C, Payan MJ, Thomas P. Recurrent dedifferentiated liposarcoma of mediastinum involving lung and pleura. Interact Cardiovasc Thorac Surg. 2009;9:741-742. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 20. | Hirai S, Hamanaka Y, Mitsui N, Uegami S, Matsuura Y. Surgical resection of primary liposarcoma of the anterior mediastinum. Ann Thorac Cardiovasc Surg. 2008;14:38-41. [PubMed] |
| 21. | Hahn HP, Fletcher CD. Primary mediastinal liposarcoma: clinicopathologic analysis of 24 cases. Am J Surg Pathol. 2007;31:1868-1874. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 66] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 22. | Evans HL, Khurana KK, Kemp BL, Ayala AG. Heterologous elements in the dedifferentiated component of dedifferentiated liposarcoma. Am J Surg Pathol. 1994;18:1150-1157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 110] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 23. | Benchetritt M, Hofman V, Vénissac N, Brennetot C, Italiano A, Aurias A, Padovani B, Pedeutour F, Hofman P. Dedifferentiated liposarcoma of the pleura mimicking a malignant solitary fibrous tumor and associated with dedifferentiated liposarcoma of the mediastinum: usefulness of cytogenetic and molecular genetic analyses. Cancer Genet Cytogenet. 2007;179:150-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 24. | Toda M, Izumi N, Tsukioka T, Komatsu H, Okada S, Hara K, Ito R, Shibata T, Nishiyama N. Huge mediastinal liposarcoma resected by clamshell thoracotomy: a case report. Surg Case Rep. 2017;3:16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 25. | Yang B, Guo WH, Lan T, Yuan F, Liu GJ, Zan RY, You X, Tan QY, Liao ZY. CT-guided 125I seed implantation for inoperable retroperitoneal sarcoma: A technique for delivery of local tumor brachytherapy. Exp Ther Med. 2016;12:3843-3850. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 26. | Mo Z, Zhang T, Zhang Y, Xiang Z, Yan H, Zhong Z, Gao F, Zhang F. Feasibility and clinical value of CT-guided 125I brachytherapy for metastatic soft tissue sarcoma after first-line chemotherapy failure. Eur Radiol. 2018;28:1194-1203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 24] [Article Influence: 3.0] [Reference Citation Analysis (0)] |