Published online Sep 6, 2020. doi: 10.12998/wjcc.v8.i17.3903
Peer-review started: March 28, 2020
First decision: July 3, 2020
Revised: July 9, 2020
Accepted: July 30, 2020
Article in press: July 30, 2020
Published online: September 6, 2020
Processing time: 159 Days and 22.1 Hours
In December 2019, the first patient with 2019-novel coronavirus (2019-nCoV) was reported in Wuhan, China, and the disease spread rapidly across the country and surrounding countries within 2 mo. As of February 29, 2020, a total of 91 confirmed cases had been reported in Gansu Province. This case report of the diagnosis and treatment of an elderly patient with 2019-nCoV pneumonia complicated by acute exacerbation of chronic obstructive pulmonary disease in Gansu Province aims to provide a better reference for the treatment of patients in the future.
The patient, a 94-year-old female, lived in Maiji District of Tianshui, Gansu Province, China. On January 30, 2020, she was admitted to the Fourth People’s Hospital of Tianshui after 9 d of close contact with a patient with 2019-nCoV pneumonia. She was subsequently admitted to Gansu Provincial Hospital of Traditional Chinese Medicine for isolation and transferred to Tianshui Gansu Provincial Hospital of Infectious Diseases on February 3, 2020 for treatment. Upon initial examination, her body temperature was 36.7 °C , pulse was 80, breathing was 20, and blood pressure was 130/80 mmHg. She was conscious with normal development and normal nutrition. The pharynx was not red, and bilateral tonsils were not red and swollen. The lungs sounded slightly coarse with no dry or wet rales. The first symptoms were cough and fatigue on 2 February. The patient was hospitalized for 12 d. After active treatment, she was discharged on February 14 with a good prognosis.
A history of exposure to the affected area or patient is a major cause of 2019-nCoV infection, and population clustering is a high risk factor for transmission. Patients may not necessarily have respiratory system symptoms as the only clinical manifestation but may also have concomitant or first onset digestive symptoms. Attention should be paid to the prevention and treatment of multiple organ dysfunction syndrome. Nucleic acid testing is extremely important and needs to be repeated several times. Laboratory and auxiliary examination indicators during the first week of admission are extremely important. It is feasible to carry out dynamic and continuous index monitoring, which can predict and guide the prevention and treatment of multiple organ dysfunction and the prognosis of the disease.
Core tip: The 2019-novel coronavirus (nCoV) pneumonia, which is caused by a 2019-nCoV infection, is characterized by fever, weakness, and a dry cough. Severe cases can progress rapidly to acute respiratory distress syndrome, septic shock, and refractory metabolic acidosis. In this article, we describe a 94-year-old woman in Gansu province with an epidemiological history of cumulative exposure who was diagnosed with 2019-nCoV pneumonia during isolation and later presented with symptoms of cough and weakness. Acute exacerbation of chronic obstructive pulmonary disease was complicated during hospitalization. It was a severe case. After 12 d of active treatment, the patient was cured and discharged.
- Citation: He TP, Wang DL, Zhao J, Jiang XY, He J, Feng JK, Yuan Y. Diagnosis and treatment of an elderly patient with 2019-nCoV pneumonia and acute exacerbation of chronic obstructive pulmonary disease in Gansu Province: A case report. World J Clin Cases 2020; 8(17): 3903-3910
- URL: https://www.wjgnet.com/2307-8960/full/v8/i17/3903.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i17.3903
In December 2019, a group of 2019-novel coronavirus (2019-nCoV) cases were first reported in Wuhan, Hubei Province, China, and local health authorities confirmed that the outbreak may be related to wild animals in the south China Seafood Market in Wuhan[1-3]. In late January 2020, as the annual Spring Festival travel rush for China begins, large numbers of people begin to move, and more patients will appear in China and around the world for some time after that[4]. Experts later confirmed human-to-human transmission of the disease spreads rapidly[5,6]. Forty-nine countries reported cases by the end of February 2020[7].
This case was reported from a family cluster in Gansu Province. The first confirmed case was a returnee from Wuhan. On January 21, the patient had dinner with the man returning from Wuhan, and then they lived together. On January 28, the Wuhan resident presented with cough, fever (body temperature 38.9 °C on the same day), and throat discomfort at the fever clinic of the Second Hospital of Tianshui. A computerized tomography (CT) examination was immediately performed. The results showed that the lower lung scattered in a patchy, high density, and blurred image. The boundary was not clear. Due to a history of visiting the Wuhan epidemic area and a suspected case of 2019-nCoV pneumonia, he was admitted to the hospital for observation. After positive nucleic acid tests for two consecutive days, he was diagnosed. After the Wuhan native was diagnosed, the patient was then quarantined.
A 94-year-old women presented with cough and fatigue for 1 d after contact with infected persons for 13 d.
The patient had close contact for 13 d with another patient from Wuhan, who was confirmed to have 2019-nCoV pneumonia on February 2 after being rechecked for positive nucleic acid by the 2019-nCoV. She presented with cough, weakness, and no other symptoms. She was treated in isolation at the Second People’s Hospital of Tianshui. Chest CT showed multiple ground-glass changes in both lungs. Her blood count was 4.69 × 109/L, and lymphocyte count was 1.4 × 109/L. She was transferred to Tianshui Gansu Provincial Hospital of Infectious Diseases on 3 February for management treatment.
The patient was usually weak. For the past 20 years, the patient has experienced chronic obstructive pulmonary disease (COPD) symptoms (cough, expectoration, shortness of breath, fatigue) 2-3 times a year. However, there was no clear diagnosis and treatment. Otherwise, the patient had a good health record. History of vaccinations is unknown.
The patient grew up in the local area with nonepidemic area life history, nontoxic substance dust contact history, and no alcohol and tobacco habits. The patient’s family members were in good health and had no family history of hereditary diseases.
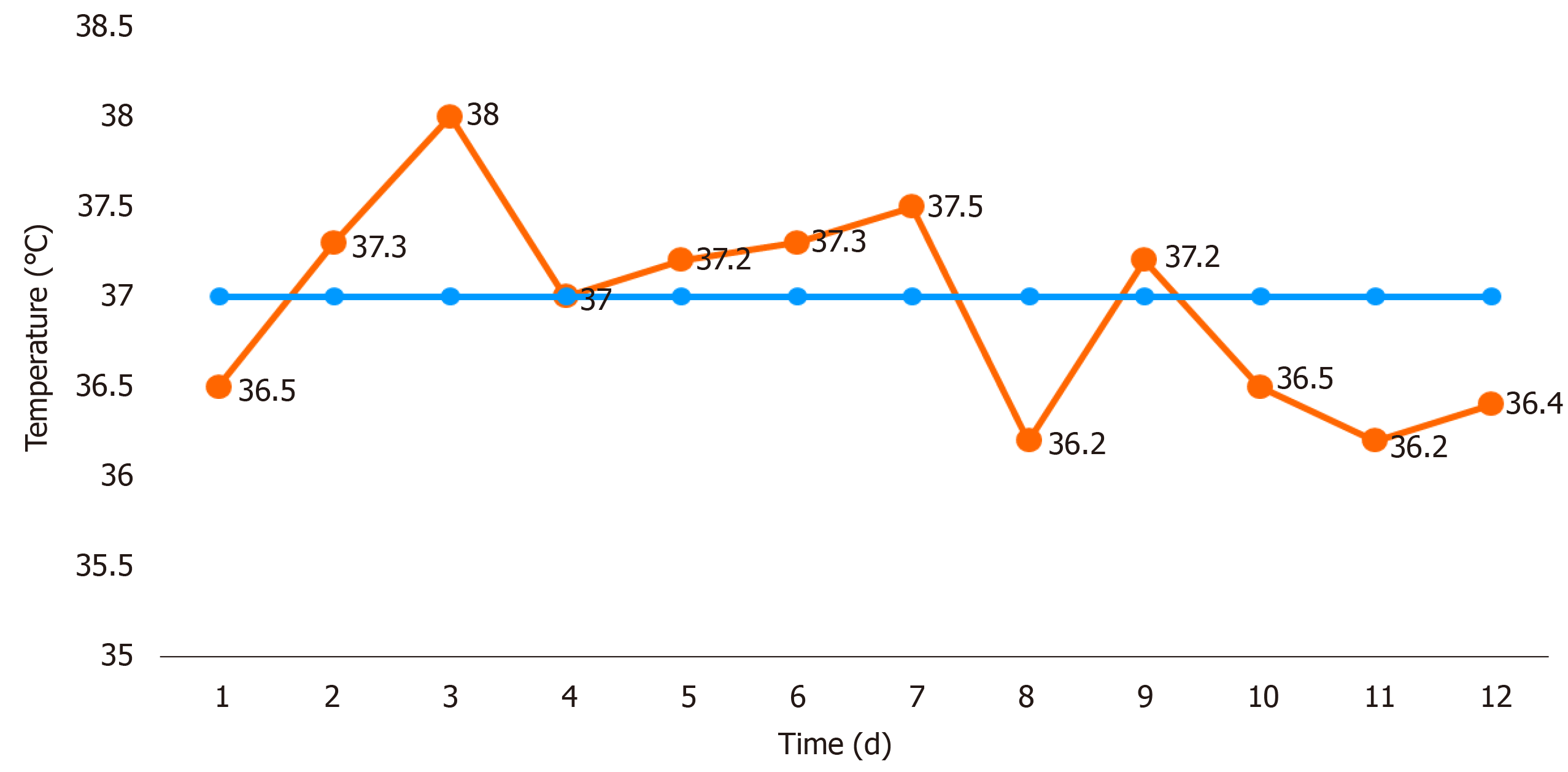
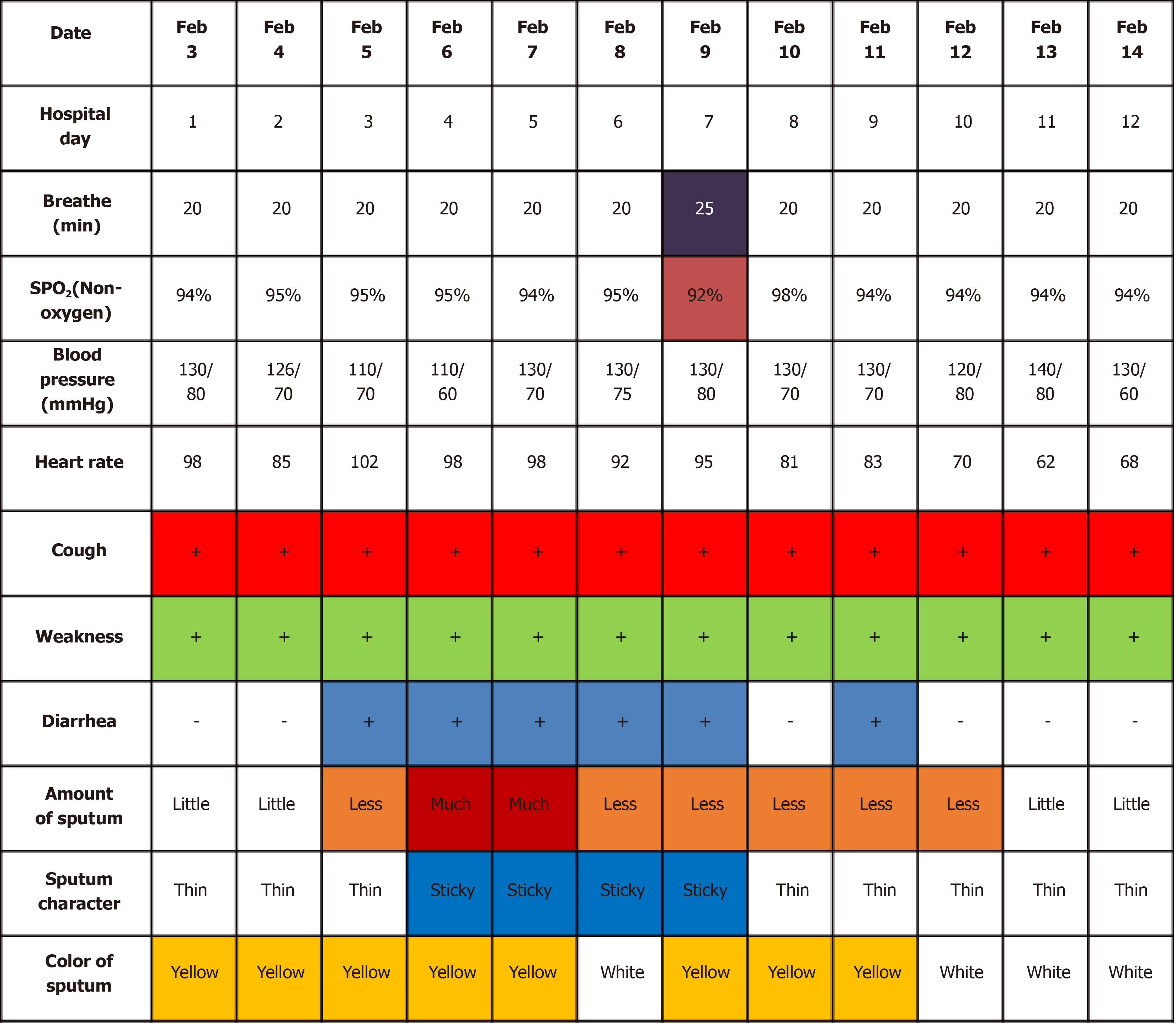
The patient developed fever on the 2nd to 7th d after admission (Figure 1). Acute exacerbation of chronic obstructive pulmonary disease (AECOPD) started on February 6 (the 4th d of admission) with a progressive increase in body temperature accompanied by marked increase in sputum volume, yellowing of color, and thickening of appearance. On the 7th d of admission, the patient experienced a decrease in oxygenation, but other vital signs were stable. No significant change was observed; cough and weakness were present throughout. Diarrhea and gastrointestinal dysfunction occurred after the 3rd d of hospitalization (Figure 2). After active treatment, the index gradually returned to normal after 1 wk in hospital.
During the period of hospitalization, the patient had a slight decrease of leukocytes and a progressive decrease of lymphocytes. In contrast to physical examination, the changes in laboratory parameters of AECOPD also began on February 6 (the 4th d of admission), with increased white blood cell count, high neutrophil count, high c-reactive protein, high creatinine, and high lactate dehydrogenase. She recovered gradually after 1 wk in hospital. At the time of discharge, except lymphocyte count, other indexes were recovered (Table 1).
| Hospital day | Day 1, Feb 3 | Day 4, Feb 6 | Day 6, Feb 8 | Day 8, Feb 10 | Day 12, Feb 14 | |
| Range | ||||||
| WBC as × 109/L | 3.50-9.50 | 3.51 | 8.00 | 5.72 | 4.14 | 6.43 |
| GRAN as × 109/L | 1.80-6.30 | 2.07 | 6.47 | 4.50 | 3.56 | 5.75 |
| LYM as × 109/L | 1.10-3.20 | 1.03 | 1.07 | 0.78 | 0.45 | 0.46 |
| PLT as × 109/L | 125-350 | 44 | 89 | 56 | 113 | 130 |
| HGB in g/L | 115-175 | 124 | 125 | 98 | 103 | 95 |
| Na+ in mmol/L | 135-145 | 134 | 136 | - | 143 | 144 |
| K+ in mmol/L | 3.50-5.10 | 3.92 | 4.20 | - | 4.71 | 5.00 |
| GLU in mmol/L | 3.90-6.10 | 7.34 | 4.85 | - | 8.14 | 8.07 |
| CRP in mg/L | 0-10.0 | 54.0 | 129.3 | - | 120.0 | 35.6 |
| CRE in μmol/L | 44.0-106.0 | 92.9 | 134.5 | - | 88.0 | 93.0 |
| BIL in μmol/L | 3.4-17.1 | 9.5 | 11.5 | - | 8.5 | 11.4 |
| AST in U/L | 0-35 | 33 | 49 | - | 53 | 22 |
| ALT in U/L | 0-40 | 8 | 16 | - | 31 | 22 |
| LDH in U/L | 120-250 | 210 | 270 | - | 322 | 239 |
| HBDH in U/L | 72-182 | 168 | 182 | - | 155 | 152 |
| CK in U/L | 40-200 | 72 | 701 | - | 158 | 46 |
| D-dimer in μg/mL | 0-0.50 | 0.35 | - | - | 0.40 | - |
| APTT in s | 22.0-38.0 | 33.1 | - | - | 29.6 | - |
| TT in s | 14.0-21.0 | 14.6 | - | - | 18.5 | - |
| FIB in g/L | 2.0-4.0 | 3.4 | - | - | 7.6 | - |
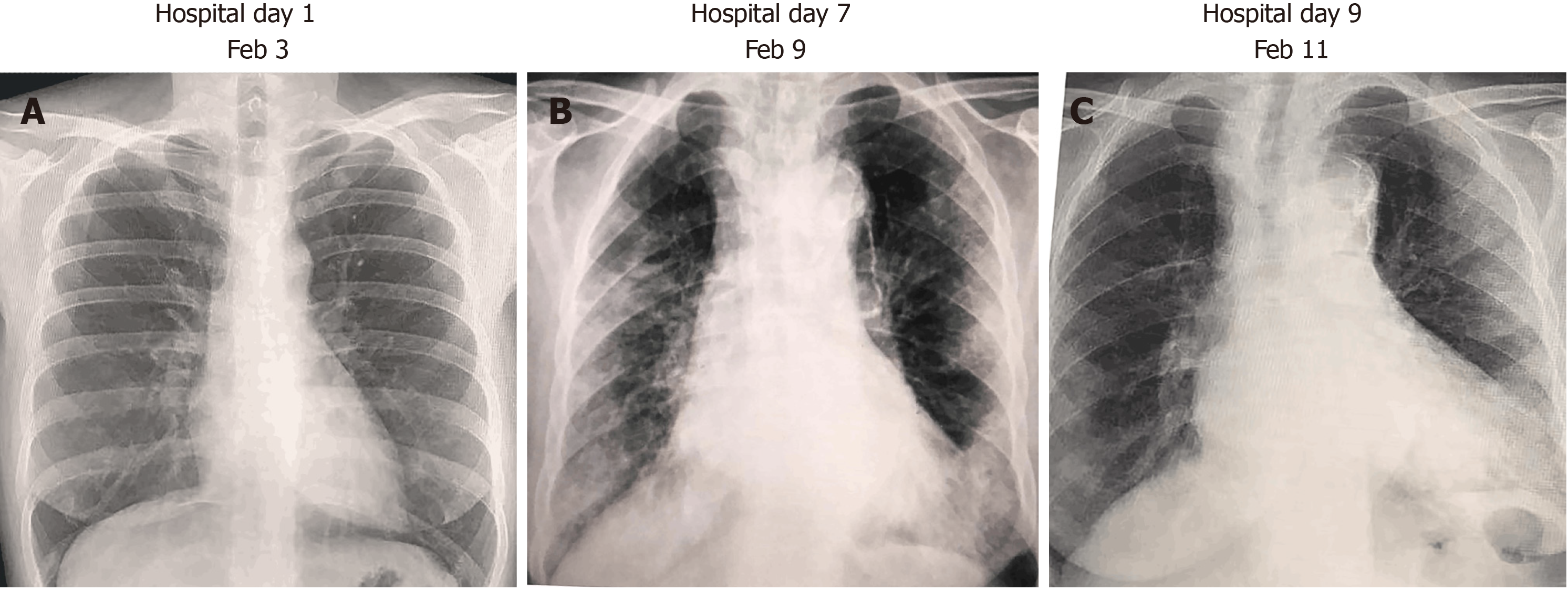
Prior to admission, the typical signs at the early stage of the disease were thickening and disorder of lung texture and exudative lesions (Figure 3A). At day 7 after admission, the bilateral lung increased in texture and density with cords and dots. The outer bands of bilateral lungs showed ground glass-like changes, and the lower left lobe showed uneven density (Figure 3B). At day 9 after admission, the bilateral lung increased in texture and density with cords and dots. The outer bands of bilateral lungs showed ground glass-like changes, and the lower left lobe showed uneven density (Figure 3C). Compared with imaging findings on February 9, the focus was absorbed obviously.
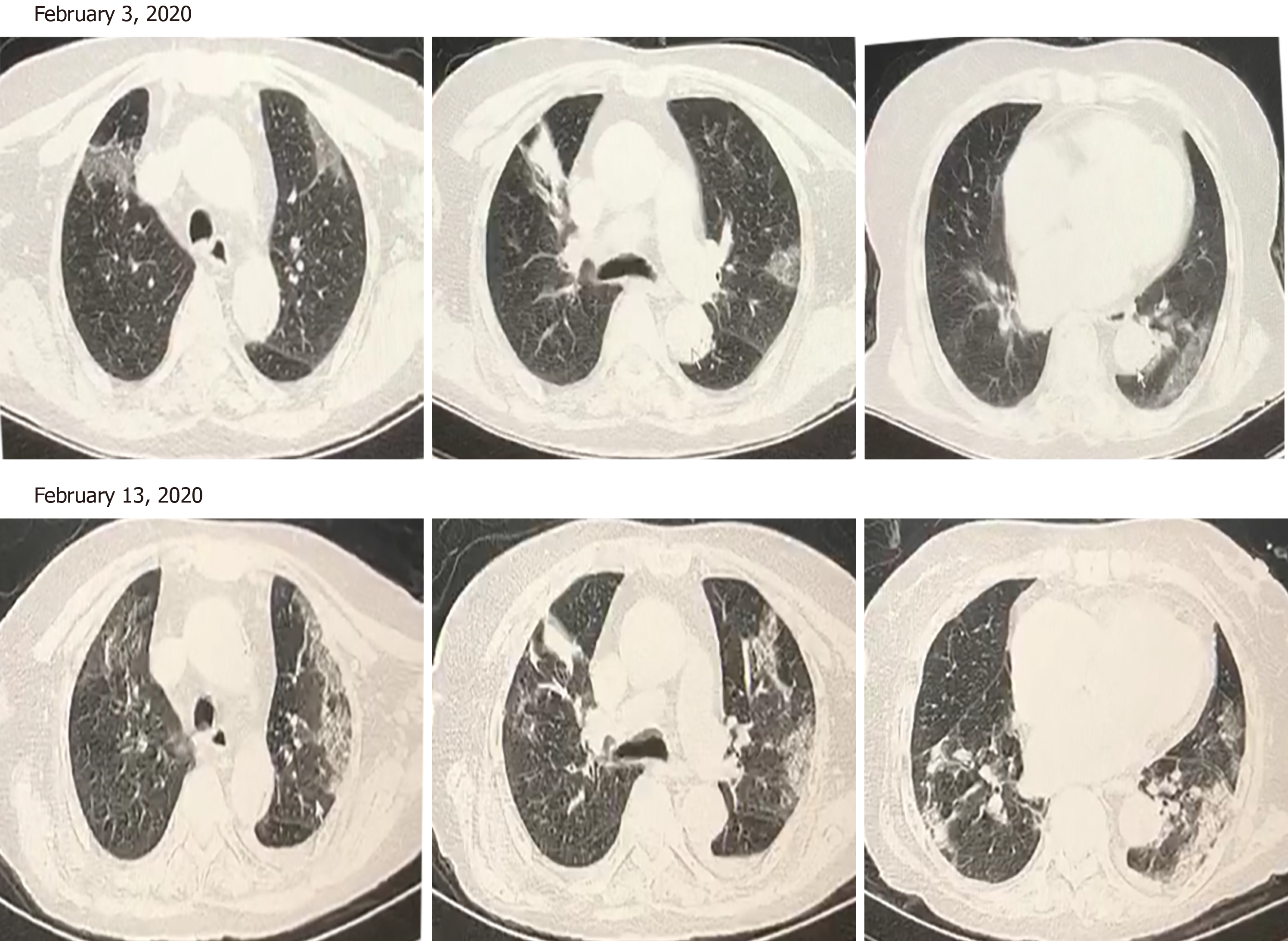
After aggressive treatment, the lesions were absorbed significantly, and the imaging changes of 2019-nCoV pneumonia could be better demonstrated on high resolution CT (Figure 4). On February 3, 2020, the 1st d of admission, CT showed multiple ground-glass shadows and old striated shadows in the lung. On February 13, 2020 (before discharge from hospital), CT showed some absorption of the lesion with partial ground-glass shadows and late reticulated shadows and striated shadows.
Nucleic acid test was performed. The first positive time of nucleic acid test was February 1, 2 d before admission. The last positive test was February 7 (Table 2).
| Specimen | 2 d before hospitalization, Feb 1 | 1 d before hospitalization, Feb 2 | Hospital day 5, Feb 7 | Hospital day 5, Feb 11 | Hospital day 5, Feb 12 |
| Oropharyngeal swab | Positive | Positive | Positive | Negative | Negative |
The patient was diagnosed as having 2019-nCoV pneumonia, according to the criteria in the current diagnostic protocol for 2019-nCoV pneumonia (third edition)[8].
The suspected case (the original observed case) at the same time conforms to the following two items: (1) Epidemiological history, history of travel or residence in Wuhan within 2 wk prior to onset, or exposure to fever with respiratory symptoms from Wuhan within 14 d prior to onset, or clustering; (2) Clinical manifestations: fever with the above-mentioned imaging features of pneumonia, early onset of normal or decreased white blood cell count, or lymphocyte count.
On the basis that the confirmed case met the criteria of the suspected case, the sputum, throat swab, and lower respiratory tract secretion samples can be tested for positive 2019-nCoV nucleic acid by real-time fluorescent reverse transcription polymerase chain reaction, or the virus gene can be sequenced.
After the patient was admitted to the hospital, she was treated according to national guidelines[8]: 100 mg Ribavirin was given three times a day for 12 d; Lianhua Qingwen capsule three times a day for 5 d; and Qingfei Paidu decoction for 12 d. On February 6, the patient presented with AECOPD and received intravenous infusion of 40 mg methylprednisolone sodium succinate once a day for 4 d, oral ceftazidime for 7 d, moxifloxacin for 5 d, oral doxofylline tablets, Montelukast Sodium Chewable Tablets, and inhaled budesonide formoterol powder three times a day for 3 d. After several days of active treatment, the patient’s fever, cough, and expectoration symptoms improved significantly.
On February 13, the patient was without fever and cough. Oxygenation levels were at 94%. Her fatigue and appetite improved, and ribavirin, ceftazidime, and other treatments were stopped. After observation, she was discharged on February 14, and the results were as follows: routine blood examination showed that the number of leukocytes was 6.43 × 109/L, neutrophils were 5.75 × 109/L, lymphocytes were 0.46 × 109/L, and platelets were 130 × 109/L; biochemical examination showed no obvious abnormality; chest CT was reexamined (compared with the former, the ground glass lesions of both lungs were absorbed); and the nucleic acid from pharyngeal swab was negative on February 11,2020 and February 12,2020 (the interval was more than 24 h). The novel coronavirus pneumonia was cured by the consultation of provincial and municipal experts. It was recommended to further adjust the heart and lung function in a general hospital. In the follow-up specialized treatment of COPD, traditional Chinese medicine suggested warming the lung and resolving phlegm for symptomatic treatment, strengthen oral nutrition, properly exercise, pat the back regularly, and encourage cough and expectoration. At present, the prognosis is good without repetition.
This article reported the diagnosis and treatment of the oldest patient with 2019-nCoV pneumonia in Gansu Province. The patient is old, complicated with COPD, and is at risk of serious illness and high mortality. The patient was stable in the early stage and developed fever, respiratory failure, and cough with a lot of yellow sputum after AECOPD. Based on the changes in the patient’s condition and the common etiological characteristics of elderly patients with COPD, the consulting team treated her with antiviral therapy in accordance with the guidelines, combined with antibiotic therapy. This improved airway obstruction, reduced airway inflammation and airway hyperresponsiveness, relieved sputum, and promoted sputum drainage. The patient’s condition gradually improved and was eventually cured and discharged. The patient was discharged with a diagnosis of 2019-nCoV pneumonia (severe) and AECOPD.
Because there is no specific drug for 2019-nCoV[9], this patient was treated with a combination of traditional Chinese medicine and Qingfei Paidu decoction in order to clear the lungs, relieve cough, reduce fever, resolve sputum, and regulate digestive function of the auxiliary treatment[10].
The patient was a second-generation case who had close contact with people returning to Gansu from Wuhan. The epidemiological history was clear, and nine people in the same family developed the disease successively. Therefore, strengthening the management of infected areas and confirmed patients while avoiding the movement and gathering of people during the epidemic period is an important means to prevent the regional epidemic of 2019-nCoV pneumonia. It is hoped that the treatment experience of this novel coronavirus pneumonia patient will be provided with more references in the future.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Montemurro N S-Editor: Zhang L L-Editor: Filipodia P-Editor: Xing YX
| 1. | World Health Organization. Emergencies preparedness, response. Pneumonia of unknown cause - China. 5 January 2020. Available from: https://www.who.int/csr/don/05-january-2020-pneumonia-of-unkown-cause-china/en/. |
| 2. | World Health Organization. Emergencies preparedness, response. Novel coronavirus - China. 12 January 2020. Available from: https://www.who.int/csr/don/12-january-2020-novel-coronavirus-china/en/. |
| 3. | Wuhan City Health Commission. Wuhan Municipal Commission of Health and viral pneumonia report on unknown causes. 3 January 2020. Available from: http://wjw.wuhan.gov.cn/front/web/showDetail/2020010309017. |
| 4. | Xu XW, Wu XX, Jiang XG, Xu KJ, Ying LJ, Ma CL, Li SB, Wang HY, Zhang S, Gao HN, Sheng JF, Cai HL, Qiu YQ, Li LJ. Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan, China: retrospective case series. BMJ. 2020;368:m606. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 5. | Centers for Disease Control and Prevention. 2019 Novel coronavirus, Wuhan, China: 2019-nCoV situation summary. 28 January 2020. Available from: https://www.cdc.gov/ coronavirus/2019-nCoV/summary.html. |
| 6. | National Health Commission of the People's Republic of China-disease Control and Prevention Bureau. Circular on the issuance of guidelines for the prevention of 2019-ncov infection in different risk groups and guidelines for the use of pneumonia masks for the prevention of 2019-ncov infection. 30 January 2020. Available from: http://www.nhc.gov.cn/jkj/s7916/202001/a3a261dabfcf4c3fa365d4eb07ddab34.shtml. |
| 7. | World Health Organization. WHO Director-General's opening remarks at the media briefing on COVID-19 - 28 February 2020. 28 February 2020. Available from: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---28-february-2020. |
| 8. | Office of the State Administration of Traditional Chinese Medicine. Circular on the trial implementation of the third edition of the 2019-ncov for pneumonia diagnosis and treatment. 22 January 2020. Available from: http://www.gov.cn/zhengce/zhengceku/2020-01/23/content_5471832.htm. |
| 9. | Cheng SC, Chang YC, Fan Chiang YL, Chien YC, Cheng M, Yang CH, Huang CH, Hsu YN. First case of Coronavirus Disease 2019 (COVID-19) pneumonia in Taiwan. J Formos Med Assoc. 2020;119:747-751. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 129] [Cited by in RCA: 133] [Article Influence: 26.6] [Reference Citation Analysis (0)] |
| 10. | Health Commission of Gansu Province. Circular on Printing and distributing the scheme of prevention and treatment of pneumonia with traditional Chinese medicine (trial implementation) for 2019-ncov infection in Gansu Province. 24 January 2020. Available from: http://wsjk.gansu.gov.cn/single/10991/83064.html. |