Published online Nov 26, 2020. doi: 10.12998/wjcc.v8.i22.5816
Peer-review started: August 25, 2020
First decision: September 29, 2020
Revised: October 8, 2020
Accepted: October 26, 2020
Article in press: October 26, 2020
Published online: November 26, 2020
Processing time: 92 Days and 4.8 Hours
Intussusception rarely causes intestinal obstruction in adults. Metastatic malignant melanoma is the main cause of intussusception of the small intestine among adults. However, malignant melanoma rarely causes intussusception of the colorectum. Moreover, emergent surgery is usually performed for such cases. Here, we report a case of a patient with colocolonic intussusception caused by a malignant melanoma, for which endoscopic reduction and elective surgery were performed.
The patient was a 64-year-old woman who underwent multiple surgeries and received chemotherapy and immunotherapy for a malignant melanoma. During immunotherapy, she had abdominal pain, diarrhea, and bloody stool. Physical examination and laboratory studies did not reveal any findings that warranted emergent surgery. Computed tomography revealed intussusception in the descending colon without intestinal necrosis and perforation. Intussusception was reduced endoscopically, and elective surgery was performed.
This report suggests that endoscopic reduction and elective surgery constitute a treatment option for colocolonic intussusception of metastatic malignant melanomas.
Core Tip: Malignant melanoma rarely causes intussusception in the colorectum, and emergent surgery is usually performed. To the best of our knowledge, this is the first report of colocolonic intussusception caused by metastatic malignant melanoma treated with endoscopic reduction and elective surgery, which could be a feasible option.
- Citation: Kasuga K, Sakamoto T, Takamaru H, Sekiguchi M, Yamada M, Yamazaki N, Hashimoto T, Uraoka T, Saito Y. Endoscopic reduction of colocolonic intussusception due to metastatic malignant melanoma: A case report. World J Clin Cases 2020; 8(22): 5816-5820
- URL: https://www.wjgnet.com/2307-8960/full/v8/i22/5816.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i22.5816
Intussusception rarely causes intestinal obstruction among adults. Metastatic malignant melanoma is the main cause of intussusception in the small intestine of adults[1-3]. Symptomatic metastatic melanoma of the colon is very rare, and there are only a few reports on intussusception due to metastatic malignant melanoma of the colorectum[4-6]. In intussusception of the colon due to metastatic melanoma, emergent surgery is commonly performed. Here, we report a case of a patient with colocolonic intussusception caused by a malignant melanoma, for which endoscopic reduction and elective surgery were performed.
A 60-year-old woman had abdominal pain, diarrhea, and bloody stool in July 2019.
The patient had abdominal pain intermittently 11 d before admission. She also had diarrhea and bloody stool, due to which she sought hospital admission.
In 2004, a melanoma in the patient’s left fifth toe was resected, and inguinal lymph node dissection was performed. The patient underwent five courses of adjuvant chemotherapy with dacarbazine, nimustine, vincristine, and interferon-β.
In June 2015, she developed intussusception and was diagnosed with melanoma metastasis following laparoscopic partial resection of the small intestine. In September 2016, she underwent partial resection of the small intestine and mesenteric lymph node removal for mesenteric lymph node metastasis. In September 2016, she was referred to our hospital after undergoing partial resection of the small intestine and mesenteric lymph node removal for mesenteric lymph node metastasis. Left supraclavicular lymph node enlargement was noted in a follow-up evaluation; thus, in July 2017, treatment with talimogene laherparepvec was initiated, but the lymph node enlargement persisted. In January 2018, pembrolizumab therapy was started. The patient’s lymph nodes gradually reduced in size.
The patient had a free previous medical history.
Her vital signs were normal. Physical examination revealed diffuse abdominal tenderness without rebound tenderness.
The results of the laboratory tests showed normal values, which were as follows: Hemoglobin, 12.4 g/dL; white blood cell count, 5.4 × 103/mm3; and C-reactive protein, 0.12 mg/dL.
Computed tomography, which was performed on the day of admission, revealed antegrade intussusception in the descending colon without intestinal necrosis and perforation (Figure 1). Therefore, colonoscopy was performed for diagnostic purposes. The patient was examined using carbon dioxide and water insufflations. Colonoscopy showed a greyish-white protruded lesion in the descending colon (Figure 2A); the mucosa surrounding the tumor was reddish and edematous, and the tumor in the descending colon fell to the anal side, causing intussusception. Intussusception was reduced naturally during the examination (Figure 2B). After the examination, the abdominal symptoms subsided. Biopsy of the protruded lesions revealed that the tumor was a metastatic melanoma.
The intussusception did not recur after eating, and elective laparoscopic surgery was performed 14 d after the reduction. Surgical findings showed a tumor with a diameter of approximately 30 mm located in the splenic flexure of the descending colon; thus, left hemicolectomy was performed.
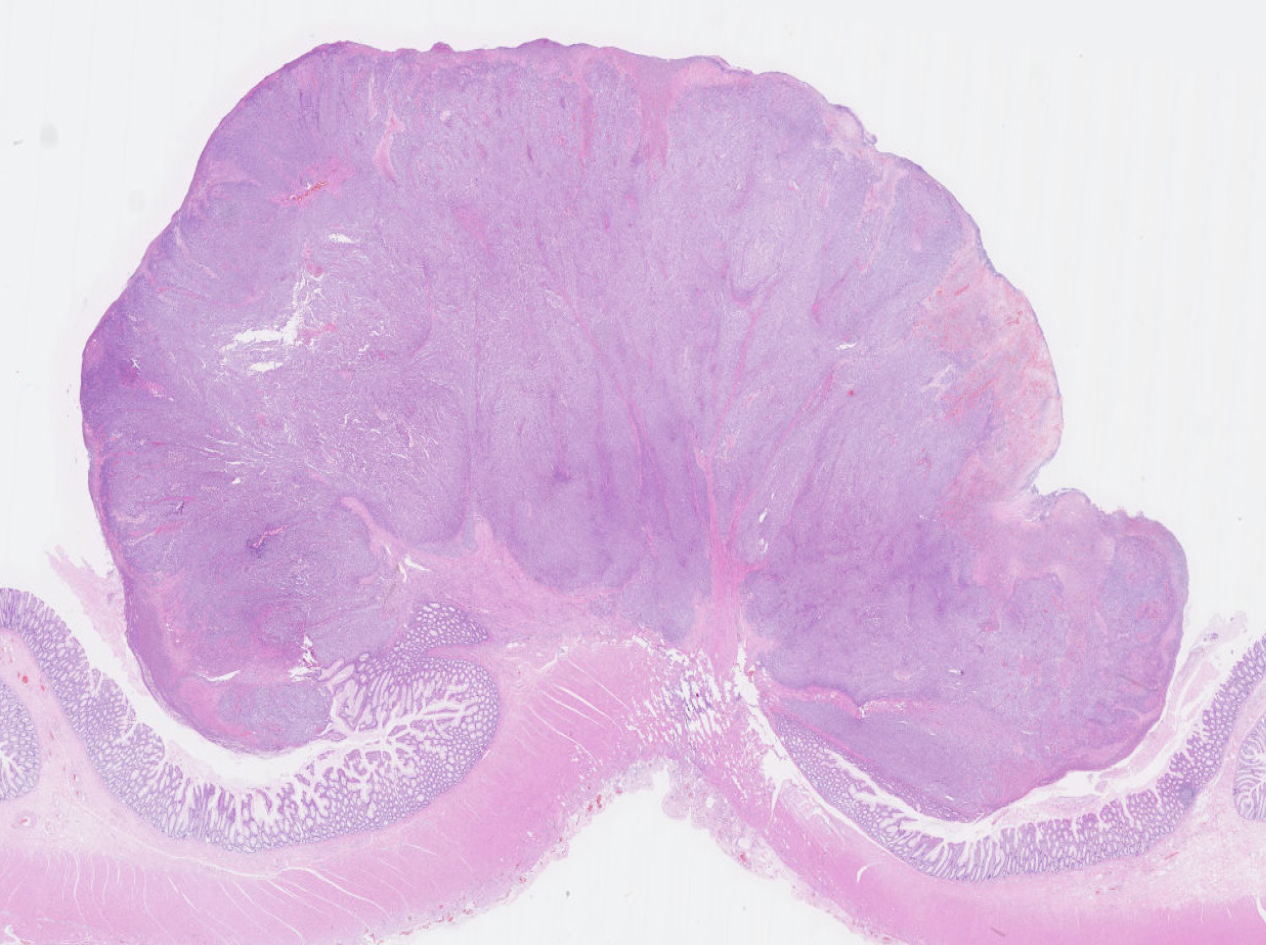
Histopathological examination revealed that the tumor cells had infiltrated into the colonic muscularis propria. The patient was diagnosed with metastatic melanoma with no metastatic tumor in 7 lymph nodes (Figure 3).
The patient’s postoperative course was good, and she was discharged on postoperative day 7. The patient is scheduled to continue to undergo immunotherapy.
To the best of our knowledge, this is the first report of endoscopic reduction and elective surgery for colocolonic intussusception caused by a malignant melanoma. Endoscopic reduction relieved the bowel obstruction associated with the disease. To treat intussusception in children, it is common to perform air or saline enema under ultrasound or fluoroscopic guidance[7]; however, if reduction cannot be achieved, surgery is generally performed. In adults, surgery is the standard treatment. In small bowel intussusception, preoperative reduction is often performed. However, colocolonic or ileocolic intussusception is often caused by a primary colorectal cancer; thus, preoperative and intraoperative reduction is not recommended because of the risk of hematogenous metastasis associated with the reduction procedure[8]. The previously recommended treatment for intussusception among adults was surgery, and preoperative reduction with barium or air is not recommended[8,9].
Recently, asymptomatic intussusception could be easily diagnosed owing to the advancement in computed tomography; sometimes, for these cases, conservative treatment is performed without surgery[10,11]. Thus, emergent surgery is not necessary for all cases of colocolonic intussusception. Furthermore, reduction procedures have been performed in some adult cases of colocolonic or ileocolic intussusception[3,12]. In addition, preoperative colonoscopy is performed to confirm the presence of colorectal tumors and make pathological diagnoses. In this case, the patient had no clinical findings that required emergent surgery such as necrosis or perforation. Thus, we carefully performed colonoscopy using carbon dioxide and water insufflations. We could establish the pathological diagnosis safely without any adverse events. Furthermore, endoscopic reduction was performed coincidentally on the patient, thereby preventing the occurrence of tumor seeding due to perforations. In addition, we were able to evaluate the patient’s general condition preoperatively. Thus, the patient underwent surgery more safely, allowing for a limited resection.
In this case, we performed endoscopic reduction of intussusception of the colon due to a metastatic malignant melanoma. Thus, in some cases, the reduction of intussusception due to other metastatic tumors may be possible. Emergent surgery is indicated in patients with intestinal necrosis or perforation or if a primary colorectal cancer is suspected. However, endoscopic reduction may be an option if the patient’s medical history suggests metastasis of another organ cancer and the patient has no intestinal necrosis or perforation.
Endoscopic reduction and elective surgery constitute a treatment option for colocolonic intussusception of metastatic malignant melanomas. If colocolonic intussusception is confirmed, based on the clinical and imaging findings, without any intestinal necrosis and perforation and there is a medical history of a malignant melanoma, preoperative endoscopy for diagnosis and reduction should be considered.
Manuscript source: Unsolicited manuscript
Corresponding Author's Membership in Professional Societies: The Japanese Society of Gastroenterology, No. 056335.
Specialty type: Medicine, research and experimental
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Lasithiotakis K S-Editor: Zhang L L-Editor: A P-Editor: Wang LL
| 1. | Marsicovetere P, Ivatury SJ, White B, Holubar SD. Intestinal Intussusception: Etiology, Diagnosis, and Treatment. Clin Colon Rectal Surg. 2017;30:30-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 198] [Article Influence: 22.0] [Reference Citation Analysis (0)] |
| 2. | Lindor RA, Bellolio MF, Sadosty AT, Earnest F 4th, Cabrera D. Adult intussusception: presentation, management, and outcomes of 148 patients. J Emerg Med. 2012;43:1-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 30] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 3. | Onkendi EO, Grotz TE, Murray JA, Donohue JH. Adult intussusception in the last 25 years of modern imaging: is surgery still indicated? J Gastrointest Surg. 2011;15:1699-1705. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 51] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 4. | Bromwich AF, Bateson EM, Wieteska J. Letter: Metastatic melanoma presenting as an intussusception of the colon. Med J Aust. 1975;1:183-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 5. | Watson RG, McMullin JP. Intussusception of the colon secondary to gastrointestinal metastatic melanoma. J R Coll Surg Edinb. 1980;25:200-201. [PubMed] |
| 6. | Behrenbruch C, Lippey J, Spillane J, Henderson M, Heriot A. Colocolonic intussusception from metastatic melanoma. ANZ J Surg. 2018;88:E214-E215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 7. | Lioubashevsky N, Hiller N, Rozovsky K, Segev L, Simanovsky N. Ileocolic vs small-bowel intussusception in children: can US enable reliable differentiation? Radiology. 2013;269:266-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 50] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 8. | Nagorney DM, Sarr MG, McIlrath DC. Surgical management of intussusception in the adult. Ann Surg. 1981;193:230-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 238] [Cited by in RCA: 233] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 9. | Huang BY, Warshauer DM. Adult intussusception: diagnosis and clinical relevance. Radiol Clin North Am. 2003;41:1137-1151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 84] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 10. | Hong KD, Kim J, Ji W, Wexner SD. Adult intussusception: a systematic review and meta-analysis. Tech Coloproctol. 2019;23:315-324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 99] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 11. | Perez MC, Sun J, Farley C, Han D, Sun AH, Narayan D, Lowe M, Delman KA, Messina JL, Gonzalez RJ, Sondak VK, Khushalani NI, Zager JS. Management of intussusception in patients with melanoma. J Surg Oncol. 2019;119:897-902. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Honjo H, Mike M, Kusanagi H, Kano N. Adult intussusception: a retrospective review. World J Surg. 2015;39:134-138. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 118] [Cited by in RCA: 170] [Article Influence: 17.0] [Reference Citation Analysis (0)] |