Published online Nov 6, 2020. doi: 10.12998/wjcc.v8.i21.5432
Peer-review started: May 20, 2020
First decision: September 14, 2020
Revised: September 17, 2020
Accepted: September 29, 2020
Article in press: September 29, 2020
Published online: November 6, 2020
Processing time: 168 Days and 18.1 Hours
Hyperkalemia is one of the most common complications of chronic renal failure. Pseudohyperkalemia is caused by elevated levels of serum potassium in vitro and is usually accompanied by thrombocythemia. Although an elevated level of potassium is typically correlated with impaired renal function, pseudo-hyperkalemia has been rarely reported in patients with chronic renal failure. Here, we conducted a review of the literature to study the case of pseudo-hyperkalemia caused by the essential thrombocythemia in a patient with chronic renal failure.
A 73-year-old woman was admitted to our hospital with complaints of palpitation, dyspnea, and acratia for 2 d and a history of essential throm-bocythemia for 1 year. The routine blood test showed platelet count of 1460 × 109/L, and biochemistry tests showed that the patient suffered from hyperkalemia (potassium: 7.50 mmol/L) and renal failure (estimated glomerular filtration rate: 8.88 mL/min). Initial treatment included medicines to lower her potassium-levels and hemodialysis. However, the therapy did not affect her serum potassium levels. Plasma potassium concentration measurements and a history of essential thrombocythemia established the diagnosis of pseudohyperkalemia. The treatments of the platelet disorder gradually normalized serum potassium levels; however, the treatments had to be discontinued later due to the severe leukopenia, and enhanced levels of serum potassium concentrations were observable in the patient. Since plasma sampling was not permitted, doctors had to use a diuretic just in case. Finally, the patient collapsed into unconsciousness and died due to multiple organ dysfunction and electrolyte disturbance.
We reviewed the literature and suggest that serum and plasma potassium values should both be measured for patients whose platelet counts exceed 500 × 109/L to eliminate chances of pseudohyperkalemia, especially for those with chronic renal failure. An inappropriate treatment for pseudohyperkalemia can aggravate a patient's condition.
Core Tip: Pseudohyperkalemia in patients with chronic renal failure has been rarely reported, as an elevated level of potassium is typically correlated with impaired renal function. Herein, we studied pseudohyperkalemia caused by thrombocythemia in a patient suffering from chronic renal failure. A review of the literature is also provided to improve the overall awareness of the phenomenon in these patients. To our knowledge, our study was the first related literature review, and is the first to report the therapeutic process and outcome for an essential thrombocythemia patient with chronic renal failure.
- Citation: Guo Y, Li HC. Pseudohyperkalemia caused by essential thrombocythemia in a patient with chronic renal failure: A case report. World J Clin Cases 2020; 8(21): 5432-5438
- URL: https://www.wjgnet.com/2307-8960/full/v8/i21/5432.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i21.5432
Hyperkalemia is a potentially life-threatening condition that needs to be treated[1]. Chronic renal failure is the most common reason for potassium elevation[2]. Pseudohyperkalemia is caused by elevated levels of serum potassium in vitro, and specific treatment is inappropriate[1]. Thrombocythemia is often associated with this artificial potassium increase[3]. Pseudohyperkalemia in patients with chronic renal failure has been rarely reported, as elevated potassium levels are usually associated with the impaired renal function. Herein, we studied pseudohyperkalemia caused by thrombocythemia in a patient suffering from chronic renal failure. To identify the timely detection of treatment alternatives for patients who showed poor prognosis, we reviewed three cases from the literature databases of pseudohyperkalemia in patients with chronic renal failure caused by an increase of platelets. To our knowledge, we are the first group to report the therapeutic process and outcomes of an essential thrombocythemia patient suffering from chronic renal failure.
A 73-year-old woman with symptoms such as palpitation, dyspnea, and acratia for 2 d was referred to the Emergency Department of our hospital on May 28, 2019.
The patient was diagnosed with essential thrombocythemia (Janus kinase 2 V617F mutation) 1 year ago, and the symptoms of palpitation, dyspnea, and acratia were detected within the past 2 d. The routine blood test showed that her platelet count was 1205 × 109/L, and its reference range (RR) was 125-350 × 109/L. She was transferred to the Hematology Department for further treatments on May 29, 2019.
The patient had a history of hypertension for 8 years. Renal insufficiency and cerebrovascular stenosis were diagnosed 4 years ago; however, her blood pressure was in control. She had aspirin irregularly, and the drug was discontinued due to purpura.
Slight pitting edema on both legs was revealed upon physical examination. Other remarkable abnormalities were not found. Vital signs were within normal limits, with a temperature of 36.7 °C, heart rate of 80 beats/min, respiratory rate of 18 breaths/min, and blood pressure of 120/63 mmHg.
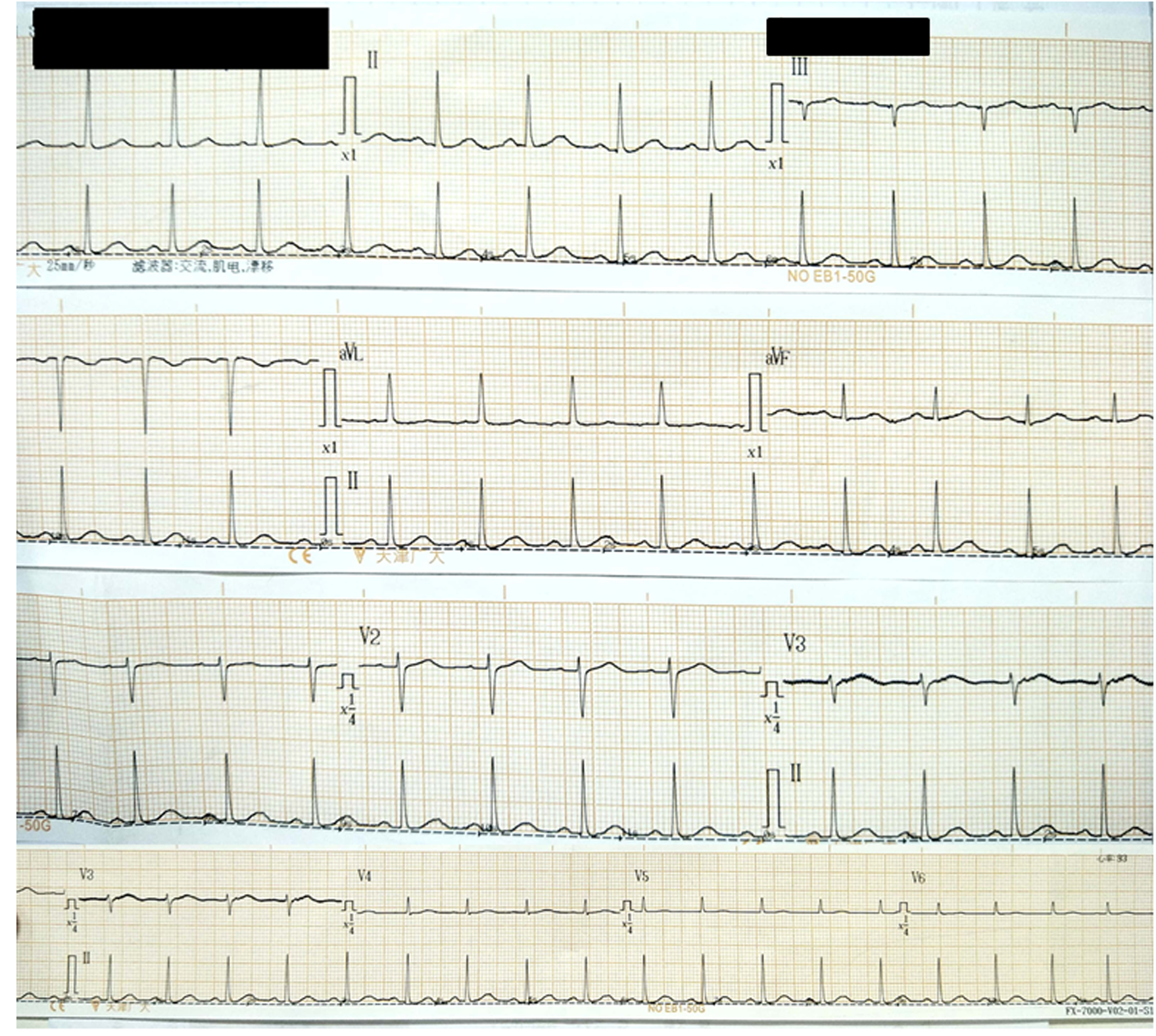
Repeated routine blood test showed white blood cell count of 51.4 × 109/L (RR: 3.50-9.50 × 109/L), hemoglobin of 60 g/L (RR: 115-150 g/L), and platelet count of 1460 × 109/L. Blood biochemistry tests showed that the patient suffered from hyperkalemia (potassium: 7.50 mmol/L, RR: 3.60-5.00 mmol/L) and renal failure (urea nitrogen: 16.63 mmol/L, RR: 2.50-6.10 mmol/L; creatinine: 579 μmol/L, RR: 40-97 μmol/L; uric acid: 2578 μmol/L, RR: 149-446 μmol/L; estimated glomerular filtration rate (eGFR): 8.88 mL/min, RR: > 90.00 mL/min). Twelve lead resting electrocardiography results were normal.
The patient was diagnosed with essential thrombocythemia, chronic renal failure, and hyperkalemia.
The patient was diagnosed with essential thrombocythemia, chronic renal failure, and hyperkalemia.
Treatment was initiated with insulin and glucose, calcium gluconate, and sodium bicarbonate. However, the therapy did not affect her serum potassium level, which was still high on the next day (8.27 mmol/L). Physicians attributed the refractory hyperkalemia to her renal failure and decided to perform hemodialysis. One day later, the level of creatinine fell to 268 μmol/L, but serum potassium concentration still fluctuated from 7.11 to 7.83 mmol/L.
Considering her high platelet counts and normal electrocardiogram (Figure 1), we inferred that the patient had pseudohyperkalemia caused by platelet clotting. Therefore, we collected two blood samples after three consecutive hemodialysis treatments. One sample was drawn into vacuum tubes with clot activator and gel separator, and the other one was injected into tubes coated with lithium heparin. Results showed that the potassium concentrations in serum were 2.35, 2.33, and 1.23 mmol/L higher than those in plasma in three tests, respectively, which verified the diagnosis of pseudohyperkalemia (Table 1).
| June 1st | June 3rd | June 4th | ||||
| Serum | Plasma | Serum | Plasma | Serum | Plasma | |
| Potassium, mmol/L | 6.32 | 3.97 | 5.42 | 3.09 | 5.20 | 3.97 |
| Sodium, mmol/L | 135.7 | 137.3 | 136.9 | 137.8 | 135.5 | 137.3 |
| Chloride, mmol/L | 91.5 | 96.6 | 91.0 | 91.1 | 91.9 | 96.6 |
| Calcium, mmol/L | 2.34 | 2.30 | 2.32 | 2.25 | 2.62 | 2.30 |
| Urea nitrogen, mmol/L | 3.64 | 4.63 | 8.78 | 8.68 | 7.11 | 8.87 |
| Creatinine, μmol/L | 220 | 240 | 469 | 481 | 346 | 315 |
| Uric acid,μmol/L | 541 | 606 | 2252 | 2236 | 710 | 825 |
Following suggestions from the clinical laboratory, the patient was treated with hydroxyurea to reduce the amounts of platelets on June 1, 2019. She received diuretics therapy (furosemide) at the same time. Consequently, the serum potassium concentrations decreased and were even lower than RR levels for a few days. The hydroxyurea treatment was discontinued on June 23, 2019, since the patient showed severe leukopenia (white blood cell count: 1.8 × 109/L). As expected, the platelet counts and serum potassium concentrations began to increase gradually, while the serum creatinine concentrations were relatively stable. On July 16, 2019, her platelet counts increased to 1386 × 109/L, and serum potassium concentration became 6.90 mmol/L. Her family members declined our initiative to collect her blood for plasma potassium concentration measurement, so physicians had to add another diuretic (torasemide) to reduce further her serum potassium level. Meanwhile, homo-harringtonine was used to control platelet counts. Details are shown in Figure 2 and Table 2.
| Creatinine, μmol/L | Potassium, mmol/L | Platelets, × 109/L | |
| June 6th | 375 | 3.13 | 1411 |
| June 7th | 473 | 3.89 | 1122 |
| June 8th | 514 | 3.32 | 933 |
| June 9th | 555 | 3.44 | 911 |
| June 12th | 714 | 3.65 | 855 |
| June 14th | 651 | 3.48 | 819 |
| June 15th | 640 | 5.45 | 811 |
| June 16th | 608 | 4.55 | 701 |
| June 17th | 651 | 4.37 | 725 |
| June 18th | 477 | 2.88 | 605 |
| June 20th | 417 | 3.58 | 534 |
| June 21st | 446 | 3.31 | 486 |
| June 22nd | 393 | 3.06 | 408 |
| June 23rd | 371 | 3.14 | 324 |
| June 24th | 359 | 3.25 | 303 |
| June 25th | 300 | 3.64 | 281 |
| June 26th | 318 | 3.45 | 266 |
| June 27th | 317 | 3.68 | 278 |
| June 28th | 315 | 3.58 | 279 |
| June 30th | 336 | 3.42 | 313 |
| July 1st | 306 | 3.32 | 310 |
| July 2nd | 311 | 3.89 | 351 |
| July 3rd | 310 | 3.94 | 356 |
| July 4th | 320 | 4.75 | 512 |
| July 5th | 315 | 4.26 | 635 |
| July 7th | 331 | 4.60 | 656 |
| July 8th | 249 | 4.79 | 607 |
| July 9th | 295 | 4.85 | 778 |
| July 10th | 249 | 4.79 | 761 |
| July 11th | 245 | 5.22 | 919 |
| July 12th | 269 | 5.71 | 965 |
| July 13th | 276 | 6.00 | 1278 |
| July 14th | 287 | 6.90 | 1386 |
| July 18th | 287 | 4.57 | 1192 |
| July 20th | 352 | 3.72 | 1281 |
The patient collapsed into unconsciousness on July 19, 2019. Her family members refused favorable treatment options, and she died on August 8, 2019 due to multiple organ dysfunction and electrolyte disturbance.
Chronic kidney disease (CKD) is a potential causes of hyperkalemia. Among patients with eGFR < 60.00 mL/min, the rate of hyperkalemia (potassium: ≥ 5.50 mmol/L) and the risk of severe hyperkalemia (potassium: ≥ 6.00 mmol/L) were reported to be 8.2 events/100 patient-months and 2.6 events/100 patients-months, respectively. Such an observation represented a five-times increase in risk as compared to those without CKD[4]. When the CKD progressed to renal failure (eGFR < 30 mL/min), the odds ratio of hyperkalemic events was 5.91 (95% confidence interval: 5.63-6.20) to 11.00 (95% confidence interval: 10.34-11.69)[5]. In this case, the patient showed a history of chronic renal failure (eGFR = 8.88 mL/min) and increased serum potassium concentration (7.50 mmol/L) at the time of admission. Therefore, the diagnosis of hyperkalemia was plausible.
The thrombocythemia could cause hyperkalemia in vitro, and this is termed pseudohyperkalemia. Platelets in the blood samples can affect the potassium measurement when the counts exceeded 450 × 109/L[6]. At a platelet count of 500 × 109/L or higher, 14% of samples are typically affected by pseudohyperkalemia[7]. The activation of excess platelets during blood coagulation in the pro-coagulation tubes has been reported to be mainly responsible for the spurious hyperkalemia[6]. Moreover, mechanical stress, such as centrifugation, can result in breakage of platelets, which could be another reason for the artificial increase in potassium concentration[8]. Pseudohyperkalemia should be taken into account when the potassium concentration in serum is at least 0.40 mmol/L higher than those in plasma[9]. For the needs of practical application, the discrepancy of 1.00 mmol/L between serum and plasma was recommended[8]. In this case, serum potassium levels exceeded those of plasma by at least 1.00 mmol/L at three different blood sampling time points, which verified the occurrence of pseudohyperkalemia.
However, the patient was not diagnosed with pseudohyperkalemia at first since she had a history of renal failure. Doctors chose to lower actively the patient's serum potassium on a "just in case" basis, primarily due to concern about severe consequences of hyperkalemia. Unfortunately, kayexalate administration was invalidated, which brought potential risks to the disease progression.
In order to identify timely pseudohyperkalemia in thrombocytosis patients with chronic renal failure, we turned to the literature database for help. We systematically searched for relevant cases in the MEDLINE database (via PubMed) [1946 to current], EMBASE [1974 to current] and Web of Science [1990 to current] with the following search terms: ("pseudohyperkalemia" OR "spurious hyperkalemia" OR "artificial hyperkalemia") AND ("blood Platelets" OR "blood platelets" OR "blood platelet" OR "thrombocytes" OR "thrombocyte" OR "platelets" OR "platelet" OR "thrombocytosis"). Forty studies were retrieved from the aforementioned databases. After browsing the titles and abstracts, three cases met the inclusion criteria and were analyzed[8,10,11]. In these cases, the patients' age ranged from 50 years to 62 years, and one patient was male. One patient complained about shortness of breath, nausea, and vomiting, while the other two presented to the hospital due to gastric ulcer bleeding with hemorrhagic shock and persistent hyperkalemia, respectively. All three cases had chronic renal failure. Two of these patients were diagnosed with essential thrombocythemia (Janus kinase 2 V617F mutation), and the other one showed increased platelet counts but refused bone marrow biopsy. Other medical history included diabetes mellitus, chronic hepatic disease, hypertension, atrial fibrillation, supraventricular tachycardia, and advanced chronic obstructive pulmonary disease. The first case believed that their patient had pseudohyperkalemia because of the relationship between serum potassium and platelet counts, but they did not measure her plasma potassium levels. In the second case, pseudohyperkalemia was suspected only when dialysis failed to lower the serum potassium concentration and was demonstrated by a difference of 2.60 mmol/L between serum and plasma potassium values. The case is similar to our study, in that both patients received some unnecessary treatments. In the third case, they set checkpoint levels in reporting laboratory test results. Since the increased potassium levels were not affected by hemolysis, an interpretative comment was added for the third case: Pseudohyperkalemia due to thrombocytosis is suspected. New samples in lithium heparin tubes were then collected, and the patient was freed from the inappropriate therapies. Therefore, we should learn from the checkpoint level system, which recommended regular serum and plasma potassium measurements for thrombocythemia patients to rule out the pseudohyperkalemia, especially for those with chronic renal failure. The cut-off value of increased platelet count was 500 × 109/L[7].
The added value of our case is the description of the total therapeutic process for a thrombocythemia patient with chronic renal failure and the presentation of her outcomes. Medicines and dialysis failed to control the patient's "hyperkalemia", but treatment of the platelet disorder led to the normalization of serum potassium levels gradually. The relationship between cease of lowering the platelet counts and initiation of increasing in serum potassium values was also noticed. Therefore, thrombocythemia was mainly responsible for the elevated serum potassium levels and not the impaired renal function. Since plasma sampling was not permitted, doctors continued to use diuretics against the possible consequences induced by hyperkalemia. Jain et al[12] recommended that patients receive treatment only when they were symptomatic or when they show cardiac effects of hyperkalemia on electrocardiogram. Thus, potassium-lowering treatments might be inappropriate for our patient and might aggravate the patients' condition. There are still no formal guidelines for physicians to deal with platelet-related pseudohyperkalemia. They prefer to take positive steps even if the serum potassium was spuriously elevated, since the consequences of hyperkalemia are severe[12]. How to manage pseudohyperkalemia in thrombocythemia patients, especially those with renal failure, still requires further investigation with evidence-based studies.
In summary, we described a case of pseudohyperkalemia caused by the essential thrombocythemia in a patient with chronic renal failure and provide a review of the related literature. We suggest that serum and plasma potassium values should be measured for patients whose platelet counts exceeded 500 × 109/L to eliminate complications due to pseudohyperkalemia, especially for those with chronic renal failure. Inappropriate treatment to pseudohyperkalemia may aggravate the patients' condition and lead to a poor outcome.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Yorioka N S-Editor: Zhang L L-Editor: Filipodia P-Editor: Ma YJ
| 1. | Evans KJ, Greenberg A. Hyperkalemia: a review. J Intensive Care Med. 2005;20:272-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 103] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 2. | Gennari FJ. Disorders of potassium homeostasis. Hypokalemia and hyperkalemia. Crit Care Clin. 2002;18:273-288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 83] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 3. | Ong YL, Deore R, El-Agnaf M. Pseudohyperkalaemia is a common finding in myeloproliferative disorders that may lead to inappropriate management of patients. Int J Lab Hematol. 2010;32:e151-e157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Seliger SL. Hyperkalemia in patients with chronic renal failure. Nephrol Dial Transplant. 2019;34:iii12-iii18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 29] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 5. | Einhorn LM, Zhan M, Hsu VD, Walker LD, Moen MF, Seliger SL, Weir MR, Fink JC. The frequency of hyperkalemia and its significance in chronic kidney disease. Arch Intern Med. 2009;169:1156-1162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 443] [Cited by in RCA: 465] [Article Influence: 29.1] [Reference Citation Analysis (0)] |
| 6. | Roccaforte V, Daves M, Alfreijat A, Riva M, Leitner M, Filippi S, Angaroni G, Montani F, Platzgummer S, Lippi G. Spurious elevation of serum potassium concentration measured in samples with thrombocytosis. Diagnosis (Berl). 2016;3:71-74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Ranjitkar P, Greene DN, Baird GS, Hoofnagle AN, Mathias PC. Establishing evidence-based thresholds and laboratory practices to reduce inappropriate treatment of pseudohyperkalemia. Clin Biochem. 2017;50:663-669. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 33] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 8. | Šálek T. Pseudohyperkalemia - Potassium released from cells due to clotting and centrifugation - a case report. Biochem Med (Zagreb). 2018;28:011002. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 21] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 9. | Sevastos N, Theodossiades G, Archimandritis AJ. Pseudohyperkalemia in serum: a new insight into an old phenomenon. Clin Med Res. 2008;6:30-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 54] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 10. | Meka NP, Malik YO. Unexplained hyperkalemia: The tip of the iceberg. Am J Case Rep. 2012;13:125-127. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Ifudu O, Markell MS, Friedman EA. Unrecognized pseudohyperkalemia as a cause of elevated potassium in patients with renal disease. Am J Nephrol. 1992;12:102-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Jain AG, Tauseef A, Hasan SA, Jain SK, Wazir M, Majeed U. Pseudohyperkalemia: To Treat or not to Treat. Cureus. 2018;10:e3570. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |