Published online Sep 26, 2020. doi: 10.12998/wjcc.v8.i18.4094
Peer-review started: March 2, 2020
First decision: April 22, 2020
Revised: June 26, 2020
Accepted: August 25, 2020
Article in press: August 25, 2020
Published online: September 26, 2020
Processing time: 203 Days and 3.5 Hours
Epidermolytic acanthoma (EA) is a rare benign skin lesion, usually found in the genital area of men and women, with epidermolytic hyperkeratosis as its distinguishing histologic characteristic. It is commonly misdiagnosed as condyloma accuminatum, verruca, and seborrheic keratosis. Since this lesion is benign, treatment is not necessary. However, it is often misdiagnosed, and patients are likely to undergo incorrect counseling and unnecessary treatment, causing undue burden to the patient. This study seeks to increase awareness of this rare condition to prevent future misdiagnoses.
A 55-year-old man living with human immunodeficiency virus presented for anal cancer screening. His physical examination revealed a flesh colored papule at the anal margin. The initial differential diagnosis included molluscum contagiosum, anal condyloma, and basal cell carcinoma. The lesion was excised to obtain a definitive diagnosis and was discovered to be EA.
EA is often misdiagnosed due to its similarity to other dermatologic conditions. Careful examination and pathologic evaluation should be obtained to ensure proper diagnosis.
Core Tip: Epidermolytic acanthomas (EAs) are papular skin lesions whose hallmark histologic feature is EHK. Herein, we describe a patient who presented with a solitary perianal EA and summarize the existing literature. EAs often present as pale papules in the genital region, trunk and extremities. EA is benign and cannot be spread to others, however they are commonly misdiagnosed as condyloma accuminatum, verruca, and seborrheic keratosis. Careful histopathological examination is necessary to obtain an accurate diagnosis and prevent unnecessary treatments. Although treatment of EA is not medically necessary, many patients prefer treatment, which can be accomplished with topical therapy or with excision.
- Citation: Ginsberg AS, Rajagopalan A, Terlizzi JP. Epidermolytic acanthoma: A case report. World J Clin Cases 2020; 8(18): 4094-4099
- URL: https://www.wjgnet.com/2307-8960/full/v8/i18/4094.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i18.4094
Epidermolytic acanthoma (EA) is a benign lesion, typically skin colored, brown, or white, small in size with a smooth surface, located in the groin and genital area, with a duration from one week to several years[1-4]. The median age of diagnosis is 39 to 65 years[1,4-6]. The incidence is 4.5 cases per 100000 and most studies show a similar rate among men and women[4]. One study, however, reported that genital lesions were more common in males[4]. The lesions are not transmitted by skin-to-skin or sexual contact[7,8]. EA may present as a single lesion or in clusters[2-4,8]. Additionally, EA may be asymptomatic or pruritic[2,9].
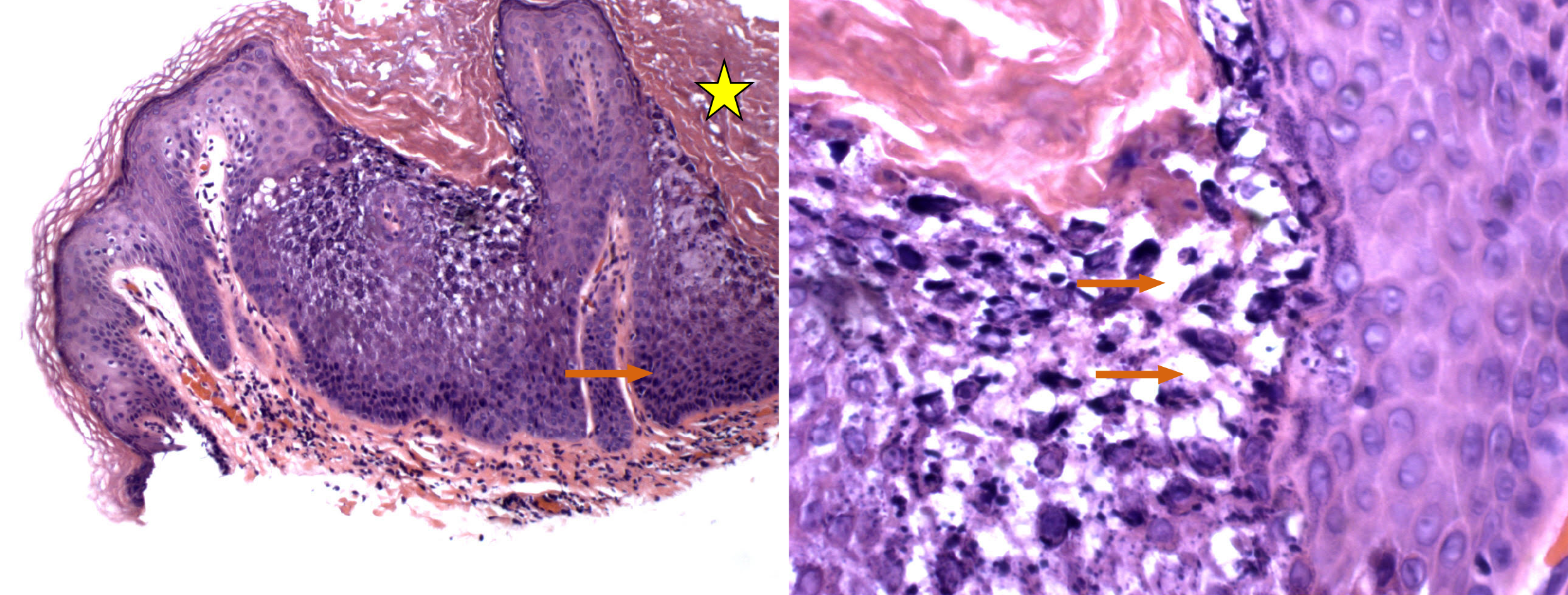
The typical histologic features include well demarcated papular lesions with perinuclear vacuolization, reticular degeneration in the granular and upper spinous layers, and epidermolytic hyperkeratosis (EHK)[2,8].
In this case report, we describe one patient’s presentation, histologic findings, and prognosis. We also conducted a literature review of the condition. We performed a PubMed search of relevant literature on EA, using key words “Epidermolytic Acanthoma” resulting in 53 related publications. The most relevant articles based on title and abstract were chosen and reviewed. The purpose of this report is to contribute to a better understanding of EA and to encourage clinicians to consider this diagnosis when examining patients with small papular lesions.
The patient was a 55-year-old and was referred to our practice for anal cancer screening.
The patient had no known history of present illness.
The patient has been living with human immunodeficiency virus (HIV) for 17 years.
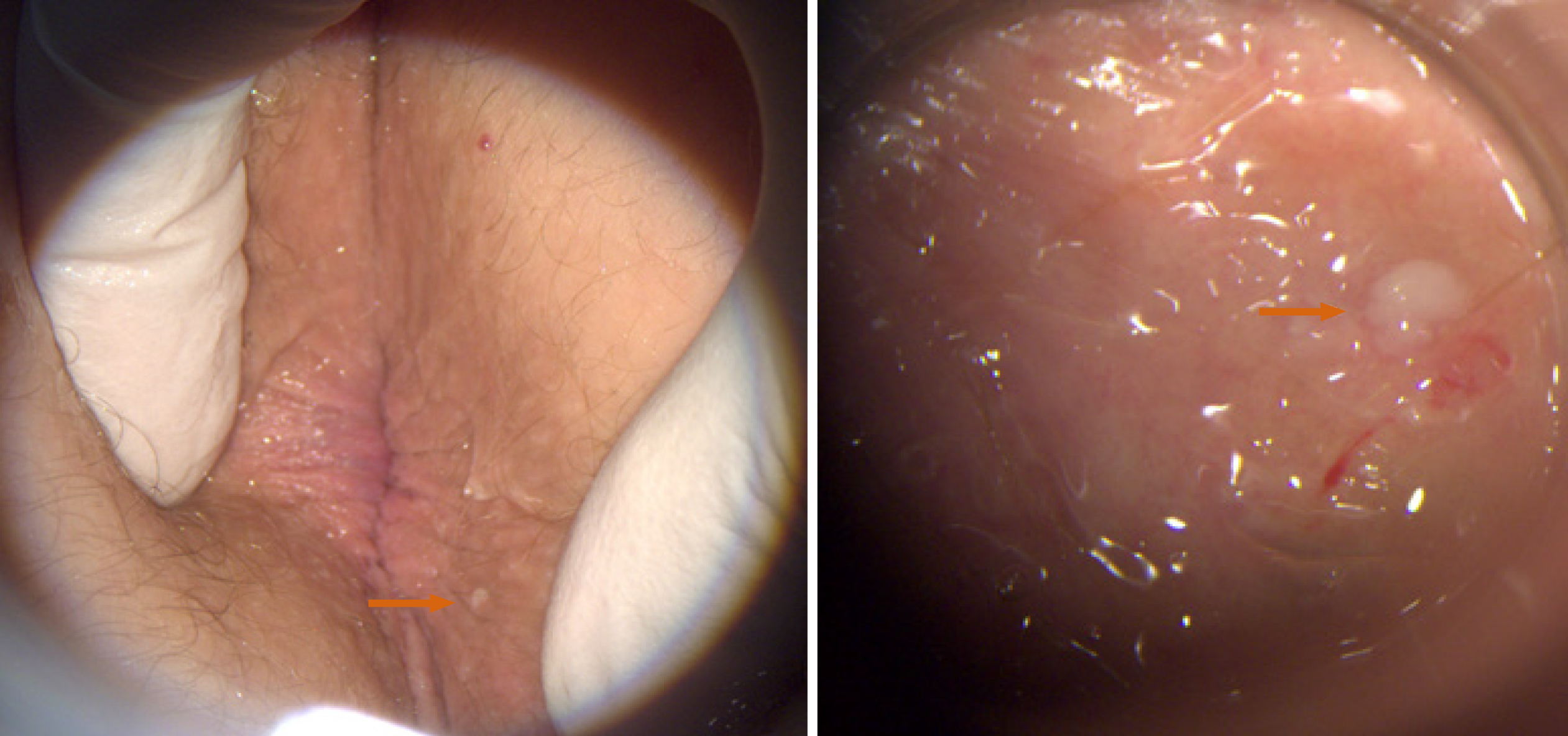
He had no gastrointestinal or anorectal symptoms and his physical examination was positive only for a three millimeter, smooth, flesh colored papule at the anal margin (Figure 1).
His cluster of differentiation 4 (CD4) count was 2200 cells/mm3, with a nadir of 1300 cells/mm3. His HIV viral load was undetectable. Anal cytology collected at this visit was benign.
Digital anorectal examination and high resolution anoscopy (HRA) were otherwise normal.
The differential diagnosis included molluscum contagiosum, anal condyloma, and basal cell carcinoma. To obtain a definitive diagnosis, the anal margin lesion was excised in the office, using local anesthetic.
Upon examination of the specimen, the lab determined the patient had EA.
The patient was diagnosed with EA.
The anal lesion was fully excised during his initial office visit.
Histologically, the specimen was described as a hyperkeratotic papillomatous lesion, consistent with a diagnosis of epidermolytic acanthoma (Figure 2). The excision site healed without complication.
In accordance with the New York State Department of Health guidelines, the patient will undergo annual anal cancer screening[10]. This screening will consist of a digital anorectal examination, anal cytology, and anoscopy. If the cytology is abnormal, the patient will then undergo HRA with biopsy of any lesion that appears to be malignant or premalignant.
EAs are small lesions, often located on the trunk or genital area, and are commonly misdiagnosed[2].Therefore, close histopathological examination is important to achieve an accurate diagnosis[8]. The principal histologic feature of EA is EHK on 50% or more of the EA surface[2,4]. EHK is defined by keratinocytes in the granular and spinous layers that have reticular degeneration, perinuclear vacuolation, coarse keratohyalin granules, and perinuclear eosinophilic inclusions[2,11,12].
While EHK is the hallmark histological finding in EA, it is not specific to this condition[13,14]. A correct EA diagnosis requires the characteristic histologic features in the proper clinical setting. EHK is also seen in epidermolytic ichthyosis (EI), epidermolytic epidermal nevus, or as an incidental finding[13,14]. These conditions are histologically indistinguishable. However, EI has distinguishing clinical features from EA, as it presents at or shortly after birth, and the skin of affected individuals appears red and blistering[15,16]. While EI is known to be caused by germline mutations in KRT1 and KRT10 genes, no such mutation has been found in EA[2,17,18]. However, reduced expression of cytokeratin (CK)1and CK10in EA has been observed on immunohistochemistry[17,19].
Many reports have confirmed the absence of human papillomavirus (HPV) in EA[2,20]. In one case report, however, a lesion demonstrated the presence of HPV type 16[21]. It is thought that in this case, HPV was an incidental finding rather than the causative agent for the EA[16].
While the patient described here was diagnosed with HIV 17 years before presenting with EA, his virus was well suppressed since diagnosis, and he always maintained high CD4 cell counts. To our knowledge, there are no published studies showing an association between HIV and EA. However, there have been case reports describing immunosuppressed patients who presented with EA. Two relevant case reports included two separate kidney transplant recipients, both developing EA with the commencement of immunosuppressive medications[7,22]. Further investigation is necessary to understand if EA is associated with immunosuppression.
EA is often misdiagnosed, and the most common misdiagnoses reported are condyloma acuminatum, verruca, and seborrheic keratosis[2,4,23]. Condyloma acuminate are more commonly known as genital warts and verruca are common warts. There are several defining features that differentiate EA and condyloma acuminatum. In one study by Lee and Wu, the average age for those with EAs was older than for condyloma (51 years and 17-33 years, respectively)[2]. Furthermore, EAs were lighter in color, smaller, and sporadically distributed compared to condyloma[2]. One of the reasons for the frequent misdiagnosis of condyloma is that both types of lesions are often found in the genital region[2]. EA has also been reported on the trunk and the extremities[4,11,24].
A case study published by Dupont et al[24] outlined the original misdiagnosis of condyloma acuminatum before the correct diagnosis of EA in a 51-year-old male patient[24]. The misdiagnosis of condyloma led to a prescribed treatment of cryotherapy. The lesion did not resolve after initial treatment and was biopsied after treatment. Pathologic examination demonstrated acanthosis, hyperkeratosis, cytoplasmic vacuolization, coarse keratohyalin granules, and eosinophilic inclusions. The lesion was then correctly diagnosed as EA.After arriving at the proper diagnosis, the patient was spared further treatment.
As EAs are benign, treatment is not mandatory[2].However, if patients desire treatment, there are several methods that may be employed. These methods include excision, cryotherapy, curettage, and ablative laser therapy[2,8]. There are also various topical therapies such as imiquimod, retinoids, lactic acid, glycolic acid, salicylic acid, and calcipotriol, which regulate the proliferation and differentiation of keratinocytes[2,8,9,20,25].One patient also reported complete elimination of EA after four weeks imiquimod 5% applied topically, while another reported softening of the lesions with lactic acid cream[8,25].Another patient found 0.1% tacrolimus ointment effective for relief of pruritus associated with EA after only a few weeks of use[26].
If EA is suspected, we recommend that the provider considers biopsy or excising the lesion to ensure an accurate diagnosis. Once EA is definitively diagnosed, we recommend explaining that treatment is not medically necessary. If a patient still desires removal of the benign papules for aesthetic, psychological, or other reasons, medical providers should explain possible treatment options as well as their associated risks and benefits to be sure an informed decision is made. If the patient has only one or two EA lesions, excision is often preferred. Topical therapy is most useful with a higher disease burden that would be associated with a painful recovery after surgical treatment of widespread disease.
Correctly diagnosing EA is extremely beneficial for patients and medical practitioners. If EA is misdiagnosed, patients are likely to undergo unnecessary treatments, as outlined above. These treatments are often painful and uncomfortable for patients and may also place an unnecessary financial burden on them. It is relevant to mention the psychological burden of misdiagnosis. In their case report, Fletcher et al[8] noted that their patient “was relieved to learn that her lesions did not represent a sexually transmitted disease and were consistent with agminated epidermolytic acanthoma[8,12,16].” We believe this case is of interest because EA is relatively uncommon and often confused with other dermatological conditions. Our primary goal in presenting this review is to provide clinicians with a knowledge to properly diagnose and treat EA.
In this manuscript, we describe a patient who presented with a solitary perianal EA and summarize the available literature. EAs are benign lesions, often presenting as pale papules in the genital region, trunk and extremities that are commonly misdiagnosed as condyloma accuminatum, verruca, and seborrheic keratosis. Careful histopathological examination demonstrating more than 50% EHK is necessary to reach an accurate diagnosis. Although treatment of EA is not medically necessary, many patients desire treatment, which includes topical or surgical therapy.
We would like to thank our patient for generously allowing us to share his case and Dr. Elaine Alt MD for providing the photomicrographs.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: D'Orazi V, Kung WM, Zhang W, Zippi M S-Editor: Gong ZM L-Editor: A P-Editor: Wang LL
| 1. | Ackerman AB. Histopathologic concept of epidermolytic hyperkeratosis. Arch Dermatol. 1970;102:253-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 50] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 2. | Lee TJ, Wu YH. Multiple epidermolytic acanthomas mimicking condyloma: a retrospective study of 8 cases. Int J Dermatol. 2018;57:28-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 3. | Moulonguet I, Serre M, Herskovitch D. [Multiple epidermolytic acanthomas of the genitalia]. Ann Dermatol Venereol. 2017;144:295-300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Roy SF, Ghazawi FM, Choate KA, McNiff JM. Solitary and multiple epidermolytic acanthoma: A demographic and clinical study of 131 cases. J Cutan Pathol. 2019;46:305-309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Shapiro L, Baraf CS. Isolated epidermolytic acanthoma. A solitary tumor showing granular degeneration. Arch Dermatol. 1970;101:220-223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Cohen PR, Ulmer R, Theriault A, Leigh IM, Duvic M. Epidermolytic acanthomas: clinical characteristics and immunohistochemical features. Am J Dermatopathol. 1997;19:232-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 32] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Yang JH, Kim JK, Won CH, Chang SE, Lee MW, Choi JH, Moon KC. Isolated epidermolytic acanthoma in a renal transplant recipient. Ann Dermatol. 2011;23:415-416. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Fletcher JW, Ramamurthi A, Parekh P. Presentation of epidermolytic acanthomas as multiple tan papules on the vulva. Proc (Bayl Univ Med Cent). 2016;29:198-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Hijazi MM, Succaria F, Ghosn S. Multiple localized epidermolytic acanthomas of the vulva associated with vulvar pruritus: a case report. Am J Dermatopathol. 2015;37:e49-e52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | NYS Guidelines recommendations on anal pap smears. Available from: http://www.natap.org/2010/HIV/032510_01.htm. |
| 11. | Abbas O, Wieland CN, Goldberg LJ. Solitary epidermolytic acanthoma: a clinical and histopathological study. J Eur Acad Dermatol Venereol. 2011;25:175-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 12. | Kukreja T, Krunic A. Multiple epidermolytic acanthomas must not be confused with genital human papillomavirus infection. Acta Derm Venereol. 2009;89:169-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 13. | Conlin PA, Rapini RP. Epidermolytic hyperkeratosis associated with melanocytic nevi: a report of 53 cases. Am J Dermatopathol. 2002;24:23-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Gaertner EM. Incidental cutaneous reaction patterns: epidermolytic hyperkeratosis, acantholytic dyskeratosis, and hailey-hailey-like acantholysis: a potential marker of premalignant skin change. J Skin Cancer. 2011;2011:645743. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 15. | Vahlquist A, Törmä H. Ichthyosis: A Road Model for Skin Research. Acta Derm Venereol. 2020;100:adv00097. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 16. | Chan MP. Verruciform and Condyloma-like Squamous Proliferations in the Anogenital Region. Arch Pathol Lab Med. 2019;143:821-831. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 17. | Adachi T, Tanese K, Ouchi T, Igawa S, Nakano H, Ishiko A. Case of isolated epidermolytic acanthoma: Genetic and immunohistochemical analysis. J Dermatol. 2016;43:974-975. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 18. | Egozi-Reinman E, Avitan-Hersh E, Barzilai A, Indelman M, Bergman R. Epidermolytic Acanthoma of the Genitalia Does Not Show Mutations in KRT1 or KRT10. Am J Dermatopathol. 2016;38:164-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 19. | Cheraghlou S, Atzmony L, Roy SF, McNiff JM, Choate KA. Mutations in KRT10 in epidermolytic acanthoma. J Cutan Pathol. 2020;47:524-529. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 20. | Batalla A, Carpintero ML, De la Torre C. Disseminated epidermolytic acanthoma with partial response to calcipotriol ointment. J Dermatol. 2013;40:144-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 21. | Jung JM, Lee SH, Won CH, Chang SE, Lee MW, Choi JH, Moon KC. A Case of Multiple Epidermolytic Acanthoma of the Scrotum: Is the Human Papillomavirus a Culprit? Ann Dermatol. 2015;27:633-634. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 22. | Chun SI, Lee JS, Kim NS, Park KD. Disseminated epidermolytic acanthoma with disseminated superficial porokeratosis and verruca vulgaris in an immunosuppressed patient. J Dermatol. 1995;22:690-692. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 23. | Kazlouskaya V, Lambe J, Elston D. Solitary epidermolytic acanthoma. J Cutan Pathol. 2013;40:701-707. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 24. | Dupont A, Marescassier H, Kaya G. Epidermolytic Acanthoma Mimicking Condyloma: A Case Report. Dermatopathology (Basel). 2019;6:23-27. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 25. | Jang BS, Jang HS, Park HJ, Kim MB, Oh CK, Kwon KS. Multiple scrotal epidermolytic acanthomas successfully treated with topical imiquimod. J Dermatol. 2007;34:267-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 26. | Tan GF, Tan ES, Tey HL. Anogenital epidermolytic acanthomas: effective treatment of pruritus with 0.1% tacrolimus ointment. Dermatol Ther. 2014;27:113-116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (1)] |