Published online Feb 26, 2020. doi: 10.12998/wjcc.v8.i4.831
Peer-review started: November 28, 2019
First decision: December 30, 2019
Revised: January 1, 2020
Accepted: February 10, 2020
Article in press: February 10, 2020
Published online: February 26, 2020
Processing time: 90 Days and 7.5 Hours
Patellar tendon rupture is a rare disease, and reports regarding patellar tendon reconstruction with ligament augmentation reconstruction system (LARS) ligaments are limited, with only three reports available in the literature. LARS ligaments are made of polyethylene terephthalate and have been certified as a more favorable option than other tendon transplants. To our knowledge, this is the first report of patellar tendon reconstruction with LARS for suture fixation due to poor quality of the tendon after multiple operations to enable early mobilization and quick rehabilitation.
A 65-year-old woman had limited ability in extending her leg and an inability to perform a straight leg raise after multiple operations due to patella fracture. The patient underwent patellar tendon reconstruction with LARS artificial ligaments. After 12 mo of follow-up, the patient was able to perform a straight leg raise, and the incision healed well without complications. The Lysholm score was 95 and the range of motion of the knee was 0-130°.
This study revealed that patellar tendon reconstruction with LARS artificial ligaments is possible in a patient with a patellar tendon rupture who required rapid postoperative recovery.
Core tip: Patellar tendon rupture is a rare disease and leads to a loss of involvement in sports activities and hinders daily life activities due to loss of function of the knee extensor mechanism. We present a case of chronic patellar tendon rupture in a 65-year-old woman who underwent multiple operations, after 12 mo of follow-up, the patient had good clinical and functional outcomes.
- Citation: Yang F, Wang GD, Huang R, Ma H, Zhao XW. Ligament augmentation reconstruction system artificial ligaments in patellar tendon reconstruction - a chronic patellar tendon rupture after multiple operations: A case report. World J Clin Cases 2020; 8(4): 831-837
- URL: https://www.wjgnet.com/2307-8960/full/v8/i4/831.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i4.831
The patellar tendon, a part of the knee extensor mechanism, can be predisposed to ruptures due to direct or indirect injury. Ruptures are rare, but serious injuries at the joint will lead to a loss of involvement in sports activities or hinder daily life activities owing to the loss of function of the knee extensor mechanism. Ruptures typically tend to occur in males aged 30 to 40 years and involve a complete tear of the tendon that runs from the tibial tubercle to the patella inferior pole[1,2]. In chronic cases, reconstruction surgery is the gold standard if a primary repair is not possible and aims to restore the ability to extend the knee[3]. Although surgical repair has been recommended for acute patellar tendon rupture, the efficacy and prognosis of reconstruction surgery for chronic patellar tendon rupture are still controversial. There is currently no gold standard for the treatment of tendon ligament ruptures, but some surgical techniques have been previously reported; for instance, one- or two-stage reconstructions[4], contralateral bone-tendon-bone grafts[5], ipsilateral semitendinosus tendon grafts[6,7], and artificial ligament grafts have been used to reconstruct the patellar tendon[8,9]. All of the previous reports included small samples, and the efficacy and prognosis of surgery were unclear. Postoperative complications are critical to the success of the reconstruction and include wound infections, septicemia, fractures, wire breaks, and quadriceps weakness[3].
Herein, we present a case of chronic patellar tendon rupture in a 65-year-old woman who underwent multiple operations; we repaired the rupture with the ligament augmentation reconstruction system (LARS) due to poor-quality soft tissues and a vascular injury. This is a rare condition that was treated with good clinical and functional outcomes at the 12 mo follow-up. To the best of our knowledge, this is the first case of the use of LARS in a patellar tendon reconstruction due to chronic tendon rupture after multiple operations for patellar fractures.
A 65-year-old retiree with no previous history of other diseases presented to hospital due to a left patellar tendon rupture after three operations. She experienced knee pain and feared going up and down stairs.
The woman underwent open reduction and internal fixation after a fracture of the left patella in another hospital 3 years ago, and was treated again for the fracture 1 mo later. The internal fixation was removed 17 mo ago, and the patient was immobilized postoperatively for 4 wk.
The patient has no previous history of other diseases.
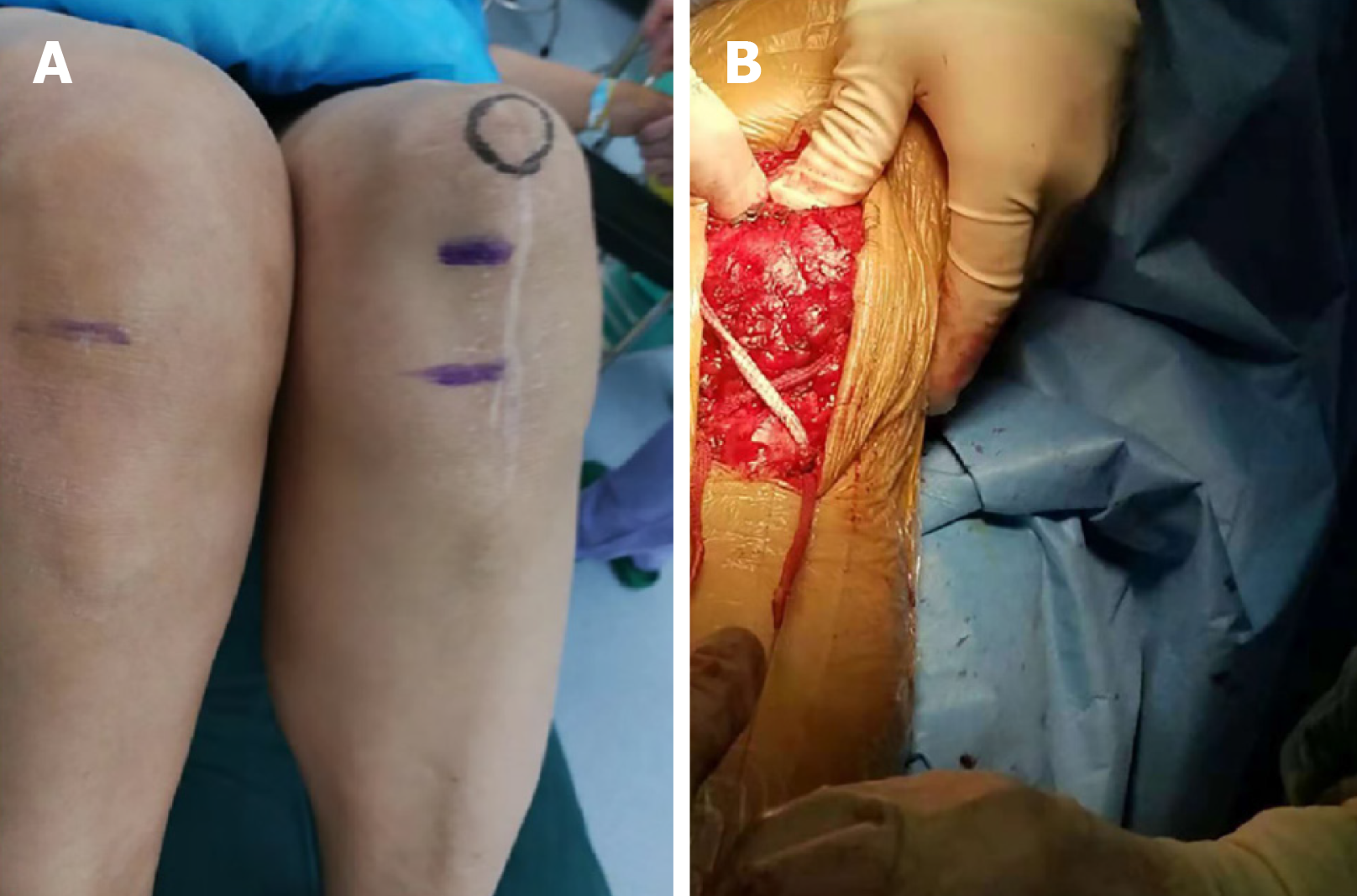
A physical examination revealed that the left knee was limited in active extension, she was unable to perform a straight leg raise, and there was palpable concavity on the patellar tendon (Figure 1A). Her body mass index was 24.4 and the Lysholm score was 38 (Table 1).
| Preoperative | Postoperative | |
| Pain | 10 | 25 |
| Instability | 5 | 25 |
| Locking | 15 | 15 |
| Stair climbing | 0 | 6 |
| Limp | 0 | 5 |
| Support | 2 | 5 |
| Swelling | 6 | 10 |
| Squatting | 0 | 4 |
| Overall | 38 | 95 |
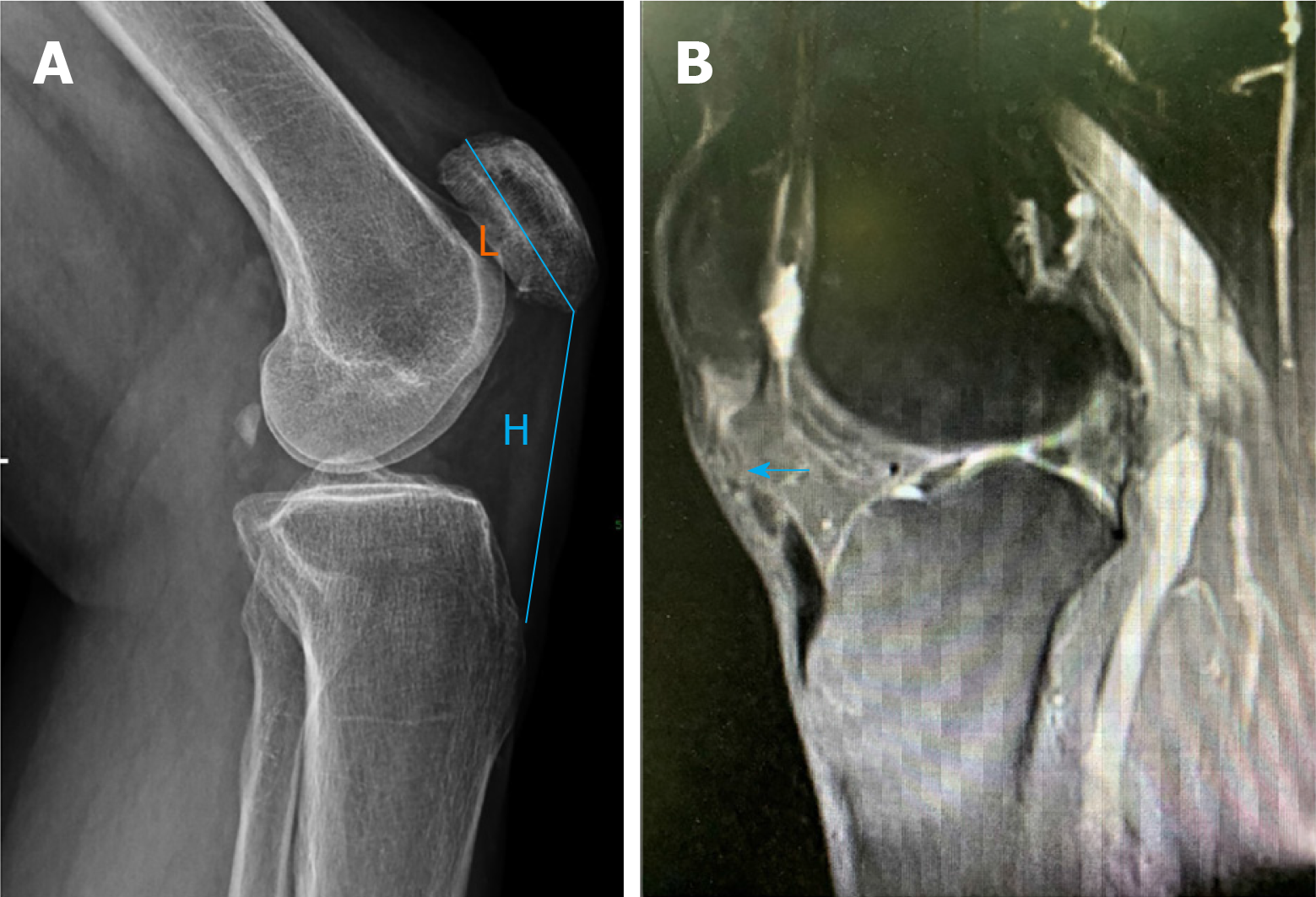
The lateral knee radiograph showed that the patella moved superiorly, which revealed a high-riding patella and the Insall-Salvati ratio was 1.53 (Figure 2A). Magnetic resonance imaging (MRI) revealed rupture of the patellar tendon (Figure 2B).
Chronic patellar tendon rupture.
The patient consented to LARS artificial ligaments instead of autograft or allograft reconstruction as she had already undergone repeated operations previously that resulted in poor-quality tendons with a poor blood supply. As autograft reconstruction requires long-term recovery and immobilization, the patient was informed of the advantages and risks of LARS artificial ligament reconstruction and signed an informed consent form before surgery. The operation was performed by the deputy chief physician. The surgeon tied a tourniquet at the proximal part of the thigh, and the surgical incision was along the longitudinal midline of the left knee. The surgical field revealed that the patellar tendon was completely ruptured, and granulation tissue was hyperplastic and adherent. We loosened the stump of the patellar ligament, braided the ligament, and made three longitudinal medial-sided and lateral-sided bone tunnels through the patella with Kirschner wires. The braided ligament was fixed through the bone tunnels at a flexed knee position of 90°. The reconstruction was performed using a “figure 8” pattern through the patellar tunnel with screw fixations to the tibia (Figure 1B). The wound was washed with sterile normal saline and sutured in layers.
Weight bearing was not allowed for 4 wk. Particular attention was paid to postoperative rehabilitation exercises. The day after surgery, the patient was able to get out of bed, and could use a brace for external immobilization. We first educated the patient on ankle pump exercises and focused on passive range of motion (ROM) exercises, then we concentrated on extensor and quadriceps strength. The patient was discharged after three days, and the ROM was 0-90°.
At the 1-mo postoperative follow-up, the wound had healed well and had no signs of infection, and the patient walked without the aid of crutches. The patient was able to complete a straight leg raise but still felt a little discomfort and dreaded descending stairs. The ROM improved to 0-120°, and the radiographs showed that the patella had moved distally (Figure 3). At the 12 mo postoperative follow-up, the affected limb was the same as the uninjured side, and the Lysholm score was 95 (Table 1). The ROM of the knee was 0-130°.
Disruption of the knee extensor mechanism can occur as a result of injuries to the quadriceps muscle, quadriceps tendon, medial and lateral patellar retinaculum, patella, patellar tendon, and the tibial tubercle[2]. Patellar tendon rupture is a rare injury that occurs in 0.6% of the general population. The estimated mean age of the patient population is 49 years, 78% are male, the most prevalent risk factors are previous knee surgery and patients who had recently undergone total knee arthroplasty[10]. Spontaneous rupture may occur in degenerated tendons, and spontaneous ruptures have been reported to be associated with local steroid injection, systemic lupus erythematosus, rheumatoid arthritis, chronic renal failure, hyperparathyroidism, infections, iatrogenic causes, and diabetes mellitus[11-16]. Although patellar tendon ruptures are rare, they should be diagnosed early and treated with surgery due to functional disability of the knee extensor mechanism. The diagnosis of patellar tendon rupture relies heavily on medical history, symptoms, signs, and imaging examinations, such as radiographs, arthrography, ultrasound, and MRI; radiographs are the most cost-effective method as the symbolic diagnostic sign is a high-riding patella. MRI can further diagnose patellar tendon rupture and provides detailed information about the injury, which contributes to the formulation of a surgical plan.
It is rare for acute tendon ruptures to develop into a chronic condition, and acute ruptures require direct primary repair as these are associated with functional disability of the knee extensor mechanism. The ideal transplants for ligament reconstruction remain controversial, and the main types of tendon transplants are as follows: Autologous, allogeneic, and artificial tendons[3]. Autografts are the most common graft material which can enhance suture repair of the patellar tendon, especially the hamstring tendon, however, the quality of the soft tissues and the prolonged rehabilitation period required are unsuitable for elderly patients, and autografts result in more postoperative complications, including infection and irritation, than other tendon transplants[13,17]. The main advantage of allografts is that they can avoid the autologous harvesting process, which reduces the morbidity of the surgical procedure, but allografts can expose patients to the risk of infectious disease and graft rejection[18]. Over the last decade, LARS artificial ligaments have been used as an advantageous option for suture fixation in ligamentous reconstruction of the knee, especially in cruciate and collateral ligament reconstructions. The use of LARS for patellar tendon reconstruction is infrequent. Talia and Tran reported the use of LARS for bilateral tendon reconstruction in a young gymnast[8]. Naim et al[9] reported a 79-year-old woman who fell and landed on her left knee, and they reconstructed her tendon using LARS ligaments 1 year later. Bouguennec and Colombet reported a 29-year-old handball player who presented with an iterative rupture and a fracture of the patellar tunnel after semitendinosus graft reconstruction was performed and revision reconstruction surgery used LARS[19]. All patients achieved rapid postoperative recovery without re-rupture or synovitis.
LARS ligaments are made of polyethylene terephthalate, which has the following advantages: (1) Avoids the need to obtain autologous tendons and donor site morbidity; (2) Accelerated rehabilitation and early return to sport activities; (3) Does not demonstrate evidence of graft rejection; (4) Encourages collagen ingrowth due to the porosity of the material; and (5) Provides the possibility of repeating the reconstruction in case of failure[9,20,21]. The disadvantages of reconstruction of the patellar ligament are the lack of long-term follow-up, large population-based studies and quality randomized trials. However, LARS ligaments have been certified as a more favorable option than other tendon transplants for anterior cruciate ligament reconstruction in which twenty-six patients were reviewed at an average follow-up of 11.6 years, especially in elderly patients requiring rapid postoperative recovery[22].
In the present case, LARS ligaments were used in an elderly woman. Although the LARS ligament has mostly been used in cruciate and collateral ligament reconstructions, especially in athletes, it can be used in elderly patients who require high-quality postoperative function and early mobilization. The application of the LARS ligament in the reconstruction of chronic patellar ligament rupture is rare, but the outcomes in these cases are good. A limitation of this case is the relatively short follow-up (12 mo), but postoperative complications were rare, as in other previously reported tendon reconstructions, such as knee synovitis, graft ruptures, surgical site infection, and residual knee instability[23]. To the best of our knowledge, this is the first study to report reconstruction with LARS ligaments in an elderly woman who underwent multiple patella operations. We suggest the use of the LARS in elderly patients who require rapid postoperative recovery.
Patellar tendon ruptures are rare but serious injuries. We report a case in which LARS artificial ligaments were chosen for suture fixation due to the poor quality of the tendons after multiple operations to enable early mobilization and quick rehabilitation. At 12 mo follow-up, the patient achieved rapid postoperative recovery, and was able to complete a straight leg raise and did not fear going up and down stairs.
We thank the patient for providing consent for this case report.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kung WM S-Editor: Dou Y L-Editor: Webster JR E-Editor: Ma YJ
| 1. | Garner MR, Gausden E, Berkes MB, Nguyen JT, Lorich DG. Extensor Mechanism Injuries of the Knee: Demographic Characteristics and Comorbidities from a Review of 726 Patient Records. J Bone Joint Surg Am. 2015;97:1592-1596. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 54] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 2. | Tanaka MJ, Chahla J, Farr J 2nd, LaPrade RF, Arendt EA, Sanchis-Alfonso V, Post WR, Fulkerson JP. Recognition of evolving medial patellofemoral anatomy provides insight for reconstruction. Knee Surg Sports Traumatol Arthrosc. 2019;27:2537-2550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 68] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 3. | Gilmore JH, Clayton-Smith ZJ, Aguilar M, Pneumaticos SG, Giannoudis PV. Reconstruction techniques and clinical results of patellar tendon ruptures: Evidence today. Knee. 2015;22:148-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 85] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 4. | Harato K, Kobayashi S, Udagawa K, Iwama Y, Masumoto K, Enomoto H, Niki Y. Surgical Technique to Bring Down the Patellar Height and to Reconstruct the Tendon for Chronic Patellar Tendon Rupture. Arthrosc Tech. 2017;6:e1897-e1901. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 5. | Temponi EF, Camelo N, Tuteja S, Thaunat M, Daggett M, Fayard JM, de Carvalho Júnior LH, Sonnery-Cottet B. Reconstruction of chronic patellar tendon rupture with contralateral bone-tendon-bone autograft. Knee Surg Sports Traumatol Arthrosc. 2017;25:2468-2473. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 34] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 6. | Chen B, Li R, Zhang S. Reconstruction and restoration of neglected ruptured patellar tendon using semitendinosus and gracilis tendons with preserved distal insertions: two case reports. Knee. 2012;19:508-512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 38] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 7. | Samagh SP, Huyke FA, Buchler L, Terry MA, Tjong VK. Treatment of a Neglected Patellar Tendon Rupture with a Modified Surgical Technique: Ipsilateral Semitendinosus Autograft Reconstruction with Suture Tape Augmentation. Case Rep Orthop. 2018;2018:2037638. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 8. | Talia AJ, Tran P. Bilateral patellar tendon reconstruction using LARS ligaments: case report and review of the literature. BMC Musculoskelet Disord. 2016;17:302. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 9. | Naim S, Gougoulias N, Griffiths D. Patellar tendon reconstruction using LARS ligament: surgical technique and case report. Strategies Trauma Limb Reconstr. 2011;6:39-41. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 25] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 10. | Clayton RA, Court-Brown CM. The epidemiology of musculoskeletal tendinous and ligamentous injuries. Injury. 2008;39:1338-1344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 486] [Cited by in RCA: 485] [Article Influence: 28.5] [Reference Citation Analysis (0)] |
| 11. | Goldstein ZH, Yi PH, Haughom BD, Hellman MD, Levine BR. Bilateral extensor mechanism disruption after total knee arthroplasty in two morbidly obese patients. Orthopedics. 2015;38:e443-e446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Grecomoro G, Camarda L, Martorana U. Simultaneous chronic rupture of quadriceps tendon and contra-lateral patellar tendon in a patient affected by tertiary hyperparatiroidism. J Orthop Traumatol. 2008;9:159-162. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 13. | Maffulli N, Buono AD, Oliva F. Ipsilateral hamstring tendon graft reconstruction for chronic patellar tendon ruptures: surgical technique. Muscles Ligaments Tendons J. 2017;7:157-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | Takata Y, Nakase J, Numata H, Oshima T, Tsuchiya H. Repair and augmentation of a spontaneous patellar tendon rupture in a patient with Ehlers-Danlos syndrome: a case report. Arch Orthop Trauma Surg. 2015;135:639-644. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Albayrak İ, Küçük A, Arslan Ş, Özbek O. Spontaneous patellar tendon rupture in a case followed up for diagnosis of systemic lupus erythematosus. Eur J Rheumatol. 2014;1:159-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Torkaman A, Yousof Gomrokchi A, Elahifar O, Barmayoon P, Shojaei SF. Simultaneous bilateral rupture of patellar tendons in diabetic hemodialysis patient: A case report. Caspian J Intern Med. 2018;9:306-311. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 17. | Woodmass JM, Johnson JD, Wu IT, Krych AJ, Stuart MJ. Patellar Tendon Repair With Ipsilateral Semitendinosus Autograft Augmentation. Arthrosc Tech. 2017;6:e2177-e2181. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 18. | Lewis PB, Rue JP, Bach BR. Chronic patellar tendon rupture: surgical reconstruction technique using 2 Achilles tendon allografts. J Knee Surg. 2008;21:130-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 28] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 19. | Bouguennec N, Colombet P. Iterative Rupture of the Patellar Tendon: A Case Report of an Original Technique for Revision Reconstruction Using an Adjustable Loop and an Artificial Ligament. Case Rep Orthop. 2018;2018:6107287. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 20. | Trieb K, Blahovec H, Brand G, Sabeti M, Dominkus M, Kotz R. In vivo and in vitro cellular ingrowth into a new generation of artificial ligaments. Eur Surg Res. 2004;36:148-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 85] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 21. | Mulford JS, Chen D. Anterior cruciate ligament reconstruction: a systematic review of polyethylene terephthalate grafts. ANZ J Surg. 2011;81:785-789. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 22] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 22. | Parchi PD, Ciapini G, Paglialunga C, Giuntoli M, Picece C, Chiellini F, Lisanti M, Scaglione M. Anterior Cruciate Ligament Reconstruction with LARS Artificial Ligament-Clinical Results after a Long-Term Follow-Up. Joints. 2018;6:75-79. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 34] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 23. | Tiefenboeck TM, Thurmaier E, Tiefenboeck MM, Ostermann RC, Joestl J, Winnisch M, Schurz M, Hajdu S, Hofbauer M. Clinical and functional outcome after anterior cruciate ligament reconstruction using the LARS™ system at a minimum follow-up of 10 years. Knee. 2015;22:565-568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 69] [Article Influence: 6.9] [Reference Citation Analysis (0)] |