Published online Sep 26, 2020. doi: 10.12998/wjcc.v8.i18.3999
Peer-review started: March 28, 2020
First decision: April 24, 2020
Revised: April 30, 2020
Accepted: July 30, 2020
Article in press: July 30, 2020
Published online: September 26, 2020
Processing time: 177 Days and 7 Hours
Atraumatic restorative treatment (ART) may be appropriate for populations without accessibility and affordability. More data are required regarding the success rate of ART in anterior teeth.
To evaluate the clinical performance of restoring class III cavities in anterior teeth of permanent dentition using the ART approach.
A longitudinal interventional field study was carried out at two rural primary health centers, Tumkur district, India. A total of 54 teeth in 39 patients were evaluated for the survival rate of class III restorations in permanent anterior teeth using the ART approach in children and adult populations. Evaluation of ART restoration was carried out using Frencken J criteria, the mean procedure time, patient acceptance and reported pain severity during the ART approach were evaluated using a visual analog scale. Calculation of the cost of ART was also performed.
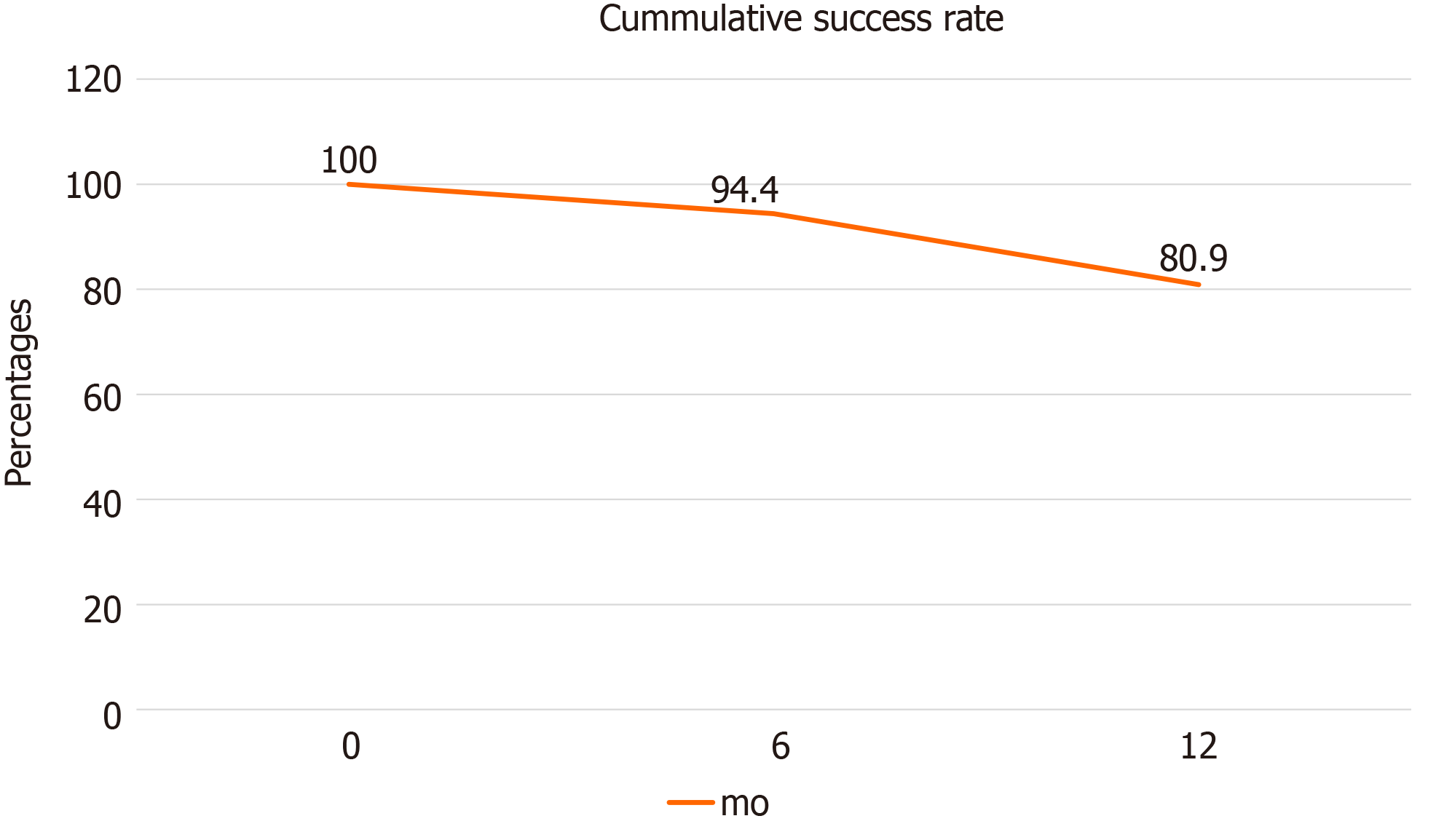
The mean time taken to perform the ART procedure was 14.79 ± 5.8 min with the majority of patients reporting only mild pain. At 6 mo follow-up, 72.2% remained in a good state, but this reduced to 27% at 12 mo. The cumulative survival rate of the restorations was 94.4% at 6 mo and 80.9% at 12 mo follow-up. Estimation of the direct cost for a single class III restoration was 186.50 INR (2.64 USD).
ART may be a good comprehensive option for basic oral health care for underserved or inaccessible populations, and preventive care for patients.
Core Tip: This study aimed to evaluate the success rate of atraumatic restorative treatment (ART) for class III anterior permanent teeth. ART is a cost-effective treatment and is best for populations without access to oral health care. The current study findings suggest that the cumulative survival rate of the restorations at 12 months follow-up was 80.9% which is an acceptable success rate. ART is suitable for areas where dental health services cannot be reached easily.
- Citation: Shivanna MM, Ganesh S, Khanagar SB, Naik S, Divakar DD, Al-Kheraif AA, Jhugroo C. Twelve-month evaluation of the atraumatic restorative treatment approach for class III restorations: An interventional study. World J Clin Cases 2020; 8(18): 3999-4009
- URL: https://www.wjgnet.com/2307-8960/full/v8/i18/3999.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i18.3999
The inaccessibility of dental services in rural populations has always been a concern. With most developing countries displaying an insufficient dentist to population ratio, India is the largest democracy and has a dentist to population ratio of 1:250000[1]. In developing countries, significant barriers such as poverty, financial restrictions, and lack of adequate experienced health specialists and workers exist[2]. To reduce the disease burden among the population, the best substitute is to implement inexpensive and affordable preventive dental health care programs. The delivery of oral care is usually a problem in such densely populated countries, due to lack of access, and affordability. Thus, the atraumatic restorative treatment (ART) approach may be the most appropriate conservative treatment[3]. ART was first developed in 1980 in Tanzania[4]. Due to the introduction of new material, glass ionomer cement (GIC), a new technique was introduced by placing GIC in the cavity using ART[5]. ART consists of the removal of caries affecting tooth structure using only hand instruments and restoration with tooth bonding or adhesive restorative materials such as glass ionomer cement[6]. ART was endorsed by the World Health Organization (WHO) and does not require aesthetics and has minimal cost. However, several aspects still cause concern[7].
The advantages of ART are that it costs less, it is easily available, restoration can be performed using only hand instruments instead of electrically motor-driven instruments, reduces healthy tooth tissue damage, less noise compared to motor-driven instruments, less sensitivity and pain, which minimizes the use of local anesthesia, and results in reduced patient anxiety[8,9]. ART was field-tested in south Asia and Africa and adopted by the WHO in 1994[10]. Based on previous studies, results for the ART approach were very successful for posterior single surface restorations; however, the success rate is less for multiple posterior surfaces and anterior teeth restoration[8,11]. New treatment strategies such as a shortened dental arch with missing molars and anterior teeth including premolars are now available. In these cases, ART appears to be promising where there are limited oral health care services[10,12]. Based on evidence-based dentistry, ART showed a better performance in developing countries with only a 5% failure rate in class 1 restorations[13]. Considering the paucity of data regarding the ART approach in anterior permanent teeth and limited studies supporting the success rate of class III restorations, the aim of the present study was to evaluate the clinical performance of restoring class III cavities in anterior teeth of permanent dentition using the ART approach in primary health care (PHC) settings in Tumkur district, India.
The present study was a longitudinal interventional field study with 12 mo follow-up after placement of ART. The study was carried out at two rural PHC settings located in Kyathasandra and Siddagangamutt of Tumkur district, Karnataka, India. ART was carried out in subjects who met the inclusion criteria and evaluation of the success rate, time taken for placement, pain analysis, and cost estimation were performed.
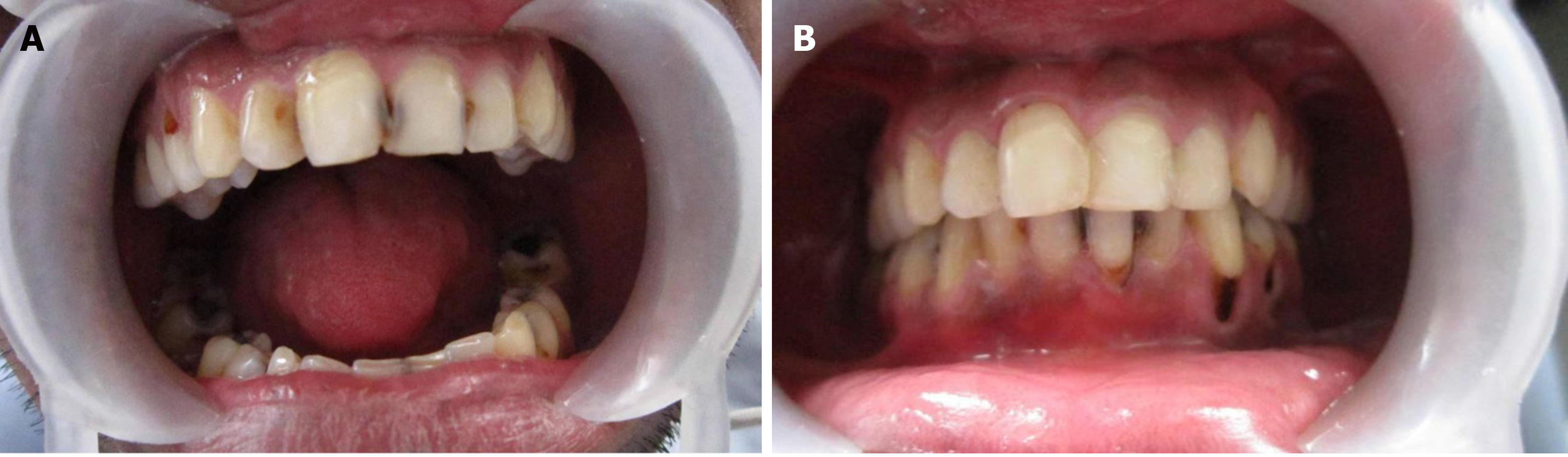
The study population included school children and adults aged 16 to 50 years within the PHC limit. Inclusion criteria were the presence of a minimum of one anterior tooth with caries extending to the dentine. The cavity entrance should be at least 1 mm permitting access of the smallest excavator and the tooth should be in good periodontal condition (Figure 1A). Exclusion criteria were teeth with symptoms of pulpal inflammation, tender on percussion, known-vital tooth, and teeth with abscess, fistula, or exposure of pulp.
By assuming a 50% success rate for GIC, a sample size of 50 teeth was derived. In total, 54 teeth in 39 patients were included in the study.
The proforma used for this study was designed in the Dental Public Health Department, The Oxford Dental College and Hospital. It comprised basic demographic information. The time taken for the restoration of teeth from isolation to finishing the procedure was recorded using a stopwatch. Patient acceptance and reported pain severity of the ART approach were assessed immediately following the ART technique using the visual analog scale (VAS). Direct costs were calculated based on the value of goods values, services, and other resources consumed. The total cost of consumables used in this study, staff time, equipment used, transport, out of pocket expenses were noted and the direct cost of restoration was calculated. The study protocol was reviewed and approved by the ethical board, The Oxford Dental College and Hospital, Bangalore, India. Permission for conducting the study in the PHC setting was obtained from the district health officer of Tumkur, India. Written informed consent was obtained from the subjects willing to participate after explaining the nature of the study.
The proforma consisted of information related to the study, including the option for subjects to withdraw at any stage of the study, and the voluntary participation of the study subjects. Instruments used in the ART kit included a mouth mirror, explorer, tweezers, straight probe, spoon excavators, enamel hatchet, plastic filling instruments, WHO probe, sterile gloves, cotton pellets, cotton rolls, low viscosity GIC Ionofil plus VOCO, plastic strips, articulating paper and petroleum jelly. The examiner who conducted the oral examination used disposable mouth masks and gloves. The instruments were sterilized using Korsolex (gluteraldehyde – 7.0 g; 1-6 dihydroxy 2.5 dioxyhexane – 8.2 g and polymethyl urea derivative – 11.6 g) which were diluted by adding 1 part to 9 parts of potable water. Moist heat sterilization was carried out later using a pressure cooker. A single trained dentist performed all the restorations. Training of the dentist to perform ART was undertaken by the research guide at the Dental Public Health Department, The Oxford Dental College and Hospital. The research guide also calibrated the evaluator who was not involved in the treatment procedure. Frencken J criteria were used to evaluate the restorations. Figure 1 shows pre- and post-ART restoration of teeth. Intra-examiner reproducibility was assessed on five restorations at two occasions and the resulting Kappa score was 0.97, which was high. A pilot study was carried out to confirm the feasibility of the study on 10% of the population.
The mean procedure time and patient acceptance of ART were also assessed. A few modifications were made before the final study. The study was scheduled to be carried out over one year. On average, 50 subjects were interviewed, a thorough oral examination was conducted and then the patients with class III cavities were treated on one of the given days during the study period. On average, approximately 4-5 restorations were performed each day, totaling 54 restorations in 39 subjects. A table fitted with a foldable cushion and soft headrest was positioned to obtain an operating position. The use of suction for saliva was not possible, hence cotton rolls were used for isolation. Some of the cavity lesion entrances were widened using an enamel hatchet by rotating it backward and forward, to permit proper access for caries removal. Removal of demineralized tissue with a conventional spoon excavator was then carried out, at the dentin-enamel junction and then the cavity floor. The unsupported, thin, enamel was cautiously broken using the enamel hatchet. The cavity was cleansed with water using a cotton pellet and then conditioned with liquid from the glass-ionomer used (Ionofil plus VOCO) on a cotton pellet for 10 to 15 s. The surface was washed with wet cotton pellets and then dry cotton pellets. Polyester matrix strips were placed and firmly wedged before the insertion of filling material into the cavity. The mixing and manipulation of the GIC were carried out as per the manufacturer's instructions. The restorative material was inserted into the cavity using the smooth side of the excavator. After placing the filling material, a strip was pressed against the restoration for 1 min. Excess material was removed using the carver and petroleum jelly was applied. Following restoration, patients were advised not to ingest food for at least 1 h.
The time taken to place a restoration starting from tooth isolation to completion of the procedure was recorded using a stopwatch and the mean time was recorded in minutes. The VAS was used to measure the perceived pain experienced on a graduated scale, with the lower limit as no pain and upper limit as severe pain, which corresponded to a range of scores from 0-10. The pain intensity was recorded by asking the respondents to draw a line perpendicular to the VAS line, at the point that represented their pain intensity. Finally, expenditure incurred during ART was calculated using direct costs.
ART was evaluated at baseline, 6-mo and 12-mo intervals by the examiner who was calibrated and was not involved in placement of the restoration. The restored teeth were evaluated using Frencken J criteria with the help of a plane front surface mirror and the WHO probe[14]. Accredited Social Health Activists assisted in fetching the study subjects to the PHC on scheduled days for evaluation. Restorations which were categorized as unsuccessful was re-restored and not included in further follow-up.
A descriptive analysis was carried out. The mean ± SD was calculated for continuous data. Categorical measurements were presented in numbers and percentages. Survival analysis (life-table analysis) was carried out at the 95% confidence interval. The statistical software SPSS version 21 was used.
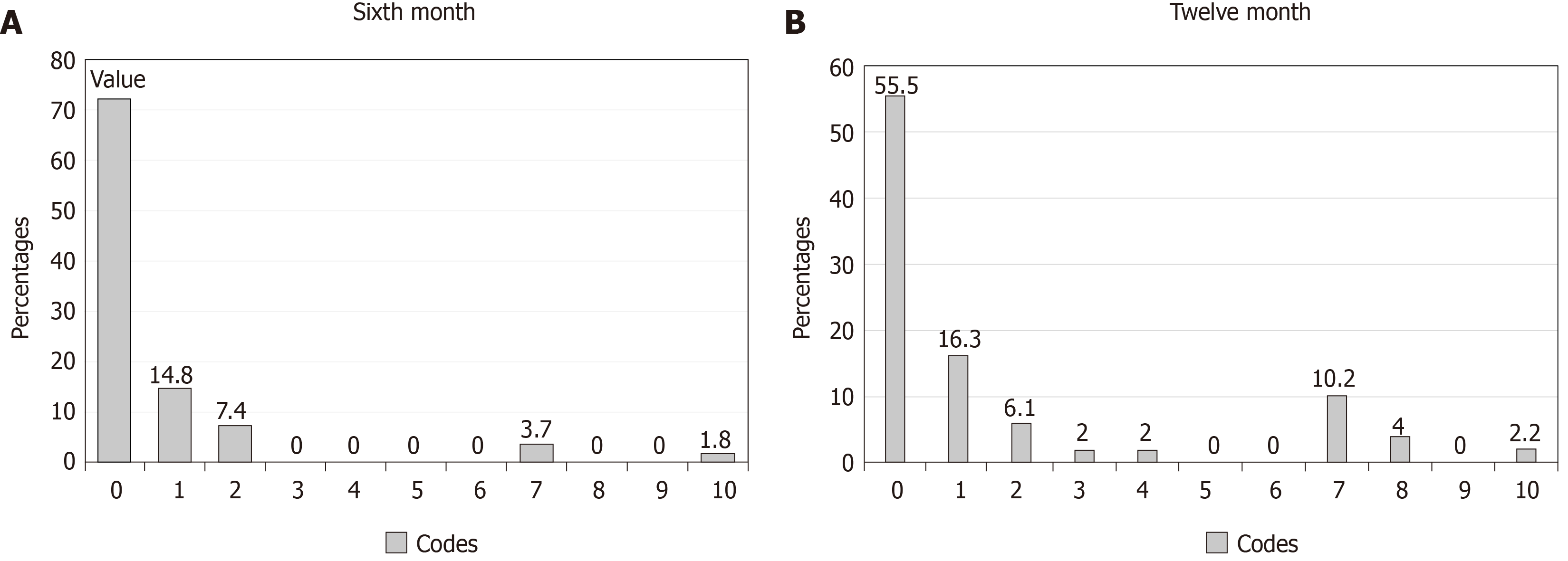
In the present study, the mean age of the subjects was 22.07 ± 7.33 years (Table 1), 16 (41.02%) subjects were 16-18 years, 14 (35.89%) were 19 to 22 years, 7 (17.9%) were 23 to 40 years and two subjects (5.1%) were more than 40 years with the majority being male subjects. The VAS was in the range of 1-3 for 28 (70.4%) subjects and was 4-7 for 11 (29.6%) subjects. The mean time taken to perform the ART procedure was 14.79 ± 5.8 min (Table 2). The majority of patients reported only mild pain (Table 3). At 6 mo follow-up, 54 restorations were evaluated and 39 (72.2%) restorations (code = 0) were in good condition, 8 (14.8%) restorations (code = 1) had a slight marginal defect which did not require repair, 4 (7.4%) restorations (code = 2) had a marginal defect which was deeper than 0.5-1 mm and required repair, none of the restorations had marginal defects more than 1 mm (code = 3). None of the restorations had completely disappeared (code = 4). None of the restorations were replaced with other restorations (code = 5), and none of the teeth were extracted (code = 6). Two (3.7%) restorations (code = 7) showed wear and tear over large parts of the restorations but were less than 0.5 mm at the deepest point. None of the restorations showed wear and tear over a large part of the restoration of more than 0.5 mm (code = 8). None of the restorations were an undiagnosed condition (code = 9) and 1 (1.8%) restoration (code = 10) was lost to follow-up (Table 4, Figure 2A). At 12 mo follow-up, 27 (55.5%) restorations were in code = 0, 8 (16.3%) restorations were in code = 1, 4 (6.1%) restorations were in code = 2, 1 (2%) restoration was in code = 3, 1 (2%) restoration was in code = 4, 5 (10.2%) restorations were in code = 7, and 2 (4%) restorations were in code = 8. One (2.5%) restoration was in code = 10 (Table 4, Figure 2B). The data were subjected to life table analyses which showed that at the 6 mo follow-up the success rate was 94.4% (88.2-99.9) and at the 12 mo follow-up was 85.7% (75.9-95.5), with a cumulative survival rate of 80.9% (69.9-91.9) at the end of 12 mo. At the 6 mo follow-up, 72.2% remained in a good state; however, this reduced to 27% at the 12 mo follow-up (Table 5). Thus, the cumulative survival rate of the restorations was 94.4% at 6 mo and 80.9% at 12 mo follow-up (Figure 3). Table 6 shows that the direct cost estimation for a single class III restoration was 186.50 INR (2.62 USD).
| Age (yr) | No. of subjects | Percentage (%) |
| 16-18 | 16 | 41.02 |
| 19-22 | 14 | 35.89 |
| 23-40 | 7 | 17.94 |
| > 40 | 2 | 5.15 |
| Total | 39 | 100.0 |
| Time taken for restoration (min) | No. of restorations in subjects | Percentage (%) |
| 9-15 | 22 | 40.7 |
| 16-19 | 32 | 59.3 |
| Total | 54 | 100.0 |
| VAS score | No. of restorations in subjects | Percentage (%) |
| 1-3 (mild) | 38 | 70.4 |
| 4 -7 (moderate) | 16 | 29.6 |
| 8-10 (severe) | 0 | 0.0 |
| Total | 54 | 100.0 |
| Code | 6 mo, n = 54 | 12 mo, n = 49 | ||
| No. of restorations | Percentage (%) | No. of restorations | Percentage (%) | |
| 0 | 39 | 72.2 | 27 | 55.5 |
| 1 | 8 | 14.8 | 8 | 16.3 |
| 2 | 4 | 7.4 | 4 | 6.1 |
| 3 | 0 | 0 | 1 | 2.0 |
| 4 | 0 | 0 | 1 | 2.0 |
| 5 | 0 | 0 | 0 | 0 |
| 6 | 0 | 0 | 0 | 0 |
| 7 | 2 | 3.7 | 5 | 10.2 |
| 8 | 0 | 0 | 2 | 4.0 |
| 9 | 0 | 0 | 0 | 0 |
| 10 | 1 | 1.8 | 1 | 2.2 |
| Interval (mo) | Evaluated restoration | Success | Failure | Success rate (95%CI) | Cumulative survival rate (95%CI) |
| 6 mo | 54 | 49 | 4 | 94.4% (88.2%–99.9%) | 94.4% (88.2%-99.9%) |
| 12 mo | 49 | 40 | 7 | 85.7% (75.9%-95.5%) | 80.9% (69.9%-91.9%) |
| Input cost | Financial cost | Economic cost | Annualized cost | Amount | |
| Expected use full life of the capital | Discount rate | ||||
| Primary consumables | |||||
| Space | 0 | 1000 INR (14.10 USD) | - | - | 400 INR (5.64 USD) (12 d) |
| Equipment (ART kit) | 0 | 4500 INR (63.47 USD) | 5 yr | 3.7 | 1216.21 INR (17.15 USD) |
| Secondary consumables | |||||
| Staff | 0 | 5400 INR (76.17 USD) | - | - | 5400 INR (76.17 USD) |
| Consumables | 2457 | 2457 INR (33.43 USD) | - | - | 2457 INR (34.65 USD) |
| Travel expenses | 600 | 600 INR (8.46 USD) | - | - | 600 INR (8.46 USD) |
| Total | 2947 | 11857 INR (167.25 USD) | 10073.2 INR (142.08 USD) | ||
The ART approach for managing dental caries depends on 2 main aspects such as pit and fissure sealants for preventing caries and cavities involving the dentine[15]. ART supported by strong evidence is considered a minimally invasive technique and there is a shifting paradigm towards the use of these conservative approaches[16].
A previous study conducted in Cambodia showed that the application of ART was successful among children in inaccessible rural areas[17]. The success rate of the ART technique not only depends on the type of cavity conditioner or the material used for restoration, but also on the complete removal of the caries, depth of the cavity, site of the restoration, and the skill of the operator. The United States Public Health Service (USPHS) and Frencken J clinical criteria are commonly used to evaluate ART restorations. In the present study, Frencken J criteria were used to evaluate the restorations and the success of ART was based on the restorations being in good condition or without major marginal defects and wear greater than 0.5 mm.
In the present study, the mean age of the study population was 22.07 ± 7.33 years. The overall survival rate at the end of the 6 mo follow-up was 94.4% (95%CI: 88.2%-99.9%), and was 85.7% (95%CI: 75.9%-95.5%) at 12 mo. The cumulative survival at the end of the study period was 80.9% (69.9%-91.9%). The restorations with scores of 2, 3, 7, and 8 may survive and provide benefit for some years without the need for restoration. The reason for this benefit, as suggested by previous studies, is due to GIC, which prevents caries by releasing fluoride components. In patients with caries infected dentine, cavity preparation with fluoride-containing GIC has a preventive effect on cariogenic microorganisms[14]. The remineralization property of fluoride also helps enamel and dentine. Previous studies have demonstrated the GIC-fluoride-recharge ability in the oral environment. Thus, GIC acts as a permanent fluoride-reservoir and offers long-term protection against secondary caries[18-20].
A study conducted in Cambodia showed a similar success rate to that in the present study, but in their study, only 7 of 89 restorations were placed in anterior teeth (maxillary incisors). As their sample size was small, it is difficult to make a direct comparison with the present findings. They assessed the restorations at 12 mo follow-up, and one restoration was considered a failure and at 36 mo two were considered failed restorations. Their results were promising, especially in the conditions in which the restorations were performed, wherein low-strength GIC was used, cavity preparation was not conditioned before fill material insertion, and interestingly, restorations were performed by dental nurses who were still learning to use the ART technique[18]. A similar study conducted in the Gambia showed 53 of 76 restorations were clinically acceptable and 26 of 76 were insufficient[13]. A previous study assessed anterior (class III and V) restorations after 3 years among 83 class III restorations, and 92% were successful[8]. Some previous studies reported that the success rate of the ART approach in anterior permanent teeth was considerably high, i.e., at 3 years, it was 91.6%, and 73.8% at 6 years[21]. This was attributed to factors such as the use of high-viscosity conventional GIC (Ketac-Molar) specifically developed for use with the ART approach combined with cavity conditioner[22]. In a previous study conducted using high viscosity GIC in class II cavities a good success rate was observed[23]. During the excavation process, particular care was taken to remove soft carious tissue especially at the enamel and at the enamel-dentin junction to enhance bonding to the restorative material[21]. In our study, the high success rate obtained can be explained by the skill of the operating personnel, as one of the experienced dentists performed the restorations. Previous studies reported that dental nurses had carried out restorations and operators should have appropriate training before performing the ART restoration technique[4,18]. Also, the long-lasting effect of ART depends on proper case selection, caries risk, size of the cavity opening, and appropriate caries preventive measures by the patient[24]. In some studies, high viscosity GIC was used and the success rate was 92% for class III using Fuji IX after two years, and two different types of GIC were used, high viscosity GIC and resin-modified GIC, in multi-surface restorations, and the success rate for both materials was similar[25-27]. In a previous meta-analysis, the results showed a 97% success rate after 1 year using high viscosity GIC material for single surface restoration and similar results were recorded in the present study[28]. High viscosity GIC has more compressive strength and is suitable for posterior teeth, whereas low viscosity GIC is suitable for anterior teeth and has good wetting behavior and aesthetics[29].
In a previous study, a composite was used as a restorative material, which has a role to play in aesthetics. The Fill-magic composite used with an adhesive system magic bond and enamel was conditioned with phosphoric acid. However, our study did not assess the aesthetic and psychological response before and after the ART procedure. Conventional GIC restored ART will have an increased risk of fracture over a follow-up of 12 to 24 mo[25,30]. A previous study compared resin-modified GIC with composite resin, and after 3 years of evaluation the composite resin was better in terms of color aspects as well as the success rate. In addition, some studies reported that the success rate of class III ART was good after 48 mo. However, this study cannot be compared with our study as it used USPHS evaluation criteria, which might lead to higher success rates for ART restorations. This is due to the criteria used in USPHS to observe exposed dentine rather than a marginal defect[22,31].
In the present study, the cumulative survival rate at 12 mo follow-up for upper central incisors was 71.4% (50.0-92.2), for upper lateral incisors was 71.7% (47.2-96.2) and for upper canines was 75% (44.9-99.9). The cumulative survival rate at 12 mo for lower central incisors and lower lateral incisors was 100%. The cumulative survival rate at 12 mo for the upper jaw was 74.5% (60.9-88.2) and for the lower jaw was 100%. These results are similar to an earlier study in which the cumulative survival for upper jaw tooth restoration was 90.3%. However similar results were seen in the lower jaw at 3 years[21]. A study was conducted on ART in China, and during 30 mo of follow-up the survival rate for class I and V was very high compared to class III cavities[32]. When comparing the cumulative survival rates of individual teeth in the present study, it was found that maxillary canines had a better survival (75%) compared to maxillary central (71.4%) and lateral incisors (71.7%). Similarly, the cumulative survival rate was 100% for both mandibular central and lateral incisors. However, caution is needed when interpreting these results due to the small sample size in this study. A previous study also reported similar results for mandibular teeth over a 3-year period[21].
The mean operating time for the ART approach was 14.79 ± 5.8 min, and these results are comparable to a study conducted in Southern China which reported that the average time taken for ART restoration was only 10.5 min, but this was carried out in deciduous teeth. However, in both studies, the criteria for selecting the cavity regarding the size or depth were not considered[32]. Regarding patient acceptance of the ART procedure, 38 (70.6%) patients had mild pain (1-3 on the VAS), and 16 (29.4%) had moderate pain (4-7 on the VAS). These observations may be due to the large-sized cavities and cavities close to the pulp, which cause significantly more pain and discomfort. A study conducted in Egypt showed similar results among school students, where 6.6% had pain and 29.2% discomfort[33]. In our study, the direct cost of ART restoration was approximately 186.5 INR (2.63 USD). This can be explained on the basis that only a few instruments are required for ART. The usual cost for GIC restoration in a private setting is 500 INR (7 USD) at places nearest the study area. The ART approach helps to save teeth, that otherwise would have to be extracted and helps to prevent the development of caries.
Different variables such as the size of the cavity, patient’s oral hygiene, and parafunctional habits were not considered in the study. As all the restoration procedures were performed by a single experienced dentist, this factor should be considered as restoration abilities may differ.
In conclusion, following ART for class III, anterior permanent teeth caries resulted in a good cumulative survival rate over the 12 mo follow-up period. ART provides an opportunity to provide economical and aesthetic oral health care for inaccessible or underserved societies and communities, along with preventive and promotion activity. Outreach dental programs can adopt ART and provide the best treatment option for cavities in permeant teeth in India and similar regions.
The atraumatic restorative treatment (ART) approach is the most appropriate for rural populations who lack access to health care. ART was first developed in 1980 in Tanzania.
Little research has been conducted to assess the success rate ART in permanent anterior teeth class III restoration.
The objective of the present study was to evaluate the clinical performance of restoring class III cavities in anterior teeth of permanent dentition using the ART approach.
A longitudinal interventional field study was carried out. Evaluation of ART was performed using Frencken J criteria, the mean procedure time, patient acceptance and reported pain severity during the ART approach were evaluated using a visual analog scale. Calculation of the cost of ART was also performed.
The mean time taken to perform the ART procedure was 14.79 ± 5.8 min. At 6 mo follow-up, 72.2% remained in a good state; however, this reduced to 27% at 12 mo. The cumulative survival rate of the restorations was 94.4% at 6 mo and 80.9% at 12 mo follow-up.
ART is a good approach for populations with poor access to dental health services.
ART is a better alternative for class III anterior permanent teeth restorations and more studies need to be conducted in this field.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: Saudi Arabia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Faustino-Silva DD S-Editor: Ma YJ L-Editor: Webster JR P-Editor: Xing YX
| 1. | Oberoi SS, Oberoi A. Growing quackery in dentistry: An indian perspective. Indian J Public Health. 2015;59:210-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 2. | Nash D, Ruotoistenmäki J, Argentieri A, Barna S, Behbehani J, Berthold P, Catalanotto F, Chidzonga M, Goldblatt L, Jaafar N, Kikwilu E, Konoo T, Kouzmina E, Lindh C, Mathu-Muju K, Mumghamba E, Nik Hussein N, Phantumvanit P, Runnel R, Shaw H, Forna N, Orliaguet T, Honkala E. Profile of the oral healthcare team in countries with emerging economies. Eur J Dent Educ. 2008;12 Suppl 1:111-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Frencken JE. The state-of-the-art of ART restorations. Dent Update. 2014;41:218-220, 222-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 4. | Kikwilu EN, Frencken J, Mulder J. Impact of Atraumatic Restorative Treatment (ART) on the treatment profile in pilot government dental clinics in Tanzania. BMC Oral Health. 2009;9:14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Wilson AD, Kent BE. A new translucent cement for dentistry. The glass ionomer cement. Br Dent J. 1972;132:133-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 522] [Cited by in RCA: 442] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 6. | Smith AJ, Chimimba PD, Kalf-Scholte S, Bouma J. Clinical pilot study on new dental filling materials and preparation procedures in developing countries. Community Dent Oral Epidemiol. 1990;18:309-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Frencken JE, Peters MC, Manton DJ, Leal SC, Gordan VV, Eden E. Minimal intervention dentistry for managing dental caries - a review: report of a FDI task group. Int Dent J. 2012;62:223-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 310] [Cited by in RCA: 284] [Article Influence: 21.8] [Reference Citation Analysis (0)] |
| 8. | Cefaly DF, Tapety CM, Mondelli RF, Lauris JR, Phantumvanit P, Navarro MF. Three-year evaluation of the ART approach in Class III and V restorations in permanent anterior teeth. Caries Res. 2006;40:389-392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Arrow P, Forrest H. Atraumatic restorative treatments reduce the need for dental general anaesthesia: a non-inferiority randomized, controlled trial. Aust Dent J. 2020;65:158-167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 10. | Lopez N, Simpser-Rafalin S, Berthold P. Atraumatic restorative treatment for prevention and treatment of caries in an underserved community. Am J Public Health. 2005;95:1338-1339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 25] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Mickenautsch S, Frencken JE. Utilization of the ART approach in a group of public oral health operators in South Africa: a 5-year longitudinal study. BMC Oral Health. 2009;9:10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Sarita PT, Witter DJ, Kreulen CM, Van't Hof MA, Creugers NH. Chewing ability of subjects with shortened dental arches. Community Dent Oral Epidemiol. 2003;31:328-334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 91] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 13. | Jordan RA, Hetzel P, Franke M, Markovic L, Gaengler P, Zimmer S. Class III atraumatic restorative treatment (ART) in adults living in West Africa--outcomes after 48 months. Community Dent Oral Epidemiol. 2011;39:164-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Frencken JE, Pilot T, Songpaisan Y, Phantumvanit P. Atraumatic restorative treatment (ART): rationale, technique, and development. J Public Health Dent. 1996;56:135-40; discussion 161-3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 216] [Cited by in RCA: 221] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 15. | Leal S, Bonifacio C, Raggio D, Frencken J. Atraumatic Restorative Treatment: Restorative Component. Monogr Oral Sci. 2018;27:92-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 16. | Giacaman RA, Muñoz-Sandoval C, Neuhaus KW, Fontana M, ChaÅ‚as R. Evidence-based strategies for the minimally invasive treatment of carious lesions: Review of the literature. Adv Clin Exp Med. 2018;27:1009-1016. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 50] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 17. | Turton B, Patel J, Hill R, Sieng C, Durward C. Healthy Kids Cambodia – A novel approach to triage for dental care in a population with extreme caries experience. Community Dent Oral Epidemiol. 2020;48:56–62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 18. | Mallow PK, Durward CS, Klaipo M. Restoration of permanent teeth in young rural children in Cambodia using the atraumatic restorative treatment (ART) technique and Fuji II glass ionomer cement. Int J Paediatr Dent. 1998;8:35-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 41] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 19. | de Araujo MA, Araújo RM, Marsilio AL. A retrospective look at esthetic resin composite and glass-ionomer Class III restorations: a 2-year clinical evaluation. Quintessence Int. 1998;29:87-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 20. | Kumari PD, Khijmatgar S, Chowdhury A, Lynch E, Chowdhury CR. Factors influencing fluoride release in atraumatic restorative treatment (ART) materials: A review. J Oral Biol Craniofac Res. 2019;9:315-320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 21. | Prakki A, Nunes MC, Cefaly DF, Lauris JR, Navarro MF. Six-year evaluation of the atraumatic restorative treatment approach in permanent-tooth Class III restorations. J Adhes Dent. 2008;10:233-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 22. | Holmgren CJ, Frencken JE. Painting the future for ART. Community Dent Oral Epidemiol. 1999;27:449-453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 23. | Gugnani N, Gugnani S. ART with high viscosity GIC and composite restorations in class II cavities: can they thrive in the post-amalgam era? Evid Based Dent. 2020;21:22-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 24. | Molina GF, Cabral RJ, Frencken JE. The ART approach: clinical aspects reviewed. J Appl Oral Sci. 2009;17 Suppl:89-98. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 25. | Zanata RL, Navarro MF, Barbosa SH, Lauris JR, Franco EB. Clinical evaluation of three restorative materials applied in a minimal intervention caries treatment approach. J Public Health Dent. 2003;63:221-226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 26. | van Dijken JW. Longevity of new hybrid restorative materials in class III cavities. Eur J Oral Sci. 1999;107:215-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 27. | Cefaly DF, Barata Tde J, Tapety CM, Bresciani E, Navarro MF. Clinical evaluation of multisurface ART restorations. J Appl Oral Sci. 2005;13:15-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 28. | van 't Hof MA, Frencken JE, van Palenstein Helderman WH, Holmgren CJ. The atraumatic restorative treatment (ART) approach for managing dental caries: a meta-analysis. Int Dent J. 2006;56:345-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 105] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 29. | Moura MS, Sousa GP, Brito MHSF, Silva MCC, Lima MDM, Moura LFAD, Lima CCB. Does low-cost GIC have the same survival rate as high-viscosity GIC in atraumatic restorative treatments? A RCT. Braz Oral Res. 2020;33:e125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 30. | Osborne JW, Berry TG. 3-year clinical evaluation of glass ionomer cements as Class III restorations. Am J Dent. 1990;3:40-43. [PubMed] |
| 31. | Saber AM, El-Housseiny AA, Alamoudi NM. Atraumatic Restorative Treatment and Interim Therapeutic Restoration: A Review of the Literature. Dent J (Basel). 2019;7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 32. | Lo EC, Holmgren CJ. Provision of Atraumatic Restorative Treatment (ART) restorations to Chinese pre-school children--a 30-month evaluation. Int J Paediatr Dent. 2001;11:3-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 59] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 33. | Farag A, Frencken JE. Acceptance and discomfort from atraumatic restorative treatment in secondary school students in Egypt. Med Princ Pract. 2009;18:26-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |