Published online Nov 6, 2020. doi: 10.12998/wjcc.v8.i21.5426
Peer-review started: April 15, 2020
First decision: April 24, 2020
Revised: September 8, 2020
Accepted: September 16, 2020
Article in press: September 16, 2020
Published online: November 6, 2020
Processing time: 204 Days and 17 Hours
There is a common pathologic relationship between parathyroid adenoma and thyroid cancer, but this relationship is infrequent in pregnant patients with primary hyperparathyroidism (PHPT).
A 27-year-old gravida 1 woman was transferred to our hospital at 16 wk of pregnancy. She was diagnosed with parathyroidoma, papillary carcinoma of the thyroid and thyroid adenoma and was managed surgically. Both the mother and the newborn were stable after a right inferior parathyroidectomy and total thyroidectomy. The healthy infant was delivered at the 40th week of pregnancy. The mother had no evidence of recurrence over three years of follow-up.
Awareness of concomitant PHPT and thyroid diseases may help in managing patients with a history of hypercalcemia.
Core Tip: Primary hyperparathyroidism (PHPT) with parathyroid adenoma associated with papillary cancer and adenoma of the thyroid is unusual. The preliminary test results showed severe hypercalcemia. The level of parathyroid hormone found in further laboratory tests was elevated and a diagnosis of PHPT was determined. Right lower parathyroid gland and total thyroidectomy were performed. This clinical case illustrates the need for awareness of concomitant PHPT and thyroid diseases.
- Citation: Li Q, Xu XZ, Shi JH. Synchronous parathyroid adenoma, papillary thyroid carcinoma and thyroid adenoma in pregnancy: A case report. World J Clin Cases 2020; 8(21): 5426-5431
- URL: https://www.wjgnet.com/2307-8960/full/v8/i21/5426.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i21.5426
Thyroid disease with associated parathyroid disease was first reported, at the earliest, in 1947[1]. Primary hyperparathyroidism (PHPT) with parathyroid adenoma associated with papillary cancer and adenoma of the thyroid is unusual[2]. The most common etiology of hypercalcemia is PHPT, which is rarely diagnosed during pregnancy[2,3]. Thyroid cancer is the second most frequent malignant neoplasm during gravidity followed by breast cancer[3]. The accurate incidence during pregnancy continues to be a challenge[2]. This disorder contributes to 67% of conditions in pregnancy, and 80% of these conditions may result in symptoms in the fetus[4]. Maternal conditions include skeletal disease, renal calculus, pancreatic lithiasis, severe hyperemesis gravidarum, muscle weakness, altered mental status, and hyperglycemia[2]. Reported symptoms in fetuses include delayed fetal development, low birth weight, premature birth, intrauterine death, fetal dysplasia, and postpartum neonatal titanic crisis (with or without seizures)[2]. Therefore, early diagnosis and appropriate treatment are necessary[5]. Previous studies revealed that the rate of misdiagnosis was as high as 80% in pregnant women with PHPT, with abortion or stillbirth occurring before a definitive diagnosis[6].
To the best of our knowledge, similar cases have not been reported.
A 27-year-old woman who was 16 wk pregnant was transferred to our department, with abdominal pain and nonspecific symptoms.
The patient had abdominal pain with nonspecific symptoms such as nausea and vomiting and abnormalities during routine prenatal testing especially hypercalcemia. She denied weight loss during pregnancy.
Previously, she had three miscarriages. She also had a history of renal calculus and had normal kidney function.
No special personal and family history.
Fetal evaluation was normal.
The preliminary test results showed severe hypercalcemia with a serum calcium content of 3.48 mmol/L (13.9 mg/dL) and increased serum ionized calcium (1.9 mmol/L, 7.6 mg/dL), low phosphate concentration (1.3 mmol/L, 4.0 mg/dL) and calcuria (310 mg/24 h). The total magnesium content was low (1.4 mg/dL, 0.6 mmol/L). Thyroid function tests, electrocardiography and fetal evaluation were normal. The level of parathyroid hormone (PTH) (782 pg/mL; 6.0-80 pg/mL) assessed in further laboratory tests was elevated and the patient was diagnosed with PHPT.
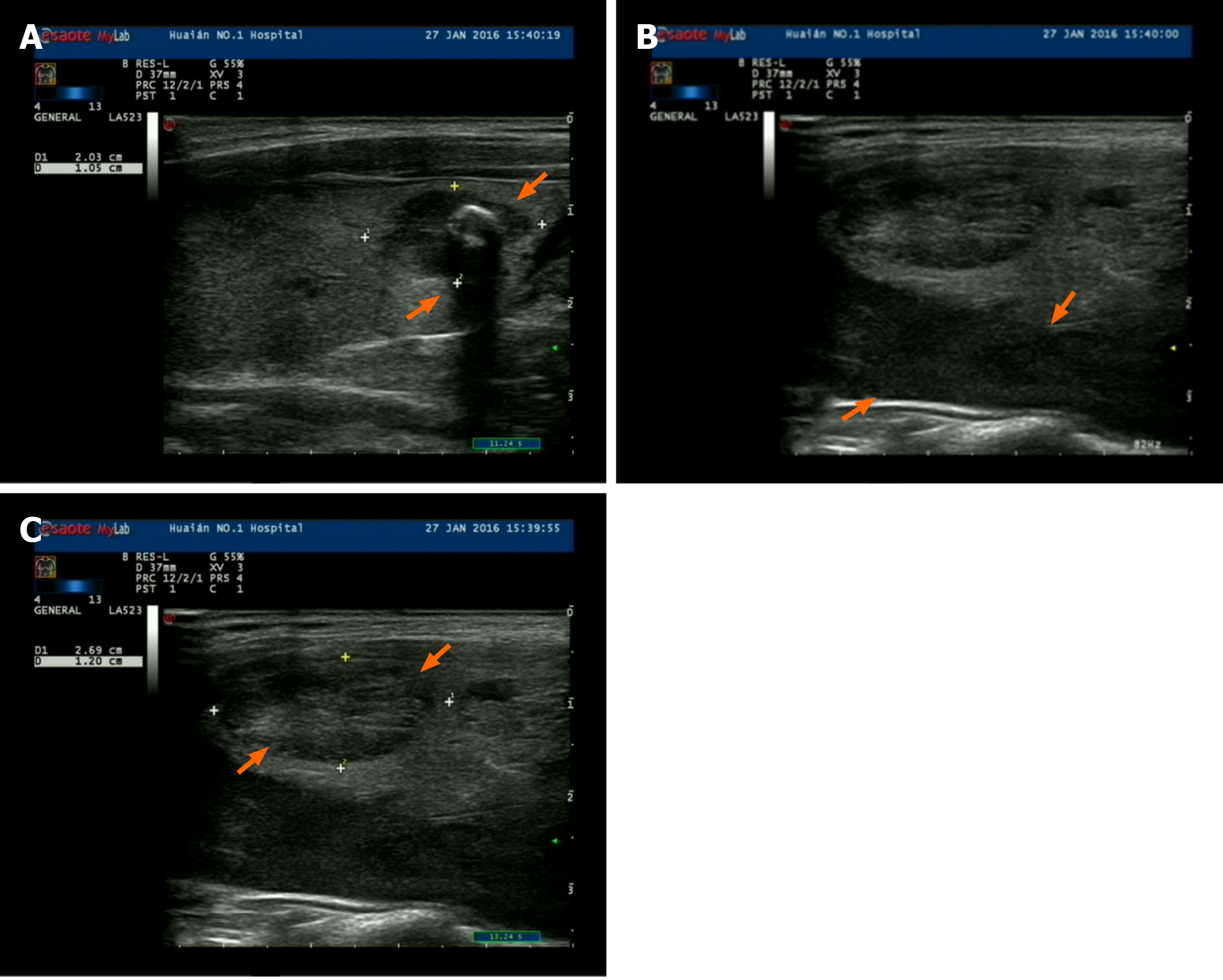
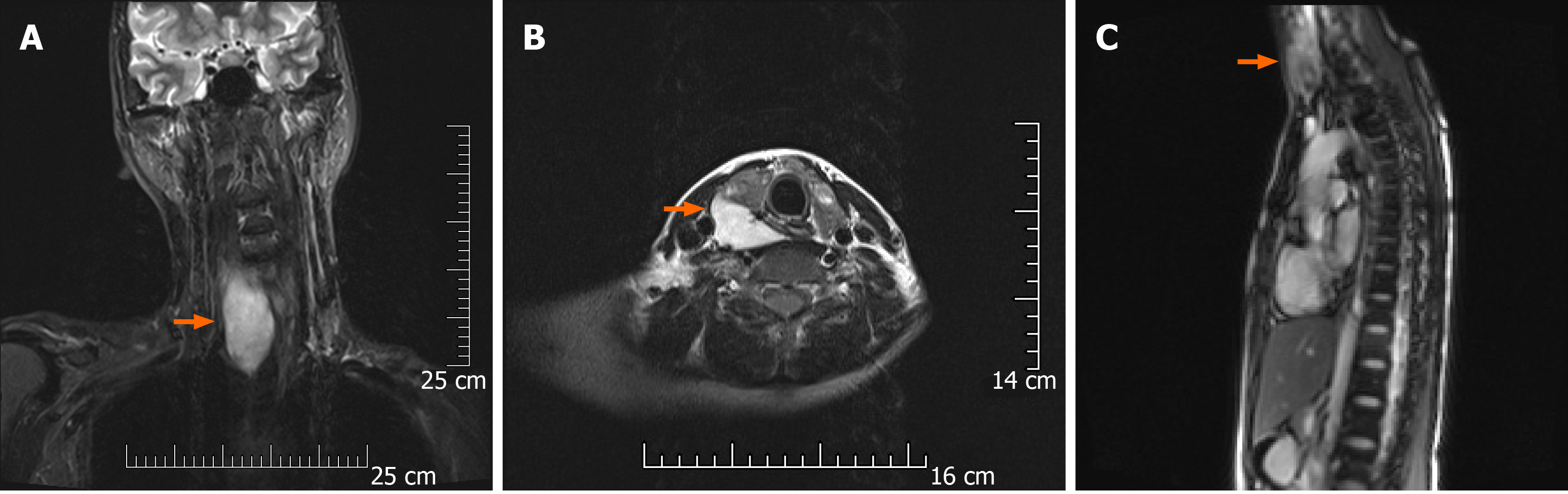
Cervical ultrasonography showed a multinodular goiter in the center of the right lobe of the thyroid, one in the lower third of the left lobe of the thyroid, a protruding solid nodule, and another 60 mm × 27 mm × 22 mm nodule with solid low echo (Figure 1) on the lateral side of the gland; however, this nodule was located close to the lower pole of the right lobe of the thyroid, indicative of a right inferior parathyroid adenoma. The parathyroid adenoma was diagnosed based on magnetic resonance imaging (MRI) (Figure 2) due to the presence of normal gastrin and normal plasma calcitonin, and as no abnormalities in the pituitary and bilateral adrenal glands were found on MRI, multiple endocrine neoplasia (MEN) syndrome was ruled out.
The histopathological results showed that a right inferior parathyroid adenoma (greatest diameter 6.0 cm, Figure 3A), a left lower lobe thyroid papillary carcinoma (follicular variant, greatest diameter 1.2 cm, Figure 3B) and multiple thyroid follicular adenomas were present (Figure 3C).
Initial clinical procedures included forced rehydration, furosemide, and supple-mentation with magnesium and phosphorus to reduce blood calcium levels. Serum calcium levels decreased to 2.68 mmol/L (10.7 mg/dL).
The nuclear groove and inclusion body were visible on histopathological examination of fine-needle aspiration biopsy (FNAB), and these findings were highly suggestive of papillary thyroid carcinoma. As the combination of FNAB and hypercalcemia may cause abnormalities in the mother and fetus, surgical treatment was performed under basic anesthesia in the 18th wk of pregnancy.
During the operation, rapid pathological assessment showed left lobe papillary carcinoma of the thyroid. Furthermore, the infiltration of lymphocytes could be seen in the surrounding tissues, and the formation of a thyroid adenoma was also observed. Right lower parathyroid gland and total thyroidectomy were performed. After extensive exploration of the neck area, there was no apparent enlargement of the lymph nodes.
After surgery, the patient’s serum calcium level immediately decreased to 2.15 mmol/L (8.58 mg/dL), and PTH recovered to 16 pg/mL. The patient was found to have hypocalcemia on day 3 (calcium 7.48 mg/dL) in accordance with the “hungry bone” syndrome. She was treated with oral calcium, intravenous calcium and vitamin D3, and upon discharge with oral calcium and vitamin D3. The postoperative vital signs in the mother and newborn were stable, and the laboratory and clinical manifestations quickly returned to normal.
A healthy female baby weighing 3300 g was born, with an APGAR score of nine and ten points at one minute and five minutes postpartum, respectively, after 40 wk of pregnancy. The patient was discharged from hospital 4 d after delivery in good condition. She was followed-up at the outpatient department after receiving L-thyroxine substitution therapy. During the 12-mo follow-up period after surgery, the intact PTH level was 25 pg/mL, and the thyroid globulin level was less than 0.1 ng/mL under T4 suppression. She had no evidence of recurrence, and her child was in good health over the three-year follow-up period.
There have been many studies on the correlation between PHPT and differentiated thyroid cancer. A retrospective study was conducted which included 824 patients with primary hyperthyroidism with at least one lobotomy, and 18 patients (8.6%) were identified as having thyroid cancer[7].
The results of the study by Burmeister et al[7] showed that thyroid cancer during parathyroid resection was involved in conditions that may not be correlated with PHPT. The correlation between thyroid cancer and PHPT may be apparent. Some investigators have described this coexistence as fortuitous[7]; however, other researchers have indicated elevated endogenous calcium levels or growth factors, for instance, insulin-like growth factors and epithelial growth factors, as elements causing goiter[8-10]. PHPT and the diagnosis of thyroid carcinoma during pregnancy is a challenging problem for obstetricians.
A more sensitive scan for thyroid nodules can be performed by ultrasound-guided FNAB before surgery[11]. According to a Swedish study, the presence of a parathyroid adenoma in women during pregnancy significantly increases the risk of preeclampsia, with an odds ratio of 6.89[6]. In fact, hyperparathyroidism should not be suspected with high levels of PTH; in contrast, patients with hyperparathyroidism should be closely monitored, including for a possible diagnosis of MEN syndrome, and for the presence of nontoxic goiter with rare nodules.
Additionally, 99mTc-MIBI scanning is now considered to be the most sensitive monitoring tool, and it has many advantages, including the inspection and measurement of ectopic glands and nonfunctional parathyroid carcinoma[12,13]. In addition to 99mTc-MIBI scanning, the preoperative localization of parathyroid glands can be performed by ultrasound and MRI.
MRI is especially useful when there is a high probability of the presence of heterotopic glands. However, parathyroidoma, hyperplasia, and cancer demonstrate similar patterns on MRI, which leads to lower idiosyncrasies[14]. If ultrasonography and/or scintillation are ambiguous, MRI is usually used to evaluate patients with PHPT. Ultrasonography is a non-invasive, easily available, low-cost and nonionized technique that is very dependable when conducted by experienced operators. Ultrasound can be used to locate cervical nodules, and guide biopsies. However, ultrasonography to estimate the location of the parathyroid gland behind the mediastinum, esophagus or trachea is not useful, and is difficult if the patient has had previous surgery[15]. With regard to localization, ultrasonic examination can enhance the orientation of thyroid gland nodes, and the precise diagnosis of tubercles is carried out by FNAB with a sensitivity of 89%, an accuracy of 90%, and a specificity of 91%[6]. Furthermore, four-dimensional computed tomography (4DCT) is an emerging imaging modality for the evaluation of PHPT. 4DCT enables successful and efficient parathyroidectomy[16].
As CT, PET/CT, 4DCT, and 99mTc-MIBI scanning may cause radiation damage to the fetus, preoperative examination in this case was only performed with ultrasound, MRI and FNAB.
This clinical case illustrates the need for awareness of concomitant PHPT and thyroid diseases. For all PHPT patients, it is necessary to perform a careful thyroid evaluation.
The authors sincerely thank the patient for her contribution to the publication of this case report.
Manuscript source: Unsolicited manuscript
Specialty type: Endocrinology and metabolism
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Casella C S-Editor: Wang DM L-Editor: Webster JR P-Editor: Xing YX
| 1. | KISSIN M, BAKST H. Co-existing myxedema and hyperparathyroidism; case report. J Clin Endocrinol Metab. 1947;7:152-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 16] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 2. | Tollin SR. Course and outcome of pregnancy in a patient with mild, asymptomatic, primary hyperparathyroidism diagnosed before conception. Am J Med Sci. 2000;320:144-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Zhang M, Wang H, Pan X, Wu W, Zhang H. Thyroid adenoma and nasopharyngeal carcinoma with metastasis to cervical lymph nodes is misdiagnosed and treated for thyroid carcinoma: A case report. Oncol Lett. 2016;12:553-555. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 4. | Schnatz PF, Thaxton S. Parathyroidectomy in the third trimester of pregnancy. Obstet Gynecol Surv. 2005;60:672-682. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 59] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 5. | Norman J, Politz D, Politz L. Hyperparathyroidism during pregnancy and the effect of rising calcium on pregnancy loss: a call for earlier intervention. Clin Endocrinol (Oxf). 2009;71:104-109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 113] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 6. | Hultin H, Hellman P, Lundgren E, Olovsson M, Ekbom A, Rastad J, Montgomery SM. Association of parathyroid adenoma and pregnancy with preeclampsia. J Clin Endocrinol Metab. 2009;94:3394-3399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 39] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 7. | Burmeister LA, Sandberg M, Carty SE, Watson CG. Thyroid carcinoma found at parathyroidectomy: association with primary, secondary, and tertiary hyperparathyroidism. Cancer. 1997;79:1611-1616. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 8. | Maiorano E, Ambrosi A, Giorgino R, Fersini M, Pollice L, Ciampolillo A. Insulin-like growth factor 1 (IGF-1) in multinodular goiters: a possible pathogenetic factor. Pathol Res Pract. 1994;190:1012-1016. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | McCarty MF. Parathyroid hormone may be a cancer promoter - an explanation for the decrease in cancer risk associated with ultraviolet light, calcium, and vitamin D. Med Hypotheses. 2000;54:475-482. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 55] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 10. | dell'Erba L, Baldari S, Borsato N, Bruno G, Calò-Gabrieli G, Carletto M, Ciampolillo A, Dondi M, Erba P, Gerundini P, Lastoria S, Marinelli P, Santoro M, Scarano B, Zagni P, Bagnasco M, Mariani G. Retrospective analysis of the association of nodular goiter with primary and secondary hyperparathyroidism. Eur J Endocrinol. 2001;145:429-434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Diaz-Soto G, Linglart A, Sénat MV, Kamenicky P, Chanson P. Primary hyperparathyroidism in pregnancy. Endocrine. 2013;44:591-597. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 59] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 12. | Aalaa M, Mohajeri-Tehrani MR. Images in clinical medicine. Ectopic thyroid gland. N Engl J Med. 2012;366:943. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Wang L, Han D, Chen W, Zhang S, Wang Z, Li K, Gao Y, Zou S, Yang A. Non-functional parathyroid carcinoma: a case report and review of the literature. Cancer Biol Ther. 2015;16:1569-1576. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 20] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 14. | Lee VS, Spritzer CE. MR imaging of abnormal parathyroid glands. AJR Am J Roentgenol. 1998;170:1097-1103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 15. | Koike E, Yamashita H, Noguchi S, Murakami T, Ohshima A, Maruta J, Kawamoto H, Yamashita H. Effect of combining ultrasonography and ultrasound-guided fine-needle aspiration biopsy findings for the diagnosis of thyroid nodules. Eur J Surg. 2001;167:656-661. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 34] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 16. | Cham S, Sepahdari AR, Hall KE, Yeh MW, Harari A. Dynamic Parathyroid Computed Tomography (4DCT) Facilitates Reoperative Parathyroidectomy and Enables Cure of Missed Hyperplasia. Ann Surg Oncol. 2015;22:3537-3542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 26] [Article Influence: 2.6] [Reference Citation Analysis (0)] |