Published online Feb 26, 2020. doi: 10.12998/wjcc.v8.i4.815
Peer-review started: November 1, 2019
First decision: December 4, 2019
Revised: December 23, 2019
Accepted: January 1, 2020
Article in press: January 15, 2020
Published online: February 26, 2020
Processing time: 116 Days and 23.2 Hours
Aortic stenosis is the most common valve disease in adults. Transcatheter aortic valve implantation (TAVI) is being increasingly applied for intermediate- to low-risk patients. Here, we describe an uncommon complication of delayed right coronary obstruction in a transapical TAVI case.
A 73-year-old woman with a EuroSCORE II of 1.21% underwent transapical TAVI because of severe aortic stenosis. The surgical procedure was uneventful. However, during routine monitoring after valve placement, the patient had a sudden onset of slow heart rate, the systolic blood pressure dropped sharply from 115 to 60 mmHg, and the central venous pressure abruptly increased from 10 to 33 cmH2O. The patient had a poor response to vasoactive agents. Transesophageal echocardiography revealed poor myocardial contractility, and electrocardiography showed a significant depression of ST-segment. Another angiography was performed immediately, which suggested complete obstruction of the right coronary artery. An emergency protocol was initiated. Cardiopulmonary bypass was established immediately. An aortic biological valve replacement under cardiopulmonary bypass was performed.
Perioperative monitoring, early recognition, and diagnosis of obstruction of coronary arteries in TAVI are important. Transesophageal echocardiography is a useful diagnostic and monitoring tool in this situation. Emergency protocols should be established during TAVI.
Core tip: Right coronary artery obstruction during transcatheter aortic valve implantation (TAVI) is relatively rare. The unique pathophysiological findings of this case were thoroughly described. Prompt recognition by anesthesiologists of this complication during TAVI is particularly important. Heart team approach has been proven to be effective and efficient in emergencies during TAVI. Sufficient knowledge about the procedure is required by the whole team. A comprehensive preoperative evaluation should be performed and emergency protocols should be established in advance so that prompt and right decisions can be made and ensure timely resuscitation of the patients.
- Citation: Xu Z, Yu H, Liang P. Delayed right coronary ostial obstruction after J-valve deployment in transcatheter aortic valve implantation: A case report. World J Clin Cases 2020; 8(4): 815-819
- URL: https://www.wjgnet.com/2307-8960/full/v8/i4/815.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i4.815
Aortic stenosis (AS) is the most common valve disease in adults in China. However, most patients with valve diseases over 50-years-old in China did not receive standard treatment according to the 2014 report from the cardiopulmonary bypass (CPB) Board of the Chinese Medical Association. Surgical aortic valve replacement has been the standard approach, with an overall 2.5%-4% mortality[1]. However, transcatheter aortic valve implantation (TAVI) is being increasingly used for the treatment of symptomatic AS.
Recently, an increasing number of intermediate- to low-risk patients have been treated with TAVI[2,3]. Along with its application, several complications have been encountered such as pericardial bleeding, paravalvular leakage, conduction abnormalities, and coronary artery obstruction. Coronary artery obstruction is the most severe complication. Here, we describe an uncommon complication of delayed right coronary obstruction in a low-risk transapical TAVI case.
A 73-year-old woman presented to the Department of Cardiovascular Surgery of our hospital complaining of palpitation and precordial discomfort.
The patient’s symptoms started 5 mo ago with recurrent episodes of palpitation and precordial discomfort, which had been worsened by exertion. The patient experienced occasional chest pain and syncope without dizziness, nausea, and vomiting.
The patient was diagnosed with hypertension 10 years ago. The blood pressure was controlled with reserpine.
The patient had a disease-free personal and family history.
The patient’s temperature was 36.7 °C, heart rate was 90 bpm, respiratory rate was 20 breaths per min, and blood pressure was 145/87 mmHg. The heart border expanded to the left. Systolic ejection murmur could be auscultated over the aortic and pulmonary areas. Our clinical consideration was AS.
Arterial blood gas analysis revealed a mild decrease of oxygen partial pressure (78 mmHg) on room air with normal hematocrit and hemoglobin count. Prothrombin, partial thromboplastin times, and d-dimers were normal. The blood biochemistries, as well as urine analysis were normal. Electrocardiogram showed a sinus rhythm with complete left bundle branch block. Chest X-ray was also normal.
Coronary artery disease was excluded before the procedure by angiography. Transthoracic echocardiography and intraoperative transesophageal echocardiography (TEE) confirmed severe aortic valve calcification and stenosis causing left ventricular concentric hypertrophy with an ejection fraction of 66%.
The final diagnosis of the presented case was severe AS with sinus rhythm and New York Heart Association functional class grade III.
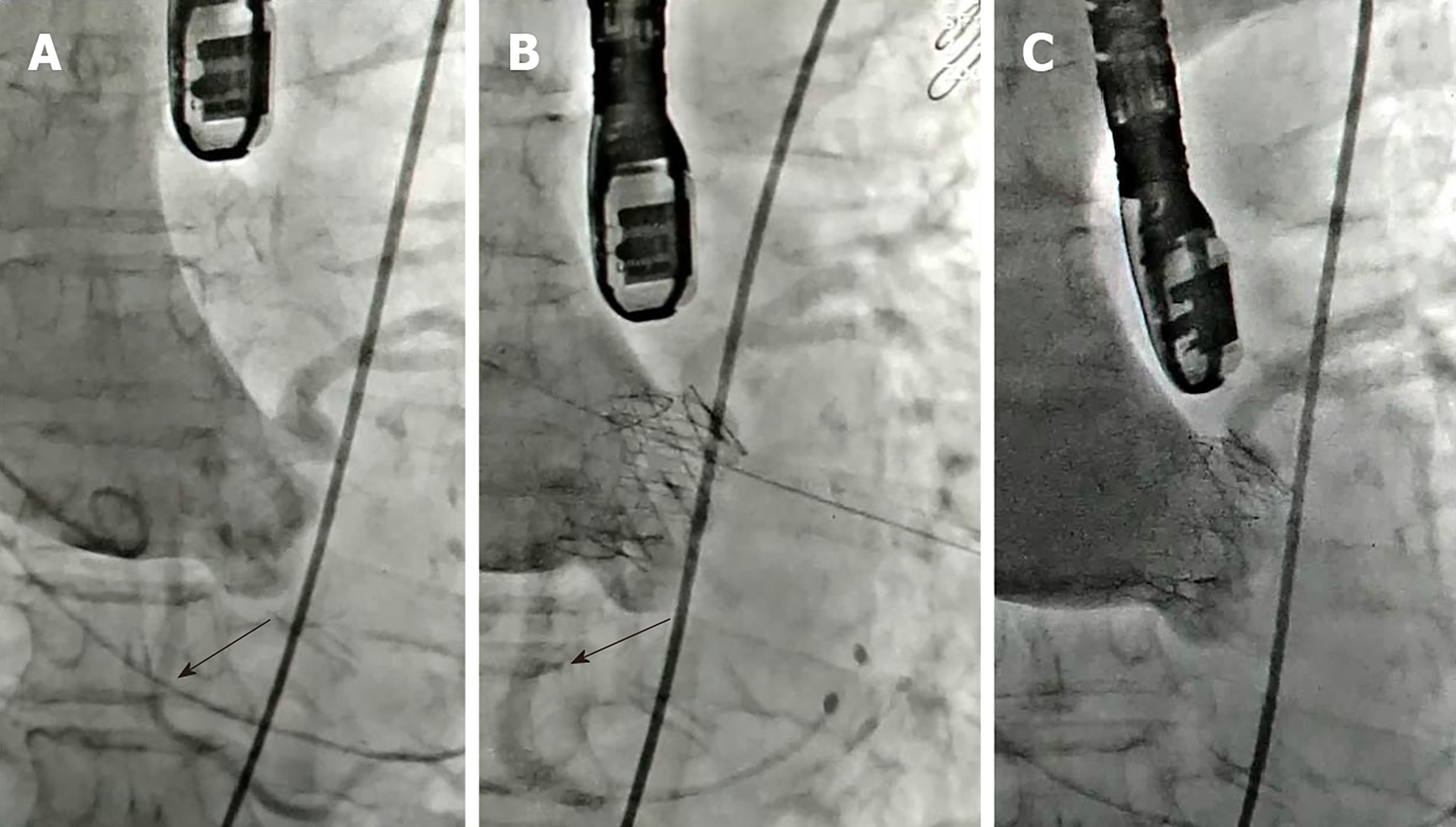
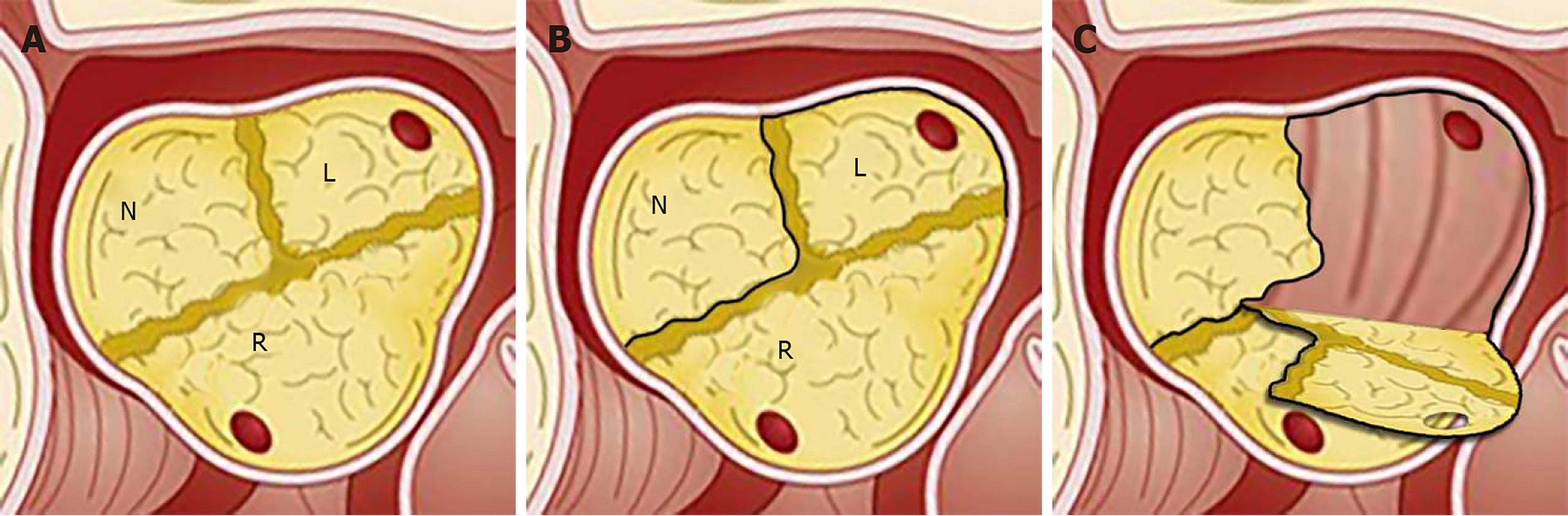
The preoperative evaluation of the patient revealed a logistic EuroSCORE II of 1.21%. Transapical TAVI was scheduled. After routine monitoring in the hybrid operating room, anesthesia was induced. Then TEE was used to guide the transapical approach. Under the guidance of digital subtraction angiography, aortic valve balloon expansion was performed by a temporary pacemaker at 160 beats per min. TEE after balloon expansion showed a 21.5 mm aortic valve annulus (Video 1). A 23 mm J-valve, a second-generation TAVI device with three unique U-shape graspers (Jie-Cheng Medical Technology, Suzhou, China), was implanted uneventfully. The heart function recovered immediately without any support of vasoactive agents. The electrocardiography showed a 95-bpm sinus rhythm with normal ST-segment. TEE showed excellent placement and function of the new valve (Video 2). The coronary arteries were intact on angiography (Figure 1A and B). The hemodynamic state was stable with a mean arterial blood pressure of 74 mmHg. At 9 min after valve deployment, the heart rate of the patient decreased, systolic blood pressure dropped sharply from 115 to 60 mmHg and central venous pressure abruptly increased from 10 to 33 cmH2O. Epinephrine, norepinephrine, ephedrine, and other vasoactive agents were given immediately to stabilize the hemodynamic status. However, the patient had a poor response to these drugs. At this time, TEE inspection showed poor myocardial contractility. Electrocardiography monitoring showed remarkable ST-segment depression. Another angiography was performed immediately. Complete obstruction of the right coronary artery was found (Figure 1C). Angiographic findings are shown in Videos. (Supplementary videos 1, 2 and 3) The right coronary ostial obstruction was diagnosed. An emergency protocol was initiated. CPB was established immediately. After aortotomy, the severely calcified left coronary leaflet was found to be dislocated to the opening of the right coronary artery causing complete obstruction (Figure 2). Then aortic biological valve replacement under CPB was performed.
The patient was extubated on the same day and was discharged from the hospital 1 wk after surgery without complications.
We report a rare case of delayed-onset right coronary ostial obstruction after successful deployment of the prosthesis in transapical TAVI. Informed consent was signed by the patient. There were some reports of delayed obstruction of a left coronary artery after uneventful TAVI[4,5]. Our case showed that obstruction of coronary arteries, either left or right, could occur in the early post-procedural period although the patient had a low perioperative risk. To the best of our knowledge, this is one of the few cases of delayed-onset right coronary ostial obstruction after successful TAVI.
Coronary obstruction during TAVI is commonly caused by calcified aortic valve leaflet, which is compressed to the openings of the coronary arteries[1]. In some cases, the original valve itself can block blood flow after balloon expansion. The implant itself can also cause obstructions if not positioned properly. However, in this case, J-Valve was used. The crown-shaped three-prong claspers of J-Valve were designed to match the annulus of the aortic valve. Such unique design allows the surgeons to hold the original valve leaflet between the claspers and the new valve, preventing the original valve from shifting to the openings of the coronary arteries[6]. Thus obstruction caused by the original valve is avoided[7,8]. In this case, the original valve and the annulus were found to be severely calcified. The patient had an enlarged right-coronary cusp. The balloon expansion before valve placement was initially intended to tear the calcified and adhesive leaflets along the physiological fissure. However, the leaflet was torn along the aortic annulus and the valve was divided into a large left-right-coronary portion and a small non-coronary portion (Figure 2). Then the large portion was squeezed between the implanted valve and the claspers. After successful valve deployment, the calcified left-non-coronary portion slowly shifted due to the contraction of the heart and the reciprocating motion of the implanted biological aortic valve. Eventually, the right coronary ostium was blocked.
The typical clinical symptoms of right coronary obstruction during general anesthesia include hemodynamic instability, which is difficult to correct using vasoactive agents, acute right ventricular failure, and various types of arrhythmia according to the blood supply area by the right coronary artery. Thus, prompt recognition by anesthesiologists is particularly important. TEE is a productive diagnostic and monitoring tool that could immediately recognize the reduced myocardial contractility[9]. In addition, it can guide the apex puncture, measure the distance between the aortic valve and the ostia of coronary arteries, and evaluate aortic regurgitations and paravalvular leakages. Therefore, we suggest that TEE should be applied in all transapical TAVI cases. Although TEE inspection sometimes could not reveal the actual state of the blood flow to the coronary arteries due to attenuation by implant and calcifications, it is still an extraordinary monitoring tool in addition to angiography.
For such emergencies, a standard protocol should be established and implemented by all the team members. Tam et al[10] reported that emergencies during TAVI required cardiopulmonary resuscitation, CPB, and stabilizing hemodynamic state. However, many large centers are insufficiently prepared for this kind of emergencies. For instance, Fernandes et al[11] reported that in emergent conditions during TAVI, there is a lack of personnel cooperation, leading to the loss of valuable resuscitation time. In our hospital, all transapical TAVI cases are performed by our experienced TAVI team. A standardized transapical TAVI protocol is followed, which requires installation of standby CPB circuit before surgery in case of emergency.
Recently, TAVI has been increasingly performed in intermediate- to low-risk patients. Although these patients have low perioperative risks, severe complications can still occur. Apex puncture, high-rate ventricular pacing, and balloon expansion can cause complications such as coronary obstruction, atrioventricular block, bleeding, and heart rupture.
From the perspective of anesthesiologists, transapical TAVI patients should be closely monitored, even after surgery. Sufficient knowledge about the procedure is required by the whole team. A comprehensive preoperative evaluation should be performed, and emergency protocols should be established in advance, so that prompt and accurate decisions can be made in emergencies, ensuring timely resuscitation of the patients.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Barik R, Eren B S-Editor: Dou Y L-Editor: Filipodia E-Editor: Liu JH
| 1. | Thomas M, Schymik G, Walther T, Himbert D, Lefèvre T, Treede H, Eggebrecht H, Rubino P, Michev I, Lange R, Anderson WN, Wendler O. Thirty-day results of the SAPIEN aortic Bioprosthesis European Outcome (SOURCE) Registry: A European registry of transcatheter aortic valve implantation using the Edwards SAPIEN valve. Circulation. 2010;122:62-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 663] [Cited by in RCA: 656] [Article Influence: 43.7] [Reference Citation Analysis (0)] |
| 2. | Mack MJ, Leon MB, Thourani VH, Makkar R, Kodali SK, Russo M, Kapadia SR, Malaisrie SC, Cohen DJ, Pibarot P, Leipsic J, Hahn RT, Blanke P, Williams MR, McCabe JM, Brown DL, Babaliaros V, Goldman S, Szeto WY, Genereux P, Pershad A, Pocock SJ, Alu MC, Webb JG, Smith CR; PARTNER 3 Investigators. Transcatheter Aortic-Valve Replacement with a Balloon-Expandable Valve in Low-Risk Patients. N Engl J Med. 2019;380:1695-1705. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3668] [Cited by in RCA: 3476] [Article Influence: 579.3] [Reference Citation Analysis (0)] |
| 3. | Popma JJ, Deeb GM, Yakubov SJ, Mumtaz M, Gada H, O'Hair D, Bajwa T, Heiser JC, Merhi W, Kleiman NS, Askew J, Sorajja P, Rovin J, Chetcuti SJ, Adams DH, Teirstein PS, Zorn GL, Forrest JK, Tchétché D, Resar J, Walton A, Piazza N, Ramlawi B, Robinson N, Petrossian G, Gleason TG, Oh JK, Boulware MJ, Qiao H, Mugglin AS, Reardon MJ; Evolut Low Risk Trial Investigators. Transcatheter Aortic-Valve Replacement with a Self-Expanding Valve in Low-Risk Patients. N Engl J Med. 2019;380:1706-1715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2802] [Cited by in RCA: 2651] [Article Influence: 441.8] [Reference Citation Analysis (0)] |
| 4. | Kukucka M, Pasic M, Dreysse S, Hetzer R. Delayed subtotal coronary obstruction after transapical aortic valve implantation. Interact Cardiovasc Thorac Surg. 2011;12:57-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 19] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Spiro J, Nadeem A, Doshi SN. Delayed left main stem obstruction following successful TAVI with an Edwards SAPIEN XT valve: successful resuscitation and percutaneous coronary intervention using a non-invasive automated chest compression device (AutoPulse). J Invasive Cardiol. 2012;24:224-228. [PubMed] |
| 6. | Liu H, Yang Y, Wang W, Zhu D, Wei L, Guo K, Zhao W, Yang X, Zhu L, Guo Y, Wang W, Wang C. Transapical transcatheter aortic valve replacement for aortic regurgitation with a second-generation heart valve. J Thorac Cardiovasc Surg. 2018;156:106-116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 34] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 7. | Wei L, Liu H, Zhu L, Yang Y, Zheng J, Guo K, Luo H, Zhao W, Yang X, Maimaiti A, Wang C. A New Transcatheter Aortic Valve Replacement System for Predominant Aortic Regurgitation Implantation of the J-Valve and Early Outcome. JACC Cardiovasc Interv. 2015;8:1831-1841. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 48] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 8. | Cheng J, Chen M, Zhu D, Zhang J, Hu J, Guo Y. Successful trans-apical aortic valve implantation for a high risk patient with aortic stenosis using a new second-generation TAVI device - J-Valve system. J Cardiothorac Surg. 2015;10:5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Mukherjee C, Hein F, Holzhey D, Lukas L, Mende M, Kaisers UX, Ender J. Is real time 3D transesophageal echocardiography a feasible approach to detect coronary ostium during transapical aortic valve implantation? J Cardiothorac Vasc Anesth. 2013;27:654-659. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Tam DY, Jones PM, Kiaii B, Diamantouros P, Teefy P, Bainbridge D, Cleland A, Fernandes P, Chu MW. Salvaging catastrophe in transcatheter aortic valve implantation: rehearsal, preassigned roles, and emergency preparedness. Can J Anaesth. 2015;62:918-926. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Fernandes P, Cleland A, Bainbridge D, Jones PM, Chu MW, Kiaii B. Development of our TAVI protocol for emergency initiation of cardiopulmonary bypass. Perfusion. 2015;30:34-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |