Published online Nov 26, 2020. doi: 10.12998/wjcc.v8.i22.5809
Peer-review started: September 1, 2020
First decision: September 12, 2020
Revised: September 17, 2020
Accepted: September 29, 2020
Article in press: September 29, 2020
Published online: November 26, 2020
Processing time: 85 Days and 4.7 Hours
Benign esophageal tumors are rare accounting for < 1% of esophageal tumors; two-thirds of which are leiomyomas. Esophageal leiomyoma is a benign tumor derived from mesenchymal tissue that is completely muscularly differentiated. Most esophageal leiomyomas are < 5 cm. Esophageal leiomyomas > 5 cm are rare. We describe a case of a large esophageal leiomyoma involving the cardia and diaphragm.
A 35-year-old woman presented to the doctor because of a choking sensation after eating. Physical examination showed no positive signs. Gastroscopy indicated an uplifted change in the cardia. Enhanced computed tomography revealed space-occupying lesions in the lower part of the esophagus and cardia, which were likely to be malignant. Positron emission tomography–computed tomography showed increased metabolism of soft tissue masses in the lower esophagus and near the cardia. Malignant lesions were considered, and mesenchymal tumors were not excluded. Endoscopic ultrasonography was performed to examine a hypoechoic mass in the lower esophagus, which was unclear from the esophageal wall. Clinical evaluation suggested diagnosis of esophageal and cardiac stromal tumors. Finally, histological specimens obtained by endoscopic ultrasonography– fine needle aspiration suggested leiomyoma. The patient underwent laparoscopic local resection of the tumor. The postoperative pathological diagnosis was leiomyoma.
Endoscopic ultrasonography-fine needle aspiration is necessary for the diagnosis of gastrointestinal leiomyomas. It provides a strong basis for diagnosis of gastrointestinal tumors of unknown nature and origin.
Core Tip: Endoscopic ultrasonography–fine needle aspiration is necessary for the diagnosis of gastrointestinal leiomyomas. It provides a strong basis for diagnosis of gastrointestinal tumors of unknown nature and origin.
- Citation: Rao M, Meng QQ, Gao PJ. Large leiomyoma of lower esophagus diagnosed by endoscopic ultrasonography–fine needle aspiration: A case report. World J Clin Cases 2020; 8(22): 5809-5815
- URL: https://www.wjgnet.com/2307-8960/full/v8/i22/5809.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i22.5809
Benign esophageal tumors are rare accounting for < 1% of esophageal tumors; two-thirds of which are leiomyomas[1-3]. Leiomyomas are the most common benign esophageal tumors. Leiomyoma is common in middle-aged patients with a male to female ratio of 2:1. Leiomyomas < 5 cm are mostly asymptomatic and discovered accidentally. The larger the leiomyoma, the more likely it is to show symptoms, such as dysphagia and chest pain. Most leiomyomas do not need treatment, but regular follow-up observation; if large leiomyomas cause symptoms, resection is required.
The pathology of leiomyoma is characterized by intersecting spindle cells with rich cytoplasm, and the malignant potential is low. In immunohistochemical examination, the specific signs of leiomyoma are diffuse positivity for desmin and smooth muscle actin (SMA) and negativity for CD34 and CD117. Abdominal computed tomography (CT) and endoscopic ultrasound (EUS) can diagnose most upper gastrointestinal leiomyomas, but there are still some difficulties in the diagnosis of atypical lesions, which can easily be misdiagnosed as stromal tumors and other malignant lesions. Tumor histological specimens can be obtained through EUS–fine needle aspiration (FNA), which provide a strong basis for the diagnosis of gastrointestinal tumors of unknown nature and origin.
Here we report a case of large esophageal leiomyoma. The CT and endoscopic findings of this case were close to those of stromal tumors. However, through EUS–FNA examination, the final diagnosis was leiomyoma.
A 35-year-old woman with hiccups and belching for > 30 years presented at the hospital because of choking and foreign body sensation during eating over the past 10 d. Abdominal CT and gastroscopy had not previously been performed.
The patient has experienced choking and foreign body sensation during eating over the past 10 d.
Patient has no relevant past medical history.
Patient has no relevant family history.
There were no positive signs.
No abnormalities were found by blood biochemical examination.
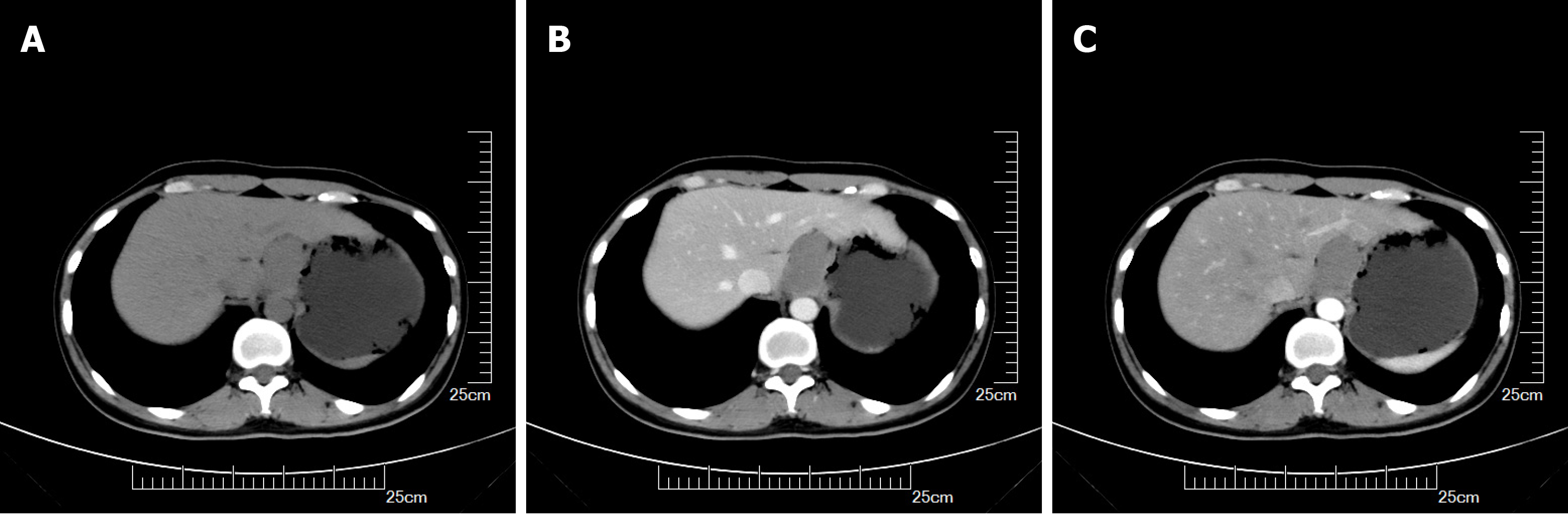
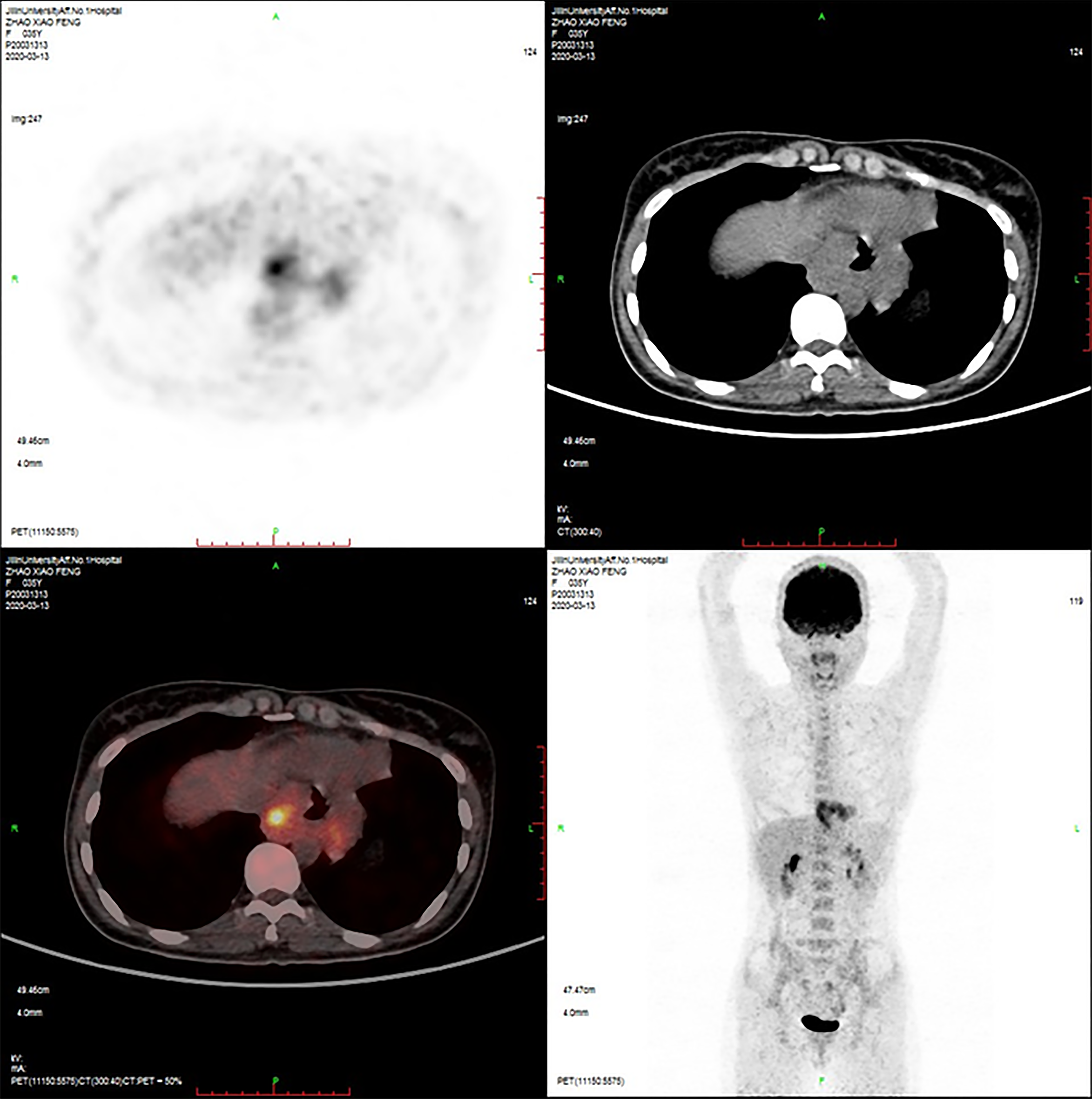
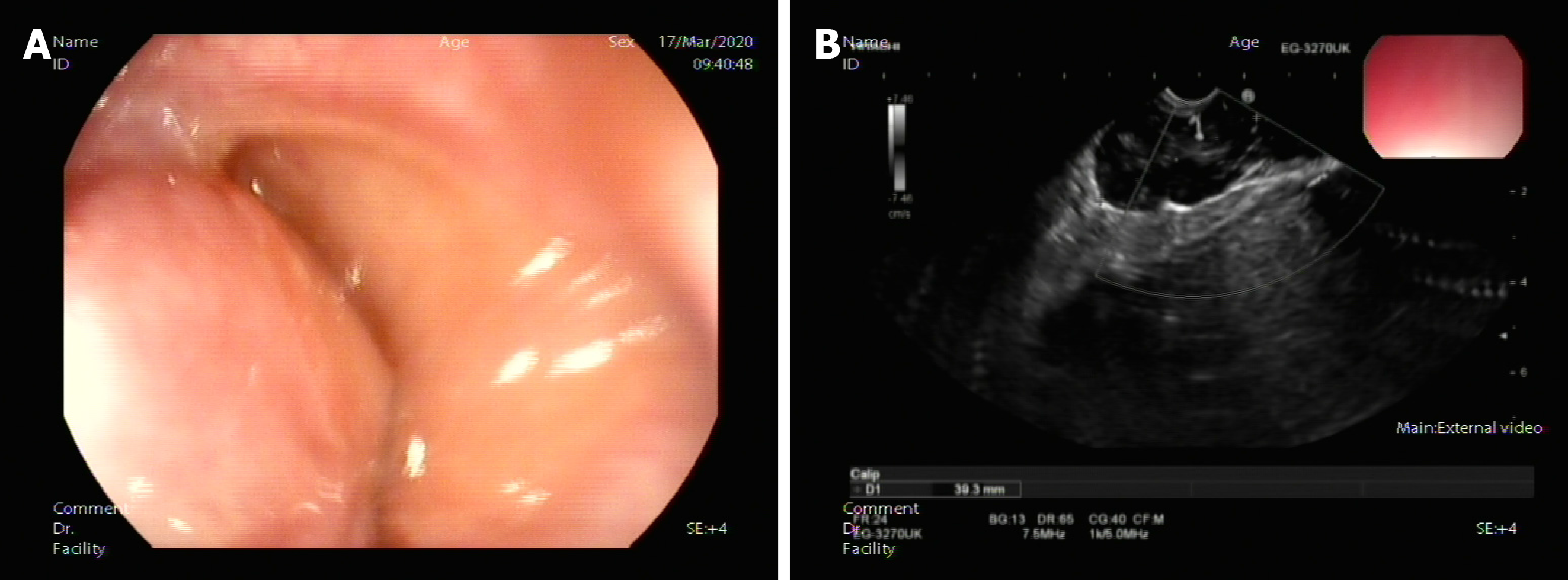
Gastroscopy showed uplifted changes in the cardia. Contrast-enhanced CT of the stomach (Figure 1) indicated space-occupying lesions in the lower esophagus and cardia, which were likely to be malignant. Positron emission tomography–CT (Figure 2) showed increased metabolism of soft tissue masses in the lower esophagus and near the cardia. Malignant lesions were considered, and mesenchymal malignant tumors were not excluded. EUS (Figure 3) examined the lower part of the esophagus near the cardia, and a hypoechoic mass was seen close to the esophageal wall growing outward. The internal echo was uneven, and there was no echo in some parts. Blood flow signals were seen inside. The mass was close to the liver and diaphragm, and the longest diameter of the section was approximately 4.9 cm. EUS diagnosed a hypoechoic mass in the lower esophagus with an unclear boundary with the esophageal wall. Combined with the above examinations, preoperative assessment was a probable stromal tumor. The tumor was large and involved the diaphragm and liver, thus making surgery difficult. Preoperative FNA examination was recommended to determine the treatment plan.
Postoperative pathological diagnosis was leiomyoma.
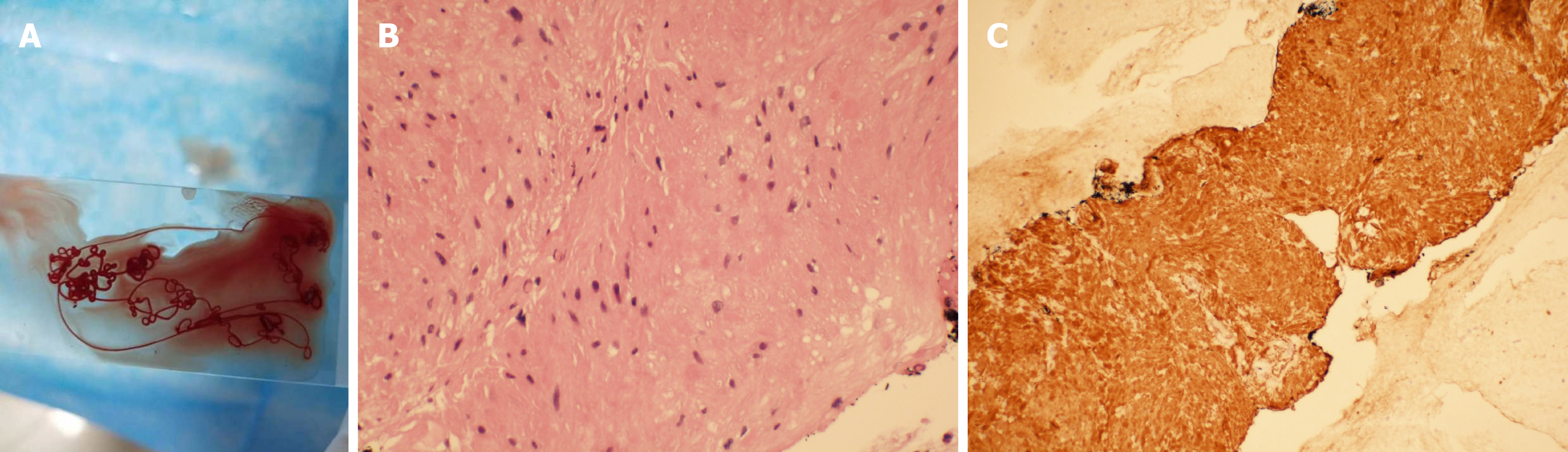
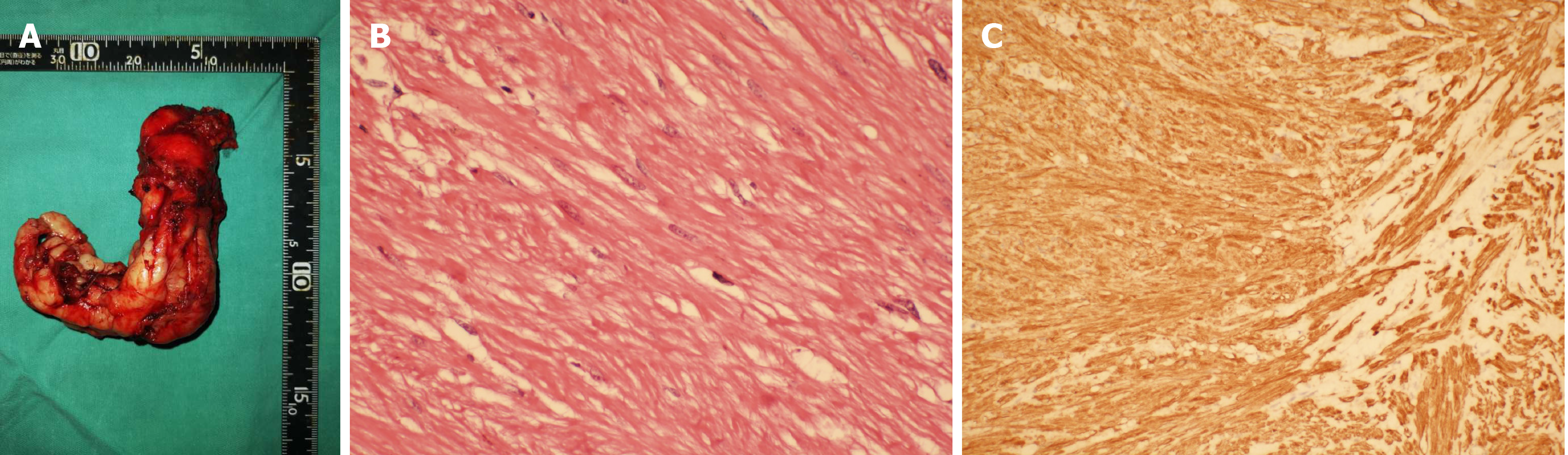
The patient agreed to undergo EUS–FNA examination. Under EUS, a puncture needle was placed in the lower part of the esophagus near the cardia and pierced the center of the tumor. A strip of tissue was obtained and sent for pathological examination (Figure 4A). Pathological examination showed a large amount of mucus-like tissue that included a small amount of smooth muscle tissue (Figure 4B). Immunohistochemistry showed: SMA (+), desmin (+), H-caldesmon (+), CD117 (-), Dog-1 (-), S-100 (-), CD34 (-), CKpan (-), SDHB (+) and Ki-67 (+ < 1%) (Figure 4C). Histological and immunohistochemical results suggested that the tumor was leiomyoma. Laparoscopic local resection of the mass was performed (Figure 5A). The postoperative pathological diagnosis was leiomyoma (tumor volume 8.0 cm × 6.0 cm × 3.5 cm) (Figure 5B). Immunohistochemistry showed: CD34 (-), desmin (+), H-caldesmon (+), Ki-67 (+1%), SDHB (+), SMA (+), CD117 (-), Dog-1 (-) and S-100 (-) (Figure 5C). These findings were consistent with the results of EUS-FNA before surgery.
The patient recovered well after the operation, and there is no information for review at present.
Benign esophageal tumors are rare accounting for < 1% of esophageal tumors; two-thirds of which are leiomyomas[1-3]. The rest are mostly cysts (20%), polyps (5%), gastrointestinal stromal tumors (< 5%) and lipomas (< 1%)[4,5]. Leiomyoma is the most common benign tumor of the esophagus. Esophageal leiomyomas are common in middle-aged patients, and the male to female ratio is 2:1[2,6]. Leiomyomas < 5 cm are mostly asymptomatic and discovered accidentally. The larger the leiomyoma, the more likely it is to show symptoms, such as dysphagia and chest pain[7-10]. The pathology of leiomyoma is characterized by intersecting spindle cells with rich cytoplasm, and the malignant potential is low. In immunohistochemical examination, the specific signs of leiomyoma are diffuse positivity for desmin and SMA and negativity for CD34 and CD117[11,12].
For most esophageal leiomyomas, the most common imaging test is upper gastrointestinal barium meal or esophagography because it is the least invasive, simplest and most common examination method[13-15]. As a noninvasive investigation method, CT examination has high diagnostic accuracy for space-occupying lesions of the digestive system and can make an accurate assessment of the exact location, size, range and distribution of blood vessels of the lesion. The CT findings of leiomyomas are soft tissue masses with clear boundaries. The tumors are of various shapes. The common growth patterns are intracavitary and transmural inside and outside the cavity. The mass density is uniform on CT scan, and enhanced scanning shows mild to moderate uniform enhancement. Compared with stromal tumors, leiomyomas have fewer ulcers[12].
EUS is currently an important diagnostic method for esophageal leiomyoma. Under EUS, leiomyomas mostly originate in the muscularis mucosa with smooth surface mucosa and mostly show uniform hypoechoic lesions. EUS is more accurate for diagnosis of lesions derived from the muscularis mucosa and muscularis propria. Previous studies have suggested that EUS makes a diagnosis based on factors such as the location, level of origin, size, echo intensity, uniformity, boundary and relationship with surrounding organs of the submucosal mass, and its specificity is 80%-88%[16,17]. Esophageal lesions from the muscularis mucosa or the muscularis propria are mainly leiomyomas, and only a few lesions derived from the muscularis propria are stromal tumors. The proportion of esophageal stromal tumors is < 7%[18]. Although EUS provides important information for identifying submucosal masses in the upper gastrointestinal tract, it still has some limitations. The main problem is that judgment of the origin level of the tumor does not match the actual situation. This may be related to incorrect operation and subjective misjudgment of the operator.
For atypical upper gastrointestinal tumors, pathological diagnosis is still the gold standard when CT and EUS imaging findings are uncertain. EUS–FNA examination not only finds submucosal lesions and accurately determines their origin, size and echogenicity, but also directly punctures larger lesions to obtain materials for histological and cytological examination and immunohistochemical staining. It is reported in the literature that the diagnostic accuracy of EUS–FNA for upper gastrointestinal submucosal masses is 95.6%, and its accuracy, sensitivity and specificity in distinguishing benign from potentially malignant lesions are 94.2%, 92.4% and 100.0%, respectively. Combined with immunohistochemical staining, the diagnostic accuracy rate can reach 98%[19-21]. This shows that EUS–FNA is an effective means to accurately diagnose this type of tumor.
For most upper gastrointestinal leiomyomas, diagnosis is not difficult by barium meal imaging, CT, EUS and other methods. However, the leiomyoma in the present case had the following characteristics. The tumor was large, wide, started from the lower esophagus, involved the cardia and reached the abdominal cavity next to the diaphragm and liver. The boundary with the diaphragm was unclear and the tumor grew outward. Enhanced scanning showed different degrees of enhancement; the echo was not uniform with an abundant blood flow signal within the tumor. These clinical features are more likely to be the characteristics of stromal tumors and other malignant lesions and are less common in leiomyomas. If EUS–FNA is not performed, histological specimens cannot be obtained, which may cause misdiagnosis and miss the opportunity for surgical treatment. Through this case, we have gained more understanding of large leiomyoma of the upper digestive tract and have provided more clinical indicators for diagnosis and treatment of the disease.
Abdominal computed tomography and EUS have high diagnostic accuracy for most upper gastrointestinal leiomyomas, but there are still difficulties in the diagnosis of atypical lesions, which can be misdiagnosed as stromal tumors and other malignant lesions. For the diagnosis of such lesions, EUS–FNA is necessary. EUS–FNA examination provides a strong basis for the diagnosis of gastrointestinal tumors of unknown nature and origin. The results are consistent with surgical pathological examination and provide good clinical indicators for final diagnosis and treatment.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bello BL, Yoshio S S-Editor: Zhang L L-Editor: Filipodia P-Editor: Xing YX
| 1. | Jiang W, Rice TW, Goldblum JR. Esophageal leiomyoma: experience from a single institution. Dis Esophagus. 2013;26:167-174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 37] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 2. | De Giacomo T, Bruschini P, Arcieri S, Ruberto F, Venuta F, Diso D, Francioni F. Partial oesophagectomy for giant leiomyoma of the oesophagus: report of 7 cases. Eur J Cardiothorac Surg. 2015;47:143-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 3. | Shin S, Choi YS, Shim YM, Kim HK, Kim K, Kim J. Enucleation of esophageal submucosal tumors: a single institution's experience. Ann Thorac Surg. 2014;97:454-459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 53] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 4. | Yekeler E, Yazicioglu A, Subasi M, Boztepe H. Giant Esophageal Lipoma as an Uncommon Cause of Diverticula. Case Rep Gastroenterol. 2016;10:446-451. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Neoral C, Aujeský R, Skarda J, Vrba R, Chudáček J, Bohanes T, Vomáčková K. Thoracoscopic treatment of benign esophageal tumors. Wideochir Inne Tech Maloinwazyjne. 2012;7:294-298. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Lee LS, Singhal S, Brinster CJ, Marshall B, Kochman ML, Kaiser LR, Kucharczuk JC. Current management of esophageal leiomyoma. J Am Coll Surg. 2004;198:136-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 92] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 7. | Cheng BC, Chang S, Mao ZF, Li MJ, Huang J, Wang ZW, Wang TS. Surgical treatment of giant esophageal leiomyoma. World J Gastroenterol. 2005;11:4258-4260. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 19] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (1)] |
| 8. | Peters JH, DeMeester TR. Esophagus and diaphragmatic hernia. In: Brunicardi FC, Andersen KD, Billiar RT. Schwartz’s Principles of Surgery. New York, NY, USA: McGraw-Hill; 2005: 906. Available from: http://www.docin.com/p-734249480.html. |
| 9. | Guo J, Liu Z, Sun S, Liu X, Wang S, Ge N. Ligation-assisted endoscopic enucleation for treatment of esophageal subepithelial lesions originating from the muscularis propria: a preliminary study. Dis Esophagus. 2015;28:312-317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Sun X, Wang J, Yang G. Surgical treatment of esophageal leiomyoma larger than 5 cm in diameter: A case report and review of the literature. J Thorac Dis. 2012;4:323-326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 18] [Reference Citation Analysis (0)] |
| 11. | Deshpande A, Nelson D, Corless CL, Deshpande V, O'Brien MJ. Leiomyoma of the gastrointestinal tract with interstitial cells of Cajal: a mimic of gastrointestinal stromal tumor. Am J Surg Pathol. 2014;38:72-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 23] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 12. | Yang HK, Kim YH, Lee YJ, Park JH, Kim JY, Lee KH, Lee HS. Leiomyomas in the gastric cardia: CT findings and differentiation from gastrointestinal stromal tumors. Eur J Radiol. 2015;84:1694-1700. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 13. | Perwaiz A, Shaw VK, Singh A, Chaudhary A. Extra-mucosal enucleation is still a safe and feasible treatment option of giant esophageal leiomyomas. Indian J Gastroenterol. 2018;37:63-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Kohli DR, Faigel DO. Esophageal leiomyomas: Making mole hills out of mole hills? Gastrointest Endosc. 2018;87:378-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 15. | Lipnickas V, Beiša A, Makūnaitė G, Strupas K. Laparoscopic approach in the treatment of large leiomyoma of the lower third of the esophagus. Wideochir Inne Tech Maloinwazyjne. 2017;12:437-442. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 16. | Rösch T, Kapfer B, Will U, Baronius W, Strobel M, Lorenz R, Ulm K; German EUS Club. Endoscopic ultrasonography. Accuracy of endoscopic ultrasonography in upper gastrointestinal submucosal lesions: a prospective multicenter study. Scand J Gastroenterol. 2002;37:856-862. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 90] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 17. | Will U, Fueldner F, Mueller AK, Meyer F. A prospective study on endoscopic ultrasonography criteria to guide management in upper GI submucosal tumors. Pol Przegl Chir. 2011;83:63-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 18. | Franco MC, Schulz RT, Maluf-Filho F. Opinion: How to manage subepithelial lesions of the upper gastrointestinal tract? World J Gastrointest Endosc. 2015;7:1262-1267. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 7] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 19. | Moon JS. Endoscopic ultrasound-guided fine needle aspiration in submucosal lesion. Clin Endosc. 2012;45:117-123. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 41] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 20. | Mekky MA, Yamao K, Sawaki A, Mizuno N, Hara K, Nafeh MA, Osman AM, Koshikawa T, Yatabe Y, Bhatia V. Diagnostic utility of EUS-guided FNA in patients with gastric submucosal tumors. Gastrointest Endosc. 2010;71:913-919. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 177] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 21. | Akahoshi K, Oya M, Koga T, Koga H, Motomura Y, Kubokawa M, Gibo J, Nakamura K. Clinical usefulness of endoscopic ultrasound-guided fine needle aspiration for gastric subepithelial lesions smaller than 2 cm. J Gastrointestin Liver Dis. 2014;23:405-412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 81] [Article Influence: 8.1] [Reference Citation Analysis (0)] |