Published online Aug 26, 2020. doi: 10.12998/wjcc.v8.i16.3527
Peer-review started: May 5, 2020
First decision: May 21, 2020
Revised: May 27, 2020
Accepted: July 30, 2020
Article in press: July 30, 2020
Published online: August 26, 2020
Processing time: 112 Days and 1 Hours
Giant ovarian cysts (≥ 15 cm in diameter) are rare. The size limit of cysts and the methodology for a safe and successful minimally invasive surgery has not been established. Here we report a case of a large 10-kg multi-locular ovarian mass, which was successfully laparoscopically removed: Our aim was to innovate the surgical practice in this field by providing a safe, effective, and minimally invasive management method for such complex and rare cases.
A 49-year-old nulliparous woman presented with abdominal distension, lasting from six Mo prior to admission; she reported worsening abdominal pain, abdominal swelling, and mild dyspnea. Imaging showed a presumed benign multi-locular (> 10 locules) left ovarian cyst that measured about 30 cm in diameter. Based on the IOTA-ADNEX model the mass had a 27.5% risk of being a borderline or malignant tumor. The patient was successfully treated via a direct laparoscopic approach with salpingo-oophorectomy, followed by the external drainage of the cyst. Tumor spillage was successfully avoided during this procedure. The final volume of the drained mucinous content was 8950 L; the cyst wall, extracted through the minilaparotomy, weighed about 1200 g. The pathologic gross examination revealed a 24 cm × 15 cm × 10 cm mass; the histologic examination diagnosed a mucinous cystoadenoma. To our knowledge, this is the first case of a giant multi-locular ovarian cyst treated with a direct laparoscopy with salpingo-oophorectomy followed by external decompression.
Choosing the appropriate technique and surgeon skill are necessary for a safe and effective minimally-invasive approach of unique cases involving giant ovarian cysts.
Core tip: To date, there are no standard guidelines regarding the maximum size of cysts that can be safely and effectively laparoscopically treated. To our knowledge, our case report is the first to describe a very large multi-locular ovarian cyst weighing 10150 g that was treated via a direct laparoscopic approach with salpingo-oophorectomy, followed by external decompression. Choosing the most appropriate technique is necessary for safely and effectively treating unique cases involving large cysts, and this choice is dependent on the experience and efficiency of the surgical team.
- Citation: Sanna E, Madeddu C, Melis L, Nemolato S, Macciò A. Laparoscopic management of a giant mucinous benign ovarian mass weighing 10150 grams: A case report. World J Clin Cases 2020; 8(16): 3527-3533
- URL: https://www.wjgnet.com/2307-8960/full/v8/i16/3527.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i16.3527
Giant ovarian cysts (≥ 15 cm in diameter) are rare in women of reproductive age.
To date, all reported techniques for managing such cysts include the preventive decompression of the cyst, followed by laparoscopic cystectomy and/or the removal of the adnexa[1,2]. However, the methodology for performing these techniques have not been fully standardized, and these techniques are technically complex, especially in cases of multi-locular masses. Moreover, the size limit of cysts for determining appropriate, safe, and successful minimally invasive surgery has not been established[3].
The minimally invasive management of giant adnexal cysts with laparoscopic adnexectomy as first step has yet to be described.
Herein, we describe a case of a large 10-kg multi-locular ovarian mass with no signs of malignancy. This mass was successfully treated via laparoscopic salpingo-oophorectomy, followed by the external drainage of the cyst without tumor spillage.
Our aim is to attempt to innovate the surgical practice in this field by providing a safe, effective, and minimally invasive management method for such complex and rare cases.
A 49-year-old nulliparous Philippine woman who was admitted to the Department of Gynecologic Oncology, Azienda Ospedaliera Brotzu Hopital in Cagliari, Italy, presented with abdominal distension, which had been present for six Mo prior to admission.
She reported worsening abdominal pain, abdominal swelling, and mild dyspnea. Moreover, she had not experienced any vomiting or urinary symptoms.
She had no previous history of any illnesses.
Upon physical examination, we determined that she was afebrile and peripheral edema was not present. Further, her abdomen was distended by a pelvic-abdominal mass that extended from the pubic symphysis to approximately 1 cm under the xiphoid process (Figure 1A).
She had no family history of malignancies and had a body mass index of 18.5 kg/m2.
The patient’s tumor marker levels were as follows: 23.5 U/mL of CA 125 protein (normal range, < 35 U/mL), 1.0 ng/mL of carcinoembryonic antigen (normal range, 0-5 ng/mL), 62 U/mL of Ca 19.9 (normal range, < 37 U/mL), 5.7 U/mL of CA 15-3 (normal range, 0-32.4 U/mL), and 32.2 U/mL of HE4 (normal range < 70 U/mL).
An abdominal ultrasound examination revealed a multi-locular (> 10 locules) mass that measured about 30 cm in diameter. No papillary projections, blood flow, or ascites were detected in the mass. Based on the patient’s clinical characteristics and ultrasound findings, the IOTA-ADNEX Model indicated a 72.6% chance of a benign tumor, 16.5% chance of a borderline tumor, 8.9% chance of stage I ovarian cancer, 0.4% chance of stage II-IV ovarian cancer, and 1.7% chance of metastatic cancer to the adnexa.
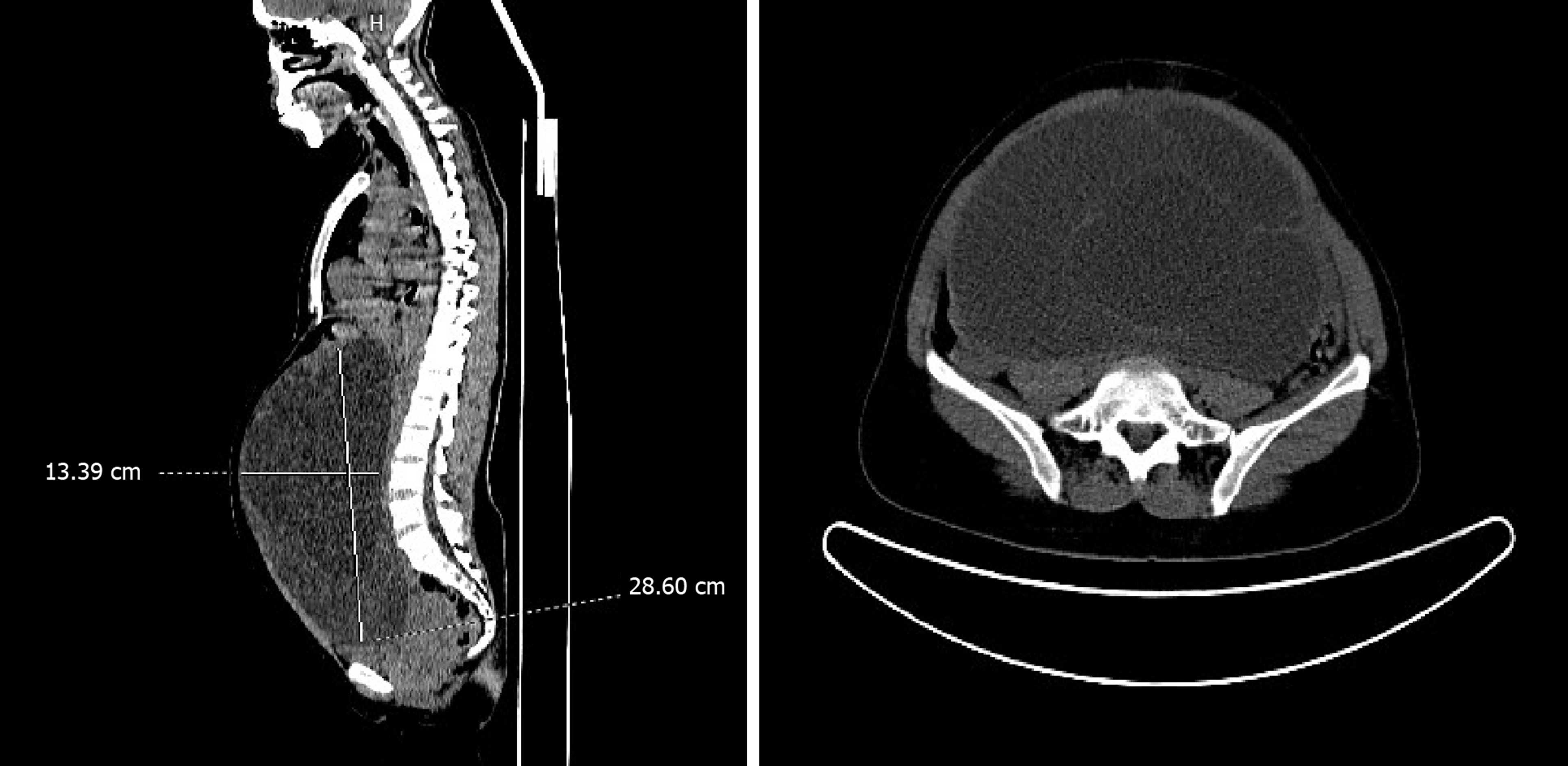
The patient also underwent a computed tomography (CT) scan of her abdomen, which revealed a mass that spanned from the pubic symphysis to the xiphoid process (Figure 2). The mass presented with internal septations, but no solid components were observed. The CT retroperitoneal examination did not reveal lymphadenopathy or metastasis. The uterus and adnexa were not visible at CT.
The final diagnosis was a multi-locular ovarian cyst.
The patient was counselled and signed informed consent for laparoscopic bilateral salpingo-oophorectomy, total hysterectomy, omentectomy, and laparotomy, as needed. The case report was performed in accordance with the institutional ethics committee guidelines and the Helsinki Declaration principles. Written informed consent was obtained from the patient for the publication of this case report and the accompanying images.
In order to visually assesses the patient’s large abdominal mass and avoid rupturing the cyst and spilling its contents during cyst removal, we performed open-entry laparoscopy with an approximately 1 cm incision, in which a 10-12 mm trocar was inserted just below the xiphoid process. Agg 0 degree.
A pneumoperitoneum pressure of 12-14 mmHg was achieved and was maintained throughout the procedure. Another 10-12 mm trocar was placed directly in the periumbilical position, two ancillary 5-mm trocars were placed bilaterally in the lower abdominal quadrants, and another 5-mm trocar was placed in the suprapubic region.
The surgery was performed under general anesthesia with the patient in the lithotomy position. Throughout the procedure, the surgical table was put in the Trendelenburg position. The angle was modified accordingly to the anesthesiologist’s needs at different phases of the surgery.
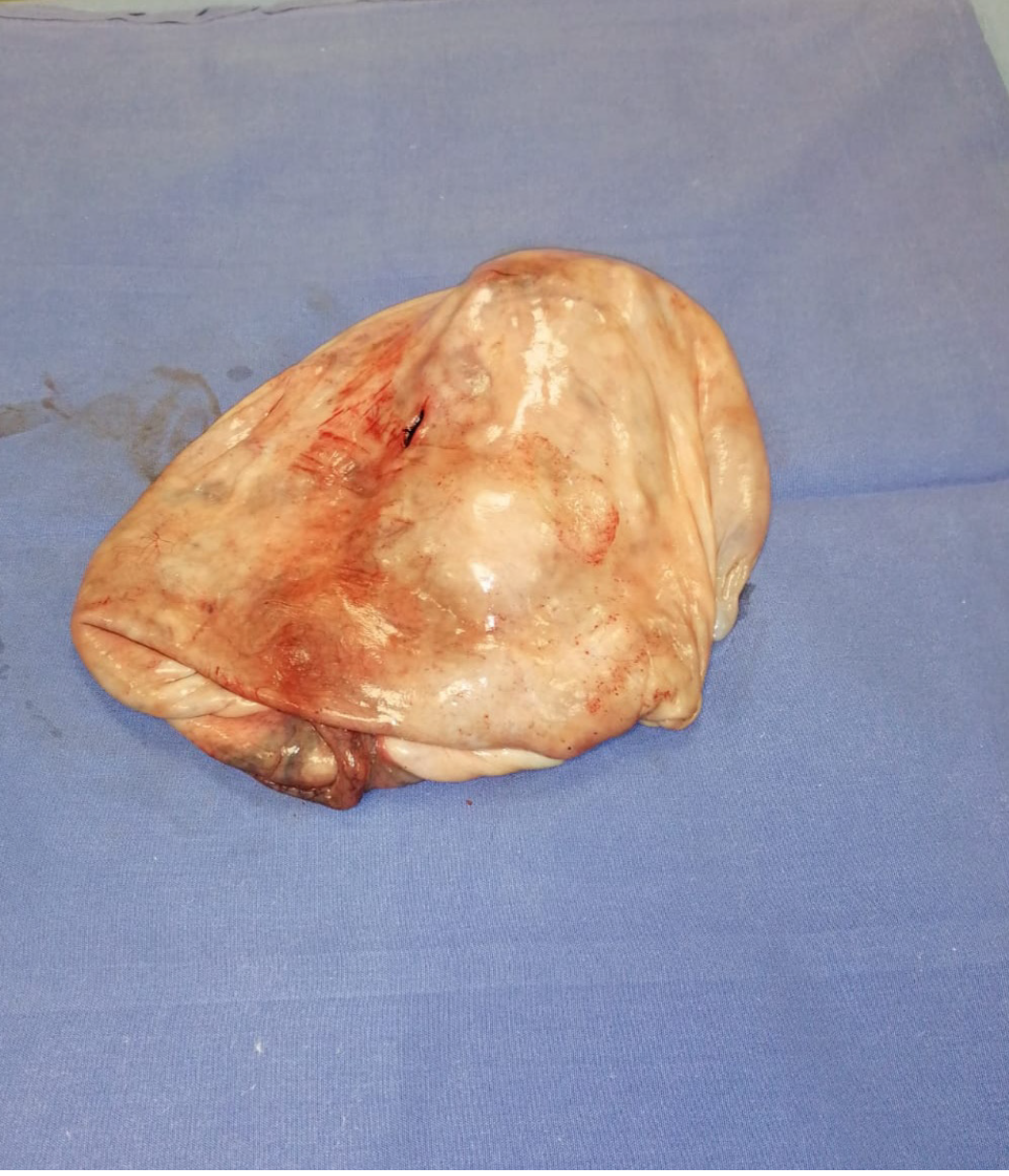
Through the laparoscope, the abdominal cavity could only be partially visualized because the large cyst was in the way. However, we were able to observe the cyst’s origin from the left ovary, by moving away parts of the mass by a laparoscopical device. After visually examining the abdominal cavity and large mass, we started left salpingo-oophorectomy under laparoscopy guidance with the coagulation and transection of the left round ligament using a Ligasure device (Tyco Healthcare, AutoSuture Co., United States, Surgical Corp., Norwalk, CT), preparation of the left infundibulo-pelvic ligament, coagulation of the left infundibulo-pelvic ligament using BiClamp LAP forceps (ERBE GmbH, Tubingen, Germany), and following transection using Ligasure (Tyco Healthcare, AutoSuture Co., United States, Surgical Corp., Norwalk, CT). Subsequent mobilization of the adnexa toward the upper abdomen and visualization of the pelvis revealed an enlarged fibromatous uterus, almost double the normal size, and an approximately 3-4-cm ovarian cyst in the right adnexa. Afterwards, a minilaparotomy was made at 4 cm above the umbilicus. The mini-laparotomy incision was protected using a wound protector/retractor (Wound Edge Protector–3MTM Steri-DrapeTM 1073, Diegem, Belgium). Then, through a mini-open procedure the cyst was externally decompressed via the aspiration of each locular component by multiple punctures completely draining their contents except two sub-compartments that were not drained because the cyst could exit by the mini-laparotomy. Indeed, the cyst was gradually removed in this way until the mass was completely extracted. The tumor spillage was successfully avoided during this part of the procedure. The final volume of the drained mucinous content was 8950 L. The cyst wall was then extracted through the minilaparotomy (Figure 3). It weighed about 1200 g.
Afterwards, we re-sutured the mini-laparotomy incision, we induced the pneumoperitoneum again, and laparoscopically visually assessed the abdominal cavity. The liver, gallbladder, spleen, and diaphragm appeared normal, and there were no macroscopic signs of malignancy. As such, we proceeded with omentectomy, total laparoscopic hysterectomy, and right salpingo-oophorectomy in accordance with our previously described technique[4]. The removal of the uterus, right adnexa, and omentum was performed through the vagina. The vaginal cuff was then laparoscopically sutured with a V-Loc wound closure device (Covidien-Medtronic, Minneapolis, MN, United States).
No blood loss or other intraoperative complications occurred. The total operative time was 180 min. The patient had an uneventful recovery and was discharged on postoperative day 2. Figure 1B showed the cosmetic after surgery (Figure 1B).
The pathologic gross examination revealed a 24 cm × 15 cm × 10 cm mass with an intact smooth wall. A histologic examination showed that the cyst wall was composed of a single layer of columnar epithelium without cytologic atypia. The final diagnosis was mucinous cystoadenoma.
Herein, we describe, for the first time at our knowledge, a case of a large 10-kg multi-locular presumed benign ovarian mass that was successfully treated via laparoscopic salpingo-oophorectomy, followed by the external drainage of the cyst without tumor spillage. Laparoscopy is the gold standard treatment for presumed benign ovarian cysts that range between small and moderate in size[5]. However, there are currently no standard guidelines or consensus for how to manage large (> 10 cm) and very large (up to the umbilicus) ovarian cysts and what the maximum ovarian cyst size should be for safe and effective laparoscopic management. The main concern regarding laparoscopic management of giant ovarian cyst is the potential risk of the capsular rupture of an unexpected ovarian cancer, resulting in cyst content spillage into the peritoneum and subsequent seeding. This has resulted in the reluctance of performing minimally invasive surgery in women with large adnexal masses[3]. However, a laparoscopic approach has been increasingly preferred due to current advances in mini-invasive surgery, including the introduction of innovative devices and techniques that have been shown to avoid tumor spillage, result in shorter hospital stays, provide better cosmetic results, and are well known for being minimally invasive.
In current literature, the laparoscopic management of large masses has been based on a preventive laparoscopic or percutaneous decompression of the cyst, followed by laparoscopic cystectomy and/or the removal of the adnexa[6-9]. This approach is typically chosen due to the limited working space during laparoscopy, which is overcome by the preliminary aspiration of cyst contents.
In our case, the presumed benign cyst was multi-locular and, based on the IOTA-ADNEX model, had a 27.5% risk of being a borderline or malignant tumor[10]. This was our reason for implementing a direct laparoscopic approach with adnexectomy using Ligasure, followed by the accurate external decompression of the cyst. We also chose this approach because the inability to completely mobilize the mass did not make it possible to perform initial decompression of multiple chambers. Further, this approach completely eliminated the risk of cyst content spillage into the peritoneum. To date, there has only been one report of a case involving the decompression of a giant multi-locular cyst. In this case by Leys et al[11] the first surgical steps were performed transcutaneously and, therefore, completely blind. As such, it was not possible to verify any potential cyst content spillage. Moreover, in cases where there is an approximate 30% risk of a borderline or malignant mass, like in our case, a technique that strictly avoids cyst content spillage is required.
In fact, the spillage of the cyst content in case of ovarian malignancy may worsen patient prognosis even if different studies obtained controversial findings. Some authors[12-14] found that in case of stage 1 epithelial ovarian cancer intra-operative cyst rupture did not influence the rate of relapse or prognosis. Vice versa, other authors reported that intraoperative rupture of stage 1 ovarian cancers worsened patient prognosis[15-17], even if in the tumor grade remained the most powerful indicator of disease free survival[17]. A retrospective analysis carried out including 194 patients with stage I mucinous ovarian carcinoma showed that capsule rupture was a significant negative prognostic factor for overall survival[18]. Noteworthy, intraoperative spillage of a mucinous cystadenoma may potentially cause pseudomyxoma peritonei. However, this condition is usually already detectable at the time of initial surgical laparoscopy inspection of the abdomen and is mostly associated with a diagnosis of mucinous cystadenocarcinoma[19,20].
Unfortunately, a direct laparoscopic approach with initial salpingo-oophorectomy for treating giant ovarian cysts can be extremely technically difficult because of the limited working space. It was due to the vast experience that the surgical team had in performing such complex techniques that allowed for the surgical outcomes in our case[21,22]. Therefore, a certain amount of experience in mini-invasive surgery for treating giant cysts and very large fibromatous uteri is required to successfully perform this procedure.
Another key requisite for successful surgery in our case was the modification of trocar position based on cyst size and the surgeon’s requirements. Particularly, the position of the 10-12 mm trocar placed just below the xiphoid process, which was placed via open procedure, was crucial in providing safe access to the mass and, therefore, avoiding cyst rupture. It also allowed for the best possible view when managing large abdominal masses. Moreover, the positioning of the periumbilical trocar was fundamental in allowing for the mobilization of the giant mass and the accurate assessment of the anatomy and identification of the adequate anatomical plans for safely performing the procedure.
To our knowledge, our case report is the first to describe a very large multi-locular ovarian cyst that was treated via a direct laparoscopic approach with salpingo-oophorectomy, followed by external decompression. To date, there are no standard guidelines regarding the maximum size of cysts that can be safely and effectively laparoscopically treated. Choosing the most appropriate technique is necessary for safely and effectively treating unique cases involving large cysts, and this choice is dependent on the experience and efficiency of the surgical team.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Chong CS, Norčič G S-Editor: Zhang L L-Editor: A P-Editor: Wang LL
| 1. | Dolan MS, Boulanger SC, Salameh JR. Laparoscopic management of giant ovarian cyst. JSLS. 2006;10:254-256. [PubMed] |
| 2. | Pelosi MA, Pelosi MA. Laparoscopic removal of a 103-pound ovarian tumor. J Am Assoc Gynecol Laparosc. 1996;3:413-417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 3. | Ghezzi F, Cromi A, Bergamini V, Uccella S, Siesto G, Franchi M, Bolis P. Should adnexal mass size influence surgical approach? A series of 186 laparoscopically managed large adnexal masses. BJOG. 2008;115:1020-1027. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 40] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 4. | Macciò A, Chiappe G, Kotsonis P, Nieddu R, Lavra F, Serra M, Onnis P, Sollai G, Zamboni F, Madeddu C. Surgical outcome and complications of total laparoscopic hysterectomy for very large myomatous uteri in relation to uterine weight: a prospective study in a continuous series of 461 procedures. Arch Gynecol Obstet. 2016;294:525-531. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 23] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 5. | Practice Bulletin No.174 Summary: Evaluation and Management of Adnexal Masses. Obstet Gynecol. 2016;128:1193-1195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 6. | Song T, Sung JH. Leak-proof technique in laparoscopic surgery for large ovarian cysts. J Obstet Gynaecol. 2020;1-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | Dubuisson J, Fehlmann A, Petignat P. Management of presumed benign giant ovarian cysts: a minimally invasive technique using the Alexis Laparoscopic System. J Minim Invasive Gynecol. 2015;22:540. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Yi SW. Minimally invasive management of huge ovarian cysts by laparoscopic extracorporeal approach. Minim Invasive Ther Allied Technol. 2012;21:429-434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Alobaid A, Memon A, Alobaid S, Aldakhil L. Laparoscopic management of huge ovarian cysts. Obstet Gynecol Int. 2013;2013:380854. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 10. | Timmerman D, Testa AC, Bourne T, Ferrazzi E, Ameye L, Konstantinovic ML, Van Calster B, Collins WP, Vergote I, Van Huffel S, Valentin L; International Ovarian Tumor Analysis Group. Logistic regression model to distinguish between the benign and malignant adnexal mass before surgery: a multicenter study by the International Ovarian Tumor Analysis Group. J Clin Oncol. 2005;23:8794-8801. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 329] [Cited by in RCA: 319] [Article Influence: 16.8] [Reference Citation Analysis (1)] |
| 11. | Leys CM, Gasior AC, Hornberger LL, St Peter SD. Laparoscopic resection of massive ovarian mucinous cystadenoma. J Laparoendosc Adv Surg Tech A. 2012;22:307-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Dembo A, Davy M, Stenwig A. Prognostic factors in patients with stage 1 epithelial ovarian cancer. Obstet Gynecol. 1990;75:263–272. [PubMed] |
| 13. | Sevelda P, Dittrich C, Salzer H. Prognostic value of the rupture of the capsule in stage I epithelial ovarian carcinoma. Gynecol Oncol. 1989;35:321-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 80] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 14. | Sjövall K, Nilsson B, Einhorn N. Different types of rupture of the tumor capsule and the impact on survival in early ovarian carcinoma. Int J Gynecol Cancer. 1994;4:333-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 83] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 15. | Webb MJ, Decker DG, Mussey E, Williams TJ. Factor influencing survival in Stage I ovarian cancer. Am J Obstet Gynecol. 1973;116:222-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 105] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 16. | Sainz de la Cuesta R, Goff BA, Fuller AF, Nikrui N, Eichhorn JH, Rice LW. Prognostic importance of intraoperative rupture of malignant ovarian epithelial neoplasms. Obstet Gynecol. 1994;84:1-7. [PubMed] |
| 17. | Vergote I, De Brabanter J, Fyles A, Bertelsen K, Einhorn N, Sevelda P, Gore ME, Kaern J, Verrelst H, Sjövall K, Timmerman D, Vandewalle J, Van Gramberen M, Tropé CG. Prognostic importance of degree of differentiation and cyst rupture in stage I invasive epithelial ovarian carcinoma. Lancet. 2001;357:176-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 480] [Cited by in RCA: 415] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 18. | Kajiyama H, Suzuki S, Yoshikawa N, Kawai M, Nagasaka T, Kikkawa F. Survival impact of capsule status in stage I ovarian mucinous carcinoma-A mulicentric retrospective study. Eur J Obstet Gynecol Reprod Biol. 2019;234:131-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 19. | Novetsky GJ, Berlin L, Epstein AJ, Lobo N, Miller SH. Case report. Pseudomyxoma peritonei. J Comput Assist Tomogr. 1982;6:398-399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 20. | Fernandez RN, Daly JM. Pseudomyxoma peritonei. Arch Surg. 1980;115:409-414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 84] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 21. | Macciò A, Chiappe G, Lavra F, Sanna E, Nieddu R, Madeddu C. Laparoscopic hysterectomy as optimal approach for 5400 grams uterus with associated polycythemia: A case report. World J Clin Cases. 2019;7:3027-3032. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 4] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 22. | Macciò A, Madeddu C, Kotsonis P, Pietrangeli M, Paoletti AM. Successful laparoscopic management of a giant ovarian cyst. J Obstet Gynaecol. 2014;34:651-652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |