Published online Sep 6, 2020. doi: 10.12998/wjcc.v8.i17.3867
Peer-review started: March 20, 2020
First decision: July 25, 2020
Revised: August 2, 2020
Accepted: August 15, 2020
Article in press: August 15, 2020
Published online: September 6, 2020
Processing time: 168 Days and 4.9 Hours
Although choriocarcinoma is thought to be a malignancy curable by chemotherapy, there remain difficult and challenging problems in cases with high prognostic scores or extensive metastases, for which the treatment is limited. Particularly, chemotherapy in combination with other treatments offers promising therapeutic potential for these cases.
We present the case of a 40-year-old female patient who suffered from life-threatening hemoptysis and paraplegia due to choriocarcinoma with pulmonary, hepatic and spinal metastases. The patient successfully recovered after multidisciplinary treatment consisting of 21 cycles of intravenous chemotherapy, radiofrequency ablation of multiple hepatic metastases, intensity-modulated radiation therapy for spinal metastases and routine physiotherapy. To our knowledge, it is the first reported case of recovery from pulmonary, hepatic and spinal metastases of choriocarcinoma with no specific primary site. Moreover, this is the first reported clinical attempt on 5-d actinomycin D as primary chemotherapy in ultrahigh-risk gestational trophoblastic neoplasia.
The case supports the opinion that the individualized treatment of choriocarcinoma by a multidisciplinary approach can accomplish optimal therapeutic effects.
Core tip: In this case report, we discuss a case of choriocarcinoma in a patient who presented with life-threatening hemoptysis and paraplegia due to metastases. We review her clinical manifestation and treatment, subsequently discussing the multidisciplinary treatment approach used to successfully treat this patient. Our study provides a new treatment modality for metastatic choriocarcinoma.
- Citation: Lin YY, Sun Y, Jiang Y, Song BZ, Ke LJ. Multidisciplinary treatment of life-threatening hemoptysis and paraplegia of choriocarcinoma with pulmonary, hepatic and spinal metastases: A case report. World J Clin Cases 2020; 8(17): 3867-3874
- URL: https://www.wjgnet.com/2307-8960/full/v8/i17/3867.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i17.3867
Choriocarcinoma is a highly malignant form of gestational trophoblastic disease that spreads rapidly throughout the body[1]. It can metastasize or infiltrate into adjacent tissues including the tubes and ovaries or spread to distant sites via blood circulation. The most common sites of metastases are the lungs, vagina, liver, brain and digestive tracts. Spinal metastasis of choriocarcinoma is extremely rare[2]. Moreover, the common symptom is most frequently hemorrhage due to metastases, presenting as vaginal bleeding, hemoptysis or hematemesis.
Modern treatment of choriocarcinomas involves chemotherapy followed by radiation or surgery, resulting in a cure rate approaching 90%. However, drugs commonly used for cancer treatment have barriers such as drug resistance and side effects[3]. Furthermore, the optimal treatment strategies for metastatic choriocarcinomas remain controversial. Therefore, a collaboration of multidisciplinary providers may help with development of novel treatment strategies that can maximize efficacy and minimize toxic effects. This is especially beneficial as new strategies for the stable treatment of metastatic choriocarcinoma are urgently needed in some patients. Chemotherapy in combination with other treatments may be a strategy that opens the door to promising therapeutic options.
A 40-year-old woman attended the emergency department on December 18, 2017 for progressively increasing hemoptysis of half month’s duration. At first, the patient presented with coughing and slight hemoptysis along with lower back pain, though she denied having dizziness or headache. The attending physician diagnosed the patient with pneumonia; however no improvement was observed with the use of antibiotics or high doses of corticosteroids. The symptoms, especially the hemoptysis, had worsened in the past half month with progressive lower limb weakness.
Her medical history included cesarean on three occasions, the last occurring about 10 mo prior to hospitalization. The postpartum lochia after the latest cesarean was minimal. Six months postpartum, menstruation resumed with occasional intermittent vaginal spotting.
The patient demonstrated distressed breathing and backache. Lung examination revealed bilateral lung crackles. Neurological examination revealed the loss of all sensations below the Th10 level with flaccid paraplegia. Vaginal examination was normal.
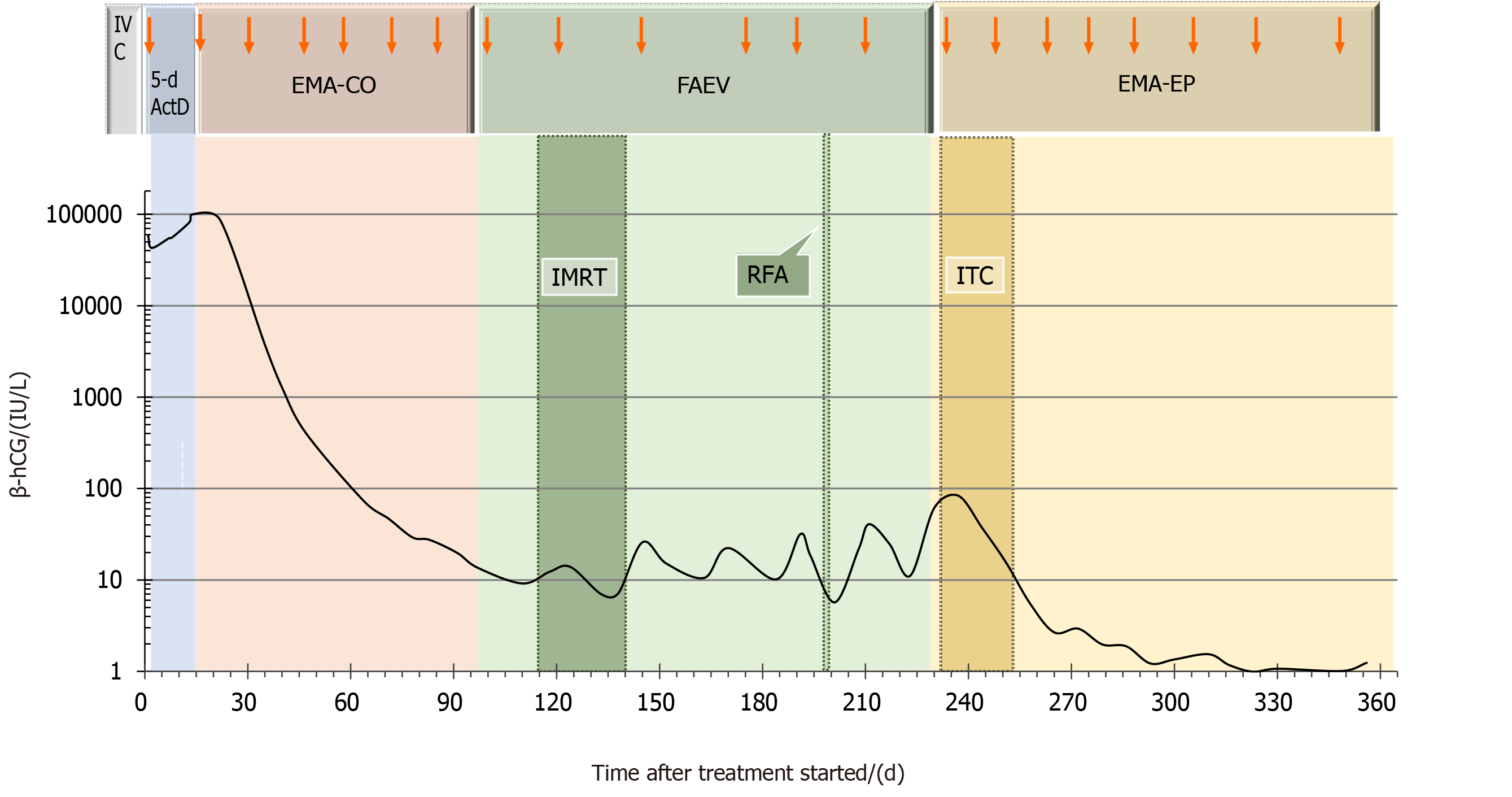
Laboratory tests revealed a white blood cell count of 15.3 × 109/L, neutrophil count of 14.4 × 109/L and hemoglobin of 10.9 g/dL (Table 1). Blood gas analysis showed (FiO2 49%): PH 7.47, PaO2 57.3 mmHg, PaCO2 34.5 mmHg and OI 117 mmHg. Serum β-human chorionic gonadotropin (β-hCG) was 58162.0 IU/L (Figure 1). A repeat β-hCG showed a continuously rising trend, up to 100014.0 IU/L.
| Age in yr | 40 | ||||||||
| Gender | Female | ||||||||
| City | Sanming, Fujian, China | ||||||||
| Dates of enrollment | 12/18/2017 | ||||||||
| Duration of treatment stay in d | 361 | ||||||||
| Symptoms and signs at enrollment | |||||||||
| Fever | No | ||||||||
| Headache/dizziness | No | ||||||||
| Hemoptysis | Yes | ||||||||
| Shortness of breath | Yes | ||||||||
| Cough | Yes | ||||||||
| Nausea/vomiting | No | ||||||||
| Lower back pain | Yes | ||||||||
| Vaginal bleeding | No | ||||||||
| Laboratory results (normal value range) | Day 1 enrollment | Day 2 enrollment | Day 3 enrollment | After one cycle of chemotherapy | After MDT and before discharge | ||||
| White blood cell count (3.5-9.5 × | 15.3 | 10.3 | 13.8 | 16.2 | 17.1 | ||||
| Neutrophil count (1.8-6.3 × 109/L) | 14.4 | 8.4 | 12.5 | 12.7 | 15.2 | ||||
| Platelet count (125-350 × 109/L) | 194 | 138 | 112 | 183 | 38 | ||||
| Hemoglobin (11.5-15.0 g/dL) | 10.9 | 9.1 | 5.8 | 9.2 | 9.3 | ||||
| Total protein (63-82 g/L) | 56 | 47 | 37 | 58 | 65 | ||||
| Albumin (35-50 g/L) | 32 | 29 | 22 | 35 | 34 | ||||
| Aspartate aminotransferase (13-69 U/L) | 52 | 35 | 37 | 40 | 20 | ||||
| Alanine aminotransferase (15-46 U/L) | 25 | 23 | 34 | 49 | 50 | ||||
| Blood urea nitrogen (2.5-6.1 mmol/L) | 4.1 | 4.0 | 6.8 | 3.1 | 2.9 | ||||
| Serum creatinine (46-92 μmol/L) | 44 | 33 | 48 | 47 | 54 | ||||
| β-hCG (< 5 IU/L) | ND | ND | 58162 | ND | ND | ||||
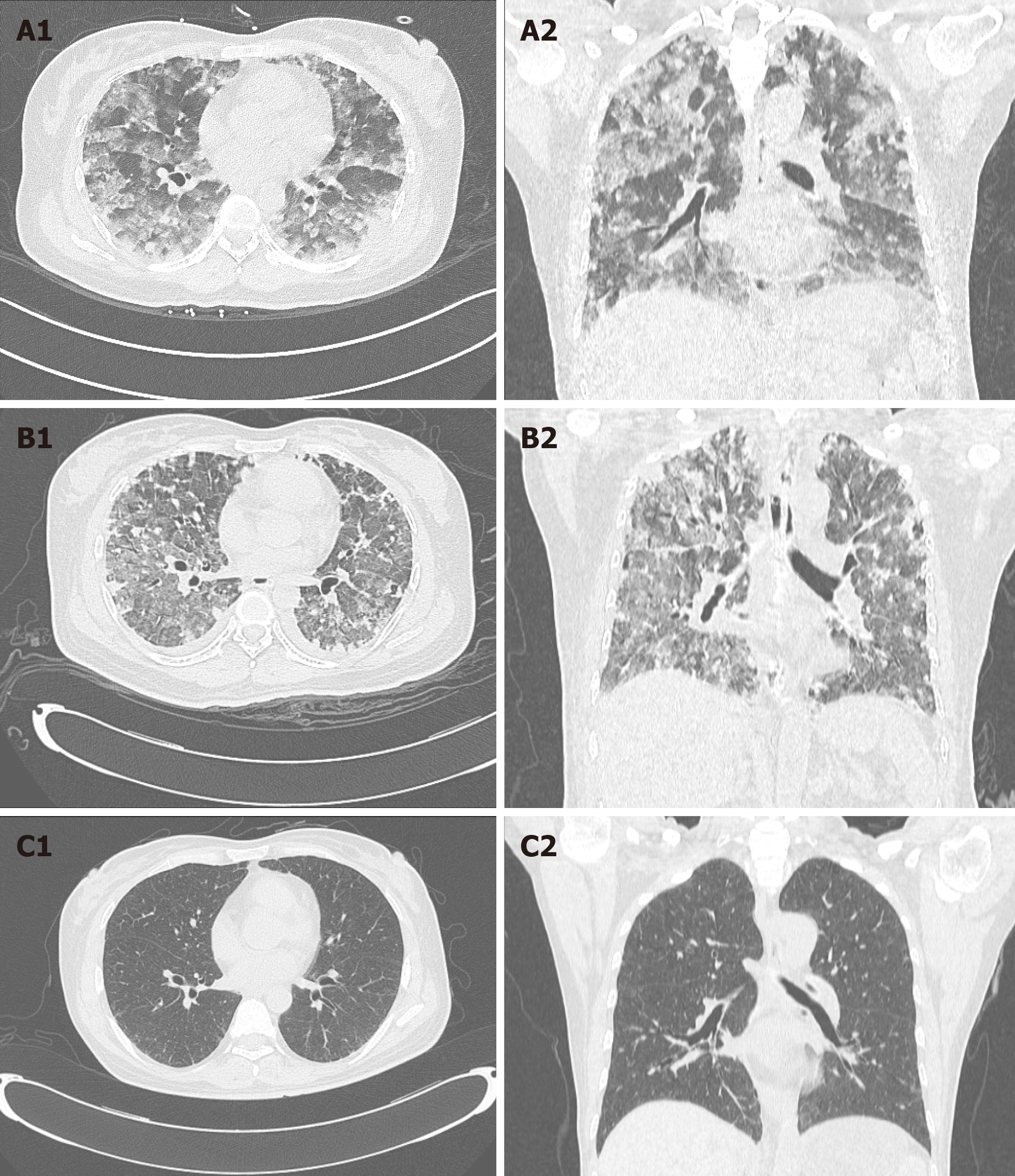
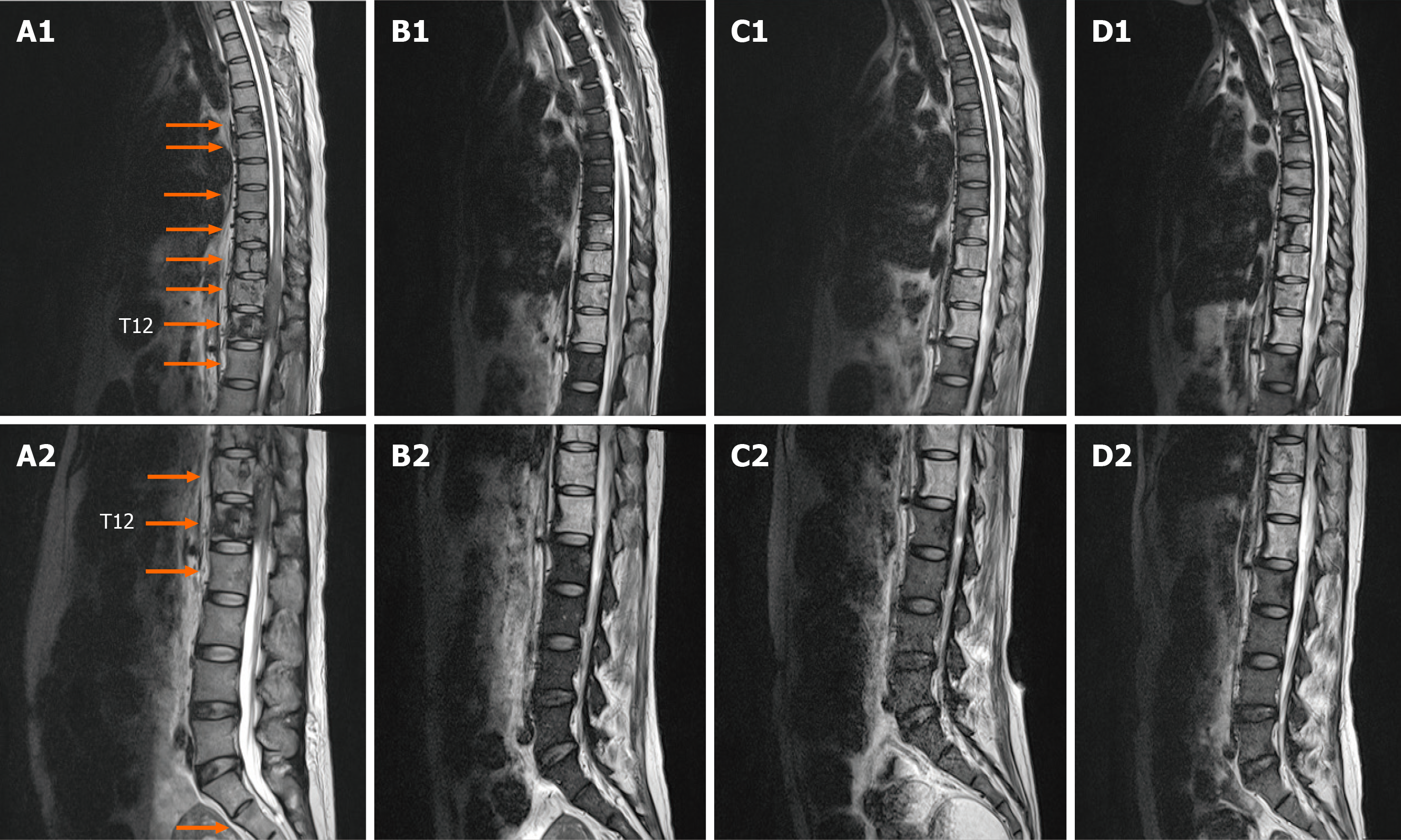
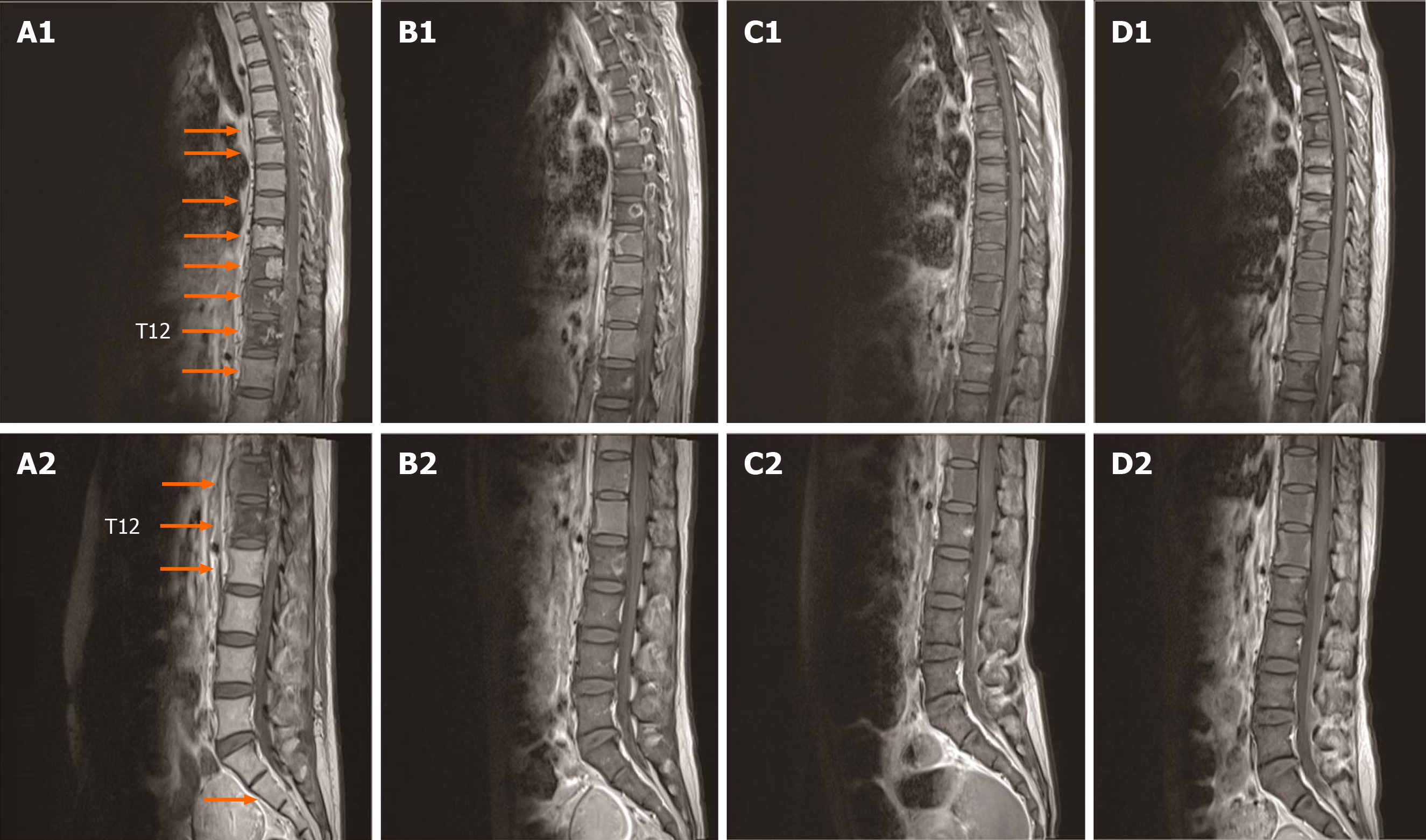
Repeat transvaginal ultrasound with Doppler showed a thin endometrial lining and normal color bloodstream signal in the endometrial cavity. Ultrasonography of the abdomen revealed multiple masses in the liver. The biggest was approximately 31 mm × 25 mm. Chest computed tomography (CT) revealed nodular opacity lesions distributed in both lungs (Figure 2). Spinal magnetic resonance imaging revealed multiple mass lesions at the portion of the body aligning at the Th5-6, Th8-12, L1 and S2 levels and involving the dorsal portion of the spinal canal at the Th9–L1 level (Figures 3 and 4). Cranial CT was normal.
According to these findings, the patient was classified as ultrahigh-risk (score 16) based on the World Health Organization prognostic scoring system. The patient was diagnosed with stage IV choriocarcinoma and concomitantly with type 1 respiratory failure and paraplegia.
During her second day of hospitalization, the patient developed an episode of sudden hemoptysis resulting in hypovolemic shock, and hemoglobin levels decreased to a low of 5.8 g/dL. Bedside fiberoptic bronchoscopy showed a massive accumulation of blood in the distal trachea. Repeated vasopressin was administered locally, and antibiotics and blood transfusion were also given. However, the patient did not improve. The patient was alleviated by trachea reintubation with mechanical ventilation, but hemoptysis remained serious.
Subsequently, a multidisciplinary team was set up quickly, including gynecology oncologists, respiratory physicians, neurologist, surgeons, radiologists, Chinese pharmacists and physiatrists. After careful consideration and fully informed consent, the patient took the risk of receiving an urgent regimen of 5-d actinomycin D (10 μg/kg per day for 5 d) as primary chemotherapy. After one cycle of chemotherapy, hemoptysis was significantly reduced, and the patient was weaned from mechanical ventilation and referred to the gynecology ward.
In the gynecology ward, the standard multiagent chemotherapy regimen using EMA-CO (etoposide, methotrexate, actinomycin-D, vincristine and cyclophos-phamide) was initiated. As supportive therapy, granulocyte colonic stimulating factor, thrombopoietin, dexamethasone, traditional Chinese medicine and external treatment, including acupuncture, acupoints and therapeutic type exercise, were also given when necessary. After six cycles of chemotherapy, the serum β-hCG level was 19.0 IU/L, however the patient continued to experience unbearable lower back pain requiring morphine. Later, the characteristic multiagent chemotherapy regimen using FAEV (floxuridine, dactinomycin, etoposide and vincristine) was started. During this chemotherapy interval, the patient underwent 18 radiotherapy sessions to the thoracic and lumbar spine with a total dose of 36 Gy in the form of intensity-modulated radiation therapy. After radiation, the pain subsided completely, and the patient gradually recovered partial mobility. A repeat spinal magnetic resonance imaging showed the nodular images in the centrum regressed (Figures 3 and 4). However, abdominal CT revealed multiple, persistent nodular lesions in the liver; the largest measured approximately 3.0 cm × 2.4 cm. After CT-mediated percutaneous radiofrequency ablation of the right liver, metastatic foci of the liver were shrunk. Despite this, the patient progressed with total increasing levels of β-hCG approaching 40.0 IU/L. Due to cerebrospinal fluid β-hCG levels of 20.6 IU/L, the patient received eight cycles of the second-line chemotherapy regimen using EMA-EP (methotrexate, etoposide, actinomycin D, etoposide and cisplatin), including four cycles of consolidation chemotherapy as well as four cycles of intrathecal methotrexate injections. After the administration of intrathecal methotrexate injections, the β-hCG level in the cerebrospinal fluid lowered to 1.6 IU/L. A repeat chest CT demonstrated normal results by the end of the treatment (Figure 2). A detailed record is provided in Figure 1.
By discharge, the patient had regained some function of her lower extremities (1-2 out of 5 on neurological motor examination). During 1-year follow-up, the patient appeared well, and serial β-hCG estimations were within normal ranges.
According to the criteria for nongestational choriocarcinoma diagnosis, the patient was diagnosed with choriocarcinoma with no pathologically confirmed origin site. No visible and palpable lesions in the uterus or adnexa were detected, whereas the lungs, liver and spine showed features of metastases. This case is rare given that the majority of cases of choriocarcinoma are of uterine origin. It could be hypothesized that the rapid growth of the tumors infiltrated the endometrium and myometrium causing regression of the primary tumor then spreading to lungs and the other distant sites by hematogenous metastasis. As metastatic lesions slowly enlarge, they are usually accompanied by hemorrhage, necrosis and vascular invasion. In the lungs, this could cause hemoptysis complicated by infection, which can lead to airway obstruction or even cardiorespiratory failure. In the spine, lesion enlargement can cause backache and progressive impairment of nerves. Clinically, these subtle signs and symptoms could easily be attributed to pulmonary infection and lumbar muscle strain, resulting in misdiagnosis and treatment delay. The findings of this case suggest that the possibility of choriocarcinoma should be borne in mind when a woman of reproductive age presents with metastatic disease of an unknown primary site.
The patient in this case had a risk score of 16 and coexisting pulmonary, hepatic and spinal metastases. Thus, this lesion belonged to a category of ultrahigh-risk gestational trophoblastic neoplasia as designated by the 2018 International Federation of Gynecology and Obstetrics guidelines. Consequently, the tumor subgroup is accompanied by a poor prognosis[4]. Women with high risk scores are more likely to develop resistance to single-agent chemotherapy and are therefore likely to benefit from combination chemotherapy. However, because of the severity and urgency of the patient’s general medical condition, initiation of standard chemotherapy or low-dose induction etoposide-cisplatin is usually prescribed and may actually cause metastatic lesion necrosis in large areas, leading to deadly massive hemoptysis, respiratory failure, septicemia or multiple organ failure. Hence, the initial chemotherapy regimen administered to this patient was a mono-therapy “5-d actinomycin D,” adjusted to the standard chemotherapy regimen of EMA-CO, and subsequently FAEV and EMA-EP after the patient’s condition improved.
Hepatic metastasis, however, is not common and is insensitive to chemotherapy. There is currently no consensus on the best management strategy for hepatic metastases. Recent reviews of the management of choriocarcinoma with hepatic metastasis support benefits of multimodality therapy, including surgical resection[5], local radiotherapy[6] and hepatic artery embolization[7]. In the present case, the patient was treated by CT-mediated percutaneous radiofrequency ablation, the advantages of which include safety and effectiveness due to its simplicity and minimal invasiveness. The strategy can be used to destroy target regional tumor cells and the local tumor blood supply, reducing local tumor burden and to some extent minimizing chemotherapy resistance.
Bone metastases secondary to choriocarcinoma are extremely rare events with poor treatment response. Treatment of bone metastases has consisted of either chemoradiotherapy[8], surgical resection[2] or other combined approach[9]. Successful treatment has been reported in only one case, in which the patient was cured by embolization of the lesion of the lumbar spine and subtotal removal of the epidural mass[9]. Given the widespread bone involvement in the current case, the patient was not well suited for surgery. Thus, multidrug chemotherapy combined with spinal intensity-modulated radiation therapy was performed. Compared with EMA-CO and EMA-EP , FAEV chemotherapy obtained longer intervals between cycles with well-tolerated toxicity, enabling the patient to receive an adequate course of radiotherapy. By attenuating symptoms of spinal cord compression and alleviating pain, intensity-modulated radiation therapy could potentially achieve the best control of spinal metastasis, though more information is needed to verify this hypothesis.
Currently, chemotherapy remains the only potentially curative therapy for choriocarcinoma, and surgery and radiotherapy may have roles in certain cases. However, developments in modern medicine could open up new horizons of treatment options for the clinician.
We have presented the first reported case of choriocarcinoma with pulmonary, hepatic and spinal metastases of unknown specific primary site. Choriocarcinoma should be suspected in any woman of reproductive age with metastatic disease from an unknown primary[10]. Moreover, this case demonstrated that administration of 5-d actinomycin D as primary chemotherapy is feasible and tolerable in critical condition, though more cases are needed to verify. The case supports the opinion that by providing a close multidisciplinary collaboration, patients suffering from metastatic choriocarcinoma, especially those with high prognostic scores or extensive metastases, may benefit from the individualized treatment and achieve the best therapeutic results.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Grawish M, Skok P S-Editor: Yan JP L-Editor: Filipodia P-Editor: Wang LL
| 1. | Seckl MJ, Sebire NJ, Berkowitz RS. Gestational trophoblastic disease. Lancet. 2010;376:717-729. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 540] [Cited by in RCA: 554] [Article Influence: 36.9] [Reference Citation Analysis (0)] |
| 2. | Naito Y, Akeda K, Kasai Y, Matsumine A, Tabata T, Nagao K, Uchida A. Lumbar metastasis of choriocarcinoma. Spine (Phila Pa 1976). 2009;34:E538-E543. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Chen Y, Qian H, Wang H, Zhang X, Fu M, Liang X, Ma Y, Zhan Q, Lin C, Xiang Y. Ad-PUMA sensitizes drug-resistant choriocarcinoma cells to chemotherapeutic agents. Gynecol Oncol. 2007;107:505-512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 4. | Ngan HYS, Seckl MJ, Berkowitz RS, Xiang Y, Golfier F, Sekharan PK, Lurain JR, Massuger L. Update on the diagnosis and management of gestational trophoblastic disease. Int J Gynaecol Obstet. 2018;143 Suppl 2:79-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 180] [Cited by in RCA: 236] [Article Influence: 33.7] [Reference Citation Analysis (0)] |
| 5. | Zong L, Yang J, Wang X, Kong Y, Ren T, Zhao J, Feng F, Wan X, Xiang Y. Management and prognosis of patients with liver metastases from gestational trophoblastic neoplasia: a retrospective cohort study. Cancer Manag Res. 2018;10:557-563. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 6. | Barnard DE, Woodward KT, Yancy SG, Weed JC, Hammond CB. Hepatic metastases of choriocarcinoma: a report of 15 patients. Gynecol Oncol. 1986;25:73-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Ranga R, Parekh C, Mankad M. Unusual Presentation of Gestational Trophoblastic Disease with Isolated Liver Metastases, Skipping Lungs: Case Report and Review of the Literature. Indian J Gynecol Oncol. 2018;16:38. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 8. | Menegaz RA, Resende AD, da Silva CS, Barcelos AC, Murta EF. Metastasis of choriocarcinoma to lumbar and sacral column. Eur J Obstet Gynecol Reprod Biol. 2004;113:110-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Lee JH, Park CW, Chung DH, Kim WK. A case of lumbar metastasis of choriocarcinoma masquerading as an extraosseous extension of vertebral hemangioma. J Korean Neurosurg Soc. 2010;47:143-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Soper JT, Mutch DG, Schink JC; American College of Obstetricians and Gynecologists. Diagnosis and treatment of gestational trophoblastic disease: ACOG Practice Bulletin No. 53. Gynecol Oncol. 2004;93:575-585. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 94] [Article Influence: 4.5] [Reference Citation Analysis (0)] |